Outline of the article: 1. Causes 2. Course of the disease 3. Symptoms 4. Diagnosis 5. Treatment 6. Prevention In the autumn - spring period, various inflammatory diseases often occur. Bronchitis and pneumonia are the most common of them. The latter is the most severe disease. In some cases, pneumonia can lead to severe complications and death. But, thanks to developed medicine and modern methods of diagnosis and treatment, inflammation can be treated quite successfully. The leading role belongs to the timely and correct prescription of medications. This article will take a closer look at streptococcal pneumonia.
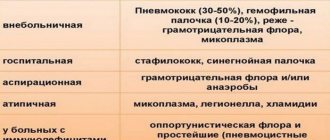
Streptococcal pneumonia is an infectious and inflammatory disease that affects the entire lung tissue, caused by streptococcus. The disease is transmitted by airborne droplets. Infection can occur outside the walls of a medical institution - community-acquired pneumonia, or while undergoing treatment or examination - nosocomial infection.
Causes of streptococcus in the throat
There are several ways for the pathogen to enter the lungs.
Most often it penetrates mechanically through the respiratory tract. This happens with descending inflammation, or with direct exposure of the pathogen from the external environment. In some cases, the pathogen enters the lung tissue through infected blood. This happens with severe bacterial inflammation in other organs and systems, with the development of sepsis.
The rarest variant of pathogen entry is lymphogenous. In this case, the pathogen enters the lungs with the help of lymph from other organs. When the pathogen enters the mucous membrane, it penetrates through it and the remaining layers, and then ends up directly in the lungs. There it begins to develop rapidly under optimal environmental conditions.
Very often, with the rapid growth of the pathological process, the pathogen enters the pleural cavity, causing exudative pleurisy.
C treptococcus is a beneficial, opportunistic or pathogenic microorganism of a spherical shape (which all cocci have). This bacterium is anaerobic, that is, it does not require oxygen for its own life.
This Gram-positive pathogenic agent is considered very common. The average person interacts with streptococcus everywhere, starting from the very first days of life, and sometimes even in the womb during the perinatal period.
Streptococci themselves are heterogeneous and are divided into several types. Such heterogeneity leads to the emergence of several classifications of this microorganism. It would be a mistake to say that all streptococcal structures are dangerous to health. Some of them live in the intestines and have a beneficial effect on digestive processes.
In general, the described organism is mostly dangerous to health and even life. Streptococcus in the throat is always pathogenic. The most common are alpha-hemolytic microorganism (also called simply green), non-hemolytic structures (gamma-type), as well as beta-hemolytic streptococci (the most dangerous).
Lesions of the throat and upper respiratory tract do not arise, as they say, “out of nowhere.” A combination of several factors is required.
The first group concerns the so-called trigger causes that initiate the pathological process. There is only one main trigger factor - a decrease in local (at the level of the pharynx) and general immunity.
What points lead to a decrease in the intensity of the body’s defense system:
- Incorrect, unbalanced diet. The nutritional factor is perhaps the main factor in reducing the body's defenses. A proper diet is recommended, high in vitamins, vitamins, and minerals. Simply put, as much pure protein, plant products as possible and as little fatty, fried, salted, smoked, etc. as possible.
- Helminthic infestations. They “draw” the immune system’s attention to themselves. The most dangerous are opisthorchis and echinococcus. These are deadly organisms.
- Infant feeding disorders. As practice shows, late breastfeeding, early weaning, and transfer to artificial feeding have a bad effect on the newborn’s immune system. There is only one reason - breast milk contains a large number of natural, unique immunomodulators. All the described actions harm the young body. This must be kept in mind when planning your diet at an early age.
- Hypovitaminosis. Avitaminosis. In other words, a lack of vitamins. Included in the structure of the nutritional factor.
- Surgical interventions. Surgeries have a serious impact on the condition of the entire body.
- Taking cytostatics as part of cancer chemotherapy. Cytostatics inhibit the production of actively dividing cells, which include T-lymphocytes and leukocytes. Such patients are literally defenseless against streptococcus.
- Taking antibiotics, especially long-term and uncontrolled. By taking drugs from this group, the patient risks not only his health, but also his life.
- Organ transplantation accompanied by the use of immunosuppressants. These drugs artificially suppress the body's defense system so that the body does not reject the transplanted organ.
- Terminal liver damage. Especially cirrhosis, toxic and other necrosis of hepatocytes.
- Proteinuria (excretion of fats in the urine). In this way, the body removes excess immunoglobulins. Occurs in diseases such as kidney failure.
- Chronic infectious lesions of any anatomical structure of the body. They draw the attention of the immune system towards themselves, which allows new microorganisms to multiply.
- Alcohol abuse.
- Tobacco smoking. It has a particularly strong effect on a woman’s body.
