Leiomyoma of the uterine body is a pathological muscular growth of the walls of the organ, which leads to oncology. The tumor itself has a benign structure, but due to neglected treatment it can become malignant. In medicine, this pathology is also called fibroids or uterine fibroids. This disease can appear in one in four women who are between the ages of thirty and forty years. This disease is considered hormone-dependent and can proceed independently. But basically the pathology requires appropriate therapy.
Let's take a closer look at what it is and how to treat uterine leiomyoma.
Features of pathology and structure of the uterus
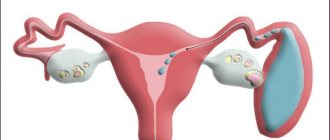
To get a specific idea of this tumor, you need to study the structure of the female reproductive organ. The uterus is a hollow organ that can carry a baby and then push it out during childbirth. This complex mechanism of work occurs thanks to the myometrium, the inner layer of the organ. Such a strong frame is formed from muscle fibers of various types in conjunction with connective tissue.
What it is - uterine leiomyoma, you can see in the photo.
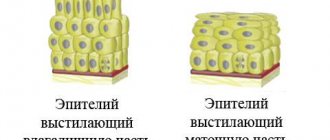
Outside, the myometrium is covered with a serous membrane, which resembles the abdominal cavity in its composition. The inner layer is called the endometrium, which consists of layers of epithelium. At a certain phase of the cycle, this layer is renewed, after which menstruation occurs. Any such processes are controlled by female hormones that are produced in the ovaries.
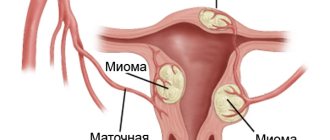
This disease is characterized by the appearance of a myomatous node. If there are several such appearances, then this is multiple uterine leiomyoma. Such growths vary in size, structure and type. Nodular forms very often do not manifest themselves in any way, and women do not know about the disease for years if they do not visit the gynecologist regularly.
The tumor does not have any special symptoms at an early stage. The clinical picture is in many ways similar to various gynecological diseases. In this regard, ultrasound and hysteroscopy are considered the most reliable diagnostic methods. Doctors do not always prescribe treatment for uterine leiomyoma to patients. Typically, when a woman reaches menopause, the tumor, in turn, freezes and regresses. Thus, it requires simple regular monitoring.
This disease is hormone-dependent in nature. In this regard, it is easily influenced by hormonal drugs. Small fibroids under the influence of medications can completely disappear or stop in their development. Removal surgery is prescribed in situations where there is a risk of serious complications, and the woman, in turn, feels severe pain along with impaired functioning of nearby organs. But even after surgery, this disease can return. This most often happens due to incorrect treatment tactics to eliminate the causes of the tumor.
Treatment of uterine fibroids
Treatment of uterine fibroids is a complex task. The very need for surgical intervention on the pelvic organs brings psychological discomfort and anxiety to a woman, and if we are talking about removing an entire organ, then such a decision should be very well weighed by the attending physician. In difficult cases, it is better to consult several specialists, each of whom can offer the most optimal and least traumatic method of treatment for the patient.
Many specialists prefer radical methods of treatment for uterine fibroids, that is, removal of nodes or the entire organ, but when the patient is young and planning a pregnancy, this approach may be unacceptable, so if possible, it is worth trying to preserve both the uterus and reproductive function. In the case of older women who already have children, radical surgery can create psychological problems, since the absence of a uterus is often difficult for the patient.
Modern approaches to the treatment of uterine fibroids involve the use of conservative therapy, minimally invasive interventions and operations to remove nodes or the entire affected organ. In each case, the choice of method is carried out individually, taking into account the nature of tumor growth, the size and location of the nodes, their number, and the age of the patient and her plans for childbearing must be taken into account.
Today, medicine has made great strides forward in the use of gentle methods of treating tumors, and it is often possible to do without surgery, so the wait-and-see approach, which was used quite recently and is used by some specialists now, is not entirely justified. If the diagnosis of fibroids is beyond doubt, then it is better to start treatment as early as possible, without waiting until the tumor reaches a large size, and there will no longer be an opportunity to resolve the issue with little blood. The patient should immediately ask which clinics can receive treatment, where there is appropriate equipment and highly qualified specialists work.
