Reasons for appearance
Today, the causes of the disease are not fully understood, but several decisive factors are identified:
- congenital or family predisposition;
- hormonal factors - the disease develops in patients with pathology of the function of the endocrine glands;
- metabolic disorders of essential substances. Osteochondropathy is often caused by impaired absorption of calcium and vitamins;
- traumatic factors. Osteochondropathy occurs after excessive physical exertion, incl. increased muscle contractions, frequent injuries. Initially, these types of loads lead to progressive compression, and then to a narrowing of the small vessels of the spongy bones, especially in areas of greatest pressure.
Symptoms of osteochondropathy
Osteochondropathy of the calcaneus (Haglund-Schinz disease) develops most often in girls 12-16 years old, characterized by gradually increasing or acute pain in the tubercle of the calcaneus that occurs after exercise. There is swelling at the site of attachment of the Achilles tendon, above the calcaneal tubercle. Patients begin to walk, leaning on their toes, and playing sports and jumping become physically impossible.
Spinal osteochondropathy (Scheuermann-Mau disease) develops most often in boys 11-18 years old. The first stage is characterized by increased thoracic kyphosis (curvature of the spine in its upper part), the second - by back pain (especially with prolonged walking or sitting), rapid fatigue and weakness of the spinal muscles, and increased thoracic kyphosis. At the third stage of spinal osteochondropathy, complete fusion of the apophyses with the vertebrae is observed. Over time, osteochondrosis develops with increasing pain.
Osteochondropathy of the femur (Legg-Calvé-Perthes disease) develops in most cases in boys 4-12 years old. At the beginning of the disease there are no complaints, after which pain appears in the hip joint, radiating to the knee. Pain occurs after exercise and goes away after rest, so children do not always complain about it. The movements of the hip joint are gradually limited, muscle atrophy develops, and the thigh on the affected side loses weight.
Osteochondropathy of the tibial tuberosity (Schlatter's disease) develops in boys 12-16 years old, especially in those who engage in ballet, competitive dancing, and sports. The patient complains of pain under the patella and swelling. When the quadriceps femoris muscle is tense, when squatting, or climbing stairs, the pain intensifies.
Symptoms and manifestations
A decrease in the quality and comfort of a patient’s life can be expressed in:
- First of all, the persistent pain syndrome in the heel and toe area.
- Changes in gait - both adults and children try to step less on the heel, the pressure on which causes pain. If both limbs are affected at once, the person shifts his weight to the front half of the foot and walks almost on his toes.
- Your legs get tired quickly even after short walks.
- A noticeable swelling develops above the tubercle on the heel bone.
- The skin around the sore spot gradually atrophies, swells, and its sensitivity becomes increased, including on the plantar side.
Improper weight redistribution leads to a significant risk of encountering:
- severe flat feet;
- hallux valgus;
- deformation of the 2nd and 3rd fingers
Diagnosis of the disease
To determine osteochondropathy of the calcaneus, they are based on clinical data and the results of an x-ray examination (fragmentation, hardening of the apophysis, “roughness” on the tubercle of the calcaneus are noted). A differential diagnosis of osteochondropathy with heel spur (in older patients) and achillobursitis is also carried out.
Diagnosis of spinal osteochondropathy occurs on the basis of examination data (increased thoracic kyphosis) and x-ray examination (the pictures show that the shape of the vertebrae has been changed - they become wedge-shaped).
Osteochondropathy of the femur is also determined by X-ray images. Five stages of change in the femoral head have been identified.
Osteochondropathy of the tibial tuberosity is determined by the clinical picture and clarified after an X-ray examination.
Diagnostics
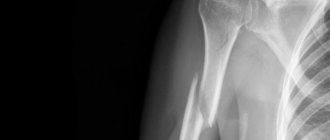
X-rays provide the most information. A picture is taken in a lateral projection, and the doctor determines the development of Haglund-Schinz disease by the compaction of the tubercle, the widened gap between it and the heel bone, and the uneven, spotted structure of the ossification nucleus (see photo).
