Symptoms of Marshall syndrome
The clinical picture consists of febrile episodes that recur every 2-12 weeks (average cycle 28 days). The temperature often rises suddenly, the fever reaches high numbers (from 40 to 41°C). Sometimes a day before the temperature rises, general weakness, asthenia, and loss of appetite appear. Then aphthous stomatitis occurs, in which small (up to 5 mm) ulcerative lesions of the oral mucosa – aphthae – appear. Pharyngitis is characterized by sore throat, hyperemia of the pharyngeal mucosa. In typical cases, cervical lymphadenitis develops - the lymph nodes in the neck area enlarge and become painful on palpation.
In 43-48% of cases, symptoms occur all together, the most common is stomatitis (55%). It is extremely rare for patients to experience headaches, nausea, vomiting, or bloating. On days 4-5, body temperature returns to normal and inflammation resolves. The intervals between attacks range from 2 to 7 weeks. Over time, the intervals between attacks may lengthen. A peculiarity of the course of fever is that at a temperature of 40°C the general health of children remains relatively satisfactory. Between episodes, appetite is restored and lost body weight is regained. Growth and general psycho-emotional development do not suffer. The course of the disease is benign, and attacks usually stop by adolescence. The description of the onset of Marshall syndrome in adulthood makes it relevant not only for pediatrics.
What is Raynaud's disease?
Raynaud's disease is a condition in which the blood supply to the arms and legs is obstructed. It occurs when the blood vessels in the fingers and toes narrow in response to cold or psycho-emotional stress (such manifestations are called a vasospastic attack). Restricting blood supply to the extremities to maintain body temperature/vital organs is a normal response of the body to extreme cold. However, Raynaud's disease is characterized by a lack of blood flow to the fingers and toes, even after relatively short-term/minor exposure to cold such as holding a glass of ice water or being in an air-conditioned room. Most often, manifestations of this condition affect the fingers, toes, hands themselves, feet, lips and tongue. They develop a painful sensation of cold, tingling or numbness, and the skin may become pale or turn blue. The same reaction can occur as a result of severe stress or anxiety.
Raynaud's syndrome can develop independently. This type of disease is classified as primary. Most patients experience this type of disease. It can occur at any age, but, as a rule, its development begins before the age of 30. The pathology is more common among people living in cold climates. Women have a higher risk of primary Raynaud's disease compared to men.
Secondary Raynaud's syndrome is less common but is often associated with complications and acute manifestations. It is combined with other pathologies, such as lupus or scleroderma. In addition, its development may be triggered by taking certain medications - for example, during chemotherapy - or working with vibrating tools such as a jackhammer, which can injure the hands or wrists.
Diagnostics
It is quite difficult to diagnose this pathology due to vague symptoms and the absence of a pathogen. Only after several attacks of the same type may a doctor suspect a pathology of an autoimmune nature. To make a diagnosis, the following diagnostic methods are used:
- Anamnesis collection. This plays a primary role in diagnosing the disease. The doctor listens carefully to the parents of the sick child, finding out how long ago the attacks began and the nature of their course. In the event that parents can accurately determine the onset of a subsequent attack, Marshall syndrome can be suspected. In addition, the specialist observes the child in the periods between attacks. Usually at this time the general condition of children is not disturbed and they develop normally.
- Inspection data. During the period of exacerbation of the disease, the doctor carefully examines the child. During the examination, inflammation of the oral mucosa, ulcers on the tonsils, stomatitis and enlarged lymph nodes are revealed.
- Clinical blood test. To clarify the picture, the sick child is sent for a blood test. If the number of leukocytes is greatly increased and the ESR is increased, then we can talk about an inflammatory process in the body.
Marshall syndrome is not diagnosed based on any specific criteria. You can talk about this disease only with periodically recurring attacks.
At the initial stage, autoinflammatory disease is often confused with chronic tonsillitis. This disease is also accompanied by fever, enlarged lymph nodes and ulcers on the tonsils. It is possible to differentiate these pathologies only after time, when the cyclical nature of attacks appears.