Conservative treatment
Non-surgical methods for treating uterine fibroids do not lead to complete disappearance of the tumor, but they can significantly slow down the growth of nodes, so this approach is applicable for women in the premenopausal period, when, with the onset of menopause, the nodes will begin to slowly regress on their own and reach a state where there is no longer a risk to health will. If the woman is young, then conservative treatment will help reduce the amount of surgery that may be required in the future.
Indications for conservative therapy may include young age and a woman’s desire to preserve reproductive function, small size of the node, asymptomatic course of the tumor, high risk in the case of surgery, as well as preparation for subsequent surgical treatment.
Since uterine fibroids grow under the influence of female sex hormones, it is quite understandable to use various groups of hormonal drugs for treatment without surgery:
- Combined oral contraceptives (Novinet, Marvelon, Ovidon, etc.);
- Intrauterine systems with hormonal activity (Mirena);
- Gonadotropin-releasing hormone (GTRH) agonists – zoladex, diferelin;
- Progesterone antagonists (mifepristone) and antigonadotropins (danazol).
Combined oral contraceptives can not only reduce the growth of nodes, but also normalize the menstrual cycle, relieve the patient from painful and heavy bleeding and associated anemia. These drugs protect against unwanted pregnancy during the period of treatment, but their disadvantage is contraindications that limit their use in women with diseases of the cardiovascular system, liver and kidneys, varicose veins, and migraines. After 35-40 years, their appointment may also be undesirable.
Intrauterine systems that secrete hormones locally are free of many of the side effects characteristic of tablet drugs and can be used until menopause. The conditions for their use will be the small size of the tumor node (up to 6-7 weeks of pregnancy), the absence of inflammatory changes in the uterus and its deformation.
of prescribing GTRH agonists is to create a medical pseudomenopause, when the natural level of sex hormones drops and a state close to menopause occurs. In addition to fibroids, they have a therapeutic effect both for endometrial hyperplasia and endometriosis, which often accompany the tumor. With this treatment, it is possible to reduce the nodes by a third or even half, but side effects force not only to limit treatment to six months, but in some cases to abandon it altogether. The most unfavorable consequences of using drugs in this group are considered to be hot flashes, feelings of heat, pressure fluctuations, sleep disturbances and emotional disorders.
Recently, progesterone antagonists have been used as conservative treatment, which help reduce the size of the nodes, but do not cause severe menopause, which gives them an advantage over the previous group of drugs. Most often they are prescribed as a preparatory step before surgery, but the possibility of long-term independent use is also being studied.
Qualitatively new approaches to the treatment of uterine fibroids include the possibility of using drugs that inhibit the activity of various tumor growth factors, as well as angiogenesis (the development of tumor vessels). The positive effect of interferon on uterine fibroids has already been proven. Many drugs are undergoing clinical trials, and the search for means that would completely eliminate surgery continues.
Hormonal therapy cannot yet be the only method of treatment, especially in young women, when withdrawal of drugs leads to the resumption of growth of nodes after 2-3 months, and the size of the uterus returns to its original state. Hormone therapy is usually prescribed before planned surgery to reduce the size of the tumor, and surgery should be performed within one to two months after treatment.
Thus, in each specific case, an individual treatment regimen is selected depending on the nature of tumor growth, the woman’s age and the presence of contraindications to specific drugs. It is worth recalling that treating fibroids yourself in this way without consultation and supervision from a gynecologist is unacceptable and even dangerous.
Surgical treatment of fibroids
Until recently, surgical treatment of fibroids involved removal of the entire organ. The operation allows you to immediately get rid of the tumor, but the risk of complications and long-term adverse consequences remains high to this day. The need for general anesthesia, manipulations inside the abdominal cavity, the possibility of bleeding and adhesions, and the high risk of subsequent pregnancy force doctors to look for new, more gentle methods of treating the tumor. Thus, if possible, a woman is tried to undergo uterine artery embolization, FUS-MRI ablation, and selective removal of nodes while preserving the uterus.
If the possibilities of conservative treatment and minimally invasive techniques have been exhausted, progression of the disease is observed, there is a high risk of malignant transformation and the woman is no longer young, then they resort to removing the entire affected uterus with or without the cervix.
Non-invasive treatments
Among non-invasive methods for removing fibroids, uterine artery embolization (UAE) and ultrasound ablation (FUS-MRI ablation) are distinguished, which, although they are classified as surgical treatment, are still not an operation in the generally accepted sense of the term.
