Symptoms of dyspareunia
Dyspareunia must be clearly distinguished from vaginismus. Vaginismus is a painful spasm of the muscles of the perineum and vagina during sexual intercourse, which can even cause a “block of the penis” in the vagina. Dyspareunia is not accompanied by muscle spasm.
Pain during disparity can be varied both in localization (in the vestibule of the vagina, in the pelvis, on one of the walls of the vagina), and in intensity and duration.
Currently, true dyspareunia is understood as a state of psychological conflict and modulation of pain against the background of disgust or a subconscious block aimed at the sexual partner or sexual intercourse in general in the absence of an organic cause of pain - chronic inflammation of the genitals, a decrease in general hormonal levels in the periclimacteric period, etc.
Symptoms of dyspareunia
A one-time occurrence of pain during or after sexual intercourse is not a symptom of dyspareunia. The disorder manifests itself in this way:
- localization of pain in the area of the external genitalia is characteristic of the onset of sexual intercourse (usually with this symptom it is impossible to begin intercourse);
- pain deep in the vagina appears directly during intercourse with full insertion of the penis;
- the degree of pain can be irritatingly unpleasant (burning, tingling), sharp (stabbing, pulling pain) and severe (pain radiating to the sacrum and anus);
- There is no muscle spasm, which makes it possible to conduct a gynecological examination, in contrast to vaginismus, which is similar in pain symptoms.
Differential diagnosis helps in making an accurate diagnosis, since deep pain is most often caused by organic lesions, and superficial pain (in the area of the external genital organs) most often indicates the psychogenic nature of the deviation.
To make a diagnosis, a series of examinations is prescribed, starting with an examination by a gynecologist and an ultrasound of the pelvis. The next step is laboratory diagnostics of hormonal levels to determine the level of concentration of sex hormones. Smears and bacteriological examination help confirm or refute the presence of infectious inflammatory processes.
In a situation where there are no deviations in all medical indicators, a clinical and psychological examination is prescribed. The main difficulty is that patients usually try to hide the traumatic causes, since these are cases of sexual or physical violence. It is appropriate to conduct a questionnaire to identify anxiety-depressive conditions and neurosis, as well as a conversation with a psychologist.
Treatment of dyspareunia
If organic pathology of the genital organs is excluded, treatment of patients with dysparenia is carried out using conservative methods together with a gynecologist and psychotherapist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Bonisan, cream-gel (lubricant). Dosage regimen: Apply a small amount of cream-gel in a thin layer to the genital area of a woman or man before and/or during intimacy.
- Contex Wave, gel lubricant. Dosage regimen: Apply a small amount of lubricant to the genital area of a man or woman before and/or during intimacy.
Causes
It was already noted above that the causes of this disorder may be psychological or consist in the presence of functional disorders in the functioning of the organs of the reproductive system.
It is impossible to establish which women are predisposed to this disease, and for which of them sex will be painful. However, there is an opinion that those representatives of the fair sex who experience pain during a gynecological examination or insertion of a tampon into the vagina experience symptoms of dyspareunia several times more often than women for whom such manipulations do not present difficulties.
Psychological reasons include a woman’s fear of sexual contact or even the disgust that sex causes. This can occur due to various traumatic experiences that a woman may have experienced in childhood, such as abuse. And it can arise as an independent manifestation in women with weak temperament, for whom sex is only an obligation. Such women are usually cold with their sexual partners, do not experience orgasm, and have a negative attitude towards sex as such. Naturally, they also experience sexual dysfunction, including lack of desire.
Often, dyspareunia can develop as a result of vaginismus, a psychosexual dysfunction that is manifested by spastic contraction of the vaginal muscles and makes it impossible to enter the penis. In some cases, sex is still possible with such dysfunction, since the woman’s pain goes away after the start of friction, but in most cases, sexual contact cannot be accomplished, since even if the man inserts the sexual organ into the vagina, the woman feels severe pain and stops intercourse.
