Hepatologist
Related specialties: gastroenterologist, therapist.
Address: St. Petersburg, Academician Lebedeva St., 4/2.
The diet according to table No. 5 is usually prescribed for diseases of the hepatobiliary tract (liver, bile ducts and bladder). Its main task is to reduce the load on gland cells, normalize bile flow and restore digestion in general.
The liver suffers daily from poor nutrition, alcohol, toxic factors, and infectious agents. As long as the hepatocytes are healthy, it can perform its physiological functions and maintain the performance of the entire body. Abuse of fatty and spicy foods increases the load on the liver, as a result of which any toxic factor can lead to cell damage and the development of the disease.
The mild course of the pathology is often reversible and does not lead to complications. Provided timely cessation of contact with the provoking factor, it is possible to completely restore the functioning of hepatocytes.
In severe cases of the disease, the risk of such undesirable consequences increases, such as:
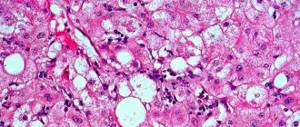
- liver failure, which develops as a result of necrosis of hepatocytes and their replacement with fatty inclusions. Symptomatically, the pathology is manifested by swelling, icteric syndrome and loss of body weight;
- coma. Disruption of the central nervous system at the initial stage is manifested by encephalopathy. As intoxication increases, consciousness is gradually depressed, which leads to the development of coma;
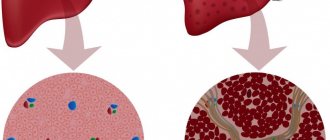
- cirrhosis. Its occurrence is based on scarring of the liver, in which dead hepatocytes are replaced by connective tissue elements.
The importance of diet
The preparation of a nutritious diet should be done exclusively by a specialist, taking into account the severity of the disease and the needs of the body. It is also necessary to take into account the person's profession and associated diseases. In case of toxic death of hepatocytes, nutrition should meet the following principles:
- frequent divided meals (every two hours in small portions);
- daily calorie content should not exceed 2500 kcal;
- products - at a comfortable temperature, since cold and hot dishes disrupt the process of bile outflow due to dysfunction of the cystic sphincter;
- Meals should be at the same time;
- ground dishes prepared by baking, boiling or stewing are recommended;
- preference should be given to low-fat types of milk, fish and meat products;
- porridge with milk is healthy;
- the diet should contain mainly vegetable fats;
- requires drinking plenty of fluids.
With regard to energy value, the diet for toxic hepatitis should include daily:
protein products, since with food the body receives essential amino acids necessary for the construction and functioning of cells. The requirement is calculated as follows: 1 g/kg of weight. According to indications, the doctor can increase the protein intake into the body to 1.5 g/kg. On average, 100 g are required daily;- daily lipid intake should not exceed 80 g. If, during instrumental diagnostics, fatty inclusions in hepatocytes are detected, dietary restrictions can reach 50 g/day. Lipids must come from both plant and animal foods;
- the daily volume of carbohydrates is a maximum of 350 g (in the absence of obesity).
What can you eat if you have toxic hepatitis?
To restore the structure of hepatocytes and normalize the functioning of the digestive organs, it is necessary to adhere to dietary nutrition throughout life. This is especially important if the toxic factor continues to affect the body (medicines, occupational hazards). The diet does not prohibit eating the following foods:
- baked goods, including day-old bread and crackers;
- low-fat milk, plenty of fish and meat;
- egg white omelet;
- light soup with cereals or pasta;
- vegetable salad;
- dried fruits;
- milk soup;
- vegetable oil;
- cereal porridge with water or milk. Oatmeal, buckwheat, millet and rice are allowed;
- non-acidic vegetables;
- honey (whole sugar can account for no more than 10% of the daily volume of carbohydrates, that is, 30 g);
- marmalade;
- bran;
- green tea.
