Is pneumonia viral and what is it?
Pneumonia is an infectious disease of a viral or bacterial nature, characterized by inflammation of the lung tissue and resulting from the penetration of various pathogenic organisms into the respiratory tract.
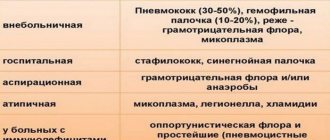
What viral pneumonia is becomes clear from the classification by etiological factor. Depending on the causative agent, pneumonia is classified into:
- bacterial;
- mycoplasma;
- leginella;
- chlamydia;
- viral;
- fungal.
Viral pneumonia occurs in approximately 50% of all cases of pulmonary inflammation. In children, the majority of the disease is caused by viruses – about 90% of the total. Among adults, viral pneumonia is less common. Mostly elderly people over 65 years of age are affected.
Typically, viral pneumonia is caused by influenza A and B viruses, in children it can be respiratory syncytial virus and the causative agents of chickenpox and measles. Less commonly, pneumonia is caused by parainfluenza viruses, adeno and coronaviruses.
Viral pneumonia can be primary or secondary, as a consequence of influenza and other viral infections.
What causes pneumonia?
The causative agent of pneumonia can be not only a virus. Bacteria and fungi are also causes. In particular cases, paracancrosis pneumonia develops, which is inflammation of the lungs around a malignant neoplasm. Most often, pneumonia is caused by infection.
Note! It is interesting that some pathogenic microorganisms that can cause pneumonia are constantly present in the human body. If your immune system is functioning properly, your lung tissue will not become infected. The situation for people with immunodeficiency syndrome is much more complicated.
Often the cause of pneumonia is self-administration of medications aimed at reducing fever. It helps pathogenic microorganisms penetrate further through the respiratory tract.
How is it transmitted?
There are two main routes of transmission of viral pneumonia:
- airborne;
- contact-household.
The main way of spreading a viral infection is through airborne droplets.
When a carrier coughs, sneezes, or normally talks, they spread the infection into the air.
It is easiest to become infected indoors with large crowds of people.
Viral pneumonia is also transmitted through household contact. All objects with which the patient has been in contact become a source of the virus. After contact with such things, a healthy person can become infected with his hands or touch his face.
Causes of viral pneumonia
There are a number of contributing factors for the development of pneumonia, in particular viral etiology.
Mostly children's age. Viral pneumonia in children occurs quite often due to the imperfection of the body's respiratory and immune systems. A child’s body is more susceptible to a viral attack than a bacterial infection. In children's groups (kindergartens, schools, clubs), viral infections spread mainly because they are more contagious.
Elderly age. Over time, any mechanism wears out. The human body is no exception. With age, the condition of the respiratory system and immunity deteriorates, which is undoubtedly a risk factor.
Reduced immunity. Naturally, with a pathological decrease in immunity due to HIV infection, or when taking immunosuppressants, the human body becomes more vulnerable to any infections. Damage to the lungs by viruses will be no exception.
Smoking. It has been said more than once about the dangers of smoking for the lungs. In this case, this addiction will contribute to the development of the disease and complicate its treatment.
Alcohol consumption. When drinking alcohol, the therapeutic effect of antiviral drugs sharply decreases, and the side effects on the body worsen. In a state of alcoholic intoxication, a person has little or no control over his actions, which can lead to a worsening of the condition.
Addiction. There are probably no diseases in which drug addiction is not a risk factor. All the troubles come from the fact that a drug addict does not control himself while intoxicated. Also an important factor is the harmful effect of narcotic drugs on all systems and organs, including the immune and respiratory.
Hypothermia. A contributing factor in pneumonia of any cause is hypothermia. As the temperature of the body and body tissues decreases, the ability to “repel” viruses is significantly reduced, making it much easier to get sick.
Stress. It has long been no secret that when under stress, the body becomes more vulnerable to any disease. Physical stress has a particularly detrimental effect: overwork, lack of sleep.