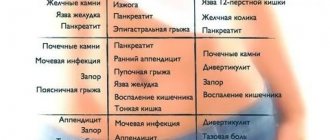
Most often, dyspareunia has physiological causes. Such reasons may lie in various diseases of the pelvic organs. Thus, pathology can develop with the following diseases:
- uterine fibroids;
- endometriosis;
- sexually transmitted infections;
- acute inflammatory processes of the pelvic organs (colpitis, vaginitis, bartholinitis and others).
If we consider other physiological causes, the main place in the development of this disorder is given to vestibulitis - inflammation of the vulva. This phenomenon is often a consequence of pelvic pain syndrome, in which nerve impulses are incorrectly perceived by the nerve centers, and ordinary touches are felt as pain.
Also, the causes of the disorder may be general somatic diseases. For example, dyspareunia can develop in a woman suffering from diabetes, skin diseases or rectal pathologies.
At the same time, such representatives of the fair sex often have a history of various injuries to the genital organs or surgical interventions on the uterus, vagina, intestines or organs of the urinary system.
Of course, painful sex can happen for simple reasons. For example, these are reasons such as:
- incorrectly selected condom;
- discrepancy between the sizes of the male genital organ and the female vagina;
- allergic reaction to latex, lubricant;
- use of an intrauterine device as contraception.
The severity of symptoms can be influenced by the position in which sex is performed and the sexual behavior of the partner (aggression, rudeness). Sometimes women begin to experience pain during coitus because they are subconsciously afraid of contracting sexually transmitted diseases or becoming pregnant.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 24 | 89 | 89 | 90 | 90 |
Diagnosis and treatment
The diagnosis of dyspareunia is made based on an examination by a gynecologist, consultation with a psychologist and sexologist. An ultrasound of the pelvic organs is also performed, which allows to exclude or confirm the presence of organic disorders in a woman, taking smears for infections and cytology. If all tests turn out to be normal, a psychologist and sexologist look for the reasons for the development of the disorder, which requires long-term therapy. And only after the true causes of the disease have been established, appropriate treatment is prescribed.
Treatment of the disorder primarily involves removing the cause that caused dyspareunia. So, if these are infections or inflammatory processes, anti-inflammatory therapy and antibacterial therapy are carried out.
Also, treatment in this case will involve the use of physiotherapeutic methods. In addition, women are recommended to perform special exercises to strengthen the vaginal muscles and learn to control them. Such exercises are good for any sexual dysfunction, for example, anorgasmia, which often accompanies dyspareunia.
Kegel exercises
Exercises are also used when a woman is prescribed psychotherapy, if the causes of the problem lie in psychological or personal characteristics. In this case, Kegel exercises (that's what they are called) are an additional method that the treatment uses, and they allow the woman to learn to control the muscles, and thereby learn to relax during sexual contact, which reduces the severity of painful manifestations.
Sometimes surgical treatment is performed according to indications. For example, when polyps or tumors are found in the uterus and vagina that make sex painful. Usually, after removal of the tumor, dyspareunia, the causes of which were physiological, goes away without a trace, and such women do not need psychotherapy at all.
Psychotherapy is prescribed when no obvious causes of the disease are found. Then the treatment will consist of psychocorrective influence on the woman individually, as well as working with the couple. Also, treatment in this case involves putting the woman into a hypnotic state to identify the causes and ways to rid her of the pathology. Sex therapy and auto-training give good results.
Treatment of pathology in each specific case should be individual, especially if no physical causes have been identified, since the female body is delicate and unpredictable, and only a professional will be able to see what kind of treatment his patient needs to restore her sexual health.
Note that the exercises described above allow women not only to get rid of this disorder, but also to prevent its occurrence. In addition, Kegel exercises can prolong women's sexual activity and increase their level of sensitivity. They also prevent the development of inflammatory processes in the pelvis. Therefore, doctors recommend that women with and without sexual disorders perform these exercises regularly to stay young and sexually active longer.