If the diagnosis is in doubt, the doctor may recommend genetic testing. More recently, the gene for the disease was identified and this gene can mutate.
For what reasons does pathology occur?
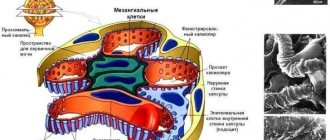
Scientists have found that Hunter disease is associated with a mutation in the IDS (iduronate sulfatase) gene. This gene encodes the lysosomal enzyme iduronate-2-sulfatase. Scientists have identified about 150 different types of mutations of this gene. Due to the connection of the gene with the X chromosome, the disease affects exclusively the stronger sex.
Women can act as carriers of the disease in question, but there is still evidence of several representatives of the fair sex suffering from Hunter syndrome. Doctors linked these cases to a new mutation. There may also be a decrease in normal chromosome activity.
Causes
Even with modern developments in medicine, Marshall syndrome has not been studied properly. The causes of this pathology have not yet been precisely determined, so it is almost impossible to prevent the disease.
With this disease, the child’s body temperature periodically rises to 40 degrees, fever and inflammation of the pharynx, tonsils and oral cavity are observed. The disease manifests itself periodically and a person can say exactly when the next attack will occur. However, it is not possible to prevent such attacks, since doctors resort only to symptomatic treatment. Any therapy prescribed for Marshall syndrome is aimed at relieving the symptoms of the disease, but is not able to prevent subsequent attacks.
There is an assumption that the disease occurs due to certain autoimmune disorders.
Although the causes of this pathology are still unknown, doctors identify several factors that may contribute to the development of the disease.
Latent infection
Hidden viral infection. There is a whole list of latent viral infections that do not manifest themselves for a long time. Such viruses penetrate the body and accumulate in particularly sensitive organs. But these infections usually do not appear periodically, since the development of the disease is provoked by reduced immunity or unfavorable environmental conditions.
Similar viral infections include herpes. Many people are carriers of this virus, but the disease manifests itself only under certain conditions. Provoking factors can be hypothermia, decreased immunity or another infection.
Chronic tonsillitis
Young children often suffer from sore throat. If not treated properly, the disease quickly becomes chronic. The bacteria that inhabit the tonsils of a sick child release many toxic substances that lead to intoxication of the body. High temperature, inflammation of the mucous membranes and fever may be the immune system's response to inflammation.
Exacerbations of chronic tonsillitis in preschool children are sometimes very difficult. There is a high temperature, stomatitis and purulent plaque on the tonsils.
Malfunction of the autoimmune system
The most likely cause of Marshall syndrome in children is called autoimmune failure. Diseases of this group can be blocked for some time, but cannot be cured. In this case, the immune system, for unknown reasons, begins to perceive its cells as foreign and fights against them. This leads to a persistent increase in temperature and severe inflammation. Interestingly, there are no visible reasons for such a reaction of the body.
What is Mikulicz syndrome?
Mikulicz syndrome (disease) is a chronic disorder characterized by abnormally enlarged glands in the head and neck, including near the ears (parotid glands) and around the eyes (tear glands) and mouth (salivary glands). The tonsils and other glands in the soft tissues of the face and neck may also be involved. Although Mikulicz's disease is almost always described as a benign condition, it always occurs in association with another underlying disorder, such as tuberculosis, leukemia, syphilis, Hodgkin's lymphoma, lymphosarcoma (non-Hodgkin's lymphoma), Sjögren's syndrome, or lupus erythematosus (SLE). People with Mikulicz syndrome are at increased risk of developing lymphomas.
Some people with Mikulicz syndrome may experience recurring fevers. Fever may be accompanied by dry eyes, decreased watery eyes, and inflammation of various parts of the eyes (uveitis). Classic signs are enlarged lacrimal gland, enlarged parotid gland, dry mouth, and dry eyes.
The exact cause of Mikulicz syndrome is not known. Some scientists believe that Mikulicz's disease should be considered a form of Sjögren's syndrome.
