04.10.2018
Uterine adenocarcinoma is a malignant tumor formed by cells of glandular tissue. It has several stages and classifications and may not show any symptoms for a long time, like most malignant neoplasms. However, as the tumor continues to grow, it can cause bleeding, pain, and other symptoms.
Have you had a full medical check-up in the last 3 years?
Not really
To diagnose adenocarcinoma, ultrasound, hysteroscopy with biopsy, CT and MRI are used. A significant study is the histological examination of the biopsy, on the basis of which the type of tumor is determined. The initial stages respond well to treatment; if the process is advanced, the five-year survival rate is very low. Therefore, for prevention, it is necessary to undergo regular examination by a gynecologist.
Statistics
Adenocarcinoma is the most common type of tumor among other gynecological neoplasms. In terms of incidence among female oncology, it ranks second after breast cancer. Women of mature age have a greater predisposition to this type of tumor, that is, the incidence is higher over the age of 40-45 years.
Although there is currently a tendency towards rejuvenation of adenocarcinoma - according to data among young people, the incidence has increased by 50%.
Main symptoms
Unpleasant signs begin to appear in patients as the tumor spreads to the cervical canal. Women of childbearing age experience abnormal bleeding between cycles or prolonged periods. During menopause - the resumption of menstruation after a long absence.
Other symptoms of adenocarcinoma:
- insomnia;
- aching pain in the lower back, lower abdomen during and after sex;
- causeless increase in temperature;
- nervousness, weakness, irritability;
- spontaneous bleeding in postmenopause.
If at stages 1-2 of adenocarcinoma the signs are weakly expressed and completely absent, then at stage 3 the tumor, as it grows, provokes a malfunction of the pelvic organs. Patients experience periodic aching pain in the abdomen, a feeling of incomplete emptying of the bladder and intestines. At the 4th stage, in the case of metastatic development and manifestations of ascites, signs of damage to the lungs, kidneys, brain, and liver are observed.
An obvious symptom of adenocarcinoma is the discharge of mucus and bloody discharge with an unpleasant odor from the vagina. Intense discharge of varying consistency in postmenopausal women may indicate that the uterine tumor is disintegrating. This is an unfavorable sign and a reason for an urgent visit to a gynecological oncologist.
The clinical picture of the disease manifests itself clearly with the formation of tumor metastases in the lungs, bones, and liver. At an early stage, symptoms may be similar to other cancers. The glandular form of cancer does not make itself known for a long time. Older women turn to doctors late, when there is obvious pain in the sternum, groundless cough, yellowness of the skin, colic in the liver, and pathological fractures. It is extremely important for young patients of childbearing age to monitor their health and well-being, not to ignore the appearance of heavy, prolonged menstruation, aching lower back pain, causeless weight loss, general weakness and malaise, and an enlarged abdomen.
It is most difficult for women after 45 years of age, because irregular bleeding becomes the norm. If the symptoms continue from month to month, then you should see a gynecologist and undergo a full examination.
Causes
The incidence of malignant tumors always does not have a clear etiology. The cause of the tumor is clear - it is a cell mutation. But there are many versions of why it occurs. There is evidence of the influence of certain factors on the process, however, what exactly causes cell degeneration is unknown. The only mechanism of development confirmed by experts is increased estrogen stimulation against the background of decreased progesterone synthesis.
Predisposing factors include:
- Age over 40-45 years . Adenocarcinoma is mostly detected in women of mature age;
- Hereditary predisposition . The connection between the development of pathology and genetic factors has been proven;
- Late onset of menopause, early onset of menstruation . These conditions are directly related to hyperestrogenemia, which causes a tendency to endometrial hyperplasia;
- Lack of sexual activity, childbirth, infertility, lack of ovulation . Not mandatory, but an important factor;
- Polycystic ovary syndrome . With polycystic disease, the production of estrogen precursors increases;
- Hormone-producing tumors . They are the founders of increasing estrogen;
- Obesity . It has been proven that adipose tissue is of no small importance in increasing extragonadal estrogen synthesis;
- Presence of hypertension, diabetes mellitus . Hyperinsulinemia increases the risk of adenocarcinoma, acting indirectly through estrogen;
- Adenomatosis and polyposis . Hyperplastic processes are fundamental in the occurrence of adenocarcinoma, especially atypical ones;
- Taking estrogen medications . Studies have been conducted that have shown that the detection rate of adenocarcinoma in the postmenopausal period increases when taking estrogen hormone replacement therapy.