List of prohibited products
Improper nutrition against the background of the effect of a toxic factor on the body is fraught with an increase in the severity of liver failure and a deterioration in the general condition of a person. The consequence of this can be fatty degeneration of the gland and cirrhosis (replacement of hepatocytes with connective tissue). To relieve the liver, food should not contain the following types of foods:
- fatty varieties of milk, fish and meat delicacies;
- smoked meats;
- pickles;
- marinade;
- semi-finished products;
- salt is limited to 8-10 g/day;
- freshly baked pastry;
- spicy seasonings;
- sour vegetables, fruits;
- salo;
- any fried foods;
- conservation;
- mushrooms, including broths;
- mayonnaise;
- fried eggs;
- okroshka;
- sausage;
- soda;
- rich broths;
- sorrel, spinach;
- legumes;
- cocoa;
- black tea (strong);
- radish;
- pancakes;
- coffee;
- horseradish;
- ice cream.
Alcohol in a toxic form of hepatitis is prohibited in any form - including low-alcohol drinks.
Features of toxic hepatitis in children
In our country, the toxic form of hepatitis is diagnosed in childhood quite rarely. But this is not a reason to say that the younger generation will not be affected by this problem.
A risk factor is the penetration of toxic compounds into the liver organ completely by accident.
The fault will lie in the negligence of the parents, as well as in cases of using medications for other purposes, without following the doctor’s instructions. Children can experience poisoning from mushrooms and plants.
The pathology is quite difficult. If proper medical treatment is not observed, death cannot be ruled out.
Children most often suffer from the acute form of the disease. The symptoms are similar to the same clinical picture that appears in adults. The prognosis in this case will be unfavorable.
Examples of daily diet
To minimize acute liver damage from toxins, it is recommended to eat approximately the following menu.
| Options | Breakfast | Lunch | Dinner | Dinner |
| 1 day | Semolina/oatmeal with dried fruits | Fruit salad/biscuits | Vegetarian cabbage soup/fish soup, rice with chicken, stewed cabbage | Vegetable stew |
| 2 | Cottage cheese with sour cream, salad with black bread | Carrot casserole | Potato soup, boiled fish | Milk rice porridge |
| 3 | Oatmeal, salad | Casserole (cottage cheese) with dried fruits | Stuffed cabbage rolls/pasta with sauce, soup | Buckwheat groats/rice with chicken |
| 4 | Protein omelet, vegetable cutlets | Lazy dumplings/yogurt | Vegetarian borscht/vegetable broth, chicken (boiled) with carrots | Pasta/barley porridge, cheese/steam cutlets, salad |
| 5 | Rice porridge, steam cutlet | Baked apples with honey and cinnamon | Vegetable soup, pasta, meatballs, salad | Carrot puree |
| 6 | Pasta with chicken/omelet with vegetables | Cheesecakes/unleavened biscuit | Milk/chicken soup, wheat porridge, meatballs | Mashed potatoes, fish |
| 7 | Buckwheat, cutlets, greens | Curd pudding | Pasta and chicken/baked potato, cabbage soup | Stewed vegetables, fish |
Dishes that are suitable for snacking during lunch can be recommended for an afternoon snack. Before going to bed, low-fat milk, light fruit salad, juices or green tea are allowed.
Delicious recipes
When chronic toxic hepatitis is in remission, the strict nutritional diet can be slightly expanded. You can diversify the menu and cheer up with the following dishes:
It is important to understand that with the continued effect of the toxic factor on the liver, it is impossible to achieve complete restoration of the structure of the organ. However, by eliminating its influence, there is a chance to improve the functioning of hepatocytes and normalize the functioning of the entire digestive tract.
The liver in our body is the most amazing and unpretentious organ. It performs more than 400 different functions, and is the main barrier between the blood coming from the intestines and all other organs. Hepatocyte cells process the incoming material, synthesize from it substances necessary for the entire body, remove and neutralize poisons and toxins.
Having a huge ability to regenerate, the liver is nevertheless susceptible to the destructive effects of harmful substances if they come in quantities that are difficult for it to cope with. In this case, inflammation of the liver develops - hepatitis, and hepatocyte cells partially die and are destroyed. What is toxic hepatitis, what factors cause it and how is this disease treated?
What is toxic hepatitis
Inflammation of the liver occurs for various reasons: bacterial and viral infections, fungal diseases and parasitic infestations, exposure to toxic substances. If the destruction of liver cells occurs under the influence of aggressive chemicals entering the body from the outside, then this disease is called toxic hepatitis. What it is?
- Acute toxic hepatitis develops as a result of exposure to a small amount of potent poison or weak irritants, but in large concentrations. As a rule, toxins enter through the gastrointestinal tract, less often through the respiratory tract and skin.
