Carrying a child is an important stage in the life of every woman, and the expected date of birth is one of the most crucial moments. But, when all the dates calculated in advance have already expired, and the baby is in no hurry to be born, this may indicate a post-term pregnancy. With this pathological condition, in most cases, various complications arise for both the expectant mother and the newborn. But don’t worry, the diagnosis of “post-term pregnancy” is very rarely made, because there are errors in any calculations.
Which pregnancy is considered post-term?
According to physiological standards, pregnancy lasts 10 obstetric months (280 days), or 40 full weeks, but not all children are born exactly on time. A pregnancy is considered full-term when the baby is born at 38–40 weeks. If birth occurs much later, doctors sound the alarm. A pregnancy is considered post-term if it lasts more than 42 weeks, and the fetus appears with signs of overripeness. The timing of post-term pregnancy is a conditional indicator that is taken into account when assessing the overall clinical picture.
According to gynecologists, childbirth at 40–42 weeks can be considered normal, especially if the expectant mother and the child in the womb feel satisfactory. If all indicators are normal and childbirth occurs at 41–42 weeks, then the pregnancy is usually called prolonged (extended). Only after 42 weeks is the pregnancy considered post-term, but if the baby is born healthy, this diagnosis is carefully checked.
There are two types of pathology:
- True (biological) post-term pregnancy - this diagnosis is made when childbirth is delayed by 2 or more weeks from the expected date, the fetus is diagnosed with signs of overmaturity.
- Imaginary (physiological) post-term and prolonged pregnancy - despite the delay in labor by 10 days or more, if the placenta retains its functions and provides normal nutrition to the fetus, and the child is born without signs of overmaturity - this is not considered post-term.
There are many cases where a child is born after 42 weeks of pregnancy without signs of overmaturity. Or, conversely, the baby is born on time, in accordance with the preliminary date of birth, but with signs of overmaturity.
Clinical recommendations for post-term pregnancy include careful diagnosis and careful management of pregnancy and childbirth.
To more accurately calculate the expected date of birth, you need to take into account the duration of the menstrual cycle, which is different for all women. With a cycle of more than 28 days, prolonged pregnancy and childbirth after 41 weeks are quite likely. If the cycle is less than 28 days, labor may begin at 36 weeks.
Determining readiness for childbirth using a test
Today there is a special test with which it is possible to determine a woman’s readiness for childbirth. To conduct such a test, you need to take the most comfortable position and put your watch next to it. Now for three minutes you need to irritate the nipples and areolas with your fingers. Next, the hand is placed on the stomach, and by carefully listening to your own sensations, you can track the contractions.
The result can be considered positive if, after stopping the effect on the nipples, the uterus contracts during the first three minutes, and at least three contractions must take place in 10 minutes.
If, at 40 weeks, the test gives only a negative result, then there is a possibility of a post-term pregnancy. However, at the same time, there are cases when the test gives a positive result, but labor is in no hurry to begin. This may be a sure sign that the baby is still not ready to be born.
Causes of the pathological condition
Post-term pregnancy occurs for completely different reasons. Even the psycho-emotional state can affect the delay in childbirth, for example, if a woman is afraid of giving birth or losing a child.
The main causes of post-term pregnancy:
- various menstrual cycle disorders;
- genetic predisposition;
- treatment with hormonal drugs;
- gynecological pathologies;
- endocrine diseases;
- long-term brain injuries;
- diseases of the gastrointestinal tract;
- liver and kidney pathologies;
- malignant tumors;
- inflammatory and infectious processes;
- suffered from influenza or ARVI during pregnancy;
- stress, nervous tension;
- infectious diseases suffered in childhood (measles, rubella, scarlet fever);
- frequent abortions;
- first birth after 35 years;
- large fetus in previous births (from 4 kg);
- breech presentation of the fetus;
- low physical activity (hypodynamia) of a pregnant woman;
- hormonal imbalance, obesity.
It is worth noting that if in the first months of pregnancy various pathological processes are detected, for example, abnormal embryonic development of the fetus, then in many cases childbirth is delayed.
Conducting a study of the general condition of the expectant mother during post-term pregnancy
To make a final decision regarding labor management tactics, it is necessary to conduct a full examination of the pregnant woman to determine her readiness for childbirth. First of all, an examination on a gynecological chair is necessary to determine the maturity of the cervix. If there is immaturity of the cervical canal, slight softening or density, its length is up to 30 mm, deviation towards the sacrum and a closed internal pharynx, the issue of stimulating its maturation is resolved.