Photo. Redness and swelling with Schinz's disease
In the later stages of the disease, the spongy substance of the new bone tissue is clearly visible in the image. Comparative x-rays of the diseased and healthy feet help to understand complex cases. In this case, it is important to carry out differential diagnosis to exclude:
- any acute inflammatory processes;
- bursitis, periostitis of the heel;
- osteomyelitis;
- heel spur;
- bone tuberculosis;
- malignant tumors.
The absence of inflammation can be judged by the norms of leukocytes and ESR in a blood test. Bursitis and periostitis are observed, as a rule, not in adolescents, but in adults. Older people suffer from heel spurs. Increased fatigue and irritability, characteristic of bone tuberculosis and cancerous tumors, do not occur with Haglund-Schinz disease.
A computer or magnetic resonance imaging scan of the heel bone helps the doctor to finally dispel doubts. In difficult cases, the orthopedist consults with a phthisiatrician or oncologist.
Treatment of osteochondropathy
Therapy for osteochondropathy of the calcaneus consists of prescribing non-steroidal anti-inflammatory drugs (if severe pain), physiotherapeutic procedures, and reducing physical activity. To relieve the load on the heel bone, special insoles-instep supports are used.
Spinal osteochondropathy is treated with massage, swimming, underwater stretching, and physical therapy. In some cases, if posture is severely impaired, surgery is prescribed.
Treatment of osteochondropathy of the femur can be surgical or conservative. Various osteoplastic surgeries are prescribed depending on the stage of the disease. Conservative treatment of osteochondropathy consists of bed rest (the patient should not sit), foot massage, and physiotherapeutic procedures. They practice skeletal traction on both hips.
To treat osteochondropathy of the tibial tuberosity, physiotherapeutic procedures and heat are prescribed. If the pain is severe, apply a plaster cast. Sometimes they resort to surgery - a fragment of the tuberosity is removed. Loads on the quadriceps femoris muscle are excluded.
An integrated approach to treatment
Any therapy for a disease cannot be used alone. The species must be combined and provide a lifestyle that promotes the restoration of damaged tissue. If possible, the patient should move as little as possible, stay in bed, and, if necessary, go somewhere to use crutches.
Conservative therapy
When osteochondropathy of the calcaneus is detected in children, its treatment can be carried out in an emergency room or on an outpatient basis at an appointment with an orthopedist.
In the acute phase, it is necessary to organize:
- Complete rest of the affected leg, immobilize it using a plaster splint.
- Physiotherapeutic procedures aimed at local stimulation of blood flow.
- Walk only in special orthopedic shoes with a wide back that does not compress the heel area.
Specialized custom-made insoles reduce pain and increase the effect of therapeutic measures. One of the main effects of wearing them is the prevention of the development of flat feet, which most people who have suffered from Schinz disease experience. This occurs due to the fact that the device distributes pressure from the heel to the entire plane of the foot, while keeping the arches in the correct position and not allowing them to fall.
Good quality insoles also improve the blood supply to the lower leg and prevent it from stagnating and constantly feeling tired.
Of the physiotherapeutic procedures to which the patient is referred, the following can be noted:
- Electrophoresis with novocaine and analgin.
- Ozokerite.
- Ultrasound and microwave therapy.
To eliminate discomfort, apply ice compresses, painkillers, non-steroidal anti-inflammatory drugs, incl. Ibuprofen.
Disease prevention
To prevent osteochondropathy of the calcaneus, it is recommended to wear loose shoes.
Prevention of spinal osteochondropathy involves physical therapy exercises to create a muscle corset. Strenuous physical activity should be limited. Wearing a corset for this disease is ineffective.
A good prevention of osteochondropathy of the femur is massage and swimming.