- Long-term stressful situations. Intense physical activity. In a word - factors in the production of excess amounts of corticosteroids, norepinephrine, adrenaline and cortisol. Patients with Itsenko-Cushing syndrome are at particular risk.
The list is incomplete. There are actually many more reasons. Also, the likelihood of developing a streptococcal throat infection is affected by endocrine pathologies such as diabetes mellitus, hypo- and hyperthyroidism, insufficient pituitary function, etc.
Microorganisms entering the bloodstream release toxins that cause intoxication of the body. The patient may experience increased body temperature, nausea, weakness, and lethargy. When streptococcus affects the upper respiratory tract, the following symptoms may appear:
- increase in size, soreness of the submandibular nodes;
- sensation of throat constriction;
- alternating chills with fever;
- pain when swallowing;
- inflammation of the tonsils, the appearance of purulent plaque on them;
- hemorrhages - hemorrhages in various parts of the body;
- nasal discharge;
- difficulty breathing.
Doctors decide on treatment tactics after conducting diagnostic measures and identifying the causative agent of the disease. Streptococcal infection that affects the respiratory system requires an integrated approach to treatment. The treatment regimen includes the following activities:
- Bed rest is mandatory, especially in case of high body temperature.
- Drink plenty of fluids to flush out toxins.
- For throat diseases, switch to soft foods.
- Taking vitamins and minerals in the form of medications and food.
- Inhalations with drugs.
- Physiotherapy.
The treatment of infections caused by streptococcus pneumoniae involves the use of medications. Doctors prescribe to patients:
- Antibacterial drugs to destroy the pathogen.
- Diuretics to remove toxins.
- Antipyretics – to reduce high body temperature.
- Antiseptics - for gargling, rinsing the nose.
- Probiotics to restore intestinal microflora.
- Antihistamines - to eliminate allergy symptoms.
Infectious inflammation, which causes streptococcus pneumoniae, requires antibacterial therapy from the first days of treatment. Streptococcus pneumoniae is active against antibiotics of the penicillin group such as Amoxiclav, Ampicillin, Amoxicillin. In case of intolerance to these drugs or in the absence of treatment results, antibacterial agents of the following groups are prescribed:
- macrolides – Azithromycin, Clarithromycin;
- cephalosporins – Cifralex, Cephalexin;
- sulfonamides – Sulfadimezin, Sulfadimethoxine.
Treatment of infections caused by streptococcus pneumoniae requires the use of medications:
- If allergic reactions develop, use antihistamines Loratadine, Zodak, Suprastin.
- To restore intestinal microflora after taking antibiotics - Bifidumbacterin, Acepol, Linex.
- To eliminate the causative agent of pneumonia - the drug Bacteriophage streptococcal.
- For the purpose of detoxification of the body, removing toxins in the urine - diuretics Furosemide, Lasix, Hypothiazide.
When treating diseases of the upper respiratory tract, doctors prescribe the following medications:
- Immunal, Imudon are immunostimulants that support the body's defenses.
- Ibuprofen, Paracetamol - reduce high body temperature.
- Furacilin, Dioxidin - solutions for rinsing when streptococcus pneumonia in the throat is diagnosed.
- Eufillin, Solutan - improve breathing and sputum discharge during inhalation.
After the symptoms of intoxication have been relieved and the temperature has decreased, physiotherapy is prescribed to treat pneumonia caused by streptococcus. The procedures help relieve inflammation, activate blood circulation, and ease breathing. Popular physiotherapeutic techniques include:
- Inhalations - thin sputum, improve bronchial drainage, lung ventilation, reduce cough, and facilitate breathing.
- Electrophoresis with drugs - increases the body's resistance, eliminates shortness of breath, produces an anti-inflammatory effect.
Streptococcal pneumonia is treated with physiotherapeutic procedures when the disease leaves the acute stage of development. During this period, doctors prescribe the following treatment methods to patients:
- Inductothermy is exposure to a high frequency magnetic field. During the session, metabolic processes, lymph circulation, and inflammation are reduced.
- Chest massage – activates the drainage function of the respiratory system.
- Microwave therapy (MW) – treatment with an electromagnetic field eliminates the inflammatory process.
To improve the patient’s condition during infection and to ease breathing, doctors recommend the following procedures:
- UHF therapy - exposure to an electric field accelerates resorption processes and increases blood circulation.
- Acupuncture – activates metabolism, improves immunity.
- Therapeutic physical education - exercises stimulate the discharge of sputum and improve blood circulation.
Methods to combat the disease
Treatment of pneumonia includes a whole range of measures. It all starts with the use of penicillin antibiotics. Products such as Amoxicillin or Ampicillin are excellent. If you are allergic to these medications, use Vancomycin. The optimal dosage and duration of therapy is prescribed by the attending physician.
Along with drug treatment, they resort to physiotherapeutic procedures and special physical training.
It is necessary to supplement the set of measures to eliminate pneumonia with breathing exercises.
