A considerable part of the pathological disorders of the gastrointestinal tract is due to benign diseases of the esophagus, the most common of which are hiatal hernia, achalasia of the esophageal cardia and Barrett's metaplasia. Despite their benign nature, diseases of the esophagus, if diagnosed late and not treated in a timely manner, can develop severe complications that often lead to death.
Function and purpose of the esophagus
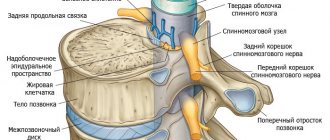
The human digestive system is a complex anatomical structure, the main function of which is to process and extract nutritional components from food, as well as absorb them into the blood and remove indigestible products from the body. The systemic vital organs are connected to each other by the digestive canal, part of which is the human esophagus - a muscular tube through which food from the pharynx enters the stomach. The motor function of the esophagus, due to muscular contraction of the walls, allows swallowed food to move freely into the stomach along its entire length in a few seconds. The speed of the peristaltic wave in the esophagus is about 5 cm/sec.
Diet therapy
The diet is based on the individual characteristics of the body, the degree of stenosis and provoking causes. Three dietary tables are widely used:
- No. 1, suggesting a full menu including pureed dishes, steamed or boiled. Hot and cold foods are excluded. You should eat small portions up to 6 meals.
- No. 1a, which involves the consumption of warm liquid and semi-liquid dishes up to 6 times a day with breaks of 2.5 hours. The amount of salt is limited, the volume of water is increased to 1.5 liters. Additionally, foods high in vitamins are introduced: A, B6, B12, C. It is not allowed to eat bread, baked goods, vegetables, sausages, smoked meats, fatty meats, canned food, sweets, sour fruits and berries, coffee with strong tea, and soda.
- No. 1b, suggesting a complete low-calorie menu with a limitation of chemically, thermally, and mechanically irritating foods to the mucous membrane. Food should be ground and boiled. The consistency is liquid, mushy. Meals are fractional.
Classification of esophageal diseases and their symptoms
A functional disorder in the functioning of the digestive organ can cause various diseases of the esophagus, the symptoms of which are expressed in bad breath, heartburn, belching or other pain in the upper abdomen. The most common symptomatic diseases of the esophagus are associated with various types of neoplasms - cyst, cancer, hiatal hernia, and so on. Let's consider diseases of the esophagus, the symptoms and treatment of which are not related to cancer, however, require increased attention from gastroenterologists.
Diagnostics
Diseases of the esophagus are confirmed by diagnostic procedures. The patient may receive a referral for one or more studies necessary to clarify the characteristics of his condition:
- esophagogastroscopy: allows you to visually assess the characteristics of the organ’s condition, perform a tissue biopsy, identify a foreign object and remove it;
- functional testing: necessary to evaluate gastroesophageal reflux;
- radiography with contrast agent (barium): performed in several projections;
- daily intraesophageal pH-metry: changes in acid-base balance are assessed during a specified time period;
- esophagotonokymography: prescribed for suspected functional disorders, allows you to assess the motility of the esophagus.
Achalasia of the esophageal cardia
Achalasia cardia is a primary neuromuscular disease associated with the absence or insufficiency of reflex relaxation of the lower esophageal sphincter, a control valve that separates the esophagus and stomach. As a rule, signs of disease of the esophagus are associated with a narrowing of its lower section, as a result of which there is a violation of the passage of food into the stomach. The frequency of achalasia cardia, according to various medical experts, ranges from 5 to 20% of all diseases of the esophagus and stomach. In European countries, the prevalence of various stages and degrees of achalasia cardia reaches 5-8 thousand people per 100 thousand population.
To date, the true causes of achalasia of the esophageal cardia in humans have not been established. Several hypotheses have been put forward according to which the development of the disease is based on a genetic factor, viral infection, autoimmune causes or degenerative processes.