The importance of hormones in the development of many female diseases cannot be ignored.
It has been proven that with increased estrogen levels, the proliferation of endometrial cells increases and the risk of developing uterine cancer increases. Thus, conditions that provoke hormonal imbalance are considered risk factors. These include obesity, postmenopausal period, PCOS and hormone-producing neoplasms.
The role of endometrial hyperplastic processes in the development of adenocarcinoma also occupies an important place, especially atypical ones, that is, accompanied by dysplasia. Adenomatosis requires special attention, as it is a precancerous condition.
Metabolic disorders also predispose to increased risk. In particular, obesity and diabetes mellitus are often concomitant diseases of adenocarcinoma. Special attention should be paid to obesity, since its role in increased extragonadal estrogen synthesis has been proven.
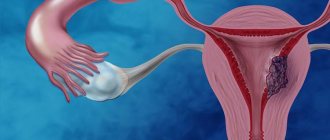
Description of adenocarcinoma
Adenocarcinoma of the uterus is a malignant tumor localized in the tissues of the ovaries and endometrium (mucosal, uterine layer). It is formed from atypical cells of glandular tissue more often in women during the postmenopausal period. At an early stage it proceeds secretly. At stages 2-3, it begins to manifest itself in the form of uncharacteristic bleeding, heavy menstruation, causeless abdominal growth, and lower back pain (when spreading throughout the pelvic organs).
Uterine adenocarcinoma is a hormone-dependent type of cancer in which healthy cells degenerate into abnormal ones. The glandular tissue of the uterine layer proliferates, endometrial cells begin to grow.
Important! The danger of pathological foci in the uterine fundus is its asymptomatic course, which poses difficulties for timely recognition and treatment. In most cases, women turn to doctors late, when the pathological process progresses, metastasizes and there is practically no chance of recovery.
Symptoms
Adenocarcinoma often occurs latently, without causing any symptoms. A woman may not suspect the presence of a tumor for a long time, which to a certain extent worsens the prognosis of the disease.
The clinical picture directly depends on the location, type and stage of the tumor.
An increase in size provokes the development of unfavorable symptoms:
- Abnormal bleeding;
- Prolonged menstruation;
- Pathological discharge;
- Menstrual irregularities;
- Pain in the lower abdomen and lower back, aching or paroxysmal.
It should be noted that symptoms are not specific to adenocarcinoma. Such manifestations can accompany a lot of gynecological diseases, however, if at least one of them appears, you need to be especially vigilant and contact a gynecologist for examination.
At later stages, when the size of the tumor becomes larger, it can invade neighboring organs and spread metastases. During these periods you may experience:
- Abdominal enlargement, ascites;
- Loss of appetite, weight loss, asthenia;
- Temperature increase;
- Urinary disorders;
- Violations of the act of defecation.
The development of such symptoms should not be allowed; you should be examined regularly in order to notice the pathology in time.
Causes
Pathology provokes mutation and uncontrolled division of glandular cells, ultimately forming a malignant tumor that begins to increase in size and invade vital systems (circulatory, lymphatic). Provoking pathogenic factors:
- absence of childbirth, because nulliparous women are at risk;
- suppression of ovulation, causing disruption of the menstrual cycle and hormonal imbalance as a result of low levels of progesterone, high levels of estrogen;
- infertility is a consequence of organic disorders of the reproductive system;
- early menarche (beginning of menstruation before age 12);
- polycystic ovary syndrome with elevated estrogen levels;
- obesity with massive production of estrogen by adipose tissue;
- anovulatory cycles, in which a mature egg is not released in the middle of the cycle;
- benign ovarian tumors;
- hypertension;
- diabetes;
- hereditary predisposition.
It is worth knowing that the likelihood of developing adenocarcinoma increases significantly in premenopausal women after 50 years. A provoking factor may be long-term use of hormonal drugs, work in harmful chemical conditions, radiation exposure, long-term absence of sexual activity, abuse of fast foods and fatty foods, frequent drinking of alcohol, and smoking.
Kinds
There are several classifications of adenocarcinoma. They are based on the location of the tumor, direction of growth, stage of development and degree of differentiation.