What to do?
If you think you have Dyspareunia
and the symptoms characteristic of this disease, then doctors can help you: a gynecologist, a sexologist, a psychologist.
Source
Did you like the article? Share with friends on social networks:
Types of dyspareunia
In the classification of dyspareunia, there are two main forms of the disease - primary and secondary. Primary dyspareunia is spoken of in cases where a woman generally has no experience of receiving pleasure and positive emotions from sex. Secondary dyspareunia is indicated by the development of painful/unpleasant sensations in a woman who previously enjoyed sex.
Dyspareunia is also divided into forms depending on the location of the pain. Superficial dyspareunia is distinguished - pain is felt at the entrance to the vagina and is most often a consequence of damage to the labia and structures of the vaginal vestibule; and deep dyspareunia, in which pain is felt deep in the vagina and pelvis, the leading cause of pain is damage to the deep genitourinary structures.
Causes of dyspareunia
Organic reasons:
• Vulvodynia and vestibulodynia; • Pelvic inflammatory diseases: salpingo-oophoritis, endometritis; • Cervical erosion; • Tumor processes in the genitals or pelvic organs; • Hypoestrogenism with vaginal dryness, vestibulitis; As a rule, hormonal levels change during menopause, which introduces some nuances into intimate life.
• Traumatization; ruptures and medical procedures performed during complicated spontaneous childbirth (episiotomy) or for diagnostic purposes;
• Condition after radiation and chemotherapy; For some pelvic malignancies, radiation therapy is performed to shrink the tumor/limit its growth and development. Healthy cells are also affected. Taking cytostatics contributes to vaginal dryness and changes in tissue structure.
• STIs; • Genital candidiasis; • Bend of the uterus; • Skin diseases: lichen sclerosus, lichen planus, eczema, psoriasis; • Side effects of some drugs; Some medications affect sexual desire or arousal, which can reduce lubrication and make sex painful. These include antidepressants, blood pressure medications, sedatives, antihistamines and some birth control pills.
• Hypersensitivity reactions to clothing, latex, spermicides, cosmetics; • Endometriosis; • Developmental anomalies of the female genital organs. The absence of a fully formed vagina, a septum that interferes with intravaginal insertion of the penis, and an imperforate hymen can lead to dyspareunia.
• Bartholinitis; • Irritable bowel syndrome; • Hemorrhoids, fissure in the acute stage.
You shouldn’t delay visiting a doctor if you get rid of the underlying disease, pain during sex goes away with adequate treatment. At the same time, the risk of developing dysparurenia of psychogenic origin remains.
Mechanical rhythmic impact during sexual intercourse on the inflamed uterus, ovary with a cyst/tumor, intestines provokes a pain syndrome, which can stop on its own some time after sex. Violent sexual intercourse can contribute to the rupture of an ovarian cyst and subsequent emergency surgery. Therefore, if there are any signs of trouble, it is necessary to consult a specialist and undergo an examination.
Psychological aspects include depressive and anxiety disorders, stress, disharmonious relationships in couples, sexual violence, mental trauma, etc. In some patients, dyspareunia has a combined origin: pain during sexual intercourse induces fear of sexual relations. Against the background of stress, hormonal levels change, which reduces the secretory activity of the glands and the production of a normal amount of lubricating secretion. Anticipation of pain leads to spasms of intimate muscles, so dysparurenia and vaginismus often accompany each other.
Sexual intercourse involves foreplay, penetration, friction and sexual release. Negative psychogenic factors reduce libido, interfere with sexual arousal, and in severe cases can completely block libido.
Eyjafjallajökull
(Eyjafjallajökull, Eyjafjallajökull, Eyjafjallajökull
)
is the sixth largest glacier in Iceland. Located in the south of Iceland 200 km east of Reykjavik. Under this glacier (and partly under the neighboring Myrdalsjökull glacier) there is a conical volcano without its own name, simply called in the press by the name of the glacier - Eyjafjallajökull.