General information about pathology
Marshall's syndrome has not been sufficiently studied to date.
Periods of illness alternate with periods of health, during which there are no significant symptoms and children do not lag behind in development.
The peculiarities of alternation are individual: in some children symptoms appear once every three to four weeks, in others - once every two months.
One of the characteristic signs of pathology, in addition to alternating periods of illness and health, is the lack of response to antibiotics, therefore other drugs are used to treat the disease.
Most often, Marshall syndrome is detected in children two to five years old, lasts five to eight years and disappears on its own by adolescence.
How does Tourette's syndrome manifest?
Symptoms of Tourette's syndrome include:
- various involuntary tics. Twitching is observed on the neck, face, and shoulders;
- chaotic and frequent movements of the tongue and lips. Moreover, this may be accompanied by shouting of various words and sounds;
- repetition of individual movements several times, repetition of syllables, words or sounds.
The list shows that the manifestations of the disease are motor (associated with movements) and vocal (associated with sounds). Everything related to movement most often manifests itself from 2 to 8 years of age, and vocal “outbursts” are also characteristic of younger children.
Any tics with this disease are not controlled. These signs of Tourette's syndrome exist as if by themselves - the patient is unable to cope with them. Moreover, in a stressful situation, such reactions intensify, become more pronounced, vivid and frequent. In conditions of complete peace and relaxation, tics are much less disturbing.
Treatment
Marshall syndrome is always treated symptomatically. Any treatment for this pathology is aimed at eliminating all symptoms, but not at preventing the next attack. Treatment with anti-inflammatory and antipyretic drugs rarely has an effect; more often, such therapy leads to relapse of the disease. The following medications can be used in treatment:
- Antibiotics. They are often prescribed at the very beginning of the disease, when there is a suspicion of the infectious nature of the pathology. In Marshall's disease, treatment with antibiotics has no effect.
- Antipyretic drugs. Medicines based on paracetamol have no effect. They can lower the temperature a little for just a couple of hours. With this autoimmune disease, it is more advisable to give the child drugs based on ibuprofen.
- Hormonal drugs. Prednisolone is considered a fairly effective anti-inflammatory drug for recurrent syndrome. This hormone is a synthetic analogue of the adrenal hormone and is involved in many metabolic processes that occur in the body. It is Prednisolone that helps reduce the time of attacks to 2-3 days.
There is an opinion that hormonal drugs help not only reduce the time of attacks, but also significantly reduce the period of remission. In this case, each subsequent attack begins earlier.
If the disease is complicated by hypertrophy of the tonsils, the doctor may recommend removing them. This is necessary in order to normalize nasal breathing in the child. Tonsillectomy cannot cure autoimmune pathology, but it can reduce the likelihood of complications. Removal of tonsils is resorted to only as a last resort; with properly selected therapy, such an operation can be avoided.
Constantly enlarged tonsils lead to impaired nasal breathing, and the child feels a lack of oxygen. This condition can lead to delays in mental and physical development.
Hunter syndrome: features of pathology
Hunter syndrome is also known as mucopolysaccharidosis type II. Hunter's disease is considered a hereditary pathology, the cause of which lies in a lack of enzymes. The disease often manifests itself in representatives of the stronger sex.
Let's look at what this genetic disorder is. Hunter syndrome is characterized by disorders of the musculoskeletal system, growth retardation, damage to the respiratory system, and cardiovascular system. The appearance of hereditary pathology is considered to be a consequence of the lack/absolute absence of iduronate-2-sulfatase. In this case, incomplete destruction and accumulation of glycosaminoglycans inside the tissues are observed. When such a rare pathology is diagnosed, people are guaranteed therapy, which is paid for from the state budget.