Presence of chronic lung diseases. Naturally, with chronic diseases such as bronchitis, the possibility of contracting pneumonia increases many times over. This occurs due to the fact that the lung tissue loses a significant proportion of local immunity.
What are the symptoms of viral pneumonia in adults and adolescents?
The symptoms of the disease at the beginning cannot be distinguished from acute respiratory diseases. At the first stage, viral pneumonia is accompanied by:
- high temperature;
- chills;
- aches in joints and muscles;
- sore throat;
- dry cough;
- shortness of breath and wheezing;
- general weakness;
- sharp pain behind the sternum.
At the second stage of the disease, a dry cough gives way to a wet cough with yellowish to rust-colored sputum. The temperature continues to remain high for 10-15 days.
Symptoms in adolescents do not differ from the manifestations of the disease in adult patients. Among schoolchildren and older youth, viral pneumonia is extremely rare.
Complications
The danger of viral pneumonia lies in its unpredictability. The following complications may occur:
- significantly increased body temperature, fever;
- sepsis;
- inflammation of the heart muscle;
- meningitis;
- oxygen deficiency;
- toxic-infectious shock;
- swelling and abscess of the lungs;
- otitis.
Attention! If pus appears in the coughed up sputum, it means that a secondary bacterial infection has occurred.
Respiratory failure often occurs. The person begins to breathe intensely, arterial and partial pressures increase, and then sharply decrease, which can result in coma.
Sometimes toxic shock occurs. The cardiovascular system malfunctions. Severe pain occurs throughout the body and in the head. Consciousness becomes confused. Such complications are usually observed in young children.
Some patients experience kidney and liver failure. In this case, immediate hospitalization is indicated. The patient must be constantly monitored by medical professionals. It is important to constantly monitor breathing, blood pressure and other vital signs.
How is it different from the bacterial form?
The difference between the viral and bacterial nature of the disease is manifested not only by the type of pathogen.
- A viral infection has a short incubation period of no more than 5 days, while bacterial pneumonia can remain asymptomatic for up to two weeks.
- A sharp increase in temperature to 39-40 degrees – this is how viral pneumonia occurs. With the bacterial form, the temperature usually stays no higher than 38 degrees Celsius.
- With viral inflammation, signs of general malaise are more pronounced, while with bacterial inflammation, specific symptoms such as cough and shortness of breath are more pronounced.
- When listening to a patient with a bacterial form of pneumonia, frequent moist rales are observed. With a viral infection, they are rarer and drier.
- On an x-ray, bacterial pneumonia, unlike viral pneumonia, is characterized by a general darkening of the lungs and the presence of fluid behind the pleura.
- Viral pneumonia is most often bilateral.
By paying attention to all these points, you can determine whether the disease is of bacterial or viral origin.
Clinical picture: how do the child’s symptoms differ?
Pneumonia is a disease that is more common in certain age groups. Thus, children under 3 years old will not be able to clearly tell you about poor health, but they experience pneumonia as much as 2-3 times more often than older children. Pneumonia in a small child can be recognized by the following signs:
- he cries for no reason and shows irritability;
- half of his chest does not rise when breathing (with unilateral pneumonia);
- the child breathes noticeably faster;
- the tips of the fingers are excited (especially during feeding or crying);
- the child expresses lethargy, eats less and appears sleepy.
Children who have reached school age show the same symptoms of pneumonia that are observed in all adults: weakness, increased sweating, lethargy, lethargy and fever.
Note! Seek medical help immediately if you notice similar symptoms in your child. In 2020, pneumonia caused 15% of child deaths.
How to determine: blood test and other tests
The diagnosis of viral pneumonia is made after an external examination of the patient, auscultation, radiographic examination and laboratory tests of blood, urine and sputum.
- On external examination, cyanosis and cooling of the extremities with a general high temperature, rapid breathing and redness of the face are observed.
- Auscultation - listening to the respiratory organs - reveals difficulty in breathing and the presence of wheezing.
- A chest x-ray shows darkening of the space around the bronchi, enlargement of the interlobar septa and peribronchial nodes, as well as clear expression of the vessels at the roots of the lungs.
