A blurred figure is a problem that is easy or difficult, but can be eliminated with desire, supported by willpower. It’s another matter when fat attacked the liver, but this did not affect the weight in any way. A dangerous disease called fatty hepatosis, when neglected, leads to irreversible, sometimes unexpected consequences. It does not manifest itself immediately, which is why precious time for the patient is lost. Let's consider the causes and treatment of fatty liver, possible complications, and preventive measures.
What is fatty liver
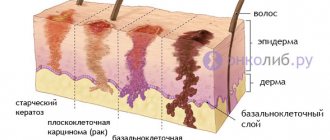
According to WHO, this is one of the most common lifestyle-related liver diseases in the world. The essence is the abnormal accumulation of large vacuoles filled with lipids by hepatocytes (liver cells), an increase in their size, the appearance of collagen fibers, and the development of inflammation.
According to the morphological criterion, we can speak of liver steatosis if fats make up 1/10 of the dry residue of the gland. The course of the disease is so asymptomatic that it is difficult for the patient to believe in the existence of a problem. Although the consequences of the condition can be quite serious, including myocardial infarction or diabetes mellitus.
The pathogenesis of the disease has not been sufficiently studied. But in 2/3 of patients it is associated with alcohol abuse. Politicians, businessmen and other categories of the population suffer from fatty liver, for whom a glass of cognac is a means of relieving stress or an attribute of numerous business meetings. The next morning they do not complain about their health, but they also do not suspect that this lifestyle negatively affects the condition of the gland.
A person's relationship with alcohol depends on specific factors. Alcohol destroys hepatocytes faster in women with their constantly changing hormonal levels. Among Mongoloids, the breakdown products of ethanol are neutralized less actively than among representatives of the European race. With concomitant pathologies, the liver becomes sensitive to alcoholic beverages.
https://www.youtube.com/watch?v=XotGAQ5Yc0o
It is responsible for the breakdown of fatty acids (FA) and replenishing the body with energy. Ethyl alcohol destroys the membranes of hepatocytes, as well as enzymes that transport and break down fatty acids, as a result of which they are not utilized, but accumulate. A weekly dose of 350 ml of vodka for men and 2 times less for women already threatens the liver with problems.
No less dangerous is excess weight, caused by dense brown fat, which is difficult to fight. It produces hormones that inhibit the breakdown of carbohydrates and lipids. The favorite place for their accumulation is the anterior abdominal wall. This form of obesity is called a “beer belly.” Other causes of the condition include:
- Metabolic disorders.
- Physical inactivity.
- Poisoning with poisonous mushrooms, petroleum products, industrial pesticides, phosphorus.
- Genetic predisposition and food preferences leading to increased levels of certain FA fractions in the blood.
- Surgical intervention on the gastrointestinal tract.
- Taking certain medications (Fluconazole, estrogens, glucocorticoids).
Factors contributing to liver steatosis also include hypervitaminosis A and chronic dysbiosis.
Causes of hepatosis
Scientists and doctors still cannot definitively answer the question of what causes fatty liver. But several reasons should be highlighted:
- Increased cholesterol levels in the blood.
- Poor nutrition.
- Weak immunity.
- The disease is very common in patients with diabetes, especially in older people.
- Excess weight can also cause illness.
- Lack of protein in the body.
- Hormonal drugs.
- Long-term use of antibiotics.
- Endocrine disorders.
- Excess carbohydrate content in the body.
- Long-term strict diet or fasting. In this case, the body receives a lot of stress and begins to accumulate fat reserves.
- Gastrointestinal diseases. Pancreatitis goes hand in hand with hepatosis. This should be associated with a deficiency of an enzyme that promotes the breakdown of fats.
- Genetic predisposition.
- Bad habits, in particular alcoholism.
Is the condition dangerous?
A hepatocyte containing an excess amount of fat has other characteristics that are not characteristic of it. Its sensitivity to insulin decreases. Glucose, which normally feeds the liver, loses this ability without the hormone. The organ “starves” and requests additional amounts of sugars. The pancreas produces increasingly larger volumes of secretions. Upon reaching a certain critical level, they still “open the doors” to the liver cells and give them energy. But the consequence of compensatory hyperinsulinemia is diabetes mellitus.