- Chronic hepatitis occurs due to repeated exposure to small doses of a toxin over a long period of time. Diseases related to hepatitis are coded according to ICD-10 under the number K71 (toxic liver damage). Alcoholic liver disease is separated into a separate group and has code K70.
Can toxic hepatitis be contagious? No, this is an exclusively therapeutic disease caused by the influence of an external chemical factor on a certain person. A group disease occurs only if all patients are simultaneously exposed to a toxin (food poisoning, industrial accidents).
Classification
According to the nature of the course, toxic hepatitis is divided into two types:
- Acute – develops in the first hours or days after exposure to poisons, has a rapid development and a severe course;
- Chronic – occurs a long time after the onset of exposure to poisons, develops slowly, and is relatively mild.
According to etiological factors, toxic hepatitis is divided into 4 groups:
- Toxic drug-induced hepatitis;
- Toxic alcoholic hepatitis;
- Hepatitis caused by industrial poisons;
- Hepatitis caused by naturally occurring poisons.
Based on the penetration of poisons into the human body, there are 3 groups of hepatitis:
- Intentional hepatitis;
- Random hepatitis;
- Occupational hepatitis.
Causes of toxic hepatitis
According to statistics, the most common cause of toxic hepatitis in Russia is alcohol abuse, as well as the subsequent uncontrolled use of medications to relieve a hangover.
Drug-induced toxic hepatitis develops as a result of a single dose of a large dose of drugs or long-term treatment, even under medical supervision. The most dangerous drugs for the liver include the following groups:
- antipyretics;
- anti-tuberculosis;
- sulfonamides;
- antiviral;
- anticonvulsants.
Separately, hepatitis can be distinguished after chemotherapy for cancer. Cytotoxic drugs used to suppress the growth of cancer cells have a negative effect on all organs and tissues, primarily on the liver. After chemotherapy, a blood test is required to monitor the state of biochemical processes in the liver. Depending on the results, diet and rehabilitation treatment are prescribed.
Another cause of toxic hepatitis is industrial poisons. This group of substances can poison the body both through the digestive tract and by contact with the skin or inhalation of polluted air. The main hepatotoxic substances used in modern industry are:
- pesticides, including insecticides;
- chlorinated hydrocarbons (petroleum products);
- phenols;
- aldehydes;
- phosphorus;
- arsenic.
Another large group of toxins that have a destructive effect on the liver are poisons of plant origin:
Poisoning with plant poisons usually occurs as a result of improper collection of mushrooms or self-medication with herbal mixtures of unknown origin.
Reasons for appearance
There are risk factors that increase the likelihood of toxic hepatitis.
Namely:
- people working in hazardous industries;
- alcohol abuse;
- women - the metabolism of the weaker sex is slower, so a high concentration of harmful components is maintained in the liver for a long time;
- children under the age of 3 years;
- people over 45 years of age;
- pregnant women;
- presence of excess body weight;
- smoking abuse;
- the presence of malignant or benign tumors;
- presence of diabetes mellitus;
- liver diseases – cirrhosis, hepatosis;
- existing hepatitis - if a person has this disease, it can turn into a toxic form;
- heredity – if genetic mutations affect the production of liver enzymes, the likelihood of toxic hepatitis may increase;
- substance abuse.
Toxic hepatitis is a disease that can appear for various reasons. The most common of them are listed in the table.
Drugs that cause toxic hepatitis
| Reasons why toxic hepatitis may appear | Description |
| Use of medications | The doctor prescribes medications in the dosage that is necessary to achieve a therapeutic effect. Also, medications are prescribed only after the diagnosis has been clarified. If you take medications without a doctor’s recommendation, and also do not follow the dosage for a long time (it is indicated in the instructions), toxic hepatitis may develop. Or the disease appears when too much of the drug is used once. The group includes many drugs. Eg:
Separately, chemotherapy can be distinguished. The appearance of toxic hepatitis after the course is allowed. Cytotoxic drugs that are administered to humans suppress the growth of cancer cells, but have a negative effect on the entire body, and especially on the liver. |
| The influence of alcoholic drinks | Alcohol poisoning accounts for 60% of all deaths due to intoxication. In addition to the fact that alcoholic drinks damage the liver, they negatively affect the entire body. The situation gets worse in the case of low-quality alcohol. |
| Exposure to industrial poisons | Substances can penetrate through the respiratory system and skin. Poisons are absorbed into the blood and then enter the liver. The following substances have a harmful effect on the organ:
|
| The influence of plant poisons | The substances have a negative effect on the liver and disrupt the functionality of the organ. This group includes poisons of mushrooms (fly agaric, toadstool), weeds (ragwort, bittergrass). |
Toxic hepatitis is not a contagious disease. Pathology cannot be transmitted to a healthy person from a patient.