- A general blood test for viral pneumonia reveals an increase in the number of leukocytes and an increase in ESR.
- In general urine analysis, a decrease in volume is observed with a simultaneous increase in the specific gravity of urine. Protein and red blood cells are present in trace amounts.
- A general analysis of sputum reveals an accumulation of leukocytes and rusty red blood cells. In mixed forms of pneumonia, bacterial associations can be determined.
- Sputum culture for flora and sensitivity to antibiotics is performed in the hospital if there is doubt about the diagnosis and the need to adjust treatment.
Diagnostics
Timely diagnosed viral pneumonia in children and adults is easier to treat. Severe consequences in this case occur extremely rarely. To make an accurate diagnosis, the doctor studies the epidemiological situation and the person’s medical history. The patient undergoes the following examinations:
- laboratory sampling;
- examination of sputum, tracheal aspirate or bronchial lavage using the fluorescent antibody method;
- X-rays of light.
There are two stages of the disease. Primary is determined by clinical signs and on the basis of laboratory information, secondary (viral pneumonia) is detected as a complication of a cold infection against the background of the immunity of the causative virus to the therapy.
Treatment
How to treat viral pneumonia is decided by the doctor after diagnosis. First of all, the patient is prescribed bed rest and plenty of fluids - up to 3 liters of fluid per day . Patients of younger preschool and older age are subject to hospitalization, the rest are usually treated at home.
Therapy is carried out in two directions:
- etiological;
- symptomatic.
Etiological treatment is the fight against the cause of the disease, that is, a specific virus. The choice of drug depends on its type.
- For pneumonia caused by the influenza virus, the drugs Remantadine, Tamiflu or Relenza should be used.
- Measles and chickenpox viruses are treated with Acyclovir or Isoprinosine.
- Cytomegalovirus can be treated with Ganciclovir.
- For respiratory syncytial pneumonia, Ribavirin is prescribed.
- If there is a suspicion of a bacterial infection, the doctor prescribes macrolide antibiotics (Rovamycin, Rulid) or benzylpenicillin (Ampicillin, Flemoxin, Amoxiclav)
Symptomatic treatment depends on the severity of the various manifestations of the disease.
- Fever, aches in the joints and muscles are well relieved by antipyretic and painkillers Ibuprofen, Paracetamol in tablets or syrups for children, as well as complex drugs - Pentalgin, Fervex, Theraflu in tablets or powders.
- Expectorants Ambroxol, Acetylcholine, herbal preparations Gerbion, Linkas, Doctor Mom in the form of tablets, syrups, and solutions for inhalation will help relieve coughs and facilitate the discharge of sputum.
- For shortness of breath, oxygen therapy is prescribed - treatment with oxygen.
- In case of vascular insufficiency, a solution of cordiamine or caffeine is administered intramuscularly.
- Vitamins are prescribed both for prevention and during treatment.
- During the recovery period, the patient is required to undergo physiotherapeutic treatment.
Viral pneumonia: symptoms, treatment and prevention of the disease
Depending on the etiological agent, viral pneumonia can occur with varying degrees of severity, complications and outcomes. Inflammation of the lungs usually occurs from the first days of ARVI.
Thus, damage to the respiratory tract is a frequent companion to adenoviral infection. The onset of pneumonia in most cases is acute, with high fever (38-39°), cough, severe pharyngitis, conjunctivitis, rhinitis, and painful lymphadenopathy. The temperature with adenoviral pneumonia lasts a long time (up to 10-15 days), and is characterized by large daily fluctuations. Characterized by frequent, short cough, shortness of breath, acrocyanosis, variable moist rales in the lungs. In general, adenoviral pneumonia is distinguished by long-term persistence of clinical and radiological changes, a tendency to recurrent course and complications (pleurisy, otitis media).