Diagnostics
To make a diagnosis of PFAPA syndrome, the diagnostic criteria proposed by Marshall (1987) are used: regularly recurring fevers from an early age (beginning 2-5 years); the presence of one of the following clinical signs: aphthous stomatitis, cervical lymphadenitis, pharyngitis; completely asymptomatic interval between episodes of fever; normal physical and neuropsychic development of the child; absence of cyclic neutropenia. There are currently no specific tests to diagnose Marshall syndrome. Diagnostic search includes:
- Consultation with a pediatrician, rheumatologist
. A detailed collection of the patient's medical history is carried out: history of the mother's pregnancy and childbirth, heredity, dietary habits, growth, development of the child, past diseases, information on vaccination, presence or absence of contact with infectious patients. The mucous membranes of the cheeks, pharynx, and tonsils are examined; auscultation of the heart, lungs, measurement of blood pressure, pulse; palpation of the abdomen, lymph nodes. - Clinical and biochemical tests
. During the period of fever, a general blood test reveals leukocytosis with an increase in neutrophils and an acceleration of ESR. During the periods between attacks, all inflammatory parameters are normalized. Also, during attacks, the level of C-reactive protein increases, liver enzymes are not changed. A 25-OH blood test can detect vitamin D3-cholecalciferol deficiency. IgG, IgA, IgM, IgD, procalcitonin, antinuclear antibodies, rheumatoid factor remain normal even with an increase in body temperature. - Additional Research
. Culture of discharge from the upper respiratory tract for microflora and sensitivity to antibiotics, culture of urine and blood for sterility (at the height of fever), radiography of the chest organs and paranasal sinuses are performed to exclude the infectious nature of the fever. In Marshall syndrome, no pathological changes are detected in these studies.
How does a syndrome differ from a disease: features and differences
Before answering the question: how does a syndrome differ from a disease? - we must still try to define these two events in the life of a living organism.
Often among the medical community these phenomena are perceived as identical: Down syndrome or disease, Itsenko-Cushing disease or syndrome, Raynaud's disease or syndrome, etc.
In addition, synonymous concepts, such as pathology, disease, disorder, anomaly and others, have very different definitions, reflecting the individual characteristics of these diverse manifestations.
A look into the past
The history of medicine, which began with the first wounds received, tells of numerous controversies surrounding the very concept of disease. Trying to find a universal understanding of this condition, people are trying to find a universal approach in the treatment of various diseases.
What is a disease?
According to experts from the World Health Organization (WHO), a disease is “a disruption of the normal functioning of the body ” and further in the text.
According to medical Wikipedia, it is already somewhat broader - “disturbances in normal functioning, performance, socially useful activities, life expectancy of the body and its ability to adapt.”
In the Great Medical Encyclopedia, the definition of a disease is “life disrupted in its course by damage to the structure and functions of the body.”
Sometimes the disease is considered as a symptom complex, that is, the appearance of several new signs that are unusual for the body.
What is a syndrome?
Different dictionaries also each have their own definition of this phenomenon. According to the Great Medical Encyclopedia, it is “ a stable set of a number of symptoms with a single pathogenesis .” In medical Wikipedia - “a set of symptoms with a common pathogenesis.”
Wikipedia - a set of symptoms with common etiology and pathogenesis. Still, there is more agreement here, i.e.
to describe features unusual for a healthy organism, they use not just a symptom complex, but a list of symptoms united by a single mechanism of occurrence and development into a larger unit.
Down syndrome
What are the similarities between the syndrome and the disease?
From the above it follows that disease is probably a broader concept than syndrome .
From the definitions of disease and syndrome it is clear that both phenomena can be considered as a set (list) of characteristics (symptoms) that are unusual for a healthy organism.
For example, stroke is a disease characterized by the presence of symptoms such as depression of consciousness, weakness in the limbs or lack of movement in them at all, speech impairment, etc.
Acute cerebral insufficiency syndrome (ACI) is characterized by symptoms such as impaired consciousness, impaired motor functions in the limbs, speech impairment up to complete aphasia (lack of speech), etc. As we can see, the similarity of the two concepts is obvious. Why, then, are different phenomena needed by definition, but similar in the presence of a set of characteristics?