Diagnostics
First of all, the doctor collects an anamnesis. Based on the patient’s complaints, the suspected causes of the pathology and the presence of predisposing factors, the doctor determines a preliminary diagnosis. This is followed by examination and palpation of the patient. This determines the color of the skin and visible mucous membranes, the size and pain of the liver.
Laboratory tests include blood and urine tests, as well as microscopy of liver tissue:
- Blood biochemistry - liver tests (ALT, AST, total protein, total bilirubin and its fractions, alkaline phosphatase);
- General blood analysis;
- General urine analysis;
- Coagulogram;
- Examination of stool for the presence of toxins;
- Liver biopsy.
Among instrumental studies, ultrasound of the hepatobiliary zone is used.
Methods for diagnosing toxic hepatitis
In order for the patient to receive the correct treatment appropriate to the disease, it is necessary. Diagnosis of toxic hepatitis is difficult due to the similarity of its symptoms with other acute and chronic liver diseases.
In addition, other clinical studies are prescribed:
- urine and blood analysis;
- coagulogram;
- tests excluding various forms of viral hepatitis.
Biological fluids can also be taken for research to determine whether they contain various types of toxins.
Instrumental research methods include:
- Ultrasound of the abdominal cavity and other organs;
- magnetic resonance and computed tomography;
- radioisotope scanning;
- laparoscopy and liver puncture biopsy.
Symptoms of acute and chronic toxic hepatitis
Symptoms of toxic hepatitis will vary slightly depending on the nature of the disease. In an acute course, the first signs usually appear after 2–4 days, less often after 12–24 hours (for example, in case of poisoning with toadstool).
Acute toxic hepatitis is accompanied by the following symptoms:
- fever;
- pain in the right hypochondrium;
- vomiting, lack of appetite, nausea;
- yellowness of the whites of the eyes;
- discolored stool;
- bleeding from the nose, gums, pinpoint hemorrhages on the skin;
- darkening of urine;
- sometimes nerve disorders resulting from exposure to toxins on the nervous system.
In the chronic course of the disease, signs may periodically appear and disappear:
- slight increase in body temperature (37.0–37.5 °C);
- discomfort in the right hypochondrium;
- bloating, diarrhea;
- bitterness in the mouth, nausea, vomiting;
- itching in the skin;
- increased fatigue.
The liver increases in size, blood tests reveal an increase in bilirubin and alkaline phosphatase, and the level of AST and ALT enzymes changes. It is necessary to conduct additional studies to exclude other forms of hepatitis, primarily infectious.
Toxic hepatitis - causes, symptoms of the disease and the role of diet during treatment
Toxic hepatitis develops for one main reason - poisons and toxins enter the patient’s body. They can be chemicals, foods, plant poisons or medicines. Alcohol is also toxic to the body and causes the clinical picture of hepatitis when consumed regularly. Such substances can penetrate in different ways: through the digestive tract, with inhaled air, and also through the skin. A person may receive large amounts of toxins at one time or take them regularly in small doses. This will determine whether toxic hepatitis develops in acute or chronic form.
This disease is a form of poisoning. Since the liver is the body's main filter, its role is to eliminate toxic substances. If they come in high doses that the liver cannot cope with, they settle in its tissues and cause inflammation. This disease can be diagnosed by the following clinical signs:
- acute or aching pain in the right hypochondrium, in the area of the liver projection;
- jaundice (yellowing of the skin and visible mucous membranes), if inflamed liver tissue compresses the bile ducts and bile does not exit the gallbladder;
- nausea, vomiting, digestive disorders;
- headaches, dizziness, tremors (shaking) of the limbs - symptoms of toxins entering the central nervous system;
- increased body temperature, general weakness;
- darkening of urine and discoloration of stool.