The incidence of viral pneumonia against the background of influenza increases significantly during periods of epidemics of respiratory infection. In this case, against the background of typical symptoms of ARVI (fever, severe weakness, myalgia, catarrh of the upper respiratory tract), noticeable shortness of breath, diffuse cyanosis, cough with rust-colored sputum, wheezing in the lungs, and chest pain when inhaling appear. In children, general toxicosis and anxiety are expressed; vomiting, convulsions, and meningeal signs may occur. Influenza pneumonia is usually bilateral in nature, as evidenced by auscultatory findings and an x-ray picture (focal opacities in both lungs). Mild cases of viral pneumonia caused by the influenza virus are characterized by moderate symptoms and end with recovery.
Parainfluenza pneumonia most often affects newborns and young children. It is of a small-focal (less often confluent) nature and occurs against the background of catarrhal phenomena. Respiratory disorders and intoxication syndrome are moderate, body temperature usually does not exceed subfebrile values. Severe forms of viral pneumonia with parainfluenza in children occur with severe hyperthermia, convulsions, anorexia, diarrhea, and hemorrhagic syndrome.
A feature of respiratory syncytial pneumonia is the development of severe obstructive bronchiolitis. Damage to the lower parts of the respiratory tract is marked by an increase in body temperature to 38–39°C and a deterioration in general condition. Due to spasm and blockage of small bronchi with mucus and desquamated epithelium, breathing becomes sharply difficult and rapid, and cyanosis of the nasolabial and periorbital area develops. The cough is frequent, wet, but due to the increased viscosity of sputum, it is unproductive. With this type of viral pneumonia, attention is drawn to the discrepancy between intoxication (moderately expressed) and the degree of respiratory failure (extremely pronounced).
Enteroviral pneumonia, caused by the Coxsackie and ECHO viruses, occurs with scant physical and radiological data. In the clinical picture, concomitant meningeal, intestinal, and cardiovascular disorders come to the fore, making diagnosis difficult.
A significant proportion of fatal pneumonias are caused not by concomitant bacterial infections, but by direct invasion and multiplication of the virus in the lungs.
The risk group for primary influenza pneumonia includes patients with immunodeficiencies, intercurrent cardiovascular diseases, children and pregnant women.
Manifestations of pathology at the initial stage are typical for influenza, but within 12–36 hours there is an increase in shortness of breath, which in most cases is accompanied by a cough streaked with blood and a scanty amount of sputum. Symptoms of viral pneumonia, such as pleural pain and massive hemoptysis, are less common.
At the time of hospitalization of an adult or child, respiratory failure, tachycardia, tachypnea, and cyanosis are usually pronounced.
As the disease progresses, the auscultatory pattern changes. At the initial stages, crepitus is heard, inspiratory wheezing and sometimes dry wheezing are observed in the lower parts of the lungs. Subsequently, breathing becomes weakened, wheezing spreads to all parts of the lungs.
When the disease reaches the terminal stage, breathing and wheezing are practically not heard, while tachypnea is significant. Sometimes agitation and dyspnea are so severe that the patient cannot tolerate an oxygen mask.
In some cases, the course of the pathology may be accompanied by complications such as acute renal failure and disseminated intravascular coagulation syndrome.
With viral-bacterial pneumonia, the interval between the appearance of the first respiratory symptoms and signs of involvement of the lung parenchyma in the inflammatory process is longer and can be up to 4 days. At this time, even a slight improvement in the patient's condition is possible.
Most often, this form of pathology is characterized by a productive cough with bloody or purulent sputum, severe chills and pleural pain.
At the time of hospitalization, signs of severe respiratory failure are usually clearly manifested: tachypnea, severe dyspnea, cyanosis. When conducting a physical examination, a varied picture is revealed.
In most cases, there are signs of local consolidation involving a lobe or several lobes of the lungs. The clinical picture is complemented by signs of massive involvement of the lung parenchyma in inflammation, which manifests itself in the form of diffuse dry inspiratory wheezing wheezing and wheezing inspiratory and expiratory wheezing. Sometimes only dry whistling and buzzing rales are observed in the absence of signs of consolidation.