Adenocarcinoma of the cervix
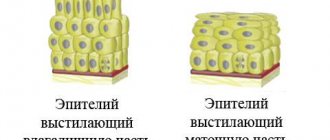
This localization of the tumor may not cause any inconvenience or discomfort. That is, a woman may not be aware of it. Therefore, for timely diagnosis, a special method of screening for cervical cancer, called a PAP test (Papanicolaou smear), has been developed. To do this, the cervical epithelium is taken using a special brush onto a glass slide, fixed and sent to the cytology laboratory. After viewing, the cytologist makes a diagnosis about the presence of atypical cells, the presence and degree of dysplasia. This laboratory method can significantly increase the level of early detection of cervical cancer.
Adenocarcinoma of the uterine body
Uterine adenocarcinoma develops in the body of the uterus. The tumor can affect any part of the uterus, however, the fundus is most often affected. As growth increases, other areas of the uterus, adnexa, and nearby organs may become involved. Diagnosis in this case is based on taking a biopsy and histological examination of the tissue. Pathology most often occurs in women of premenopausal age.
In accordance with the WHO morphological classification, endometrioid and non-endometrioid tumors are distinguished. The second type is rare.
Endometrioid adenocarcinoma
This type of tumor is the most common, accounting for more than 80%. Develops against the background of endometrial hyperplasia and excessive estrogen stimulation. The tumor is represented by tubular glandular structures covered with epithelium. They can be the basis for the development of various neoplasms, differentiated by their structure: tubular, papillary, follicular and cystic. Endometrioid tumors are characterized by a favorable course and positive prognosis. The five-year survival rate with this type of tumor reaches 90%.
Among endometrioid tumors there are:
- Adenocarcinoma (secretory and ciliated cell);
- Adenocarcinoma with squamous differentiation (adenoacanthoma and adenosquamous carcinoma).
Non-endometrioid tumors are rare and account for about 20%. These include: serous papillary cancer, clear cell, mucinous, squamous, mixed and undifferentiated forms of adenocarcinoma.
Diagnostic measures
The main method for recognizing uterine adenocarcinoma is biopsy. A biopsy helps not only determine the type of tumor, but also its degree of malignancy. A biopsy is performed during hysteroscopy: a special flexible sensor is inserted into the body of the uterus - a hysteroscope, which allows you to see the uterine cavity and perform a targeted biopsy of suspicious areas, followed by transfer of the material to histology for study.
The extent of tumor spread can be assessed by:
- MRI;
- CT;
- PET CT (is the most informative method for detecting metastases);
- fluorescent endoscopy by introducing photosensitizers into the uterine cavity to visualize small formations up to 1 mm, followed by examination of the biopsy specimen for histology.
Stages
Depending on the size and degree of involvement of neighboring organs and tissues, several stages of adenocarcinoma are distinguished:
- First stage. The tumor is small, located isolated in the endometrium, without affecting neighboring tissues;
- Second stage. The neoplasm is medium in size, extends to the muscle layer and cervix;
- Third stage. As the tumor grows, it begins to involve the surrounding tissue and appendages; metastases are detected in the pelvis and lymph nodes;
- Fourth stage. Adenocarcinoma is quite large in size and can invade the wall of the intestine and bladder. Distant metastases are observed.
Classification of adenocarcinomas
Endometrial adenocarcinoma is divided into 4 types:
- highly differentiated;
- moderately differentiated;
- poorly differentiated;
- endometrioid adenocarcinoma.
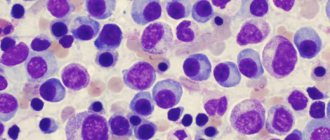
With a highly differentiated type, cancer cells differ little from healthy ones, and, conversely, with low differentiation, pathological cells differ sharply from normal ones, this always indicates the malignancy of the process.
Well-differentiated adenocarcinoma of the uterus - with it, only elongation and enlargement of the nucleus are observed in the affected cells. This makes diagnosis difficult, but this type of tumor is considered more favorable: the myometrium is affected slightly and superficially. Metastases are minimal - no more than 1%.