To prevent osteochondropathy of the tibial tubercle, athletes are recommended to sew 2-4 cm thick foam pads into their uniform during training.
Video from YouTube on the topic of the article:
The information is generalized and is provided for informational purposes. At the first signs of illness, consult a doctor. Self-medication is dangerous to health!
Osteochondropathies
Osteochondropathies
– a group of cyclical, long-term diseases, which are based on malnutrition of bone tissue with its subsequent aseptic necrosis. Secondary clinical and radiological manifestations of osteochondropathy are associated with resorption and replacement of damaged areas of bone. Osteochondropathies include Legg-Calvé-Perthes disease, Ostgood-Schlatter disease, Köhler disease, Scheuermann-Mau disease, Schinz disease, etc. Diagnosis of osteochondropathy is based on ultrasound, x-ray and tomographic data. Treatment includes immobilization, physiotherapy, vitamin therapy, exercise therapy. Surgical treatment is performed according to indications.
Classification
In traumatology, there are four groups of osteochondropathy:
- Osteochondropathies of the metaphyses and epiphyses of long tubular bones. This group of osteochondropathy includes osteochondropathy of the sternal end of the clavicle, phalanges of the fingers, hip joint, proximal metaphysis of the tibia, heads of the II and III metatarsals.
- Osteochondropathies of short cancellous bones. This group of osteochondropathy includes osteochondropathy of the vertebral bodies, the lunate bone of the hand, the navicular bone of the foot, and the sesamoid bone of the first metatarsophalangeal joint.
- Osteochondropathies of the apophyses. This group of osteochondropathy includes osteochondropathy of the pubic bone, apophyseal discs of the vertebrae, calcaneal tuberosity and tibial tuberosity.
- Wedge-shaped (partial) osteochondropathy affecting the articular surfaces of the elbow, knee and other joints.
Taking into account the characteristics of the pathological process, four stages of the disease are distinguished:
- First. Necrosis of bone tissue. Lasts up to several months. The patient experiences mild or moderate pain in the affected area, accompanied by impaired limb function. Palpation is painful. Regional lymph nodes are usually not enlarged. X-ray changes during this period may be absent.
- Second. "Compression fracture." Lasts from 2-3 to 6 or more months. The bone “sags”, damaged bone beams wedge into each other. Radiographs reveal homogeneous darkening of the affected parts of the bone and the disappearance of its structural pattern. When the epiphysis is damaged, its height decreases and an expansion of the joint space is detected.
- Third. Fragmentation. Lasts from 6 months to 2-3 years. At this stage, the dead areas of bone are reabsorbed and replaced by granulation tissue and osteoclasts. Accompanied by a decrease in bone height. Radiographs reveal a decrease in bone height, fragmentation of the affected parts of the bone with a chaotic alternation of dark and light areas.
- Fourth. Recovery. Lasts from several months to 1.5 years. The shape and, somewhat later, the structure of the bone are restored.
Osteochondropathies
Perthes disease
The full name is Legg-Calvé-Perthes disease. Osteochondropathy of the hip joint. Affects the head of the hip bone. It most often develops in boys aged 4-9 years. The occurrence of osteochondropathy may be preceded (not necessarily) by trauma to the hip joint.
Perthes disease begins with a slight lameness, which is later joined by pain in the area of the injury, often radiating to the knee joint. Gradually, the symptoms of osteochondropathy intensify, movements in the joint become limited. Upon examination, mild atrophy of the muscles of the thigh and lower leg, limitation of internal rotation and abduction of the hip are revealed. Possible pain when loading the greater trochanter. Often the affected limb is shortened by 1-2 cm, caused by upward subluxation of the hip.
Osteochondropathy lasts 4-4.5 years and ends with restoration of the structure of the femoral head. Without treatment, the head becomes mushroom-shaped. Since the shape of the head does not correspond to the shape of the acetabulum, deforming arthrosis develops over time. For diagnostic purposes, ultrasound and MRI of the hip joint are performed.