FUS-MRI ablation involves exposure of the myomatous node to a focused ultrasound beam, which leads to heating of the tumor tissue and their irreversible death. In addition, with this effect, blood flow in the tumor is disrupted and relapse does not occur. The procedure is carried out under MRI control, which gives a chance to target neoplasia without damaging surrounding tissue. Selective necrosis of the tumor leads to a decrease in its size, thereby the woman gets rid of pain, heavy uterine bleeding, and compression of neighboring organs by nodes.
FUS-MRI ablation
The undoubted advantages of the method are:
- The duration of the procedure is only 3-4 hours;
- Targeting the tumor;
- Possibility of outpatient ablation without general anesthesia;
- Preservation of the uterus and no blood loss, as in the case of surgery;
- Restoration of working capacity the very next day.
Indications for FUS-MRI ablation are the presence of pain, uterine bleeding, node sizes from 2 to 15 cm, signs of compression of neighboring organs and tissues. As a rule, the procedure is performed immediately if the diameter of the tumor does not exceed 9 cm, but if the tumor is larger, then it is more advisable to prescribe hormone therapy for several months to reduce the size of the tumor.
The method is very good, but it also has contraindications, which are also associated with the need for MRI: claustrophobia (fear of closed spaces), severe obesity, the presence of pacemakers and implants made of metal materials. In addition, certain difficulties may arise with abdominal wall scars and adhesions. FUS ablation cannot be performed in case of inflammatory processes in the pelvis, ovarian pathology, infertility and unrealized reproductive function, severe deformation of the uterus, or the presence of subserous nodes on the pedicle. The most common complications of the procedure include local first-degree burns and minor inflammatory reactions.
Uterine artery embolization (UAE)
Uterine artery embolization (UAE) is a fairly promising treatment method, which in many cases allows you to do without surgery. In case of high surgical risk, UAE is an alternative to conventional surgical treatment.
The essence of UAE is the cessation of blood flow through the vessels supplying myomatous nodes. A special conductor is inserted through a puncture in the femoral artery, through which an embolic substance (polyvinyl alcohol) will flow into the branches of the uterine artery. In this case, the nutrition of the nodes stops, and in a healthy myometrium it is restored due to collaterals (bypass paths).
The advantages of the method are a selective effect on fibroids, absence of bleeding and other postoperative complications, preservation of the uterus and reproductive function. The procedure also does not require general anesthesia and a long hospital stay. UAE can be performed in all cases, with the exception of the presence of subserous fibroids on the leg, inflammatory process in the pelvis, tumor pathology of the ovaries and cervix, infertility in the absence of children, renal failure and allergies to contrast agents. In case of concomitant pathology that complicates the operation (diabetes, hypertension, obesity), UAE is preferable.
Among the complications of the method is the so-called post-embolization syndrome, associated with damage to tumor tissue, when there may be an increase in body temperature, the appearance of nausea and vomiting, abdominal pain, and leukocytosis in the blood. The described symptoms disappear within two days after UAE, subject to symptomatic therapy.
Surgery for uterine fibroids
When the possibilities of gentle methods are exhausted or are impossible due to the multiplicity of nodes, their large size, and the risk of a malignant process, the doctor is forced to resort to radical methods of removal . Surgical treatment remains the main treatment, and up to 80% of women with fibroids undergo it.
Indications for surgical treatment of uterine fibroids are:
- Large knots;
- Multiple growth pattern;
- Rapid growth of nodes;
- Localization of fibroids in the cervix;
- Continued tumor growth during menopause;
- Dysfunction of nearby organs and severe uterine bleeding;
- Necrosis of the node.
In each case, the woman’s age, the presence of concomitant pathology, the nature of growth and the location of the tumor are also taken into account. Radical surgery involves removing the entire uterus. If the patient has background pathological changes in the cervix (epithelial dysplasia, leukoplakia, etc.), then the uterus is removed along with the cervix, although, of course, doctors try to preserve it.
laparoscopic myomectomy
Myomectomy is considered a gentle method of surgical treatment of fibroids - selective removal of nodes while preserving the uterus. This organ-preserving approach is very justified in young women under 40 years of age who want to preserve the uterus and menstrual function, as well as if the patient wishes to become pregnant in the future. The size of the nodes for such an operation ranges from 20 to 50 mm, then it is most optimal to remove them.