Moderately differentiated adenocarcinoma of the uterus - this type, developing in the endometrium, can penetrate into the myometrium. Characterized by squamous cellulose. It occurs infrequently, usually against the background of cervical cancer (cervical cancer). Squamous epithelial cells with a moderate form are polymorphic, there are a large number of them, they actively divide and grow. This form is worse in severity; it is often complicated by metastases - 9% of cases. If a woman is under 30 years of age, there will most often be no metastases.
Poorly differentiated adenocarcinoma of the uterus - the number of cancer cells reaches a record number and continues to grow. This is the 3rd degree of pathohistology of uterine cancer, with a severe course, the cells are located in clusters in the form of stripes or individual clusters of irregular shape. Poorly differentiated uterine cancer is characterized by pronounced cell polymorphism and malignancy. The prognosis is extremely unfavorable. Penetration into the myometrium occurs 3-4 times deeper and wider. The growth of metastasis increases in this type by 16-18 times relative to the first 2 forms.
Endometrioid adenocarcinoma of the uterus, or papillary form, is the most common type, accounting for 75% of uterine cancer cases. The tumor contains mucus and has a mucous membrane. Depends on estrogen levels. This form of cancer is distinguished by its cellular diversity: with this tumor, tubular and papillary epithelial cells of a glandular nature appear, which actively divide and are arranged in several layers, which is why the tumor resembles cauliflower. This type of tumor grows superficially into the myometrium, which has a good prognosis.
Be sure to read: Causes of Ewing's sarcoma
Stages of adenocarcinoma:
- The tumor is small. It does not go beyond the mucous membrane. The cure rate is 87% with early diagnosis.
- The tumor begins to occupy the cervical canal, but does not yet affect other organs. The prognosis for successful treatment is 76%.
- Cancer spreads to neighboring organs and lymph nodes. Treatment success is only 63%.
- Complete damage to all body systems and metastasis to distant organs. The recovery rate is only 37%.
Forms of the disease
Based on differentiation, three types of tumors are distinguished. The degree of differentiation indicates the level of difference in cellular structures. The lower it is, the worse the prognosis.
Highly differentiated
There is a small number of atypical cells that are morphologically different from normal tissue cells. Most cells have a normal structure, polymorphism is insignificant.
Moderately differentiated
Cell polymorphism is more pronounced, atypia covers half of the cellular composition. Cell proliferation occurs faster. This tumor is more malignant than the previous type.
Poorly differentiated
Extensive polymorphism, most cells have an atypical structure. Atypia predisposes to increased proliferation, which means rapid growth of adenocarcinoma. Poor differentiation is a sign of a malignant tumor prone to metastasis.
Stages of development
The stages of adenocarcinoma are determined by oncologists according to the FIGO system:
- stage zero - precancerous condition;
- Stage 1 - tumor localization within the uterus;
- Stage 2 with lesions in addition to the cervix and body;
- Stage 3 with tumor growth beyond the borders of the uterus, but without entering the pelvic area;
- Stage 4 (advanced) with growth beyond the pelvis, damage to the bladder and intestines.
The level of malignancy of uterine carcinoma is determined taking into account the degree of tumor differentiation, which will determine the choice of optimal treatment and life prognosis for women.
- The most malignant adenocarcinoma is a poorly differentiated uterine tumor (q3).
- Moderately malignant tumor – q2.
- The least malignant is a well-differentiated uterine tumor (q1).
Diagnostics
The diagnosis is made on the basis of a comprehensive examination, including examination, history taking, laboratory and instrumental studies. In the diagnosis of adenocarcinoma, screening for early detection of pathology is of great importance.
Primary (early) diagnosis includes:
- Ultrasound screening. Uterine sonography is the leading method in screening for uterine cancer and is performed vaginally for complaints of vaginal bleeding. The algorithm for diagnosing abnormal bleeding is based on sonography, the results of which are used to select a further technique. If the thickness of the M-echo is less than 4 mm, dynamic observation is prescribed, 4-12 mm - hysteroscopy with biopsy, more than 12 mm - aspiration biopsy;
- Endoscopic diagnostics. Sonography alone is not a sufficiently informative diagnostic method, so it must be supplemented by other methods. Hysteroscopy of the uterus is performed using a hysteroscope inserted into the vagina. During the procedure, the specialist examines the uterine cavity, notes the presence of hyperplasia and neoplasms, and performs a targeted tissue biopsy for histological examination. This method allows you to increase the reliability and efficiency of diagnostic measures, as it provides visualization of the internal state of the uterus.