Physiotherapeutic methods speed up the healing process. If the illness is accompanied by severe fever and symptoms of severe intoxication of the body, physiotherapy is not used. In this case, it is recommended to use jars, mustard plasters and make special compresses.
Electrophoresis. This method is useful for pneumonia, it allows you to speed up resorption and relieve inflammation from the affected area. During this procedure, calcium chloride and lidase are used. If the patient has severe bronchospastic syndrome, magnesium sulfate is used. If there is severe pain, resort to novocaine.
Inhalation therapy. It improves lung ventilation and relieves inflammation. It is prescribed exclusively by the attending physician. It all depends on the phase of pneumonia and its course. Bioparox is often used for inhalation.
UHF electric field. This method is necessary in order to provoke resorption of the lesion in a shorter time. Its action is aimed at increasing blood circulation and reducing signs of intoxication.
Inductothermy. This method involves influencing the body with a special magnetic field of high frequencies. This allows you to speed up metabolism, enhance lymph circulation and relax smooth muscles. This method is used for aseptic purposes.
Microwave therapy. Its action is to influence the body of waves of different frequencies. Therapy is used to improve breathing and relieve inflammation.
Applications and acupuncture. When the main symptoms of the disease begin to subside, these methods are resorted to. They are able to improve the functions of the body and relieve a person from vegetative-somatic disorders.
Physiotherapeutic methods are widely used to treat both children and adults. Drug treatment alone is not enough to fully restore lung function. Elimination of the disease must be comprehensive.
Streptococcus pneumoniae: characteristics, pathogenicity, diagnosis, treatment
Streptococcal pneumonia is an inflammation of the lung tissue that is caused by bacteria of the genus streptococcus pneumoniae.
Pneumonia caused by streptococcus pneumonia is relatively rare - in approximately 1/5 of all cases of pneumonia in children and adults. Due to the specificity of the pathogen, the disease begins acutely. Rapidly developing symptoms almost always force the patient to consult a doctor, which facilitates timely initiation of treatment.
In very rare cases, streptococcal inflammation is asymptomatic, which is typical for latent pneumonia.
Most often, the microorganism streptococcus pneumoniae lives in the upper respiratory tract, affecting them:
- Streptococcus in the nose causes rhinitis.
- In the throat - sore throat.
- In the throat, streptococcus causes pharyngitis and laryngitis.
The seasonality of inflammation characterizes the need of the pathogen in environmental conditions. Since bacteria prefer moist, warm air, such inflammation most often occurs in autumn or spring.
Streptococcal pneumonia is very often a complication of other diseases caused by this pathogen, but in some rare cases it can enter directly into the lung tissue without affecting other organs and systems.
Most often, the disease occurs against the background of measles, influenza, chicken pox, or whooping cough.
Streptococcus often causes pneumonia in children. This is due to the anatomical and physiological structure of the lungs and airways.
Streptococcus pneumoniae (streptococcus pneumoniae, pneumococcus) is an opportunistic microorganism that is a natural inhabitant of the human respiratory system and is localized mainly in the nasal cavity, pharynx, bronchopulmonary apparatus and other organs. Pneumococcus causes the development of an inflammatory process only under certain negative conditions that weaken the immune defense and reduce the overall resistance of the body.
Streptococcus pneumoniae is the causative agent of lobar pneumonia, pharyngitis, tonsillitis, rhinitis, sinusitis, and otitis media. Streptococcus pneumoniae can grow and multiply in oxygen-free conditions. Penetrating into the systemic bloodstream, the microbe spreads throughout the body, causing secondary infection of internal organs - meninges, joints, bones, endocardium, peritoneum, subcutaneous fat. The peak incidence of pneumococcal infection occurs in the autumn and spring, when the air becomes quite warm and humidified.
Pathological processes caused by streptococcus pneumonia are more often diagnosed in children. This is due to the structural and physiological features of the respiratory organs, as well as an imperfect immune system. Streptococcus pneumoniae is a pneumotropic microorganism that causes severe bronchopulmonary diseases in the elderly and immunocompromised individuals. The microbe can cause the development of purulent complications.
Pneumococcal pneumonia is a dangerous disease that is a consequence of inflammatory processes in other organs of the respiratory system. The microbe rarely enters the lung tissue directly. Pneumococcal pneumonia has high mortality rates among children throughout the world. The alveoli of the lungs lose their airiness and are filled with purulent exudate.
As a result, patients experience shortness of breath, cough and fever, breathing becomes rapid and difficult, and the chest retracts while inhaling. Streptococcal pneumonia is characterized by rapid development. Early referral of patients to a doctor prevents the pathology from transforming into an advanced form thanks to timely treatment. In extremely rare cases, pneumococcal inflammation is asymptomatic.