The radiographic picture of the lungs is diffuse infiltrative opacities, similar to those in primary influenza pneumonia, or a combination of diffuse infiltrates with foci of focal consolidation.
Viral pneumonia is an acute, pronounced process of inflammation of the lower lung tissue caused by infection. The main causative agents of pneumonia are respiratory viruses.
The fundamental respiratory group of pathogens that provoke the occurrence and development of the disease include:
- viruses of groups A and B;
- parainfluenza;
- adeno- and interoviruses;
- herpes 1, group 3;
- respiratory syncytial.
Concomitant diseases that provoke the occurrence of viral pneumonia:
- measles;
- chicken pox;
- Epstein-Barr virus infection;
- cytomegalovirus.
Infection occurs by airborne droplets - through the mouth, nose, inhalation or exhalation, or through contact with an active carrier. Once in the body, the pathogen penetrates the cells of the respiratory tract, pulmonary alveoli and settles on the epithelial layer.
Paralyzing the supply of oxygen, the microbe multiplies, thickening the round cell peribronchial tissue and infiltrating the interalveolar septa.
This leads to disruption of the functions of the respiratory-pulmonary tract, accumulation of fluid in the alveoli is formed, and a failure of intercellular oxygen exchange occurs.
The risk group for pneumonia includes preschool children, adolescents, patients with an immunodeficiency state, concomitant infectious diseases (for example, HIV), as well as elderly people with a history of chronic pathologies of the respiratory system. Infection is also facilitated by unfavorable environmental conditions, habitat and abuse of bad habits. Pneumonia of bacterial origin or mixed type (viral-bacterial) is most often recorded in adult patients.
Epidemiological outbreaks of ARVI and the off-season period are the most favorable conditions for the development of the disease.
The incubation period from the moment the pathogen enters the body until the first symptoms appear depends on the type of virus and the host’s immune defense.
Thus, latent (passive) carriage for influenza is from 1 to 4 days, for adenovirus – up to 14 days, for parainfluenza infection – no more than 6 days.
The incubation period of cytomegalovirus infection ranges from 3 days to 2 months after infection.
- Type of causative virus.
- Patient's age.
- The patient's health status (history).
- Individual resistance of the body.
Most often, initial signs of infection appear within a week. An alarming indicator of the presence of a pathogen in the body is a slight increase in body temperature.
How to protect yourself
An important factor in the prevention of viral pneumonia is vaccination. It is necessary to be vaccinated every fall before outbreaks of various seasonal infections begin.
If an adult has never had chickenpox, then he should be vaccinated against chickenpox, since this virus is likely to cause pneumonia in an adult.
To protect yourself from viral pneumonia during an epidemic of influenza and other viral infections, you must follow simple rules:
- Wash your hands with soap after each visit to public places or direct contact with other people.
- Ventilate the room regularly.
- Carry out wet cleaning daily using antiseptic agents.
- If possible, install humidifiers in the bedroom. Dry mucous membranes are most susceptible to infectious agents.
- No smoking! Smoking is one of the main factors in the occurrence of respiratory diseases.
- Regularly engage in physical exercise and condition the body.
- Rinse your nose and throat daily with isotonic saline solution.
- Take vitamins and immunostimulants as a preventive course.
- Eliminate spicy, fatty foods, alcohol, strong tea and coffee from your diet.
Prevention
A number of preventive measures help prevent viral pneumonia. Thus, during periods of increased risk of morbidity (autumn-winter period), vitamin therapy is recommended. To boost immunity, it makes sense to take immunomodulators. A physical method of prevention will be hardening. A healthy lifestyle is the primary prevention. Viral pneumonia does not spread outdoors, so spending more time outside is beneficial. Eliminating predisposing factors as much as possible will help reduce the risk of getting sick. When in contact with sick people, you should use a medical mask. It must be changed every 2 hours.
If there is a risk of infection, you should immediately start taking antiviral drugs for prophylactic purposes.