Why does fatty liver occur?
Among the risk factors for fatty liver, the following should be noted:
- alcohol abuse. Unfortunately, it is the most significant for our compatriots;
- unfavorable genetic predisposition;
- overweight and obesity;
- excess iron;
- diabetes
- poor nutrition;
- viral hepatitis;
- fast pace of weight loss;
- malnutrition;
- effect of toxic substances on the liver.
Symptoms of fatty liver
Signs of hepatosis appear gradually:
- At the initial stage, the disease has an inconspicuous course. Small inclusions of lipids can be judged only by analyzing liver transaminases.
- Fat deposits increase. In the morning, a person feels slightly nauseous and there is a bitterness in the mouth. Physical effort causes pain in the right side, which is already a sign of impaired motor activity of the biliary tract.
- Connective tissue replaces most of the liver. Palpation reveals its increase. Ultrasound shows the heterogeneity of the organ.
- Numerous fatty cysts cause complete dysfunction of the gland. A person suffers from a dull aching pain in the right side, constant flatulence, and bowel disorders. Cirrhosis is not far off.
Laboratory tests and instrumental examination are required for a final diagnosis.
Diagnostics
Fatty liver disease is often discovered incidentally. A patient who comes in with pain in the heart is suddenly told about a disorder in the structure and function of the gland. The doctor collects medical history data, asks about the regularity and doses of alcohol taken, and about concomitant diseases. Afterwards, a physical examination of the patient is carried out, the sizes of the spleen and liver are determined.
You can learn about indirect signs of fatty hepatosis and changes characteristic of cirrhosis using ultrasound. Modern devices make it possible to assess which tissue is more abundant in the gland: normal or degenerated. Ultrasound compression elastography determines the risk of cirrhosis and the prognosis of its development.
Blood biochemistry reveals inflammation and impaired bile metabolism. A test for hepatitis viruses is prescribed. Special indications require additional examination for immunological parameters, CT scanning and biopsy.
Establishing diagnosis
As a rule, making a diagnosis of fatty hepatosis with the modern development of imaging diagnostic methods (ultrasound, magnetic resonance and computed tomography) does not present any particular difficulties, especially taking into account the anamnesis and clinical picture. Typically, a needle biopsy of the liver is not performed specifically to diagnose liver obesity. It can be performed for other reasons, for example, if hepatocellular cancer is suspected, or for various forms of chronic hepatitis, but fatty hepatosis in this case can be identified as a concomitant diagnosis.
How to treat fatty liver
Therapeutic measures begin with eliminating the factor that provoked the disease. With ethyl alcohol this is always possible. If there is an addiction to alcohol, a narcologist is involved in treatment. Patients are prescribed a diet, and physical activity in the fresh air is recommended. If this is not enough, the hepatologist prescribes medications that normalize lipid metabolism in the body.
Medicines
There is no specific therapy for hepatic steatosis. The regimen is selected to eliminate factors contributing to gland dystrophy, correct metabolic processes, and improve the restoration and detoxification of hepatocytes.
The doctor prescribes medications with antioxidant and membrane-stabilizing properties. Among them is a group of sulfoamino acids and phospholipids designed to protect the liver:
- Phosphogliv.
- Essliver forte.
- Essentiale.
- Dibikor.
- Heptral.
An effective cure for fatty liver is the drug Hofitol based on artichoke leaf extract. Has choleretic properties. Vitamins from its composition normalize metabolism.
Taurine also deserves attention, providing stabilization of plasma membranes and dissolution of fatty acids, increasing blood flow in the liver. It also has antioxidant, antisclerotic and hypotensive effects.
Treatment
Treatment of hepatosis includes not only taking special medications, but also following a diet to reduce the percentage of fatty tissue in the body. Treatment of fatty liver involves eliminating factors that contribute to the accumulation of fatty tissue.
Also, treatment of the disease involves increasing physical activity, which must be combined with dietary nutrition. At stages 3 and 4 of fatty hepatosis, mandatory medication is required.