Diagnosis of pathology caused by Streptococcus pneumoniae is based on data obtained during microbiological examination of sputum, blood, and pleural exudate. X-ray or tomographic examination of the lungs can confirm the diagnosis of pneumonia. All patients are prescribed etiotropic antimicrobial treatment with antibiotics from the group of penicillins, macrolides, aminoglycosides, and cephalosporins.
Development scheme
Streptococcal infection
When the streptococcus pathogen enters the lymph, internal organs become infected. Depending on the location of the disease, streptococcus pneumoniae is classified into several types.
In the nose
As a result, inflammation occurs in the nose, and many mistakenly believe that the infection will not go further than the nose, but streptococcus gets into the ears and can even affect the brain. Initially, green, viscous nasal discharge begins to appear.
In the throat
With further development of the infection, mucus from the nasopharynx enters the larynx and irritates it. As a result, a sore throat and a dry cough appear in the throat. Yellowish mucus is often visible on the palatine arches and tongue . In some cases, the sore throat becomes constant, and a purulent plaque (gray) appears on the enlarged tonsils.
Thus, streptococcus pneumonia was initially in the nose, but it reached the throat and then can get into the lungs.
In the respiratory tract
Once a child develops pronounced shortness of breath and coughs up viscous sputum mixed with blood, we can safely say that a bacterial infection has spread through the respiratory tract and developed into pneumonia.
Staphylococcal infection
Staphylococcal pneumonia usually develops against the background of other acute respiratory viral infections, so its movement in the body can be schematically divided into several stages.
Runny nose
The child's eyes begin to water, and clear mucus appears from the nose. A rash sometimes appears on the skin.
Pharyngitis
In addition to watery eyes, hoarseness and a dry cough are added. Swallowing is difficult.
Pneumonia
The cough gradually turns from dry to wet: when coughing, mucopurulent sputum of a yellowish-green color appears. Shortness of breath is clearly heard. At this stage, even the lungs can be affected: purulent processes begin in them.
Briefly about the dangers of streptococcal structures
The described pathogenic agents in the throat are dangerous in all cases and need to be gotten rid of as quickly as possible.
- Hemolytic structures are capable of dissolving tissues and blood cells (hemo - blood, lysis - dissolve). This is a direct path to hematological disorders. Since streptococcus spreads throughout the body, generalized damage to the circulatory system can be expected. The process is accompanied by the destruction of red blood cells and the release of large amounts of hemoglobin (pathognomonic sign).
- Streptococcal agents can quickly spread throughout the body through the blood and lymph. This causes the possibility of damage to distant tissues and organs. In addition to classic infections of the upper respiratory tract, the described organisms can provoke pneumonia, acute bronchitis, abscesses, lesions of the gastrointestinal tract, and disrupt the functioning of the heart (many people know the thesis that carious teeth and a sore throat harm the heart, this is true “thanks to” staphylococcus).
- Alpha- and especially beta-hemolytic streptococci are able to resist many antibiotics and adapt to changing conditions. Such resistance causes difficulties in treatment. Before prescribing a course of therapy, it is necessary to accurately determine the sensitivity of the flora to antibacterial agents. Treating “by eye” is useless and even harmful.
A streptococcal throat infection is often compared to Staphylococcus aureus infection. If we consider the second microorganism, it is definitely more difficult in terms of control, and also more aggressive. But it causes mostly purulent processes.
Streptococcus more often provokes problems with the circulatory system. Although both agents belong to the pyogenic (pyogenic) flora. Many diseases caused by streptococci occur in a latent, latent or sluggish form. This makes diagnosis difficult.
Approaches to the treatment of streptococcus in children
The main principle of treatment of streptococcal infection is its timeliness. Since the earlier therapy is prescribed, the less likely it is to develop complications.
Drug therapy
Treatment with drugs can be divided into local and general therapy. The latter includes the prescription of antibacterial agents. Antibiotics should be prescribed in accordance with the isolated pathogen and should be selected according to the sensitivity of the bacteria to them. More often, drugs from the group of aminopenicillins, cephalosporins or macrolides are prescribed.
It is very important to follow all doctor’s recommendations for taking antibiotics. And despite the fact that the child’s condition may improve after taking the first pill, it is important to drink the course dose of drugs strictly. Because due to the irrational use of antibacterial agents, the resistance of microorganisms to drugs increases.
The main principle of treatment for streptococcal infection is antibacterial therapy.
Local treatment usually includes the use of antiseptic and analgesic aerosols (Tantum Verde, Hexoral, Miramistin). It is also recommended to gargle, if the patient’s age allows, with antiseptic solutions (Chlorhexidine) or herbal preparations (Chamomile, Sage).
Physiotherapy
Physiotherapy during the acute period is contraindicated. It is not prescribed because physiotherapy creates favorable conditions for the proliferation of bacteria due to warming up. Physiotherapy can be prescribed to patients with chronic tonsillitis in remission.
Surgery
Surgical treatment consists of complete removal of the tonsils. It is indicated for chronic tonsillitis, with frequent relapses and ineffectiveness of the prescribed treatment. The operation is also performed for persons with constant development of complications (peritonsillar, retropharyngeal abscesses).