What is the difference between a syndrome and a disease?
Let's continue with the example of stroke (disease) and acute cerebral insufficiency (syndrome). Acute cerebral insufficiency syndrome is characterized by a stable set of symptoms, they were listed above. There may also be disturbances in vision and swallowing, but this is always a more or less stable clinical picture.
In case of a stroke, in addition to the symptoms of ACN, there may be signs of respiratory distress, such as increased breathing (tachypnea) or various types of pathological breathing, which leads to impaired ventilation of the lungs and gas exchange in them, respectively, to an imbalance of blood gases (hypoxia, hypercapnia). And this is acute respiratory failure syndrome. In addition, during a stroke there may be signs of unstable hemodynamics, i.e. decreased blood pressure (hypotension), rapid pulse (tachycardia), arrhythmias - this is a syndrome of cardiac failure.
Thus, during a stroke there may be a large number of signs that are not characteristic of a healthy body , but are combined according to the development mechanism into larger units - syndromes: acute cerebral failure, acute respiratory failure, heart failure, etc. At the same time, acute cerebral insufficiency syndrome can develop in other diseases, i.e. The cause of ACN syndrome can be traumatic brain injury, encephalitis, meningitis, brain tumor, etc.
Consequently, the difference between a disease and a syndrome is that a disease is often characterized by the presence of several syndromes (but can also have one), and one or another syndrome can develop in various diseases. Thus, DIC syndrome or disseminated intravascular coagulation syndrome can develop with bleeding, sepsis, severe pneumonia, arterial hypotension, etc.
Today, about 1,500 syndromes . It should be noted that the widespread use of the syndrome approach has led to a simplification of the concept itself. So let’s say “convulsive syndrome” simply means a symptom called “cramp”, “pain syndrome” means the symptom “pain”.
The question arises: why is the so-called needed? a syndromic approach that has entered medical practice, especially at the prehospital stage and in intensive care units.
Probably the reason for this is the time factor, when establishing a nosological diagnosis (essentially establishing the cause of the occurrence of certain symptoms that are not characteristic of a healthy organism - i.e.
disease) is difficult, syndromic diagnosis, being a stage in establishing a nosological diagnosis, with a minimum scope of diagnostics is sufficient to justify pathogenetic treatment.
So, in case of acute abdominal syndrome, the cause of which may be appendicitis, peritonitis, intestinal obstruction, cholecystitis, diseases of the pelvic organs and others, a syndromic diagnosis is sufficient to prescribe surgical treatment.
Source: https://vchemraznica.ru/chem-otlichaetsya-sindrom-ot-bolezni-osobennosti-i-otlichiya/
Marshall syndrome. Symptoms and manifestations
Patients have a distinctive flat, sunken midface with a flattened nasal bridge and a wide space between the eyes (hypertelorism). The cranial vault is thicker than normal. Many patients have calcium deposits in the skull. The frontal sinuses may be absent. Eye defects that occur in patients with Marshall syndrome include: myopia, cataracts, and wide spaces between the eyes. Hearing loss can range from mild to severe, and distorted sounds are caused by nerve damage. Other symptoms and manifestations seen in some patients with Marshall syndrome include: squinting (esotropia), retinal detachment, glaucoma, and the absence of some nasal bones.
Special neurological, neuropsychological examination
Finger agnosia
The examiner covers the patient's eyes and asks him to spread his fingers. Then, lightly touches the patient's fingers. The person must respond by identifying the finger as soon as it is touched.
This examination is performed first with the eyes open to eliminate misunderstandings or lack of vigilance. The test is not performed if the patient has tactile insensitivity.
To diagnose finger agnosia, a false recognition rate of at least 20% is required.
Right-left disorientation
The doctor gives the patient a card with written instructions. For example, “put your left hand to your right ear.” Ask the patient to read it out loud. If he reads incorrectly, the doctor gives instructions orally. It will ask you to follow the instructions.
Dysgraphia
The examiner shows the patient his watch. The person first writes the numbers without saying them out loud. Then the doctor shows the word "SEVEN". After reading, you need to ask the patient to write.