Medicines to treat the disease must be prescribed by a doctor. Basic treatment includes the following drugs:
- preparations containing essential phospholipids: “Essentiale Forte”, “Essliver”, “Phosphogliv”, “Fosphonciale”;
- medications containing amino acids: Hepa-Merz, Glutargin;
- drugs – hepatoprotectors: “Heptral”, “Geptor”;
- medicines containing herbal ingredients: “Karsil”, “Gepabene”, “Legalon”;
- medications that improve blood viscosity: “Curantil”, “Trental”;
- preparations based on alpha-lipoic acids: Dialipon, Berlition;
- choleretic drugs: “Holosas”, “Allohol”;
- B vitamins;
- Milk thistle tablets.
Treatment of fatty liver is accompanied by physiotherapy.
Taking medications for hepatosis is indicated only as prescribed by a doctor. Treatment also takes place under the supervision of a specialist to monitor the effectiveness of the treatment.
From the very beginning, the treatment of fatty liver will consist of getting rid of all the causes that preceded the disease, be it another disease that accompanied hepatosis, or some other factor.
The main rule for treating any liver disease is strict adherence to dietary nutrition. Fatty hepatosis requires therapeutic diet No. 5, which is followed for about 2 years. Gradually, the menu can be expanded by adding other products to the menu with the doctor’s permission.
The complex treatment of the disease also includes drug therapy, with the help of which the functionality of the liver and bile ducts is restored. In the treatment of fatty liver, hepatoprotectors (medicines that have a positive effect on liver function) are widely used. These may be drugs such as:
- Essentiale;
- Rezalut;
- Ursosan.
The specific medicine and duration of its use must be prescribed by a doctor, but most often the course will last at least 2 months. There is also the possibility that the pills will need to be taken for life for preventive purposes.
Treatment for fatty liver does not involve any hospitalization or cessation of physical activity. On the contrary, exercises performed under the supervision of specialists lead to the utilization, or “burning” of fats and a reduction in fatty degeneration. The main principles of therapy are:
- weight loss;
- physical therapy, swimming, moderate increase in physical activity;
- drugs that have the ability to stabilize cell membranes: Heptral, Berlition, drugs, complexes of vitamins, antioxidants.
- ursodeoxycholic acid preparations.
However, despite the possibilities of modern therapy, diet plays a leading role in the treatment of fatty degeneration. Diet for fatty liver - diet No. 5 on the list of diets according to Pevzner, is called “liver” and must meet the following requirements: with a normal ratio of proteins and carbohydrates, the intake of fats is limited:
- Refractory fats (butter, lard), foods containing purines (brains, liver, liver, canned food, smoked meats, sausages), oxalic acid, and cholesterol are excluded.
- Frying food in oil or deep-frying is not allowed.
- There are foods rich in fiber and ballast substances that improve peristalsis and have no energy value: cereals, bran, vegetables and fruits, apples.
- Among lipotropic products, egg whites, low-fat cottage cheese, and boiled sea fish are allowed in limited quantities.
- Bakery products - made from coarse, peeled flour, better than yesterday's baked goods. It is strictly forbidden to eat butter dough and fried pies.
- Almost everything from fermented milk products is possible, the only limitation is the minimum fat content in sour cream, as well as the exclusion of fatty and spicy cheeses.
If you follow the diet, as well as the recommendations of your doctor, increase the level of physical activity and, most importantly, completely stop drinking alcohol, the liver will fully restore its functions and fatty hepatosis will be overcome.
www.infmedserv.ru
The basis of the diagnosis still remains palpation in the area of the right hypochondrium, and then the doctor’s assumptions are supplemented by MRI, CT, angiography, ultrasound, liver enzyme tests, and serological studies to exclude the possibility of viral hepatitis.
This entire process is conducted by a gastroenterologist, so at the first symptoms of the disease, immediately consult a doctor.
Treatment of fatty liver is complex, including both the medication part and a number of preventive measures that the patient must follow:
- Normalize your lifestyle.
- Adhere to diet therapy and vitamin therapy with the inclusion of ascorbic acid.
- Increase physical activity.
- Cleanse the liver by fasting, arranging fasting days.
- Normalize metabolism with fractional nutrition.
- Reduce weight by an average of 2 kg per month.
Medicines for fatty liver
A disease such as fatty liver requires treatment. After all, if you launch it, the consequences will be the saddest.