Access during the operation can be laparotomic, laparoscopic and hysteroscopic. With the laparotomy approach, an incision is made in the anterior abdominal wall, through which the doctor can examine the affected organ, remove the nodes or the entire uterus, and qualitatively suture the vessels and tumor bed. Laparotomy is preferred in case of myomectomy if a woman is planning a pregnancy, since the outcome of the suture may depend on the quality of the sutures. To prevent uterine rupture in the area of scars left after myomectomy, delivery is performed by cesarean section.
Laparoscopic access avoids large incisions and postoperative scars, and also has a good cosmetic effect. With this access, it is possible to remove not only individual nodes, but also the entire organ (hysterectomy), but this will require appropriate equipment and high professionalism of the surgeon.
hysteroscopy
Hysteroscopic access is justified for small submucosal nodes, when it is enough to penetrate the uterine cavity to remove them. Such operations are performed on young women for whom it is important to preserve reproductive function.
The issue of radical treatment of fibroids should be decided by an experienced and highly qualified surgeon who is determined to preserve the woman’s uterus if possible, and only if more gentle methods are ineffective, multiple large nodes or the risk of malignancy of the tumor process will preference be given to complete removal of the organ. The treatment option that the surgeon will offer depends not only on his professionalism, but also on the technical capabilities of the medical institution, the availability of endoscopic equipment, etc. Many women are ready to travel hundreds of kilometers in order for it to be the most comfortable and least traumatic.
Along with the described methods of treatment, the woman’s lifestyle is important; she should avoid stress and intense physical activity, get rid of bad habits if they exist, take vitamin complexes and iron supplements in case of anemia. Treatment with folk remedies, which patients often resort to instead of going to the doctor, is unacceptable. The tumor will not resolve, but the risk of other complications is very high. Thus, douching with various infusions can lead to damage to the mucous membrane of the genital tract and the development of inflammation, and taking medicinal herbs internally will only waste time.
In general, the priority in the treatment of uterine fibroids in recent years has become the use of minimally invasive and non-surgical methods that allow preserving the uterus and reproductive function. Perhaps research in the field of genetics will help find not only new effective treatment methods, but also develop preventive measures that will eliminate the very need for treatment.
Given the increase in the incidence of tumor pathology of the uterus, special importance is attached to preventive measures. Every woman not only should, but is obliged to visit a gynecologist at least once a year if she takes responsibility for her health . It is also recommended to undergo an ultrasound of the pelvic organs, be examined for sexually transmitted infections and treat them in a timely manner. Intrauterine manipulations, such as abortions and frequent curettages, should be avoided, and if a woman considers it necessary to postpone pregnancy for a while, then she should think about taking contraceptive medications, because they will not only help avoid abortion, but will also help normalize hormonal levels. A healthy lifestyle and taking care of your health can help a woman maintain reproductive function, give birth to healthy children and avoid tumors.
Types of uterine leiomyoma
Let us now consider the classification. Depending on the location of the myomatous node, this tumor has different names in medicine.
- Intramural leiomyoma of the uterine body is more common than other types. It is formed in the inner region of the muscle layer. Its formation occurs quite deeply. Symptoms are manifested by pain in the pelvic area, irregular cycles, and, in addition, disruption of the activity of neighboring organs.
- With submucosal leiomyoma, tissue grows under the lining of the uterus. Often, this type of tumor can grow inside an organ, and it is not always possible to conceive a child.
- Subserous leiomyoma forms under the serosa, as is obvious from the name. It can be located on the outside and most often grows towards the abdominal cavity. The difference between this type is the absence of symptoms. The only thing women notice is a slight discomfort in the lower abdomen.
- Multiple leiomyomas are the formation of several nodes that differ in volume, location of attachment and tissue composition.
- An unspecified form of uterine leiomyoma means a latent form of a tumor that cannot be confirmed by diagnosis. This can happen extremely rarely due to the small size of the tumor or due to its slow growth. Gynecologists can only guess about the presence of a problem. Women need to be constantly monitored by a doctor so as not to miss the onset of the disease.
Nodular uterine leiomyoma is diagnosed in many patients. This is a fairly common gynecological disease. It occurs in 30% of women of late reproductive age and patients during menopause. As for the prognosis of this disease, there are doubts. If the problem is detected in a timely manner, a comprehensive examination is carried out and therapy is prescribed, the disease can be quickly cured. But there is a high risk of relapse, so it is important to visit your gynecologist regularly.
With an advanced form of nodular leiomyoma, the formation can become malignant, and therefore even a fatal outcome is possible.