Traditional medicine against streptococcus
It is impossible to influence streptococcus in the throat using traditional methods. The only method is antibacterial therapy.
Do not self-medicate.
Mode
A strep throat infection does not require hospitalization. Children with tonsillitis are treated at home. Indications for hospitalization are severe infection and complications.
Restrictions for children during illness and recovery
For the entire febrile period, children are prescribed bed rest. During the period of convalescence, children are advised not to engage in active sports, and are also exempted from physical education at school for a month.
Treatment of streptococcal pneumonia
As mentioned above, streptococcal pneumonia is caused only by bacteria of the genus Streptococcus.
Streptococcus is a gram-positive aerobic bacillus. The most common cause of the disease is alpha-hemolytic Streptococcus pneumoniae. Less commonly, beta-hemolytic Streptococcus pyogenes may be a possible causative agent.
In the rarest cases, inflammation can be caused by all other strains of streptococcus.
Normally, Streptococcus agalactiae can be found in the human throat. Its presence is normal if the pathogen is less than 10 to the 5th - 10 to the 6th power. If the amount increases above 10 to 5 - 10 to 6 degrees, it can become pathogenic and also lead to streptococcal pneumonia.
Also, normally, opportunistic species of streptococcus can be identified in humans, such as Streptococcus acidominimus, Streptococcus viridans and many others. In the case of all types of opportunistic flora, a change in its status to “pathogenic” is considered when the number of microorganisms exceeds 10 to the 6th power.
Negative factors play an important role: frequent illness, uncontrolled use of antibiotics or immunosuppressants, congenital and acquired immunodeficiencies, chronic diseases, poor social and living conditions, unfavorable working conditions - all this significantly weakens the body and can lead to the development of pneumonia.
With timely and correct treatment, recovery occurs in 6-10 days. It is very important that the patient remains in bed during treatment.
After identifying the pathogen, the patient is prescribed specific antibiotics. To correct intoxication, a loading dose of diuretins is used and patients are given large amounts of water and tea.
To correct dysbiosis, the patient is prescribed eubiotics. The use of multivitamin complexes also has a positive effect for treatment.
In case of development of exudative pleurisy, drainage of the pleural cavity is indicated, followed by washing it with antiseptics or antibiotics. With adequate and timely treatment in children and adults, the chance of complications is significantly reduced, which will most likely save a person’s life.
Treatment with medications
Treatment of the disease includes a whole range of measures. The diagram looks like this:
- Antibiotic therapy. First of all, penicillin drugs are prescribed: Ampicillin, Azlocillin, Amoxicillin, etc. If the patient is allergic to these drugs, then antibacterial drugs with the active substance vancomycin can be prescribed: Vancomycin, Vancorus, Vero-Vancomycin, etc. Dosage, duration of administration, and, if necessary, replacement with similar drugs is determined and prescribed only by the attending physician.
- Diuretics (diuretics). To remove waste products of microbes, that is, eliminate signs of intoxication, a high dose of diuretics is prescribed: Furosemide, Hypothiazide, Lasix. It is possible to use folk diuretics: decoctions of birch leaves, bearberry, lingonberry, strawberry, tansy, tea from rose hips, fruit drink from taiga berries. In addition, you should drink at least 2 liters of water per day.
- Eubiotic drugs. To eliminate dysbiosis and normalize intestinal microflora caused by pathogenic microorganisms and antibiotics, products consisting of live or dried beneficial lacto- or bifidobacteria are prescribed. This group includes the following drugs: Linex, Bifidumbacterin, Normobakt, Lacidofil.
- Vitamin therapy. Vitamins take an active part in the oxidative, reductive and metabolic processes of the body, therefore they are prescribed in the complex treatment of any type of pneumonia. However, not all vitamin elements are combined with antibiotics. Some cannot be taken at high temperatures, so only a specialist should prescribe the appropriate vitamin complex or individual vitamins.
- In the presence of exudative pleurisy, thoracostomy is prescribed - drainage of the pleural cavity. Intracavitary tubes are inserted into the organ, through which excess fluid is released, then the cavity is treated with antiseptics or antibiotics.
During the treatment process, it is important to comply with bed rest and doctor's instructions.
If therapy was started on time, then complete recovery occurs in a week and a half.
How are microorganisms transmitted?
Streptococcus occurs in almost 100% of the adult population. The prevalence of the agent is determined by the number 98-99%. Where do these numbers come from?
It's all about the virulence (ability to infect) of this microorganism. The infection can affect a potential host in several ways. Each of them occurs in everyday life.
- Airborne path. Pathogenic structures are released into the environment with particles of mucous secretion (saliva, mucus) when sneezing, coughing, or even just breathing. The airborne route is the main transmission route for microorganisms. Considering how many people are infected, it is not difficult to calculate the likelihood of encountering a carrier of streptococcus. It is not recommended to be in the same closed room with such people.