Symptoms of esophageal achalasia
This type of digestive system disease is characterized by a triad of symptoms, which is expressed in the following manifestations:
- Dysphagia, that is, a violation of the act of swallowing when taking solid and liquid food.
- Esophageal regurgitation, or food vomiting.
- Cramping pain behind the sternum.
An additional symptomatic sign of esophageal disease during a diagnostic examination is hypertension, that is, increased pressure in the sphincter region and low amplitude of peristaltic waves. In some cases, esophageal peristalsis is preserved, however, motor functions are completely absent.
Treatment of achalasia cardia
The main method of medical care for restoring cardia patency was symptomatic therapy. Of the medicinal pharmaceutical treatments, the most rational was considered to be the use of various antispasmodics, adrenergic agonists, nitrates (Nitroglycerin®) and other dosage forms that eliminate the main pain symptom. However, pathogenetic treatment of esophageal disease with medicinal drugs for achalasia cardia does not give a positive result. During endoscopic examination a year later, recurrence of dysphagia occurred in 50% of patients, and serious complications - perforation or rupture of the esophageal wall, bleeding or peptic stricture of the esophagus - were observed in 15% of patients. Today, there are more than 60 methods of operations for achalasia cardia, which indicates the seriousness of this clinical pathology. The most effective and optimal method of surgical treatment is considered to be endoscopic intrasphincteric injection of botulinum toxin into the lower esophageal sphincter, which allows increasing the average rate of satisfactory results in restoring full passage of food.
Description of the pathology
Obstruction is the appearance of a barrier that causes narrowing or blocking of the esophageal lumen.
Poor permeability makes it difficult for food and liquid to enter the stomach. In most cases, the pathology develops after damage to the esophagus. Less commonly, obstruction of the esophagus occurs against the background of the development of cancer in its wall. External compression of the tract by nearby pathological tissues is also possible.
Signs of vascular disease of the esophagus are often low-contrast at the initial stage. The patient may experience periodic general symptoms of malaise. But varicose veins are dangerous due to sudden bleeding.
How does a person feel:
- aching generalized pain in the chest;
- dryness and sore throat;
- salty taste of saliva.
Without treatment, varicose veins can last a long time, for years. Factors that provoke bleeding include heavy lifting, high fever due to colds, and trauma to the esophagus.
The close proximity of the digestive and respiratory systems contributes to the confusion of symptoms during inflammatory processes. Thus, the appearance of a coma in the sternum or esophagus is possible with the development of tracheobronchitis, tracheitis, laryngitis, since swollen tissues compress the lumen of the esophageal tube. With catarrh (inflammation) of the upper respiratory tract, difficulty and pain when swallowing are added.
Most often, acute inflammatory diseases occur with fever, cough, and signs of intoxication. If the process is sluggish, and discomfort in the esophagus is the only sign, it is difficult to distinguish digestive pathology from respiratory pathology on your own. The correct diagnosis will be made by an otolaryngologist, and you should contact him.
Hiatal hernia
According to statistics, the symptoms of gastroesophageal reflux as the main manifestation of a hiatal hernia are constantly growing. Currently, diseases of the digestive system are diagnosed in 10% of the world's population, and are comparable in prevalence to chronic cholecystitis, gastric ulcer or duodenal ulcer.
What is a hiatal hernia (HH)
According to the International Classification of Diseases (ICD10), this type of esophageal disease is assigned code K44.9. The disease is formed as a result of displacement into the chest of one of the parts of the anatomical organ - the abdominal segment or the cardiac part of the esophagus, which are normally located under the diaphragm. A diaphragmatic hernia can be either a congenital defect due to an embryonic defect or an acquired clinical condition. The most likely causes of a hiatal hernia are:
- Weakness of the ligamentous apparatus of the esophageal opening of the diaphragm. As a rule, this condition occurs in people after 60-65 years.
- Increased intrauterine pressure due to injury to the esophagus, chronic constipation, difficult working conditions and other conditions.