The treatment process will not be simple and quick even in the initial stages. It is necessary to abandon the previous lifestyle and follow all the doctor’s advice.
First of all, it is necessary to identify the main factor that provokes this disease. Most often this is alcohol, which is prohibited during treatment.
Experts also advise giving up smoking. Some medications can also affect the disease process, so it is worth informing your doctor about all medications you are taking.
During the treatment period, the patient must adhere to a certain diet high in protein. But you should completely avoid fatty and fried foods.
In addition, doctors prescribe a certain set of medications for treatment. These include:
- essential phospholipids – Essentiale Forte, Phosphogliv, Essliver Forte;
- hepaprotectors of plant origin – Karsil and others;
- vitamins of group B, PP, C;
- products containing ursodeoxycholic acid.
To get rid of this disease, you need to take these drugs for at least 2 months. And you may have to do this for the rest of your life to prevent fatty liver.
Obesity on the human body is noticeable to the naked eye, but a fatty liver is much more difficult to identify. You can’t do without the help of a specialist, ultrasound (not always detectable) and magnetic resonance computed tomography.
A fatty liver of 15% of the total weight should be a cause for concern and immediate treatment.
In the treatment of fatty liver, the main emphasis is on eliminating the factor that provokes the disease. The most likely cause is alcohol. Smoking and certain medications are also excluded.
Patients are prescribed diet No. 5, which is dominated by animal proteins, boiled cod, cottage cheese, and porridge - buckwheat and oatmeal. Changing eating behavior towards eliminating fatty foods and overeating. Animal fats are reduced to a minimum.
Medicines of the lipotropic group (acids: folic and lipoic, vitamin B12, hydrolysates and liver extracts).
General recommendations
1. It is necessary to establish proper nutrition. The diet must be developed by a doctor. It should be balanced and gentle.
These should be light soups: cereal, dairy, fruit and vegetable. Boiled meat, sea fish, one chicken egg per day, and fermented milk products are required in the diet.
2. Flour products and baked goods are limited.
3. Honey, cottage cheese, still mineral water are useful.
The main problem with fatty hepatosis is the need to oxidize excess fat and treat hepatitis. Therefore, only qualified assistance from specialists will help avoid serious consequences.
In the case of an unspecified diagnosis or suspicion of fatty hepatosis, consultations with several specialists are necessary: a gastroenterologist, a hepatologist, a surgeon and, possibly, an oncologist.
Treatment with folk remedies is based on the use of herbal preparations, tinctures, decoctions of vegetables and fruits.
narodnymisredstvami.ru
Any treatment must begin with diagnosis. And even more so when it comes to the liver.
After all, the liver plays the role of a kind of filter for the body. Every day the gland pumps up to one hundred liters of blood, cleansing it.
If there is any disturbance in the functioning of the blood, it is not filtered, and other organs become infected and poisoned. Diagnosis is also necessary because the disease does not have clear symptoms at the initial stage.
And with improper treatment, fatty liver will actively develop.
Today, there are a large number of research methods that guarantee maximum reliability. Fatty liver is determined using laboratory and instrumental studies.
The patient must donate blood for a biochemical analysis. After all, only an ultrasound examination cannot always reveal the full picture of liver problems.
Fatty liver can be detected using magnetic resonance imaging.
If the liver has already increased in size, the doctor may suspect fatty hepatosis during a standard medical examination and palpation. In any case, a timely visit to the doctor plays an important role.
This is why it is so important to undergo regular preventive medical examinations. Indeed, in the modern world there are a large number of external factors that affect the liver.
And there is hardly a person who has never been treated with antibiotics in his life. Sometimes even one course is enough for severe consequences.
In order to prescribe the correct treatment for fatty liver, it is important to establish the root cause of this problem and eliminate it. Only then do they restore the normal functioning of the organ.
At the initial stage of fatty hepatosis, it is the elimination of the main factor that will help completely get rid of the disease. So, first of all, it is important to completely stop drinking alcohol, follow a strict diet, and stop taking medications.
The main condition in the treatment of fatty liver is diet. Basically, diet No. 5 is prescribed, which consists of the following menu:
- Vegetable and cereal soups;
- Lean meats, without cartilage and tendons;
- Poultry meat must be skinned;
- Just not fresh bread;
- Biscuits, crackers;
- Low-fat dairy products;
- Any fruit;
- Weak tea or coffee;
- Compote;
- Olive oil for salad dressing.