The height of the peak is 1666 meters, the glacier area is approx. 100 km². A volcanic crater with a diameter of 3-4 km (until 2010 it was covered with glaciers). The volcano is classified as a thyroid volcano. The nearest village (Skogar) is located at the southern end of the glacier. The Skoga River, on which the famous Skogafoss waterfall is located, originates from the glacier.
Writing
- The spelling “Eyjafjallajökull” is present on Soviet and Russian maps: map of Iceland (PKO “Cartography”, GUGK, 1981), Atlas of the World (Roscartography, 1999).
- The spelling “Eyjafjallajökull” is present on Soviet topographic maps produced in the 1960s, in the Great Soviet Encyclopedia, and most scientific works in Russian on the geography and geology of Iceland.
- The spelling "Eyjafjallajokull" is often found in the press and articles. There is also a humorous poem by T. Krasnov in Russian, which makes it easier to remember the name “Eyjafjallajokull”.
- The spelling “Eyjafjalajökull” also appears in printed publications and on Internet sites, for example: Eyjafjalajökull Volcano - Geowikipedia wiki.web.ru;
Slight discrepancies in spelling are due to the complex pronunciation of glacier. According to a study by American linguists, only 0.005% of the world's population can pronounce the name of the glacier correctly.
Name
Translation from (Il. Eyjafjallajökull) - glacier of the island mountains. The name is formed from three words:
- isl. Eyja
- island - isl. Fjall
- mountain - isl. Jökull
- glacier.
Information about volcanic eruptions
After the eruption in 1821-1823, the volcano was considered dormant.
But on March 20, 2010, the volcano began to erupt again with the formation of a fault in the eastern part of the glacier, approx. 0.5 km. No large ash emissions were recorded during this period.
On April 14, 2010, the eruption intensified with the release of large volumes of volcanic ash, which led to the closure of the airspace of about 20 European countries from April 16-20, 2010.
On April 17, a small amount of volcanic ash fell in Moscow. Fragments of plagioclase crystals were observed in it.
On April 17-18, the eruption continued. The height of the eruptive column was estimated at 8-8.5 km. This means that on these days a small fraction of the erupted material entered the stratosphere.
However, according to the Federal Air Transport Agency, 440 flights were unable to take off from Russia on April 18 due to an ash cloud.
On the evening of April 18, the atmosphere over Europe cleared to a large extent. Many airlines conducted test flights (without passengers), and no visible damage to the jet turbines was observed.
Due to the repeated eruption of the Eyjafjallajokull volcano, the airspace had to be closed sporadically in May 2010.
Sources and additional information:
- Eyjafjallajökull - Wikipedia;
- Eyjafjallajökull to everything! - newspaper “Moskovsky Komsomolets” No. 25331 dated April 19, 2010;
- Eyjafjallajokull volcano in Iceland - information;
- Eyjafjalajökull volcano - all about geology;
- Eyjafjallajokull - photographs of the Icelandic volcano;
- 0.005 percent of people can pronounce the name of the Icelandic volcano - Lenta.Ru;
- Eyjafjalajökull volcano - Geowikipedia wiki.web.ru;
- “Eyjafjallajokull” - poem by T. Krasnov;
- The volcano again - the newspaper "Business Petersburg";
- The volcano threatens Europe again - VRN culture.
Literature on the
Eyjafjallajökull
:
- Erik Sturkell et. al. 2010. Katla and Eyjafjallajökull Volcanoes, Developments in Quaternary Sciences, vol 13, 5-21.
- Sturkell, E., P. Einarsson, Freysteinn Sigmundsson, A. Hooper, BGÓfeigsson, H. Geirsson and H. Ólafsson, Katla and Eyjafjallajökull volcanoes, In: The Mýrdalsjökull Ice cap, Iceland — Glacial processes, sediments and landforms on an active volcano . Developments in Quaternary Sciences, vol., 13, eds. Anders Schomacker, Johannes Krüger and Kurt H. Kjær, p. 5-21, 2009.