- Impaired motility of the digestive tract, for example due to esophageal dyskinesia, chronic pancreatitis or cholecystitis.
- The result of an asthenic physique.
The most severe complication of a hiatal hernia is bleeding, peptic ulcer or esophageal stricture, metaplasia (Barrett's esophagus).
Types and symptoms of hiatal hernia
According to clinical and morphological characteristics, hiatal hernias are divided into three types (see table).
| Type of hiatal hernia | Signs of esophageal disease |
| Sliding (axial) hernia | This type of pathology, in which the diaphragmatic-esophageal membrane is not broken, is diagnosed in 90% of cases and is characterized by free slipping of the upper stomach and lower sphincter into the abdominal cavity and back. |
| Paraesophageal (fixed) hernia | The clinical condition is the movement of the distal part of the esophageal opening and cardia under the diaphragm, while part of the stomach is located above the diaphragm. |
| Mixed | The pathology combines both types of hiatal hernia. |
Symptoms of esophageal disease are similar to other pathologies of the gastrointestinal tract:
- due to the hernial sac, the phrenic nerve is irritated, and hiccups occur,
- due to gastroesophageal reflux, acidic stomach contents enter the esophagus, which provides a person with painful heartburn and frequent belching,
- movement of the hernial sac during a sliding hernia causes the patient to experience burning and unbearable pain behind the sternum,
- Swallowing disturbances (dysphagia) occur even when consuming liquid food.
Treatment of diaphragmatic hernia
The choice of treatment for hiatal hernia depends on the degree of exacerbation. At the initial stage, the use of conservative therapeutic measures is effective. The comprehensive treatment program includes medications:
- Prokinetics that improve the condition of the mucous wall of the esophagus - Trimedat® , Motilak® , Ganaton® , etc.
- Antacid group drugs that help neutralize hydrochloric acid that is part of gastric juice - Gastalom® , Maalox® , etc.
- Proton pump (pump) inhibitors that neutralize gastric acidity.
- B vitamins to speed up stomach recovery.
A mandatory therapeutic condition for the treatment of a hiatal hernia is a diet that excludes foods that cause increased acidity and gas formation. Alcoholic drinks, fried, fatty, salty, smoked and pickled foods are excluded from the diet. Small meals 5-6 times a day are recommended.
Nutritionists recommend: for diaphragmatic hernia, you should drink up to 2 liters of alkaline mineral water daily.
If drug therapy is ineffective, surgical intervention is considered.
Treatment options
Therapeutic tactics depend on why the pathology arose, as well as on the degree of its development. When a foreign particle gets stuck in the esophagus, it is removed through an esophagoscope with bougienage (expansion) of the narrowed lumen. In case of esophageal dysfunction due to the development of oncology, surgical methods are used.
After establishing the cause of the obstruction, therapy is prescribed aimed at eliminating the underlying disease, which was the result of dysphagia.
1. Surgical method - used to remove a foreign body and eliminate some other causes of food not entering the stomach.
2. The use of radiation therapy is used for tumor processes.
3. The affected areas of the esophageal mucosa are treated endoscopically.
4. The use of self-expanding stents increases the esophageal lumen and promotes its better patency.
5. The doctor can prescribe medications that alleviate the manifestations of the pathology.
6. The patient must adhere to a special diet: eat pureed soups and cereals, dairy and fermented milk products, eat only lean meat. Portions should be made small, but taken 5-6 times a day. It is forbidden to consume coarse and heavily fried foods in the diet, or drink alcohol.
Therapy is selected for each individual, depending on the severity of the disease and the causes of swallowing disorders.
In extremely severe conditions, the patient is treated in a hospital, and a flexible tube inserted into the stomach through the oral cavity or gastrostomy tube (as indicated) is used for feeding.
Treatment of patients with benign esophageal obstruction is carried out in the surgery department; in the presence of esophageal cancer, the patient may be in the gastroenterology or oncology department. The treatment regimen for esophageal obstruction depends on the cause of this pathology.