The fact that hepatitis is of toxic origin will be indicated by the history. In origin, this disease can be occupational (develops in employees of the chemical and other industries), medicinal (after taking certain medications and chemotherapy), and also alcoholic. The first condition of treatment is the complete elimination of the influence of poisons and toxins on the patient’s body. The patient’s diet is no less important.
The liver is involved in the digestive process by synthesizing bile and regulating the metabolism of essential nutrients, so it is important to make its work as easy as possible. Under such conditions, liver cells will be able to regenerate more intensively, and damaged tissues will be replaced more quickly with healthy ones.
Toxic hepatitis is an inflammation of the liver caused by medications, chemicals or alcohol
Symptoms
The clinical picture of an acute type of hepatitis includes the following manifestations:
- disturbances in the functioning of the digestive system;
- loss of orientation in space;
- spider veins and subcutaneous hemorrhages;
- change in the color of urine and feces, jaundice;
- overexcitation or lethargy;
- coma, hallucinations, dizziness;
- hormonal imbalance.
An enlargement of the spleen and liver, cytolysis of hepatocytes, and neutrophilic-type leukocytosis are also observed. The intensity of clinical symptoms depends on the type of toxic effect and the stage of the pathology. In the chronic form of hepatitis, there may be no signs. Manifestations are not specific.
Hepatitis is often diagnosed in pregnant women. In this case, severe liver failure develops gradually, so it is quite difficult to identify pathology at an early stage. The patient feels fine for a long period. People who are in her close circle can become infected. The list of possible complications includes:
- fetal death;
- cholestatic hepatitis, accompanied by disruptions in the blood clotting process;
- bleeding in the early postpartum period.
Symptoms of the disease
Despite the fact that there are many liver poisons, the signs of toxic hepatitis are quite similar. The manifestations of the disease mainly depend on the form of the disease, and not on the type of poison that provoked the disease.
Signs of acute form
The pathology is characterized by an abrupt onset. Symptoms are noticeable 3-5 days after poisoning.
The acute form of toxic hepatitis occurs with the following main symptoms:
- intense pain in the area where the liver is localized, caused by an increase in the size of the organ and its capsule;
- fever and significant increase in temperature;
- aches in the joints and throughout the body;
- weakness;
- impaired orientation in space;
- nausea with vomiting. There may be blood in the vomit;
- bleeding from the nose;
- jaundice;
- spider veins;
- darkening of urine;
- pinpoint hemorrhages under the skin;
- lightening of feces.
In addition, a person experiences mental activity or, conversely, inhibition.
Symptoms appear quite quickly. It is necessary to respond to the signs of the disease in a timely manner and begin effective therapy.
11 symptoms of obstructive jaundice
Signs of chronic form
Clinical symptoms for this form of the disease usually occur several months or years after the onset of exposure to the poison.
The chronic form of toxic hepatitis occurs with the following manifestations:
- pressing pain in the liver area of aching nature. The painful syndrome intensifies after eating and can periodically disappear on its own;
- slight increase in temperature;
- jaundice;
- itching of the skin due to cholestasis and accumulation of bile acids;
- decreased performance and rapid onset of weakness in the body;
- an increase in the size of the liver and spleen;
- bloating;
- loss of appetite;
- nausea with periodic vomiting;
- the appearance of bitterness in the mouth.
All of the above signs can disappear and appear on their own. At the first manifestations of the disease, you should consult a doctor and undergo an examination. Timely treatment will reduce the destructive effects of toxins on the liver.
The disease is especially dangerous for children. The disease is uncommon in childhood and for this reason it is difficult to diagnose.
Treatment of toxic hepatitis
Treatment of toxic hepatitis consists of removing poison from the body as quickly as possible, symptomatic therapy and creating optimal conditions for liver regeneration. For this purpose, hepatoprotective substances are used. As a rule, these are vitamins, enzymes and herbal products.
Treatment of toxic hepatitis with folk remedies can only be used under the supervision of a doctor. Help relieve nausea and normalize liver function:
- juice from sauerkraut;
- mint infusion;
- grapefruit juice;
- infusion of horseradish roots;
- calendula decoction;
- pumpkin juice and pulp.