In order to ensure restoration of the shape of the head, it is necessary to completely unload the affected joint. Treatment of osteochondropathy is carried out in a hospital with bed rest for 2-3 years. Skeletal traction may be applied. The patient is prescribed physio-vitamin and climate therapy. Constant exercise therapy is of great importance to maintain the range of motion in the joint. If the shape of the femoral head is abnormal, osteoplastic surgery is performed.
Ostgood-Schlatter disease
Osteochondropathy of the tibial tuberosity. The disease develops at the age of 12-15 years, boys are more often affected. Swelling gradually appears in the affected area. Patients complain of pain that worsens when kneeling and walking up stairs. The function of the joint is not impaired or only slightly impaired.
Treatment of osteochondropathy is conservative, carried out on an outpatient basis. The patient is prescribed a limitation of the load on the limb (in case of severe pain, a plaster splint is applied for 6-8 weeks), physiotherapy (electrophoresis with phosphorus and calcium, paraffin baths), and vitamin therapy. Osteochondropathy proceeds favorably and ends with recovery within 1-1.5 years.
Köhler's disease-II
Osteochondropathy of the heads of the II or III metatarsal bones. It most often affects girls and develops at the age of 10-15 years. Köhler's disease begins gradually. Periodic pain occurs in the affected area, lameness develops, which goes away when the pain disappears. Upon examination, slight swelling is revealed, sometimes - hyperemia of the skin on the back of the foot. Subsequently, shortening of the second or third finger develops, accompanied by a sharp limitation of movements. Palpation and axial load are sharply painful.
In comparison with the previous form, this osteochondropathy does not pose a significant threat to subsequent impairment of limb function and the development of disability. Outpatient treatment with maximum unloading of the affected part of the foot is indicated. Patients are given a special plaster boot, vitamins and physical therapy are prescribed.
Köhler's disease-I
Osteochondropathy of the navicular bone of the foot. Develops less frequently than previous forms. It most often affects boys aged 3-7 years. Initially, pain in the foot appears for no apparent reason, and lameness develops. Then the skin on the back of the foot turns red and swells.
Treatment of osteochondropathy is outpatient. The patient is limited in the load on the limb, in case of severe pain, a special plaster boot is applied, and physical therapy is prescribed. After recovery, it is recommended to wear shoes with arch support.
Schinz's disease
Osteochondropathy of the calcaneal tuberosity. Schinz disease develops rarely, usually affecting children aged 7-14 years. Accompanied by the appearance of pain and swelling. Treatment of osteochondropathy is outpatient and includes exercise limitation, calcium electrophoresis and thermal procedures.
Sherman-Mau disease
Osteochondropathy of the vertebral apophyses. Common pathology. Scheuermann-Mau disease occurs in adolescence, most often in boys. Accompanied by kyphosis of the middle and lower thoracic spine (round back). The pain may be mild or completely absent. Sometimes the only reason to visit an orthopedist is a cosmetic defect. Diagnosis of this type of osteochondropathy is carried out using radiography and CT scan of the spine. Additionally, to study the condition of the spinal cord and ligamentous apparatus of the spinal column, an MRI of the spine is performed.
Osteochondropathy affects several vertebrae and is accompanied by severe deformation that remains for life. To maintain the normal shape of the vertebrae, the patient must be provided with rest. The patient should remain in bed in a supine position for most of the day (if pain is severe, immobilization is performed using a posterior plaster bed). Patients are prescribed massage of the abdominal and back muscles, therapeutic exercises. With timely, correct treatment, the prognosis is favorable.
Calvet disease
Osteochondropathy of the vertebral body. Calve's disease develops at the age of 4-7 years. The child, for no apparent reason, begins to complain of pain and a feeling of fatigue in the back. Upon examination, local pain and protrusion of the spinous process of the affected vertebra are revealed. Radiographs reveal a significant (up to ¼ of normal) decrease in vertebral height. Usually one vertebra in the thoracic region is affected. Treatment of this osteochondropathy is carried out only in a hospital. Rest, therapeutic exercises, and physiotherapy are indicated. The structure and shape of the vertebra is restored within 2-3 years.