In case of benign esophageal obstruction, it is preferable to use endoscopic dilation of esophageal stenosis, endoscopic bougienage of the stenotic area. In recent years, techniques such as endoscopic dissection of a cicatricial stricture of the esophagus, and in severe forms of obstruction, endoprosthesis replacement (stenting) of the esophagus have been widely used. To restore patency of the esophagus, it may be necessary to remove a foreign body, surgical removal of a tumor, or esophageal cyst. Conservative or surgical treatment of the disease, which has led to external compression of the esophagus, is also carried out.
Malignant forms of esophageal obstruction require pathogenetic treatment: radiation or chemotherapy, surgical removal of the tumor followed by esophagoplasty. Conservative measures include normalizing the level of essential nutrients in the blood and electrolytes. If necessary, nutrition is adjusted and medications are prescribed to treat anemia.
There is no universal treatment method for all pathologies of the esophagus. The vastness of the etiology and development of diseases implies an individual approach to therapy:
- For inflammation, antacids (protect the mucous membrane from the aggressive effects of acid thrown from the stomach) and decongestants are used.
- In case of achalasia in the initial stage, bougienage and expansion with special balloons are prescribed.
- Diverticula are sutured surgically.
- Strictures and adhesions after burns are dissected.
- In the treatment of Barrett's pathology, innovative methods of radiofrequency ablation and argon coagulation of the affected mucosa are used.
Damage to the esophagus as a result of trauma and extensive tissue ruptures require surgical intervention, in some cases plastic surgery.
Treatment with folk remedies does not provide complete healing, but can maintain the body in a state of remission. This treatment is aimed at maintaining a normal level of acidity in the esophagus and preventing reflux. Flax seeds and oats are brewed as antacids. To maintain a normal pH level, drink the following infusion as tea:
- St. John's wort;
- chamomile;
- rosehip;
- calendula.
Compliance with diet and food processing rules is important. You should reduce your consumption of fried, fatty foods and avoid overeating. Stick to a strict diet during an exacerbation period.
For diseases of the esophagus, symptoms and treatment are specific. Most of them are curable; it is important to correctly identify the disease and select individual therapy.
Barrett's esophagus
A serious complication of a hiatal hernia is metaplasia or Barrett's esophagus. According to diagnostic parameters, this is an acquired disease that occurs with gastroesophageal reflux, a condition of the esophagus when the epithelial lining is manifested by the replacement of cylindrical intestinal metaplasia, which subsequently leads to the development of adenocarcinoma of the esophagus.
This precancerous condition is observed in 10% of patients treated for a burning sensation behind the sternum (heartburn) with gastroesophageal reflux. The characteristic symptomatic signs of the disease are:
- severe dysphagia,
- frequent and prolonged heartburn,
- vomiting with blood,
- pain in the epigastrium (under the stomach).
A special feature of Barrett's metaplasia is rapid weight loss that occurs due to swallowing disorders and pain associated with dysphagia.
Nutrition for diseases of the esophagus
The choice of scheme depends on the cause of unpleasant omissions. If the pain is pronounced, then fasting is prescribed for a period of 2 days. Then the patient is fed often, not food is given in small portions.
Let's consider an approximate nutritional plan for such pathologies:
| First days: | Subsequent days: |
| After hunger, a person is given food in pureed, crushed form. These are meat products, as well as various broths without seasonings and other ingredients that can cause irritation to the mucous membranes. The amount of fat is minimal, but it is important to ensure that a person receives a sufficient amount of proteins and carbohydrates for the normal functioning of vital organs and systems. | Vegetables and fruits are placed on the patient; at the initial stage they are eaten pureed, like puree. Then they are ground on a grater, you can stew and cook the meat, chopping it with a blender or using a meat grinder. |
Food should not be hot, sour, salty or too spicy. This will irritate the mucous membrane not only of the esophagus, but also of the stomach. For burns of various causes and injuries, it is recommended to drink cool liquid.