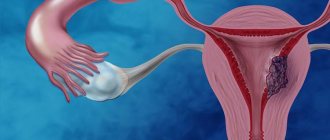
Subserosal
This localization of fibroids occurs in about a third of women with this disease. The myomatous node is located under the serous membrane (peritoneum), covering the body of the uterus from the outside. The node grows into the pelvis or abdominal cavity.
The tumor is always located on the base (“pedicle”), which is formed by the layers of the serous membrane and contains blood vessels and nerve fibers. The “leg” can be wide or narrow.
Symptoms
The small size of a myomatous node of subserous localization is usually not accompanied by any manifestations. As the tumor grows, it can compress neighboring structures, which is accompanied by the appearance of corresponding symptoms. Most often, subserous uterine leiomyoma manifests itself with the following symptoms:
- Pain of varying intensity in the lower abdomen and lumbar region when the tumor compresses nerve bundles or grows into the peritoneum.
- Disorders of urination or defecation (if the tumor is located in the area of the ureters, bladder or rectum).
- Infertility due to compression of the fallopian tube, etc.
The most serious complication of subserous localization of uterine leiomyoma is torsion of the movable “leg” of the myomatous node. As a result, a sharp malnutrition of the tumor occurs with a fairly rapid development of its necrosis. This condition is accompanied by the appearance of severe abdominal pain, an increase in body temperature and other manifestations of general intoxication due to the breakdown of necrotic tissue and the formation of peritonitis.
Torsion of the “leg” of the tumor is an indication for emergency surgery.
Leiomyomatosis and stages of its maturation
Any leiomyomatosis forms in the myometrium and goes through some stages of maturation:
- First, a muscle knot is formed, which grows from smooth muscle and fibrous fibers around small vessels. At this stage, there are still no clinical manifestations, since the size of uterine leiomyoma is small.
- Then comes maturation. At this time, the fibroid is actively growing and forms a ball of muscle fibers, which becomes denser over time. Adjacent tissues begin to gather around it, forming a special capsule. This process is also called tumor maturation. During diagnosis, fibroids are quite easy to detect, and the patient already develops clinical symptoms.
- The next stage is the aging of the leiomyoma. Considering that the tissues degenerate due to pathological processes, the node stops growing.
In each individual case, oncology can behave differently. You should not expect the same symptoms in all women with this diagnosis.
Leiomyoma and its causes
The detected gynecological tumor directly depends on the woman’s hormones. In the presence of a large amount of estrogens, cells divide pathologically, and during menopause this process stops. The true causes of leiomyoma are still not fully understood, but there are the following provoking factors:
- Brain injuries are a central factor, along with vascular pathologies and psycho-emotional disorders. Hormones of the pituitary gland and hypothalamus control the functions of the ovaries. The ovaries, in turn, are responsible for the processes of follicle maturation and ovulation. Thus, any disruptions in brain activity can lead to dysfunction of the reproductive system.
- The classic factor is infectious and inflammatory diseases of the ovaries of a chronic nature, including polycystic disease. Against this background, a hormone imbalance occurs, which leads to the diagnosis of leiomyomatosis. In medical practice, the classical factor is encountered more often than others.
- With the uterine factor, any mechanical trauma to the reproductive organ can provoke the appearance of neoplasms. Even against the background of good functioning of the ovaries, the uterus is capable of not receiving hormones due to damage to the receptors. Complicated childbirth, along with abortion and surgery, can cause similar trauma.
- Associated factors are disturbances in the functioning of the endocrine system, thyroid disease, and so on. All this causes the growth of the myomatous node.
If a woman knows in advance about her predisposition to at least one of these factors, she is recommended to visit a gynecologist and more carefully monitor her health.
What are the symptoms of uterine leiomyoma?
Symptoms of the disease
The clinical picture of this disease directly depends on the growth of the tumor, and in addition, on the number of nodes, their location and the progression of the pathology. Small interstitial muscle nodes are not dangerous to the body. But submucosal leiomyoma of the uterus, even if it is small in size, can significantly manifest itself with the following symptoms:
- Presence of menstrual irregularities. Your periods may become irregular, heavy, and longer. At an early stage, such manifestations are relieved by medications, so patients do not immediately consult a doctor. But gradually the blood loss becomes significant and causes discomfort and pain. In this case, anemia occurs, and then it is no longer possible to do without the help of a doctor.