Medical therapy
First you need to stop complete contact with the toxic agent, as well as prompt elimination of them.
It is important to eliminate unpleasant symptoms, as well as the regeneration of hepatocides. The liver has the ability to repair itself. Damaged cells can recover up to 75%.
During the treatment of toxic hepatitis, it is customary to use special medications with a hepatoprotective effect.
During hepatitis, the course of treatment is 6-7 months. This is a really long time, but the pathology is also serious.
How dangerous is the disease?
The main harm of the toxic type of hepatitis is incurable and life-threatening complications. The most likely of them:
- Liver failure. When most of the cells of an organ are destroyed and replaced by fat cells, digestive and enzyme-forming functions are disrupted. The patient suffers from edema, weight loss, as well as pathologies of the nervous system leading to coma.
- Cirrhosis. With this disease, there is a gradual death of liver cells, as well as their subsequent replacement by scar tissue. If the development of cirrhosis is not stopped in time, it can lead to death.
Diet for toxic liver hepatitis
What diet should you follow for toxic liver hepatitis? Avoid all foods that are difficult to digest:
- fatty meat (pork, lamb, duck), lard;
- fatty fish;
- eggs;
- canned food;
- mushrooms;
- smoked meats;
- seasonings and sauces;
- pastries and fresh bread;
- strong tea, coffee, cocoa;
- sparkling water;
- nuts;
- onions, garlic, radish, sorrel;
- confectionery, ice cream;
- fatty varieties of cheese and cottage cheese, sour cream, butter.
Alcohol and nicotine are strictly prohibited!
You can’t eat fatty, spicy, fried foods. Food is steamed, baked or boiled.
The daily diet must include:
- porridge;
- dried bread;
- bran;
- chicken, veal;
- lean varieties of fish;
- milk and low-fat cottage cheese;
- vegetables and fruits.
It is also useful to drink green tea, a decoction of dried fruits, and eat figs and green vegetables.
Nutrition for toxic hepatitis should be taken in small portions, 5–6 times a day. It is advisable to adhere to the principle of separate nutrition: do not mix protein and carbohydrate foods in one meal, and eat fruits separately from everything else.
Features of the diet for hepatitis C
The basic rules of nutrition for hepatitis C include the following:
- The daily calorie intake should be 3100 kcal. It is this amount that allows the body to provide decent conditions to fight the virus;
- The patient’s diet should have the following ratio of proteins, fats and carbohydrates - 100/100/450, respectively;
- Salts - no more than 10-15 grams per day.
- It is worth remembering that with hepatitis C you need to eat in small portions five to six times a day. In this case, all food should be approximately the same temperature.
- Dishes in the diet of a patient with hepatitis C should be prepared either by steaming, or by stewing and boiling. Avoid fried foods completely.
During an exacerbation, it is necessary to transfer the patient to a more strict diet - table 5a, which involves reducing the daily amount of salt to 7-8 grams, and reducing fat to 70 grams. instead of 100.
What foods are prohibited for hepatitis C?
In case of exacerbation of viral hepatitis C, it is necessary to completely avoid the following foods:
- Fried fatty meats (and all fried foods in general);
- Marinated or smoked dishes;
- Rich meat and mushroom dishes, which have an increased level of carcinogenicity, thereby poisoning the body even more;
- Do not eat spicy vegetables (onions, peppers, radishes, radishes);
- Fresh baked goods and any fats of confectionery origin;
- Sour fruits;
- Chocolate;
- Hot strong coffee and tea;
- Any carbonated drinks;
- Alcohol in any form is strictly prohibited if you have hepatitis C.
A patient with hepatitis C is strictly prohibited from eating all these foods.
What can a patient with hepatitis C eat? Despite the large number of forbidden foods, the diet of a patient with hepatitis C can be quite varied and, importantly, tasty. Thus, the menu of a patient with hepatitis C may include the following products:
- Milk and dairy products are low-fat;
- Hard cheese (mild and low-fat);
- You can eat lean meats and fish;
- Any cereals and porridges with water or milk;
- Fruits and vegetables, fresh or boiled (stewed, blanched, baked);
- You can eat nuts, seeds, dried fruits;
- Herbal decoctions, green tea, compotes, jelly, water;
- Yesterday's baked goods;
- Marmalade, jelly, mousse, caramels.