- In some cases, CT and MRI are used.
Treatment
Therapy should be comprehensive and include various techniques: medications, radiation and surgery. The attending physician establishes a treatment regimen individually, after a complete examination of the patient. Surgery is advisable in the first two stages; the operation should be carried out in a way that minimizes the risk of possible complications. Radiation and drug therapy are auxiliary methods.
Tactics
The chosen tactics are directly related to the patient’s condition, the type and stage of the detected adenocarcinoma, the degree of malignancy and location. First, the doctor considers the feasibility of the operation and determines the scope of the operation. Then he selects medications and the method of radiation therapy.
Surgical methods and operation
The indication for surgical intervention is the first and second stages of adenocarcinoma. There are hysterectomy (removal of the uterus without appendages) and panhysterectomy (complete removal of the uterus with appendages). The choice of surgical method is determined solely by the attending physician.
Hysterectomy varies in the extent of the operation:
- Supravaginal (partial removal of the uterus, performed if there is a desire to preserve the cervix and the need to reduce the operation time);
- Extirpation (the most common, complete removal of the uterus);
- Wertheim's method (implies removal of the uterus along with the surrounding tissue, part of the vagina, appendages and lymph nodes).
The extent of the operation depends on many related factors: age, health status of the patient, tumor size. Doctors are inclined to believe that it is better to remove appendages during menopause to prevent relapses in the future.
Medicines
Drug therapy includes the use of cytostatics and hormonal drugs to enhance the effect of treatment and prevent complications. Cytostatics are aimed at suppressing tumor proliferation, stopping growth and increasing size.
They are used in combination with surgical and radiation treatment.
Other treatments
An auxiliary treatment method is radiation therapy, carried out in the preoperative and postoperative period. There are external and intracavitary radiation therapy.
- External or external irradiation is effectively used in the treatment of malignant neoplasms. It can be static or dynamic; the radiation source is located at a certain distance from the patient. Can be used alone and in combination with other treatment methods;
- Brachytherapy (intracavitary irradiation). A special applicator is placed near the tumor into which radionuclides are injected. Can be used in combination with the remote method.
Treatment of cervical adenocarcinoma in Israel
In Israeli clinics, doctors take on those cases that are considered hopeless in hospitals in the CIS countries, although there are many doctors there who studied in the Russian Federation, Ukraine and other post-Soviet countries.
ACSM in Israel is treated using the following methods:
- surgical;
- chemoradiation.
Successful treatment of adenocarcinoma in Israeli clinics is due to the fact that operations are performed with the help of robotic surgeons. This minimizes the risk of complications, while the adenocarcinoma is completely removed. If the patient is indicated for surgery, the extent of surgical intervention depends on the stage of the disease. For ACSM it is indicated:
- cryodestruction (rarely prescribed for TisN0M0);
- laser removal of adenocarcinoma;
- electroexcision of the cervix (stage 0-1A);
- high cervical amputation (stage 1A-1B);
- simple hysterectomy with lymphadenectomy (stage 1A–2);
- extended hysterectomy with lymphadenectomy and subsequent chemoradiotherapy (stage 2B-3).
At stage 4 of cancer, the tumor is first reduced and the metastases disappear. For this, therapy is prescribed:
- targeted;
- immunotherapy;
- systemic chemotherapy;
- contact beam.
Oncology centers use gentle chemoradiotherapy. It is no less effective than intensive courses, while causing less harm to patients. The selection of medications used in chemotherapy regimens depends on the susceptibility of the tumor to a given drug and the general condition of the patient.
You can receive treatment in the following medical institutions:
- Clinic "Assuta", Tel Aviv. This medical center is on the list of the best medical institutions in the world. Stage 0-1 ACSM is treated with minimally invasive operations, under local anesthesia, using the Novalis scanning system and an electronic scalpel. Brachytherapy and neutron therapy are performed. In advanced cases, first chemoradiotherapy, then surgery and a course of chemotherapy.
- Oncological clinic named after. Rabin. The Department of Gynecological Oncology treats ACSM using the latest achievements of Israeli medicine. If the prognosis is unfavorable, when the diagnosis is confirmed by cytological and histological studies using computer analysis, radical hysterectomy (removal of the uterus) is resorted to. According to indications, they resort to gentle treatment with chemotherapy, phototherapy, laser treatment, and conization of the uterus in order to preserve the woman’s opportunity to become a mother in the future.