Dyscalculia
The person is given a card with the simple equation “85–27” written on it. They will ask you to write and calculate. Then they ask you to multiply the numbers in your head without writing them down.
As the number of symptoms increases, the responsible brain damage becomes larger.
Specialist for consultation – neurologist
Side symptoms
In addition to the previously mentioned fever, a general depressed state, typical of any serious illness, may also indicate a disease such as Marshall syndrome in children. Diagnosis in children is difficult due to the abundance of symptoms known to science, similar to other colds. Patients may experience weakness and increased aggressiveness. Moreover, very often a child, in addition to a high temperature, experiences tremors, pain in muscles, bones and joints. Many patients also complain of severe headaches with Marshall's disease. The syndrome can also cause abdominal pain, and vomiting is even less common.
Although the symptoms of Marshall syndrome are very similar to those of colds, usually no other signs of infection are detected. Sometimes some children may experience irritation and redness of the mucous membrane of the eye, as well as tearing, coughing, nasal congestion and discharge. Nervous disorders and allergic reactions, as well as other symptoms, were not noticed.
Syncope in humans - classification, causes, prevention and treatment
In modern medicine, the term “fainting” has not been used for a long time. It has been replaced by a new definition - syncope or syncope. Syncope itself is a symptom of poor circulation in the brain. Always appears suddenly. Characterized by temporary or prolonged loss of consciousness, often accompanied by loss of muscle tone, lethargy, and dizziness.
Patients with syncope experience paleness of the skin, weakness, and nausea. A person quickly recovers from syncope. The average duration of the condition is 20–30 seconds. In older people, syncope is accompanied by retrograde amnesia; they may not remember the events that preceded the fainting.
What is syncope?
During fainting , a person does not respond to external stimuli; his pulse and breathing slow down. There is rarely involuntary urination, and there is no tension in the muscles. After syncope there is a headache, weakness, and drowsiness.
Fainting occurs most often in women and children.
The main causes of syncope
The brain needs intense blood circulation. For full functioning, the brain needs 13% of the total blood volume. Often, due to starvation, overwork, illness or stress, the normal functioning of the body's systems is disrupted.
The causes of “oxygen starvation” and fainting are:
- ischemic heart diseases (ischemic attacks);
- cardiovascular diseases;
- low blood glucose (for example, due to diabetes, pregnancy, or fasting);
- poisoning or dehydration of the body;
- arrhythmia or one-time rhythm disturbance;
- neuralgia of the glossopharyngeal nerve;
- VSD (vegetative-vascular dystonia);
- mental illness (including history, neuroses, depression);
- viral diseases;
- high body temperature;
- head injuries and tumors;
- epilepsy, impaired pericardial function;
- hyperventilation of the lungs.
Classification of sycopal conditions
Syncope conditions are divided into several types. They are classified according to the pathophysiological mechanism.
Orthostatic collapse
Fainting occurs if a person is exposed to heat or cold for a long time, during intense physical exertion. , an abnormal reaction occurs . For example, if you suddenly stand up or jump. This type of fainting is caused by pathologies in the heart, multiple system atrophy, side effects of medications, and Parkinson's disease.
Syncope is also caused by a lack of autonomic regulation of the body. They also occur in diabetes mellitus, amyloid neuropathy, as a reaction to alcohol or medications.
This type of syncope is caused by bradycardia , vasodilation as a consequence of hypotension or hypertension. Situational fainting is provoked by pain, unpleasant sharp sounds, coughing, emotions, a tight collar or a sharp turn of the head.
Cardiogenic syncope
In 20% of cases, this type of fainting is caused by pathology in the functioning of the heart muscle. More often this is a violation of conductivity, rhythm, morphological and structural changes of the heart. Pulmonary hypertension, cardiac myxomas, aortic stenosis. The likelihood of fainting increases when the body's need for blood is much greater than what the bloodstream throws out.