What should the diet be like during an exacerbation of hepatitis C?
During the period of relapse, a patient with hepatitis C is completely transferred to a strict diet - table 5a. Recipes for dishes with this diet imply cooking only by steaming or by baking/boiling. With such a gentle diet, the ratio of proteins, fats and carbohydrates should be: 80/70/350. At the same time, the calorie content of the total daily diet must be reduced from 3100 to 2300-2500.
The menu of a patient with acute hepatitis C should consist of the following dishes:
- White crackers;
- Vegetable light soups;
- You can eat ground porridge;
- Puréed lean meats or poultry;
- Grinded cottage cheese with sugar;
- You can boil grated vegetables;
- Freshly squeezed fruit juice diluted with a little water;
- Rose hip decoction;
- Compote or jelly;
- Tea, water.
Diet number 5a involves recipes for preparing dishes with thorough grinding. This will ensure a mechanical and chemical sparing regime for all organs of the gastrointestinal tract of a patient with hepatitis C for the period of treatment. It is worth remembering that fasting during acute hepatitis C is not recommended at all.
Diet during rehabilitation after hepatitis C
Useful video about hepatitis C
Gastroenterologists in your city
Select city:
According to WHO, there are 150 million people worldwide suffering from chronic hepatitis C (HCV), and every year another 3-4 million people become infected with the virus. Although this disease is a sluggish pathological process, it still leads to liver failure and death. Every year, 350 thousand people with HCV infection die from liver diseases associated with the virus. Therefore, the task of doctors and patients is to delay the death as much as possible, because the effectiveness of expensive antiviral therapy has not yet been proven.
Features of diet No. 5
Gradually, liver cells restore their function. Therefore, doctors will allow patients with toxic hepatitis more and more familiar foods. The menu should remain balanced in proteins and carbohydrates, but with a minimum amount of animal fats.
So, you should prepare pureed soups every day - vegetable, fish, fruit, but with low-fat broth, second broth, or without meat at all. Dressing with sauteed vegetables for soups is prohibited. Second courses of beef, ham, as well as fish - pike perch, bream or cod, hake are already acceptable. They are cooked in a double boiler or baked in the oven.
Dishes made from cottage cheese are allowed - casseroles, soufflés, as well as cheesecakes and even lazy dumplings. Cheese can be consumed, but not the spicy varieties. Not only porridges are prepared from vermicelli or pasta, but also soups and puddings. From eggs - steam omelettes. They are included in the menu whole, for example, after cooking, but not more than 1-2 pieces. in Week.
For baked goods, it is still better to give preference to day-old bread and crackers, but sometimes you can afford a bun or cheesecake. Almost all vegetables are allowed, but after heat treatment and chopping - as a main dish or side dish. To improve the taste of dishes, use dill, parsley or bay leaves. Among sweets, honey, marmalade or marshmallow, and berry jelly can be included in the diet.
Forecast
In general, with timely diagnosis and proper treatment, the prognosis is favorable. The liver has an exceptional ability to regenerate and easily restores up to 75% of dead cells.
An unfavorable outcome may result from acute injury from a large dose of poison and a delay in medical care (for example, the venom of the toadstool causes the first signs of poisoning to appear after the liver has been exposed to it).
Chronic toxic hepatitis can be complicated by cirrhosis of the liver - the replacement of functional hepatocyte cells with scar tissue. As a rule, this occurs as a result of constant exposure to toxins on the liver, when the poison prevents the cells from recovering normally, for example, when drinking alcohol.
Toxic hepatitis is a non-contagious liver disease that occurs as a result of poisoning the body with chemicals: alcohol, drugs, plant poisons and industrial toxins. The disease is accompanied by pain in the right hypochondrium, nausea, indigestion, and fever. When treating toxic hepatitis, it is important to exclude exposure to a destructive factor, quickly remove the poison from the body and create favorable conditions for liver restoration. To do this, take hepatoprotective medications and follow a gentle diet.
Causes of the disease
There are many ways for poisons to enter the human body:
- Random.
- Professional. When working in hazardous industries.
- Deliberate.
The routes of poisoning are varied.
- Through the digestive system. Eating toxins.
- Through the respiratory system. Inhalation of toxic fumes.