- Pain syndrome may appear due to severe contraction of the myometrium. Large fibroleiomyomas do not allow the epithelium to peel off, and pain occurs. Severe pain can occur with subserous fibroids. Directly with the intramural form, the sensations are pulling and aching. If necrosis has occurred in the tissues of the uterus, sharp pain will be felt.
- Disturbances in the functioning of neighboring organs. Leiomyomatosis can cause disturbances in the functioning of the intestines and bladder. Against this background, the woman will feel a frequent urge to go to the toilet. Or, on the contrary, there may be difficulties with bowel movements or urination.
- The appearance of dysfunction of the reproductive organs. Against the background of leiomyoma and concomitant diseases, as well as hormonal imbalance, women develop infertility, and in addition, ovulation is disrupted. The reason for this is the unfortunate location of the myomatous node in the organ cavity, which prevents the attachment of the egg. Leiomyoma during pregnancy sometimes has unpleasant consequences in the form of premature termination and miscarriage. But according to statistics, such cases occur quite rarely.
What it is?
Uterine leiomyoma is a tumor-like growth of cells in the muscular layer of the uterus (or myometrium), which has a benign course.
Such a tumor-like formation (or myomatous node) is formed by smooth muscle fibers of the myometrium with inclusions of connective tissue. Often the node has a so-called pseudocapsule, which is formed from muscle fibers compressed by the tumor. Due to the abnormal growth of uterine muscle tissue, the structure of blood circulation and innervation in the area of the myomatous node also changes.
The formation of leiomyoma can begin in almost any part of the myometrium.
Moreover, it can be single or multiple. The further direction of growth of the tumor-like formation is hardly predictable and occurs in different directions. Based on this, the disease is classified according to the location of the myomatous nodes in the uterine muscle layer. There are the following types of uterine leiomyoma:
- Submucosal (submucosal).
- Intermuscular (intramural, interstitial).
- Subperitoneal (subserous).
- Interligamentous (intraligamentary). Although most doctors classify such leiomyoma as a type of subserous localization.
In approximately 5% of cases, myomatous nodes form in the muscle layer of the cervix.
Diagnosis of the disease
At the first appointment with the gynecologist, the uterus is examined and the patient’s complaints are collected. As part of a two-handed examination, the deformation of the organ and its size are determined. It is the size of the uterus that is of great importance. The specialist selects a specific day of the cycle, and during the year, exactly at this time, the examination is carried out. If the uterus has not increased in size over the course of a year, then doctors talk about the slow progression of the disease.
Thanks to the use of a gynecological speculum, it is possible to detect submucosal nodes growing towards the cervix. For more accurate results, colposcopy methods are used. The most accurate way to diagnose oncology is considered to be an ultrasound examination, which can be used to establish:
- The total number of myomatous nodes along with their characteristics.
- Structure, duration and type of leiomyoma.
- Endometrial pathology.
- The nature of the functioning of the ovaries.
In addition to ultrasound examination, hysteroscopy is performed, and a smear is taken for flora along with a biopsy for oncocytology.
Treatment of leiomyoma
We have already studied how leiomyoma is diagnosed. Next, we will find out how this disease is treated. In medical practice, this tumor is usually treated using conservative methods. Very often it disappears on its own or regresses during menopause. In this regard, doctors are in no hurry to perform surgical removal of uterine leiomyoma. The choice of appropriate treatment directly depends on the result of the examination and the general well-being of the patient. The prerequisites for therapy using traditional methods are the following factors:
- The tumor size is up to three centimeters along with a slight enlargement of the uterus.
- Asymptomatic course of the disease.
- A woman's planning for pregnancy in the future.
- The presence of intramural or subserous type of fibroids.
Diagnostics
The clinical picture of the disease directly depends on the location of the myomatous nodes. In this case, the course of the disease can vary from completely asymptomatic to the development of severe symptoms (bleeding, pain, etc.).
A routine gynecological examination reveals an enlarged uterus, which often has an irregular shape or uneven surface. Traditionally, the degree of uterine enlargement is indicated in weeks of conditional pregnancy.
The use of additional diagnostic techniques helps to establish the exact location of myomatous nodes in order to select further tactics. These include:
- Ultrasound scanning of the pelvic organs. It is the most common and accessible method for diagnosing this disease.
- Magnetic resonance imaging (MRI).
- Endoscopic methods – hysteroscopy and laparoscopy.