Cerebrovascular syncope
Occurs with “steal” syndrome , which is based on blockage or sharp narrowing of the subclavian vein. This syndrome is accompanied by fainting, dysarthria, diplodia and dizziness.
The patient's history of syncope is characterized by frequent arrhythmic breathing , weak pulse, dilated pupils, and low blood pressure. Differentiated diagnosis is carried out simultaneously by neurologists and cardiologists.
Attending physicians pay a lot of attention to clinical symptoms. With a one-time fainting, it is difficult to make a diagnosis. Sometimes fainting is caused by a person’s stress or trauma and is obvious and does not require additional diagnostics.
If a person begins to lose consciousness frequently, and the frequency of fainting is observed, the doctor pays attention to this. The symptoms that accompany syncope are also taken into account. It is important to pay attention to the person’s well-being during and after syncope.
It is recommended to indicate what diseases the patient has suffered previously. Whether the person took medications , the functioning of the respiratory system is additionally analyzed, doctors check the heart, and the functioning of consciousness. The patient is often referred for general examinations and tests: ECG, x-ray of the heart and lungs, blood and urine tests. Additionally, diagnostics are prescribed:
- X-ray of the skull;
- monitor EGE;
- 10-second massage of the carotid sinus;
- encephalography;
- CT.
First aid for fainting
Unfortunately, not everyone knows how to provide first aid for syncope. Therefore, it is important to know the precursors of fainting and protect yourself. And learn to help other people when necessary.
A few minutes before fainting, a person may hear a squeaking or “buzzing” sound in the ears , and see “flies” or “stars” before their eyes. Fainting is often accompanied by severe nausea, dizziness, a feeling of weakness and profuse sweating, sticky cold sweat, and “darkening” in the eyes.
If a person feels any of these symptoms or observes them in another individual, it is recommended:
- lie on a flat surface and raise your legs at an angle of 40–50 degrees;
- remove tight clothing and allow air to flow;
- inhale ammonia;
- massage the area of the temples or dimples above the upper lip.
If a person has already lost consciousness, then the victim should be laid on a flat surface. The head is placed on one side so that the tongue does not sink in and interfere with the act of breathing . It is important to open all windows and doors to allow more oxygen into the room.
It is necessary to clear the space around the patient; if there are many people around, you should ask them to move away. The victim should be freed from narrow, tight clothing, and all buttons should be undone. And call an ambulance.
Since it is unrealistic to understand the cause of fainting and assess the real state of a person’s health “by eye”.
In order for the respiratory and circulatory systems to work normally again, it is necessary to influence the skin receptors. You can rub the shells of your ears, splash your face with cold water, rub your palms or soles, or pat your cheeks.
Treatment and prevention of syncope
Syncope is treated with medication. The doctor prescribes each specific drug after diagnosis and collection of tests , when he determines the cause of loss of consciousness. For example, with hypotension (low blood pressure) syncope is treated with intramuscular injections of Cordiamine 2 ml or Metazone 1%. Sometimes therapy involves injecting 10% caffeine under the skin.
If fainting occurs in people with mental disorders , then psychotropic medications are first prescribed. The course of treatment lasts at least two months. The attending physician then decides whether to treat the syncope in isolation or not.
If fainting is caused by vegetative-vascular dystonia, B vitamins, neotropics and vasoactive substances are prescribed.
Prevention of syncope caused by alcohol, pregnancy, exhaustion or stress includes:
- a thoughtful daily routine with room for rest and relaxation;
- working with a psychologist and undergoing therapy;
- nutrition and diet;
- vitamin therapy;
- walks in the fresh air, physical activity - yoga, Pilates, running.
Fainting may result in hospitalization. Patients who have frequent recurring attacks , have a disruption of the cardiovascular system, undergo therapy in a hospital. Indicators for special treatment are:
- cardiac ischemia;
- negative family analysis;
- fainting caused by arrhythmia;
- trauma after fainting (during a fall).