- Clinic "Top Ichilov", Tel Aviv. CACC of the cervix is treated with conservative and surgical methods. For chemotherapy, the latest medications are used, which are effective in 90% of cases (despite the fact that adenocarcinoma is resistant to most drugs). The hysterectomy is performed with the help of the Da Vinci robot, which ensures precision and efficiency. The risk of damage to large vessels is reduced, and the tumor is excised within healthy tissue.
Approximate prices for treatment
| Service | Price (USD) |
| Consultation with a gynecological oncologist, cytological examination | 400–900 |
| Full range of diagnostics | 3800 |
| Histological examination | 690 |
| Conization | from 3200 |
| Cervical amputation | from 1200 to 4500 |
| Extended hysterectomy | from 44 000 |
| Chemotherapy course | from 1200 |
| Contact radiotherapy | from 10 000 |
| External beam radiotherapy | from 12 000 |
Patient reviews about treatment.
Oksana, Nizhny Novgorod. “I decided to undergo cervical cancer treatment in Israel and I do not regret the choice I made. In Russia, I was threatened with hysterectomy, but the doctor advised me to try a new method. In Israel, at the Top Ichilov clinic, I underwent laser treatment and a course of chemotherapy. Now I’m healthy and thinking about a third child.”
Elena, Izhevsk. “I was always sure that this couldn’t happen to me. The diagnosis of cervical cancer left me in shock. Friends advised me to go to the Rabina MC, to the Davidov oncology department. They received treatment there and liked everything.
Treatment prognosis and possible consequences
Further prognosis largely depends on the patient’s age category, health status, stage and type of adenocarcinoma. In the first and second stages, the prognosis is favorable, the five-year survival rate reaches 70-90%. The third stage worsens the prognosis, it all depends on the degree of spread of tumor cells, however, the rate decreases to 60%. The fourth stage is the most unfavorable prognosis, since the spread of metastases in the body does not provide a chance for complete recovery.
Consequences include tumor recurrence, metastasis and death.
Mechanism of uterine damage
Based on the hypotheses of uterine damage, the following mechanisms for the development of pathology are distinguished.
Estrogenic causes of cancer formation occupy first place, accounting for up to 70% of pathologies. Anovulatory bleeding, late onset of menopause, and infertility are often markers of a probable pathological process. This is accompanied by hyperplastic processes in the endometrium, which over time and under the influence of additional damaging factors can become the first stage of cancer formation.
But the course of such diseases is more favorable. Tumors are usually highly differentiated, progress slowly and metastasize. Such adenocarcinomas are sensitive to the action of gestagens. But there is a high probability of detecting primary multiple carcinomas located simultaneously in the mammary gland, intestines, and ovaries.
The second mechanism for the development of oncology is not associated with hyperestrogenism. When examining a biopsy specimen, such tumors do not show an increase in estrogen receptors, which is observed in the first type. The formation of carcinoma occurs against the background of an atrophically changed endometrium; its cells are poorly differentiated. They are capable of autonomous existence and development, metastasize early and are not sensitive to gestagens. The course of the pathology is more aggressive, the prognosis is unfavorable. This type of cancer is difficult to treat.
The malignant process occurs in stages. Initially, functional disorders occur in the body, which may be associated with hormonal imbalance. In the second type of pathology development, this may be the onset of menopause, which is characterized by atrophic changes in the endometrium.
Against the background of functional changes, background morphological deviations in the structure of tissues appear. This may be glandular cystic hyperplasia, endometrial polyps. Gradually, a precancerous process forms - grade 3 atypical hyperplasia, after which malignant neoplasia develops. Gradually, it turns into non-invasive cancer, which, if left untreated, grows into the endometrium.
Pathways of metastasis
In the body, tumor spreads in three ways:
- Hematogenous.
- Lymphogenic.
- Implantation.
Endometrial cancer is more likely to metastasize through the lymphogenous route. In this case, the external and internal iliac, obturator, and inguinal lymph nodes are affected. Which nodes the tumor cells will go to depends on the primary location of the lesion, the depth of germination and the degree of differentiation.