Partial osteochondropathy
They usually develop between the ages of 10 and 25 and are more common in men. About 85% of partial osteochondropathy develops in the knee joint. As a rule, an area of necrosis appears on the convex articular surface. Subsequently, the damaged area can separate from the articular surface and turn into an “articular mouse” (a loose intra-articular body). Diagnosis is carried out by ultrasound or MRI of the knee joint. In the first stages of the development of osteochondropathy, conservative treatment is carried out: rest, physiotherapy, immobilization, etc. With the formation of an “articular mouse” and frequent joint blockades, surgical removal of the free intra-articular body is indicated.
Osteochondritis dissecans (Koenig's disease)
Osteochondritis dissecans of articular surfaces are osteochondropathy with a single etiopathogenesis and different anatomical localization. The disease is based on impaired blood circulation in a limited area of the epiphysis. As a result, marginal aseptic necrosis of a small area of subchondral cancellous bone is formed, the shape of which resembles a lentil, biconvex or plano-convex lens. Subsequently, this bone fragment, covered with hyaline cartilage, is completely separated into the joint cavity and transformed into a “joint mouse” that blocks movements in the joint.
The etiology of the disease has not been fully elucidated. The vascular theory has received the greatest recognition, according to which avascular necrosis occurs as a result of a reflex spasm or embolism of the terminal vessels supplying a limited area of the epiphysis.
Clinic.
There are 3 stages in the development of the pathological process.
/ the stage of the disease is poor in symptoms: pain in the knee joint of varying intensity is of an uncertain nature, moderate synovitis is possible.
// stage. B the pain becomes more constant and intensifies when walking. Patients experience a feeling of limited movement in the joint, the supporting function of the limb decreases, and lameness may appear.
Stage III occurs after separation of the necrotic osteochondral fragment into the joint cavity. Sometimes it is possible to palpate a freely moving intra-articular body. Its size can range from large lentils to medium-sized beans. When the “articular mouse” is pinched between the articular surfaces, sharp pain and sudden restriction of movements occur—joint blockade. Over time, hypotrophy of the quadriceps femoris muscle develops and arthrosis occurs.
X-ray at the first stage reveals a limited area of bone compaction in the subchondral zone of the convex articular surface of the femoral condyle. It is usually biconvex, reaches dimensions of 1.0×1.5 cm and is limited by a narrow rim of the lucency. Then (in stage II) the compacted osteochondral fragment is demarcated from the maternal bed: the clearing zone around it expands, the fragment begins to protrude into the joint cavity. At the /// stage, a niche is determined in the area of the articular surface of the femoral condyle, and the intra-articular body is found in any part of the knee joint (usually in one of the inversions, and when the joint is blocked, between the articular surfaces).
Treatment for osteochondritis dissecans depends on the stage of the disease.
In stages I and II , conservative treatment is indicated, including limiting the load with the complete exclusion of jumping and running, immobilization of the diseased limb with a plaster splint, physiotherapeutic procedures (phonophoresis of chondroxide or hydrocortisone, electrophoresis of calcium chloride, paraffin-ozokerite applications), the use of chondroprotectors (mucosate, structum) .
Surgical treatment is indicated in stage III of the disease (in the presence of a free osteochondral fragment blocking the joint and the supporting phenomenon of chronic synovitis), and is also the method of choice in stage II of pathological changes.
Osteochondropathy
What is osteochondropathy
The disease is a group of pathologies characterized by improper nutrition of the bone tissue of the musculoskeletal system, which causes necrosis and tissue degeneration. Osteochondropathy occurs over a long period of time and is benign. Mainly affected by pathology are the tibia, pelvis, patella and knee joint, femur, and pubic ischial joint.