Based on the results obtained from CTG supplemented by ultrasound scanning of the fetus, together with the results of urine and blood tests, a conclusion is formed. Every day, the pulse and blood pressure are measured, weight dynamics are measured, and a conversation with the woman about her well-being is measured, which helps the assessment taking into account the data obtained on the baby’s heartbeat, assessed either by a doctor using a stethoscope and listening through the stomach, or using a special fetal monitor.
Important
If the condition is satisfactory, preparations can be made for natural childbirth with stimulation, or the issue of the date of cesarean section can be decided (when the prognosis is unfavorable).
Clinical picture
Symptoms of post-term pregnancy are as follows:
- the volume of the abdomen decreases by 7–10 cm;
- weight decreases by 2–3 kg;
- the density of the uterine walls increases;
- the amount of amniotic fluid decreases;
- immaturity of the cervix is observed;
- the bones of the child’s skull are compacted, the fontanel and bone sutures are tightened;
- milk is released from the milk ducts instead of colostrum;
- fetal hypoxia (lack of oxygen) is observed;
- movement decreases;
- the child’s heart rate slows down, heart sounds are uneven and muffled;
- due to hypertonicity of the uterus, the height of the uterine fundus increases, especially if the child is overweight.
Doctors consider these symptoms to be indirect, since they cannot 100% confirm a post-term pregnancy. But these are characteristic signs that cannot be ignored; sometimes they are an indication for artificial induction of labor.
Medical tactics
Post-term pregnancy is not an indication for cesarean section. The operation is performed only when several relative indications are combined.
Clinical recommendations are based on the condition of the woman's birth canal. If there are signs of cervical maturity corresponding to 7 points on the Bishop scale and above, labor induction is performed. The pregnant woman undergoes an examination, and on the appointed day, early in the morning, an amniotomy is performed - opening the fetal bladder. After a few hours, contractions normally start. If this does not happen, stimulation is carried out with an oxytocin solution in an individually selected dosage.
This tactic is preferable to waiting, because Fetal weight gain continues, which increases the risk of having a large baby. In 0.1% of cases, against the background of complete well-being, intrapartum death occurs, the cause of which cannot be determined.
If the cervix is immature, observation is carried out for some time in anticipation of its spontaneous ripening. But many clinics prefer using prostaglandin gel or kelp sticks to prepare the cervix. Labor is initiated by inducing the Fergusson reflex. The woman is examined in a chair at least twice a week, during which the doctor uses his fingers to peel off the lower part of the amniotic membrane from the walls of the uterus.
The prognosis for the mother and child is based on complications that arise during pregnancy. If there is only postmaturity, this will not have long-term consequences for the newborn. But for women with a predisposition to late delivery, the doctor will suggest giving birth a programmed character. Preparation begins at 39 weeks.
Stages of pathology development
Depending on the degree of the pathological process, post-term pregnancy is conventionally divided into three stages:
- The first stage is characterized by the following signs: rapid heartbeat and excessive activity of the baby, a sharp decrease in the volume of amniotic fluid. This clinical picture develops at 41 weeks of pregnancy, that is, childbirth is delayed by 1 week. The first degree of post-term pregnancy must be correctly identified and distinguished from prolonged pregnancy.
- At the second stage of postmaturity, the pregnant woman experiences more pronounced symptoms - a daily decrease in abdominal volume by 1-2 cm, oligohydramnios, changes in the location of the uterine fundus, and the amniotic fluid becomes cloudy. The fetus has placental insufficiency, hypoxia, muffled heartbeat, rare movements, and signs of overmaturity may appear. Such changes occur when labor is delayed by 2–3 weeks.
- At the third stage, post-maturity is 3–4 weeks, the prognosis for the pregnant woman is extremely unfavorable. Possible disturbances in blood flow in the placenta and its detachment, the volume of amniotic fluid sharply decreases. The condition of the fetus is critical, sometimes secondary malnutrition (lack of body weight) develops, and the child is born in an extremely serious condition. At this stage, doctors take all possible measures for the woman’s successful delivery, most often a caesarean section.
What leads to pathology
The reason for the prolongation of pregnancy is a combination of several factors, but the main influence is exerted by the neuro-endocrine system. The background for pathology can be:
- puberty of the expectant mother occurred later than normal;
- irregular menstrual cycle;
- infantilism of the genital organs;
- history of severe childhood infections;
- diseases of the endocrine system;
- metabolic disorders;
- inflammatory processes in the pelvis;
- mental trauma;
- gestosis;
- pathology of the fetal adrenal glands;
- history of delayed birth.