The likelihood of contracting viral pneumonia is quite high only if there are predisposing factors. It is necessary to especially carefully monitor and care for children and the elderly. If there are people around with bad habits, it is necessary to explain the importance of combating them. The key to health is proper nutrition and a healthy lifestyle. Sports will help strengthen the respiratory system and reduce the risk of getting sick. Self-medication of any disease, including viral pneumonia, should be avoided. Eating enough vitamins and microelements will help keep the body in good shape. And even if infection occurs, the body will be able to cope with the disease faster and easier.
Prevention measures for older people
For older people, ways to protect themselves from the virus are the same as for other people. The main thing is to remember that people over 65 years of age are the most susceptible to various infections.
- During an epidemic, they should not visit places with large crowds of people, since the immune system of these patients is weakened, and there are also concomitant diseases (bronchial asthma, diabetes mellitus, cardiovascular disorders, liver and kidney diseases).
- Persons over 65 years of age are not recommended to go outside unless absolutely necessary, and if even the most harmless symptoms of a cold appear, call a doctor immediately.
- Vaccination is especially important for older people. Flu vaccinations reduce the risk of death among patients over 65 by 50%.
General information
Viral pneumonia is an acute inflammation of the respiratory tract of the lungs, caused by viral pathogens, occurring with a syndrome of intoxication and respiratory distress.
In childhood, viral pneumonia accounts for about 90% of all cases of pneumonia. In the structure of adult morbidity, bacterial pneumonia predominates, and viral pneumonia accounts for 4–39% of the total (persons over 65 years of age are more often affected). The incidence of viral pneumonia is closely related to epidemiological outbreaks of ARVI - their rise occurs in the autumn-winter period. In pulmonology, a distinction is made between primary viral pneumonia (interstitial with a benign course and hemorrhagic with a malignant course) and secondary (viral-bacterial pneumonia - early and late).
Viral pneumonia
Is there a vaccine against this disease?
The vaccine against pneumonia is widely known and is one of the mandatory vaccinations for children, but it involves protecting the body from pneumococci. Accordingly, this vaccination protects against the bacterial form of the disease. And this vaccine alone is not enough to protect against viral pneumonia. There is no vaccine against this disease, as such. But there are vaccines against various viruses.
Since the same viruses can cause both influenza and pneumonia, the influenza vaccine can also be considered a vaccine against viral pneumonia.
It is known that influenza viruses are constantly modified, so vaccines are also regularly improved. Every year, drugs are created against the most common strains of the virus at the moment. In this regard, it is necessary to be vaccinated annually in the fall, no later than two weeks before the expected development of the seasonal epidemic. After using the vaccine, antibodies are produced in the body within two weeks.
Even if a vaccinated person is still infected, the disease will pass in a very mild form. It is impossible to become infected from vaccination, since the vaccine does not contain live bacteria or viruses.
What happens inside the lungs
April 20, 16:04
The regional Ministry of Health has changed the procedure for hospitalization of patients with community-acquired pneumonia
Now patients with community-acquired pneumonia will be sent to Barnaul Hospital No. 5
Pneumonia is an inflammatory disease of the lower respiratory tract, small bronchi, and pulmonary alveoli. Despite the fact that it is an infectious disease, it is almost impossible to become infected from another person, the doctor emphasizes. The exception is viral pneumonia. This is exactly what COVID-19 causes.
“Inflammation caused by microbes causes the alveoli to fill with fluid. Because of this, gas exchange is disrupted and breathing becomes difficult. The most common causative agent of pneumonia is the microbe pneumococcus. Vaccination against pneumococcus will help prevent the disease,” explains Irina Bakhareva.
Prognosis and mortality
Viral pneumonia is usually milder than bacterial pneumonia and usually ends with recovery. Cure occurs on average after two to three weeks.
About a third of patients stay sick longer, this is usually associated with the development of complications:
- addition of a bacterial infection;
- Chronical bronchitis;
- meningitis;
- encephalitis;
- pleurisy;
- lung abscess;
- otitis;
- pyelonephritis;
- obstructive bronchiolitis in infants.
All these complications can occur due to reduced immunity, previous diseases, as well as due to untimely initiation of therapy. The possibility of death is less than 1% and only among the risk group.