Any fatty foods or fried foods are strictly contraindicated. Porridge can be consumed exclusively in the form of puddings.
In rare cases, pasta products made exclusively from durum wheat are allowed. But you need to forget about baking and fresh bread for a while.
As for cooking methods, steam, boiled and baked cooking options are allowed. Sometimes you can eat low-fat natural cottage cheese.
With fatty hepatosis, it is very important that the body receives a sufficient amount of protein and calcium. The following products should be completely excluded from the diet: sausages, sausages, semi-finished products, spices, sauces, sugar, animal fat, seasonings, seafood.
Medications
As additional therapy, certain medications are prescribed, which are called hepatoprotectors. They help restore liver cells, which helps quickly overcome obesity.
Complete regeneration of the organ occurs. It is also important to normalize the functioning of the biliary tract.
In the treatment of fatty hepatosis, the following hepatoprotectors are highly effective:
- Resolute;
- Essentiale;
- Ursosan;
- Phosphogliv.
These drugs are essential phospholipids. They are extracted from soybeans, which means they are of completely natural origin. Plant flavonoids are often prescribed. Under their influence, free radicals are completely neutralized. This group is represented by the following medications: Gepabene, Karsil, Silimar, Legalon.
Fatty liver – fatty liver disease – is the accumulation of excess fat in the liver cells. Often this disease acts as a specific reaction to intoxication of the body (for example, from exposure to alcohol). Fatty liver can also be called fatty liver disease or fatty cell degeneration.
The second name reflects the essence of the pathological process: active liver cells are replaced by others filled with fat. The work of the liver as a filter becomes more difficult, in response to which the process of increasing the volume and size of the organ begins.
In addition to intoxication, obesity can be associated with other serious diseases of the body, pregnancy and unnatural processes (for example, starvation).
Treatment of the liver will consist of creating the most comfortable working conditions for this organ through diet, folk remedies and drug therapy.
In the treatment of the disease in question, the main emphasis is on eliminating the influence of the main factor that provoked it. Alcohol in this case is absolutely prohibited. This also applies to smoking and the use of certain medications.
Additionally, diet No. 5 is prescribed, the main components of which are characterized by an increased content of animal proteins in their complete form in combination with products of litiotropic factors, which in particular include boiled cod, cottage cheese, products made from buckwheat and oatmeal, etc.
In general, nutrition requires changing existing habits related to it, limiting the consumption of too fatty foods, and avoiding overeating.
The intake of fats into the body is also limited, which especially applies to fats of animal origin and refractory fats. Preparations of the lipotropic group (folic acid, lipoic acid, vitamin B12, preparations with hydrolysates and liver extracts) are also prescribed separately.
If a fatty liver is suspected, consultation with several specialists is necessary. In particular, this is a gastroenterologist and hepatologist, as well as a surgeon.
Possible complications
The direct consequences of fatty hepatosis include:
- Liver fibrosis, which is characterized by the replacement of hepatocytes with connective tissue, the formation of scars and other unusual elements that replace liver cells.
- Weakening of the immune system, expressed in the body’s inability to resist pathogenic microbes of a viral and bacterial nature.
The final stage of fibrosis is cirrhosis, which affects the external and internal structure of the organ. It is accompanied by multiple immunoinflammatory processes leading to death.
Prevention
To maintain liver health, it is recommended to follow your doctor’s advice:
- To refuse from bad habits.
- Exercise. Include physical activity, for example, half an hour a day on an exercise bike, walking.
- Lead a healthy lifestyle.
- Eat right, excluding baked goods, cakes, and pastries. Eat vegetables, fruits, and cereals rich in fiber.
- Be careful when using various liver cleansing techniques. Before such procedures, it is better to consult a doctor.
- Detect dystrophic processes in the gland in a timely manner, which will avoid serious complications.
Disease prevention
It consists in eliminating factors from life that can provoke the development of the disease. Mandatory preventive measures:
- proper nutrition;
- active lifestyle;
- refusal to drink alcoholic beverages;
- control of blood cholesterol levels in people over 40 years of age.