- Contact and household path. These are any contacts with people of a non-sexual nature: handshakes, kisses (especially since streptococcus lives mainly on mucous membranes). Also interaction with household items of sick people. Transmission of agents is possible through toys, hygiene items, medical instruments (this also occurs if doctors do not follow the rules of hygienic treatment). Most often, children encounter streptococcus right at birth, becoming infected from infected medical personnel in maternity hospitals.
- Dust path. Slightly less common. Penetration of pathogenic agents is possible with particles of house dust, exfoliated skin, and pieces of fabric. Workers of textile enterprises and offices are especially at risk.
- Oral-genital route. Fans of oral-genital contact are in danger. Streptococcus lives on the mucous membranes, including the genitals. There is only one piece of advice - to protect yourself carefully and not take risks.
- Perinatal path. Streptococcal flora easily overcomes the placental barrier and enters the child’s body. This happens in the womb of an infected mother. Therefore, already during pregnancy planning, it is recommended to undergo a course of treatment. It is impossible to cure streptococcus entirely, but it is quite possible to suppress it and transfer it to a latent, “sleeping” phase.
- Descending path. From mother to child when the fetus passes through an infected birth canal. Through blood transfusion.
There is a high probability of transporting a pathogenic organism in the presence of a nutritional factor (for example, if hygiene rules are not followed and food is eaten with unwashed hands). Each case needs to be examined separately.
Symptoms and clinical picture
The disease begins acutely with a rise in body temperature, severe chills, myalgia, arthralgia, shortness of breath, cough, hemoptysis, loss of performance, severe fatigue, and pain in the side. Intoxication of the body is rapidly developing.
In severe cases, the patient develops symptoms of respiratory or cardiovascular failure, which can lead to serious consequences. In this case, acrocyanosis, memory loss, tachycardia, arrhythmias, and asthma attacks are noted.
With the development of exudative pleurisy, the patient complains of pain in the side. In this case, there is a displacement of the mediastinal organs to the side. Exudative pleurisy develops in children very often - in 1/3 of cases.
In some cases, the pathological process can lead to chronic abscesses in the lungs.
Also, streptococcal pneumonia can lead to the development of purulent pericarditis, glomerulonephritis, and sepsis.
- Percussion notes dullness of percussion sound in the affected area. In case of development of exudative pleurisy, dullness is heard throughout the entire fluid level.
- Auscultatory data make it possible to accurately listen to the area with decreased vesicular breathing, wheezing and whistling.
- One of the most informative methods in diagnosing pneumonia is radiography. The radiograph shows areas of darkening of the pulmonary pattern; in the case of pleurisy, the fluid level is increased.
- A general blood test will allow you to suspect the nature of the pathogen. In the case of streptococcal pneumonia, neutrophilic leukocytosis with a regenerative shift of the leukocyte formula to the left, increased ESR, thrombocytopenia, and in rare cases anemia are noted.
- An important part of making a diagnosis is bacterial analysis. With the help of bacterial analysis, you can accurately identify the etiological agent and at the same time test it for sensitivity to antibiotics. This is the only way to choose the most suitable drug. They also take into account the number of opportunistic microorganisms, which are normally no more than 10 to 5 - 10 to 6 degrees.
Differential diagnosis should be carried out with other types of pneumonia, including atypical. But most often streptococcal pneumonia is confused with staphylococcal pneumonia. This is a gross mistake, because with staphylococcal pneumonia, characteristic sputum with a rusty tint appears, whereas with streptococcal pneumonia it is not present. Moreover, streptococcus is characterized by the development of pleural empyema, which is not observed with staphylococcal etiology of the disease.
Diagnosis of the pathological process
The rapid onset of the disease requires mandatory consultation with a doctor. A specialist will be able to stop the inflammatory process in the early stages. A correct diagnosis increases the chances of successful treatment. It is preliminarily set if several prerequisites are present. These include:
- previous illnesses, in particular influenza and whooping cough;
- acute symptoms;
- the presence of exudative pleurisy;
- detection of abnormalities in blood tests.
Primary diagnosis involves collecting an accurate and reliable history. Then a sound study is carried out in the suspected affected area. Auscultatory listening allows you to identify areas of difficulty breathing and the presence of wheezing. Radiography shows particular effectiveness. A complete picture of what is happening is complemented by a blood test. Thanks to it, the level of leukocytes, changes in ESR and the presence of thrombocytopenia are monitored.
Microbiological studies can make an accurate diagnosis and identify the presence of pneumonia. Bacterial analysis is aimed at identifying the main causative agent of the disease and its quantitative content in the body.
To make an accurate diagnosis, differential methods are used, including ultrasound, CT and MRI. Everything is supplemented by biological and biochemical research.
What symptoms does the patient feel?