The sooner a patient sees a doctor, the less likely it is to get a complication of viral pneumonia!
How is viral pneumonia treated?
In case of severe disease, immediate hospitalization of the patient is required. This also applies to groups of people who have an increased risk of death. For example, newborns and elderly people. When the course of the disease is mild, only medical supervision is necessary. For bacterial pneumonia, broad-spectrum antibiotics are used. For viral infections, special medications are used against the causative virus.
Inflammation due to influenza, for example, is treated by taking Oseltamivir or Zanamivir. They are used the first two days after the first manifestations. RSV can be cured with Ribavirin. For chickenpox or herpes virus, Acyclovir, etc. is used. Each virus and type of virus corresponds to a specific medicine.
Note! The drug will not work if the causative virus has been identified incorrectly. All of the above medications cannot be taken on your own. They should be prescribed by your doctor after a detailed diagnosis.
conclusions
- Pneumonia can be viral, most often occurring during a seasonal flu epidemic.
- Risk groups include children of primary preschool age and adults over 65 years of age.
- The main preventive measures are to follow good hygiene, lead a healthy lifestyle, minimize contact with other people and get immunized.
- Treatment of viral pneumonia in adults and children is carried out with antiviral agents and drugs that alleviate symptoms.
- Recovery occurs in about two to three weeks.
Features of the viral type depending on the causative virus
| Enterovirus | The clinical picture is not clear. In the classic course, the symptoms of such pneumonia are not expressed. A person complains of high blood pressure, fatigue, problems with the intestines and other gastrointestinal organs |
| Parainfluenza | The most common causative agent of viral pneumonia in newborns. The manifestation of symptoms is mostly moderate - the disease passes without visible complications. Occasionally, cases of severe symptoms are recorded. For example, loose stools or cramps |
| RSV | Pneumonia caused by respiratory syncytial virus leads to inflammation of the bronchioles. Patients have a persistent cough, lung failure (it can reach up to 39 degrees) |
| Adenovirus | A characteristic feature is extremely pronounced symptoms at the initial stage of the disease. On the first day, the temperature even rises to 39 degrees and remains in this state for up to 15 days. In addition, frequent coughing and shortness of breath are observed. Sometimes the disease is accompanied by conjunctivitis |
| Flu | The first signs are mild. Symptoms of the disease are moderate at each stage. Acute pain, respiratory failure and high fever occur only in cases where we are dealing with severe pneumonia |
Note! Adenoviral pneumonia lasts the longest. They most often cause complications and relapses. The duration of the disease in the acute stage is from 10 to 15 days.
Consequences and complications
Pneumonia is considered a dangerous pathology. Delayed or incorrectly prescribed treatment can lead to very serious consequences, including the death of the patient.
Complications after pneumonia include:
- meningitis;
- sepsis;
- pleurisy;
- lung abscess;
- pulmonary edema;
- severe respiratory failure with suffocation.
As soon as the first symptoms appear, you should immediately seek help from a doctor. This is the only way to avoid complications.
Prevention
During the autumn-winter period, doctors recommend that children and adults take vitamin complexes, take care of personal hygiene, and try to avoid large crowds of people and communication with patients.
It is necessary to control the body's water balance. To do this, you need to drink clean water, teas, juices, and compotes more often. Smokers should give up this bad habit. If your work involves a large number of people, it is advisable to get vaccinated against the flu in the fall. Preventing viral pneumonia is much easier than getting rid of it.
Treatment of pneumonia due to coronavirus
The main points of the treatment regimen for patients with viral pneumonia caused by COVID-19 are as follows:
- hospitalization and placement in boxes (isolated wards);
- bed rest;
- drug therapy;
- oxygen therapy.
Access to such patients is permitted only to medical professionals; access to other people is strictly prohibited.
There is no etiological treatment for viral pneumonia with the new coronavirus COVID-19 - this means that medications that can directly affect this pathogen do not yet exist.
note
Currently, research is being conducted on the effect of various drugs on coronavirus that were used to treat other diseases - these are drugs used in the treatment of malaria, AIDS, some anti-inflammatory drugs, and so on.