The lowest probability of metastasis (0-1%) is in a tumor located in the fundus of the uterus, which has a high or moderate degree of differentiation. But it should not grow beyond the mucous membrane.
The risk of metastases of up to 6% is observed when cancer invades ⅓ of the myometrium and maintains high or moderate differentiation. A large area of damage, with transition to the cervix, leads to metastases in 30% of cases.
Damage to the iliac nodes occurs with a tumor in the lower segment of the uterus; from the bottom and middle part of the organ, metastases are found in the lymph nodes located along the aorta. If adenocarcinoma affects the cervix, then metastasis occurs in the same ways as with cervical cancer.
Hematogenous spread usually occurs simultaneously with lymphogenous spread. Metastases are found in the lungs, liver and bones.
The implantation path is spread through the peritoneum, as well as germination to the myometrium and perimeter. The tumor can grow through the appendages into the abdominal cavity, bypassing the pelvis. Therefore, the greater omentum is damaged. This is especially true with low differentiation. Worse prognosis for serous and clear cell adenocarcinoma of the uterus.
Reviews about the treatment and its effectiveness
When I was diagnosed with a highly differentiated tumor of the first stage, I underwent abdominal surgery to remove the uterus and appendages. My age is 45 years old. Irradiation was canceled due to necessity. Now I feel better, my body is recovering, I went back to work.
I am 62 years old. Periodic bleeding was observed for six months. A diagnosis of uterine cancer, stage 1C was made. They performed an operation to remove the uterus along with the appendages, after which they prescribed radiation therapy, three courses, I think it’s called brachytherapy. I have been regularly examined for five years and feel great.
Forecast
If the form of cancer is a highly differentiated endometriotic tumor of the uterus and there are no metastases, then at the initial stage of the oncological process the prognosis for uterine adenocarcinoma is positive. A timely operation for resection (removal) of the tumor body in full, followed by courses of radiotherapy or chemotherapy, can even guarantee recovery for patients.
The situation is more complicated with the prognosis for stages 3-4 of uterine cancer. A woman of childbearing age is deprived of the opportunity to have children, because the entire uterus must be removed. But even at stage 3, the probability of cure today reaches 75% thanks to the latest equipment in specialized clinics and the highly qualified oncologists.
The unfavorable nature of uterine adenocarcinoma is when it metastasizes and spreads to nearby organs. The survival rate even with complete removal of the uterus, adjacent lymph nodes and vagina is low. Stage 4 cancer – advanced Tumor metastasis no longer guarantees a prognosis for life beyond 5 years.
Prevention
Preventive measures include primary and secondary prevention.
- Primary prevention is aimed at preventing the development of adenocarcinoma. To do this, it is necessary to undergo regular examination by a gynecologist, ultrasound examination of the pelvic organs, and timely treatment of detected pathologies. Don’t forget about maintaining a healthy lifestyle, eliminating bad habits, playing sports, and eating right. If you are overweight, you need to take weight loss measures; if you have hypertension and diabetes, you need to take treatment measures.
- Secondary prevention includes measures to prevent the development of complications and relapses after treatment.
Prognosis for uterine adenocarcinoma
The prognosis of the pathology depends on a number of related factors: the patient’s age, general condition, extent of the process, and the presence of metastases. After treatment of uterine adenocarcinoma in stages 1–2, the five-year survival rate ranges from 70–98%. Patients with treated stage 3 pathology achieve a five-year survival rate of 10–60%; the worst prognosis after treatment for stage 4 uterine adenocarcinoma is a five-year survival rate of no more than 5%. Relapse of the disease is observed in 75% in the first 3 years after therapy. Moreover, in 50% of patients, metastases are localized in the vagina, in 30% in nearby lymph nodes, in 28% - distantly.
Specific prevention of uterine adenocarcinoma has not been developed. Nonspecific preventive measures include:
- regular gynecological examinations;
- annual examination of the pelvic organs by ultrasound;
- maintaining a healthy lifestyle;
- treatment of precancerous processes of the endometrium and hormonal disorders;
- normalization of weight in obesity;
- correction of diabetes mellitus, arterial hypertension;
- balanced diet.
Sozinova Anna Vladimirovna, obstetrician-gynecologist
just today
( 37 votes, average: 4.30 out of 5)
Why does your chest hurt: spring problems
The use of hormone-containing medications during menopause: a review of medications