- Hjaltadottir, S., KS Vogfjord and R. Slunga, 2009. Seismic signs of magma pathways through the crust at Eyjafjallajokull volcano, South Iceland, Icelandic Meteorological office report, VI 2009-013
- Hooper, A., R. Pedersen, F. Sigmundsson, Constraints on magma intrusion at Eyjafjallajökull and Katla volcanoes in Iceland, from time series SAR interferometry, In: The VOLUME project – Volcanoes: Understanding subsurface mass movement, eds. C. J. Bean, A. K. Braiden, I. Lokmer, F. Martini, G. S. O'Brien, School of Geological Sciences, University College Dublin, p. 13-24, 2009
- Larsen, G., 1999. Gosið í Eyjafjallajökli 1821-1823 (The eruption of the Eyjafjallajökull volcano in 1821-1823). Science Institute Research Report RH-28-99. 13 p.m. Reykjavik.
- Oskarsson, Birgir Vilhelm 2009. The Skerin ridge on Eyjafjallajökull, South Iceland: Morphology and magma-ice interaction in an ice-confined silicic fissure eruption. M.Sc. thesis, Faculty of Earth Sciences, University of Iceland. 111 p.
- Pedersen, R., Freysteinn Sigmundsson and Páll Einarsson, 2007: Controlling factors on earthquake swarms associated with magmatic intrusions; Constraints from Iceland, Journal of Volcanology and Geothermal Research, 162,73-80.
- Pedersen, R., Sigmundsson, F., Temporal development of the 1999 intrusive episode in the Eyjafjallajökull volcano, Iceland, derived from InSAR images, Bull. Volc., 68, 377-393, 2006.
- Pedersen, R., F. Sigmundsson, InSAR based sill model links spatially offset areas of deformation and seismicity for the 1994 unrest episode at Eyjafjallajökull volcano, Iceland, Geophys. Res. Lett., 31, L14610, doi:10.1029/2004GL020368, 2004.
- Sigmundsson, F., Geirsson, H., Hooper, AJ, Hjaltadottir, S., Vogfjord, KS, Sturkell, EC, Pedersen, R., Pinel, V., Fabien, A., Einarsson, P. Gudmundsson, MT, Ofeigsson, B., Feigl, K., Magma ascent at coupled volcanoes: Episodic magma injection at Katla and Eyjafjallajökull ice-covered volcanoes in Iceland and the onset of a new unrest episode in 2009, Eos Trans. AGU, 90(52), Fall Meet. Suppl., Abstract V32B-03
Treatment of dyspareunia
If there are confirmed organic causes of dyspareunia, treatment is carried out by specialists of the appropriate profile (gynecologists, urologists, venereologists). Taking into account the identified etiological factors, drug therapy (anti-inflammatory, sedatives, HRT, local anesthetics), gynecological massage, and physiotherapy are prescribed. According to indications, surgical intervention is performed (correction of anatomical defects, vaginoplasty, dissection of the fibrotic hymen, removal of condylomas, removal of Bartholin gland cysts, etc.). If necessary, a suitable method of contraception is selected. For genital prolapse, the use of a uterine ring is recommended.
In the treatment of psychogenic dyspareunia, individual and couple psychotherapy, psychocorrection of a married couple, hypnosuggestive therapy, body-oriented therapy, auto-training, and sex therapy can be used. The goal of psychotherapeutic treatment is to change attitudes towards sexual intercourse, eliminate the expectation of pain, and harmonize marital relationships. Recommendations are given on changing sexual techniques, selecting lubricants, and using techniques to relax the vaginal muscles. It is important to remember that effective elimination of psychogenic dyspareunia is possible only with the interested participation of both partners.
LiveJournal