- Possible absorption through the skin.
Regardless of how they enter the body, all these harmful substances ultimately end up in the liver, destroying it.
Toxins differ in their origin:
- Medicines. Even in small, medicinal doses, medications, in addition to their positive effect, negatively affect the functioning of many organs. When the recommended dosage is exceeded, the consequences can be simply devastating.
Under their influence, accumulation of fat cells in the liver, formation of foci of inflammation, death of hepatocytes and proliferation of connective tissue can occur.
- Industrial poisons. Route of entry is through the skin or respiratory tract. Substances such as phosphorus, arsenic, pesticides, aldehydes and many others cause toxic hepatitis in a person who comes into contact with them without personal protective equipment.
- Alcohol. Uncontrolled drinking of alcoholic beverages has a destructive effect on the human liver. The entire alcohol-containing solution taken can be absorbed into the blood and flow through it to the liver cells. There, ethyl alcohol is converted into acetaldehyde, which disrupts cell metabolism, causing toxic hepatitis.
- Poisons of plant origin. Their hepatotropic effect causes acute hepatitis.
Stages
| Latent period | It begins with the entry of toxic substances into the body and continues until symptoms appear. |
| Stage of acute clinical manifestations | The following signs of toxic liver damage appear: jaundice, fever, weight loss, weakness and loss of appetite, dyspeptic disorders. At this stage, damage to vital organs is typical. |
| Exit stage | This is the interval from the most developed clinical picture to recovery or death. |
Diet for chronic hepatitis
Main characteristics:
- Energy value - from 2400 to 2900 kilocalories.
- Avoid eating foods containing purines and oxalic acid.
- Limit the amount of salt to two teaspoons.
- Avoiding foods rich in coarse fiber and also stimulating the secretion of gastric juices.
The bulk of the fat should come from vegetable oil, sesame, olive and pumpkin oil are especially valuable for the liver.
A little butter is also allowed. Particular attention should be paid to proteins that contain lipotropic substances. They are responsible for improving cholesterol metabolism in the body and preventing liver infiltration
Lipotropics are found in dairy products, lean beef, fish, and eggs. The norm of easily digestible carbohydrates should be 80 g per day. This can be sweet fruits, sugar and all sugar-containing products. Although it would be healthier to replace sugar with honey. The list of recommended and prohibited foods is similar to diet No. 5a, but with the removal of the restriction on eating exclusively ground or boiled food.
Complications
A mild form of the disease can be treated quite easily. As for more severe and advanced forms, hepatitis can cause the following complications:
- liver failure, which disrupts the normal functioning of this organ;
- damage to the central nervous system, which leads to periodic convulsions and loss of consciousness;
- cirrhosis of the liver, which most often leads to death.
Complications of the disease lead to very serious consequences. Therefore, it is very important to stop the destructive effect on the liver in time.
- Efficacy: therapeutic effect after a week
- Terms: 6 months or more
- Cost of food: 1400-1450 rubles per week
Development of pathology
Chlorinated hydrocarbons enter the body:
- by contact (through the skin);
- when inhaled;
- when consumed internally.
Once in the blood, they reach the liver and first of all destroy its enzymes - substances without which the processes of neutralization in the liver, as well as metabolism in its cells, cannot take place.
Biphenyls and chlorinated naphthalenes enter the liver in the same way, their effect on it is similar, in addition, these substances destroy hepatocytes (liver cells).
Benzene and derivatives enter the circulatory system and then enter the liver:
- by contact (in case of contact with the skin and mucous membranes);
- when taken orally.
Metalloids and metals bind certain chemical elements that are important for the functioning of the liver - in practical terms, this means that they also block the production, activation and action of liver enzymes.
Insecticides enter the body through the skin and through inhalation. They have a detrimental effect on both the liver enzyme system and hepatocytes, destroying their cells and intercellular connections.
Natural hepatotropic poisons are mainly acquired by ingestion (for example, by eating poisonous mushrooms). Their effect on the liver has not been fully studied, since the patient often dies, and it is not possible to study the entire cycle of liver disorders.
The effect of drugs on the liver is very different - from the destruction of intracellular elements to blocking the main functions of the liver.
note
Toxic hepatitis is only one manifestation of the toxic effect of a number of substances on the liver.