In the vast majority of cases, we are talking about inflammation of the tonsils - tonsillitis, which is also called tonsillitis. The symptom complex is very variable.
The clinical picture includes the following manifestations:
- Intense pain syndrome. The discomfort has a burning, aching, pulling character. The larynx is very sore, there is a desire to mechanically influence the affected area. The pain intensifies when eating or drinking cold water. The intensity of the sensation decreases slightly when drinking warm drinks.
- Breathing disorders. It becomes harder to breathe. Shortness of breath develops (increased number of respiratory movements per minute). This is observed due to swelling of the throat. It becomes more difficult for air to pass through. This is an extremely dangerous symptom that should be treated immediately by a doctor. Possible suffocation, asphyxia and death of the patient. This scenario is especially likely in children.
- Separation of purulent exudate from the throat. The pus may be liquid: yellowish or greenish exudate with a strong, unpleasant odor. The formation of special putrefactive clots, so-called plugs, is possible. These are also yellowish lumps with a pungent odor. The separation of this kind of exudate is a direct indication of the presence of pyogenic flora, streptococci or staphylococci in the throat.
- Formation of specific whitish spots in the throat. The patient himself can detect them by visually assessing the pharynx. The spots are located in a random order and look like plaque.
- Cough. Occurs due to severe sore throat.
- Increase in body temperature to febrile levels and above.
- Signs of general intoxication of the body: headaches, nausea, vomiting, weakness, weakness and drowsiness.
Such manifestations quickly subside, which is not typical for staphylococcal lesions. The symptoms, however, remain, although in a milder form. This is the latent or chronic phase of streptococcal throat infection.
Pharyngitis is additionally manifested by a severe cough and voice disturbances. However, such a disease is relatively rare (in approximately 3-5% of clinical cases, streptococcus makes itself felt in this way).
How is the examination carried out?
Otolaryngology specialists (ENT doctors) diagnose streptococcal throat infections.
At the initial appointment, it is necessary to collect an anamnesis (identify what the patient was or is ill with), determine the nature of the complaints, and record the data presented. This will help in the future. The diagnosis is verified (confirmed) using laboratory tests.
Their list is as follows:
- Serological analysis. There are several methods. Makes it possible to distinguish some microorganisms from others.
- Taking a smear from the throat with further inoculation of the biomaterial on nutrient media (bacteriological examination). Helps to build the correct therapeutic model and determine the sensitivity of streptococcus to antibiotics.
- General blood analysis. Gives a picture of inflammation with a shift in the leukocyte formula towards an increase, accelerated erythrocyte sedimentation. Also, as already mentioned, an increase in hemoglobin concentration indirectly indicates a streptococcal infection.
In addition, a visual assessment of the throat is performed. Classic visual signs of tonsillitis are detected: hyperemia of the throat, loose tissue structure, whitish or yellowish plaque, etc.
In the system, these examinations are quite sufficient to make a diagnosis and select the correct treatment.
Normal levels of streptococcus are 10 to 3 - 10 to 5 CFU/ml. This amount lives on the mucous membranes of the nasopharynx of most people.
All indicators are above 10 to 6 degrees CFU/ml. are considered pathological. Treatment is required only when the bacterium becomes the cause of the disease. If the norm is exceeded and there are no symptoms of inflammation, no therapy is required.
Local and systemic antibiotics
Antibiotics are widely used to treat streptococci in the throat. They are used in the form of solutions and tablets, respectively. Antibacterial agents of several groups can be prescribed at once (but not simultaneously):
- Penicillins. Oddly enough, sometimes streptococcus is sensitive to the penicillin series, which cannot be said about Staphylococcus aureus.
- Macrolides. Azithromycin or Erythromycin.
- Fluoroquinolones. Used in extreme cases.
- Cephalosporins. Prescribed in case of intolerance to penicillins, as well as in case of microorganisms insensitivity to them.
In some cases, the use of tetracyclines is justified. But they give a lot of side effects, so such drugs are prescribed with caution.
Preference is given to local antibiotics (such as Hexoral, Sebidin, Rinza Lorcept) since they produce a targeted effect and directly contact the streptococcus in the throat.
If the lesion is generalized (extensive), systemic antibacterial drugs (in the form of tablets) cannot be avoided. In complicated forms, medications are used in the form of intramuscular injections. The total duration of treatment is from 7 to 14 days.
Treatment
Comprehensive treatment is prescribed, including:
- bed rest;
- gentle (mechanically and thermally) diet;
- drinking plenty of water;
- medicinal effects on streptococcus (antibiotic therapy);
- symptomatic treatment.
Streptococcus pyogenes retained sensitivity only to a single class of antibiotics - beta-lactam antibiotics, which include penicillins, cephalosporins and carbapenems. To macrolides (Azithromycin, Clarithromycin), resistance above 30% is observed in some regions.
A 10-day course of penicillin is optimal for tonsillopharyngitis. But not all patients may adhere to such a course.