Patients with viral pneumonia are treated according to regimens that are used for other viral pneumonias. Involved:
- solutions for intravenous infusion. Infusions are necessary to remove organic toxins from the body and relieve intoxication syndrome. Electrolytes, saline and protein solutions, and so on are used - isotonic sodium chloride solution, glucose solution, protein preparations, blood serum and others;
- injectable medications to reduce fever. The most accessible method of eliminating hyperthermia is analgin in combination with diphenhydramine; if they are ineffective, corticosteroids are used;
- antibacterial and antifungal drugs - prescribed for signs of bacterial and mycotic (fungal) infection.
Mention is made of the use of antiretroviral drugs, immunostimulants, and, when an autoimmune component of the disease is identified, immunosuppressants and glucocorticosteroid drugs.
Oxygen therapy is prescribed from the very beginning of patient treatment. It is carried out using oxygen probes, masks or oxygen helmets (devices that allow oxygen to be pumped into the lungs under pressure).
Important
Patients with severe breathing problems require mechanical ventilation - they are connected to a ventilator (artificial lung ventilation).
Treatment of the disease
Treatment of the disease is complex and depends on the form and severity of the inflammatory process.
Mild pneumonia is treated on an outpatient basis, while moderate and severe pneumonia is treated in a hospital setting. Sometimes the patient is hospitalized in the intensive care unit and intensive care unit; treatment with oxygen or mechanical ventilation may be required.
The mainstay of treatment is antibiotic therapy. For mild severity, oral administration of broad-spectrum drugs is prescribed. After the result of the analysis to identify the pathogen and its sensitivity is received, treatment can be adjusted.
If we are talking about moderate and severe forms of the disease, people with reduced immunity, children or the elderly, then preference is given to injections of antibacterial drugs. Their concentration in the blood is greater and they act faster with this method of administration. It may be necessary to take combined antibiotics from different groups. The duration of the course is 10-14 days for a mild course, 3-4 weeks for a severe form of the disease.
Symptomatic therapy is carried out. Antipyretics, immunomodulators, bronchodilators and mucolytics, antihistamines, and analgesics are prescribed. If there are violations of the body systems, adequate treatment is prescribed.
In case of severe intoxication, detoxification therapy is prescribed. It is performed in a hospital setting and by intravenous drip.
The following may also be prescribed:
- Oxygen therapy.
- Physiotherapy.
- Massage.
- Inhalations.
- Physiotherapy.
All patients are recommended:
- Bed rest.
- Limiting physical activity.
- Drink plenty of fluids.
- Easily digestible food, rich in vitamins and microelements.
Development of pathology
The new coronavirus infects a person when it comes to him from an infected person. The modes of transmission of the virus are airborne droplets and contact (by shaking hands, kissing, etc.).
The pathogen cannot circulate in the air for a long time - it dies within just a few hours. But it has already been established that COVID-19 can survive on certain surfaces for up to several days, which means that, having touched such a surface, it can then be introduced into one’s own body through the mucous membranes of the eyes or respiratory tract.
It is important to understand that an infected person does not have to become sick himself to infect another person.
The coronavirus enters first the upper respiratory tract, and then into the lower parts of the bronchial tree and lung tissue, in which, under its influence, the inflammatory process starts. One of the main and dangerous elements of this process is infiltration - saturation of the lung tissue with exudate, its swelling and compaction.
As a result of such changes, the lungs are not able to maintain, as before, the respiratory function - absorb oxygen for its further transportation throughout the body and remove carbon dioxide.
note
An autoimmune component is suspected in the development of viral pneumonia in COVID-19. This means that the body ceases to distinguish between its own tissues and perceives them as a “stranger,” and therefore begins to fight them, literally “pitting” the immune system on them.
With favorable development of the pathology, the compactions of the lung tissue disappear (dissolve), but connective tissue begins to grow in this place.