Source: https://psiho.guru/terminy/sinkopalnoe-sostoyanie-prichiny-poyavleniya-vidy-lechenie.html
Differential diagnosis of DiHS/DRESS syndrome
The diagnosis of DiHS/DRESS syndrome depends on the stage of the disease. In her debut it is carried out with:
- viral and bacterial diseases (infectious mononucleosis, measles, rubella, infections caused by enteroviruses, adenoviruses, HHV6, HHV7, EBV, CMV, parvovirus B19, acute febrile phase of HIV infection, scarlet fever, secondary syphilis, etc.);
- various manifestations of drug hypersensitivity (serum sickness and serum-like syndrome, exudative erythema multiforme and other drug maculopapular exanthemas, with Stevens-Johnson syndrome, drug-induced erythroderma, acute exanthematous pustulosis);
- graft versus host reaction.
At the stage of multiple organ symptoms and high blood eosinophilia, the differential diagnosis must be made with:
- idiopathic hypereosinophilic syndrome;
- Charge-Ostrich vasculitis;
- lymphomas.
Tourette's syndrome: questions and answers
Why is the syndrome called that?
It got its name in honor of Gilles de la Tourette. This physician published a major report on 9 patients with this syndrome in 1885.
Who is more likely to suffer from Tourette's syndrome?
Symptoms of Tourette's syndrome are more common in men - 3-4 times more often than in women (according to various sources). Also, the syndrome is more common in children - half of the patients get rid of it (spontaneously) by the age of 18.
How dangerous is Tourette's syndrome?
There is no direct danger to the life and health of the patient or others. It all comes down to the fact that due to awkwardness and difficulty in communication, the sick person begins to withdraw into himself and avoid people. Psychotherapy and competent treatment help resolve this issue.
With the right approach and timely treatment, Tourette syndrome allows you to live quite fully and without any problems. But to make an accurate diagnosis and exclude other, more dangerous problems, consultation with a psychotherapist and neurologist is required.
Diagnostic tests
Determination of Leigh syndrome is not carried out on an outpatient basis; the patient is placed in a hospital. The initial stage is to differentiate the disease from pathologies with a similar clinical picture:
- encephalomyelitis;
- amaurotic idiocy;
- infectious-allergic origin;
- myoclonus-epilepsy;
- leukodystrophies.
During a visual examination, attention is paid to neurological manifestations:
- tremor of the upper and lower extremities;
- developmental delay;
- lack of body weight;
- fasciculation of the tongue muscles.
Diagnosis includes an informative study of the hereditary factor if the disease has an autosomal recessive form. When genes are mutated, it is impossible to determine the transmission of pathology from mother to child. In this case, molecular analysis is recommended.
Further activities are carried out using special equipment:
- Using magnetic resonance imaging in FLAIR and T2 in these modes, damage to the medulla oblongata, thalamus, and basal ganglia, which are especially sensitive to hypoxia, is detected. The violations are symmetrical. In some cases, there is an abnormal change in the white matter of the hemispheres due to a cystic neoplasm.
- Molecular diagnostics are used to identify the type of mutation of the SURF1 and BCS1L gene.
- Electrocardiography.
- Fundus ophthalmoscopy.
- Electroneuromyography shows the destruction of myelin in the white matter of the peripheral nervous system (demyelination) due to a decrease in the speed of impulses. The ECG shows a predominance of slow wave activity.
CSF is collected to determine protein levels and lymphocytic pleocytosis. A biochemical blood test reveals a high level of ketone bodies, which indicates the presence of lactic acidosis.
How does Tourette's syndrome occur, is there any treatment?
It is impossible to completely cure the disease with the help of specific programs, but often it can disappear on its own. For example, this happens during puberty. If Tourette's syndrome persists with age, it often duplicates various mental disorders such as panic attacks. This syndrome does not have life-threatening consequences, but it worsens the patient’s quality of life, if only for the reason that the patient feels awkward and cannot communicate with others like an ordinary person.
Treatment of Tourette's syndrome involves smoothing out severe symptoms and improving the patient's quality of life.