A pregnant woman may have various pathologies of the reproductive system, uterine fibroids, but their effect on the late onset of labor has not been proven.
The reasons for the onset of labor are hormonal changes. Throughout gestation, the concentration of estrogen increases due to estriol and estrone. The placenta participates in the synthesis of these hormones, but their precursor begins to be produced in the fetal adrenal glands. With developmental anomalies, as well as pathology of the placenta, normal hormonal regulation is disrupted, cervical ripening does not occur and contractions do not appear. Changes in the placenta are considered secondary; they often occur under the influence of natural processes. But disruption of hormone production can lead to a deterioration in fetal metabolism. Placenta previa rarely becomes a causative factor in prolonging pregnancy. More often this condition causes miscarriage.
A child is born late with signs of overmaturity
Diagnostic methods
Diagnosis of post-term pregnancy is carried out after delivery is delayed by one week. To make a diagnosis of “post-term pregnancy”, the doctor takes the following actions:
- Patient interview. It is important for the doctor to establish the exact dates of the last menstruation, knowing which he will be able to calculate the timing of ovulation. The estimated date of conception and the time of the baby’s first movement are also specified.
- Examination and measurements of a pregnant woman. All indicators are compared with the data recorded earlier in the exchange card.
- Ultrasound examination of the uterine cavity. Based on the results obtained, the specialist determines the level of aging of the uterus and the amount of amniotic fluid. Ultrasound allows you to obtain the necessary information to assess the intrauterine condition of the baby, the density of the bones of his skull and the size of the fontanel.
- Dopplerography. This technique determines possible circulatory disorders and allows one to evaluate the vascular bed.
- Amnioscopy – performed in the presence of a dilated cervix. The purpose of the study is to determine the condition of the baby inside the womb using a small amount of amniotic fluid.
Postterm pregnancy: when is hospitalization required?
Experts in the field of obstetrics argue that even mild prematurity is a more favorable pathology for the future of the baby and the mother herself than a pregnancy that is post-term.
Important
Even a few extra days of postmaturity can become a high risk for the baby and the pregnant woman; the danger to life for both increases higher and higher every day. In this regard, today it is not customary to wait a long time for a natural birth; doctors are making attempts to induce labor in order to stimulate the birth of a child naturally.
A woman hospitalized in a maternity hospital due to post-term pregnancy is under special close supervision, since among such births there is a high perinatal fetal mortality during childbirth, in comparison with all other groups (not taking into account deep prematurity). Doctors today do not allow pregnancy to go beyond the 41st week; at this time, hospitalization and preparation for childbirth are carried out, possibly surgically, if conservative tactics of labor induction do not produce results.
Immediately after hospitalization, the woman undergoes an ultrasound examination and Doppler testing of the fetus, CTG and all the necessary tests are prescribed in order to clarify the timing of pregnancy and assess the maternal health and condition of the baby, their readiness for childbirth. Doctors ask the expectant mother in detail about her well-being, noting the slightest changes, comparing dynamics with previous days, and also look at the readiness of the reproductive tract for delivery and the possibility of a natural birth by assessing the size of the fetal head in relation to the maternal pelvis. If it is established that the birth dates are overdue, a council of doctors together with the pregnant woman decides on how and at what time the birth will take place, assessing all the data they have.
Hospitalization can be carried out in three cases:
- as prescribed by a doctor from the antenatal clinic when transitioning according to timing,
- based on the results of examinations and examinations in the maternity hospital, if consultations are prescribed,
- at the request of the woman, when she is only a few days away from PDD and is ready for hospitalization in the maternity hospital.
note
In the presence of a completely physiological course of gestation, relatively physiological indicators of ultrasound screening in combination with fetal CTG data, general good maternal condition and the absence of complaints, before the 41st week of gestation the expectant mother does not necessarily need to be hospitalized in a hospital in advance.
But with postmaturity, starting from the 40th week, instrumental studies, especially CTG, will become frequent in order to objectively monitor the picture of what is happening.
Why is pathology dangerous?
Failure to begin labor at 42–43 weeks is fraught with the development of severe complications for both the pregnant woman and the unborn child. In the last stages of pregnancy, a woman may develop anemia and gestosis (pathological symptom complex), which complicates delayed childbirth.
The most common complications during childbirth are:
- untimely outpouring of water;
- violation of the integrity of the birth canal;
- premature placental abruption;
- ruptures of ligaments and tissues of the birth canal;
- heavy bleeding;
- infectious complications in the postpartum period.