To determine the possible cause of hormonal imbalance, various laboratory methods are used: determining the level of thyroid hormones, adrenal glands, estrogen, progesterone, etc. In order to diagnose complications of the disease, general clinical and other studies are also prescribed.
According to statistics, in more than half of women, uterine leiomyoma is completely asymptomatic and is an unexpected “find” during a gynecological or ultrasound examination.
Surgery for leiomyoma
Doctors prescribe surgical intervention to patients in the following cases:
- The presence of an advanced disease, when the submucosal leiomyoma of the uterus is very large.
- Presence of submucosal nodes.
- The presence of torsion of the legs of the nodes along with necrosis of the uterine walls.
- Development of subserous fibroids with extremely severe symptoms.
- Location of leiomyoma on the cervix.
- The presence of hyperplastic processes.
- Lack of any effect from conservative treatment.
Modern surgical techniques make it possible to preserve the reproductive organs during surgery for uterine leiomyoma, removing only the neoplasm. Such operations include myomectomy, FUS ablation, along with partial removal of the uterus through defundation. Absolute removal of the organ is performed using hysterectomy. An operation aimed at removing a tumor does not always lead to its complete disappearance. Sometimes fibroids can grow back.
What else is used in the treatment of uterine leiomyoma?
Use of medications
The main thing in treating this disease is to be able to stop the cause of its occurrence. Therefore, very often specialists prescribe hormonal therapy in order to reduce estrogen levels and normalize their quantity. The following medications are used for this:
- GnRH analogs.
- Antiprogestogens.
- Progesterone analogues.
- Combined oral contraceptives.
All medications have their own individual contraindications for use. For example, some of them cannot be taken if a woman has a history of hemorrhagic syndrome. As part of their use, you must first read the instructions and discuss the dosage regimen with your doctor. Treatment with hormonal drugs is always required for a long time. In parallel with this, patients are prescribed therapy with folk remedies, and in addition, it is advisable to use sedatives, antianemic and vitamin preparations.
The duration of treatment is about six months or more. At this time, it is necessary to monitor the pathological process using ultrasound once every three months. If necessary, the doctor will adjust the dosage or replace medications. Alternative medicine methods such as hirudotherapy, homeopathy, bee products, and so on can be used as auxiliary drugs.
But it should be remembered that leiomyoma is a disease that has its own complications and dangers for the body. You cannot self-medicate; you should definitely consult a specialist. There are cases of this tumor degenerating into cancer; this transformation is called uterine leiomyosarcoma. Therefore, under no circumstances should this disease be left to chance.
Reviews about uterine leiomyoma
Women write about this disease that it is an extremely unpleasant pathology. Many people have to undergo surgery to remove leiomyoma. Usually ladies write that with the removal of the tumor, all problems associated with the unpleasant clinical manifestations of this disease go away.
But the main disadvantage of surgical intervention is the inability to give birth to a child. Also, those who had to undergo a hysterectomy report that after the operation they developed adhesions, constipation and problems in the intimate area. Women write that after undergoing a hysterectomy, they began to experience caries, problems with bones, hot flashes and dizziness.
Thus, based on reviews, we can say that hysterectomy due to leiomyoma entails many negative consequences. And among the advantages, women name only getting rid of menstruation and preventing the possible degeneration of leiomyoma into a malignant neoplasm. Women also write that hysterectomy, despite all the disadvantages and consequences, is by far the most effective solution to such a problem as uterine leiomyoma.
What it is and how to treat the pathology is now clear.
Treatment
Treatment or removal of a node of this type is carried out strictly as prescribed by the attending physician. There are two treatment approaches:
- Conservative. It is applicable for small and medium-sized nodes, as well as for the expected onset of menopause. Because during this period the node may disappear on its own. It is carried out with the help of hormonal drugs that stop the production of hormones in the body. As a result, menopause occurs and the tumor stops growing;
- Surgical. Laparoscopic or abdominal surgical removal of the tumor is performed. If there is no need to preserve reproductive function, part of the uterus or all of it may be removed. You can learn more about this from the article “Surgery to remove uterine fibroids.”
A separate type of procedure is uterine artery embolization. Simply put, this is a local blockage of the arteries and stopping the blood supply to the node. This is a low-traumatic intervention, performed laparoscopically. Prescribed for active fibroid growth or severe bleeding. Allows you to completely preserve reproductive function.