Therefore, (one of them) can be used:
- Amoxiclav – 6 days;
- Amoxicillin – 5 days;
- cephalosporins (Cefalexin, Cefaclor) – 5 days;
- Azithromycin – 5 days.
If you are allergic to penicillins, Co-trimoxazole may be prescribed. If sensitivity to it is confirmed, streptococcal bacteriophage can be used. To prevent dysbacteriosis, Acepol, Bifiform, Linex are used. Therapy includes antihistamines Diazolin, Claritin, Zodak, etc.
Immunomodulators, despite advertising their effectiveness, should not be used without an immunological study and consultation with an immunologist, so as not to increase the risk of developing autoimmune aggression in the body.
Local treatment for sore throat includes gargling with antiseptic solutions and herbal decoctions. Bioparox is not used in many countries due to possible complications. You can use Hexoral, Aqualor. Miramistin.
Possible complications
Pyogenic flora gives many complications. Among them:
- meningitis. Inflammation of the brain;
- glomerulonephritis;
- otitis;
- pharyngitis;
- arthritis;
- pneumonia;
- bronchitis.
The list can be supplemented with another 20-30 items. Streptococcus can cause infection in any system of the body. In addition, the process may become chronic.
Streptococcus is a dangerous neighbor, which, however, occurs in almost everyone. He needs to be kept in check. Otherwise, the consequences may be unpredictable. Treatment of streptococcus in the throat is the prerogative of the doctor. Self-medication is unacceptable.
source
If treatment with antibacterial agents is not carried out in a timely manner, serious consequences may develop. The spread of streptococcus can cause respiratory failure, oxygen starvation, and heart failure. The development of pathologies cannot be excluded:
- acute glomerulonephritis (autoimmune kidney disease);
- lung abscess (purulent tissue damage);
- chronic lymphadenitis (inflammation of the lymph nodes).
The infectious disease must be cured completely. Otherwise, the infection, spreading through the bloodstream, can cause the following complications:
- pleural empyema - accumulation of pus in it;
- soft tissue necrosis;
- damage to the membranes of the heart - pericarditis, myocarditis, inflammation of the valves - endocarditis;
- sepsis – blood poisoning;
- meningitis - inflammation of the meninges;
- anemia;
- peritonitis;
- If the disease is severe, death may occur.
Prevention
A specific vaccine against streptococcal infection has not yet been registered. One drug, Streptavax, is in clinical trials.
Therefore, for prevention, general recommendations are used to strengthen the body’s resistance:
- maintaining personal hygiene;
- wet cleaning of premises and ventilation;
- balanced diet;
- treatment of foci of infection;
- hardening;
- an active way of life without bad habits.
Streptococcus is widely distributed in the external environment. It can coexist with humans. But with a decrease in immunity, hemolytic streptococcus (the most dangerous of all types of streptococcus) can cause a number of diseases that require treatment with antibiotics. With proper treatment, the prognosis is favorable. If left untreated, serious complications develop, including autoimmune diseases.
Impact of pneumococcus on the body
The bacteria Streptococcus pneumoniae can exist without access to air. Once in the body, they penetrate the blood and spread throughout the body. The affected area is often the respiratory tract. The following pathologies often develop:
- Damage to the lower respiratory tract provokes bronchitis and pneumonia.
- If staphylococcus affects the nasopharynx, the lymph nodes atrophy, laryngitis, pharyngitis, tonsillitis, and sore throat occur.
- When the mucous membranes of the nose become inflamed, rhinitis and sinusitis are diagnosed.
When the virus enters the pleural cavity, it causes exudation (fluid accumulation) and the development of pleurisy. The spread of microorganisms can lead to necrosis of the mucous membranes of the bronchi, trachea, and lungs. Streptococcal infection causes the following pathologies:
- otitis – inflammation of the middle ear;
- osteomyelitis – damage to the bone marrow, bones;
- laryngitis - an inflammatory process of the mucous membranes of the larynx;
- pharyngitis - a disease of the pharynx;
- bronchitis – damage to the mucous membranes of the bronchi;
- sinusitis - suppuration in the sinuses.
Causes and mechanisms of disease development
There are several ways for the pathogen to enter the lungs.
Most often it penetrates mechanically through the respiratory tract. This happens with descending inflammation, or with direct exposure of the pathogen from the external environment. In some cases, the pathogen enters the lung tissue through infected blood. This happens with severe bacterial inflammation in other organs and systems, with the development of sepsis.
The rarest variant of pathogen entry is lymphogenous. In this case, the pathogen enters the lungs with the help of lymph from other organs. When the pathogen hits the mucous membrane, it penetrates through it and the other layers, and then ends up directly in the lungs. There it begins to develop rapidly under optimal environmental conditions.
Very often, with the rapid growth of the pathological process, the pathogen enters the pleural cavity, causing exudative pleurisy.