In case of post-term pregnancy, the consequences for the child can be very sad; the development of pathological processes seriously threatens the health and even the life of the unborn baby.
Possible complications in the child:
- development of hypoxia;
- asphyxia (compression of the respiratory tract) during childbirth;
- damage to the respiratory system;
- neurological disorders;
- infectious skin diseases (pustules);
- intracranial hemorrhages;
- limb fractures.
The worst consequence is the death of a newborn during delivery or in the first twelve months of life.
Features of management of post-term pregnancy and childbirth
At week 41, the pregnant woman is admitted to the hospital, where, based on the studies performed, a decision is made on the further direction of pregnancy and childbirth.
It is worth noting that childbirth in this case can occur suddenly without medical intervention. But, taking into account the possible negative consequences of the protracted process of bearing a child, doctors most often opt for drug stimulation of labor.
Before childbirth, medicinal preparation of the cervix is carried out. To activate the labor process, doctors can use a gel with prostaglandin E2. Its action is aimed at softening the cervix and stimulating labor. After this, drugs that cause prenatal contractions begin to be administered.
In the event of the development of irreversible pathological processes, doctors may decide to perform a surgical delivery (caesarean section).
During the management of a post-term pregnancy, the doctor must constantly monitor the baby’s heart rate. At the slightest suspicion of hypoxia, doctors artificially accelerate labor.
Consequences of prolonging pregnancy
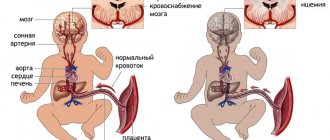
Increasing the duration of pregnancy negatively affects the process of childbirth and the condition of the newborn. An overripe fetus has a significantly larger body weight and head size. Due to the compaction of the fontanelles, the cranium adapts less well to the configuration of the small pelvis, therefore, in post-term infants, lesions of the central nervous system occur in 30% of cases.
By this time, the placenta begins to age, calcifications appear in it, which impair the supply of nutrients and oxygen to the fetus. Chronic fetal hypoxia leads to involuntary bowel movements, and meconium, the original feces, appears in the amniotic fluid. The child swallows this liquid, which can lead to the development of aspiration syndrome.
25% of babies are born weighing more than 4 kg. This condition is called macrosomia. It increases the incidence of birth injuries in newborns.
Women with post-term pregnancies are more likely to have a caesarean section. Therefore, the number of consequences associated with surgical intervention increases:
- bleeding;
- infectious processes;
- urinary retention;
- pulmonary embolism.
Those who are asked to give birth on their own may face the following complications:
- cervical and vaginal ruptures;
- divergence of the symphysis pubis;
- urinary disturbance;
- postpartum ulcers;
- hypotonic bleeding;
- fistulas;
- genital infections.
During pushing, it may be necessary to use obstetric forceps; the consequences of manipulation can be injuries to the nervous system. In post-term pregnancy in combination with placental pathology, the risk of intrapartum fetal death is increased.
What does a post-term baby look like after birth?
As soon as the baby is born, he is examined by neonatologists. Based on the results of the examination, it is possible to diagnose a post-term pregnancy.
The most common consequences of a long pregnancy for a baby:
- unnatural head shape;
- wrinkled greenish or yellow skin;
- protracted fontanel;
- dense skull bones;
- long nails and hair;
- exceeding the norm for weight and height.
As a result of intrauterine growth retardation, a child may appear with hypotrophic signs (low weight, underdevelopment of organs). In the postpartum period, such a baby needs especially careful monitoring during the first year of life.
Signs of postmaturity
But there are still cases of actually post-term pregnancy. This situation usually requires quick delivery, and labor should not be rushed to begin.
What slows down labor and clearly indicates post-maturity?
- A sharp decrease in the volume of amniotic fluid is a prerequisite for the development of weak labor.
- The absence of “anterior waters” (the so-called “flat bladder” that covers the baby’s head) inhibits labor and slows down the dilation of the cervix.
- An immature cervix at 40 weeks indicates a high probability of post-term pregnancy.
- The dense bones of the child's skull, narrow sutures and fontanels make the pushing period more difficult - much more effort will be required from mother and baby.
- The absence of cheese-like lubricant flakes in the amniotic fluid (according to ultrasound data) indicates dry skin of the child, which indicates overmaturity.
- Signs of aging of the placenta, which are easily detected on ultrasound, indicate that the placenta can no longer cope with the needs of a growing child.
- Amniotic fluid cloudy from meconium (the baby's first intestinal secretions) (according to ultrasound data) indicates oxygen starvation of the child.