Types and causes of occurrence
Pathology develops as a result of impaired blood circulation in individual bone elements. Necrosis of spongy bone is preceded by altered metabolism, genetic predisposition, previous bone injuries and traumatization, and infections. The clinical picture may be aggravated by:
- imbalance of hormones caused by dysfunction of the thyroid gland, adrenal glands, pituitary gland, ovaries,
- metabolic disorders, low metabolic rate,
- lack of calcium, magnesium, minerals, vitamin deficiency,
- unnatural position of the spine,
- overweight and obesity.
There are many types of disease depending on the location of the pathology.
Damage to long spongy bones:
- Legg-Calvé-Peters disease (osteochondropathy of the femoral head),
- Keller's disease II (osteochondropathy of the second and third metatarsals),
- osteochondropathy of the phalanges of the hands,
- osteochondropathy of the sternal region of the clavicle,
- Blunt's disease (osteochondropathy of the tibia).
Damage to short spongy bones:
- Keller's disease I (osteochondropathy of the navicular bones of the feet),
- Kienböck's disease (osteochondropathy of the lunate bone on the hands),
- Calve's disease (osteochondropathy of the vertebral bodies),
- Müller's disease (osteochondropathy of the sesamoid bone of the first metatarsophalangeal joint).
- Schinz-Haglund disease (osteochondropathy of the calcaneus),
- Osgood-Schlatter disease (osteochondropathy of the tibial tuberosity),
- osteochondropathy of the pubic bone,
- Koenig's disease (osteochondropathy of articular surfaces).
The risk group includes young people who are actively involved in sports at the time of the formation of the skeleton. They have a high risk of spontaneous fractures.
Stages and symptoms
The clinical picture worsens as the disease progresses:
- the first stage - there are no symptoms at all or slight pain occurs when moving the limb, which intensifies when pressing on the area of deformity. Lymph nodes are not enlarged. The clinic continues for several months,
- the second stage is a compression fracture lasting up to six months. The joint space widens, the height of the epiphysis decreases, the bones sag and wedge into each other. The structure of bone tissue changes
- the third stage is the fragmentation of the bone into small parts over several years. Necrotic areas are destroyed and replaced by osteoclasts. Bone size decreases
- fourth stage - the bone structure is restored over a period of several months to one and a half years.
The disease develops over three to four years. Inflammation affects tubular bones, vertebral bodies, and bones of the lower extremities. Bones can break under the patient's own weight. The patient complains of:
- pain in a certain position, increasing with exercise,
- lameness,
- swelling and swelling without inflammation,
- a change in posture noticeable to the naked eye,
- limited range of motion. If treatment is not started in time, arthrosis develops.
Which doctor should I contact for osteochondropathy?
Initially, in case of diseases of the skeletal system, you need to consult with an orthopedist and rheumatologist, but often the pathological process also affects nerve tissue, so a neurologist is also involved in the treatment.
Treatment methods
Proper treatment reduces the risk of spontaneous fractures and strengthens bones.
Therapy includes five components:
- drug therapy,
- physiotherapy (electrophoresis with calcium or phosphorus, UHF, paraffin baths, warming),
- massotherapy,
- physical therapy, exercises of which are selected individually for each patient,
- wearing a skeletal bandage, plaster boot and other orthopedic devices.
The doctor prescribes specific medications, dosage and treatment regimen in accordance with the identified disease. In the acute period, you need to stay in bed and strain the affected area as little as possible to reduce pain and further destruction of bone tissue.
results
With proper and timely therapy, the disease is easily treatable and deformities of the musculoskeletal system are corrected within several months.
It is possible to avoid joint dysfunction and restore bone structure. It is important to follow every recommendation from a specialist at the Kuntsevo Medical and Rehabilitation Center in order to prevent cosmetic defects during recovery.
Rehabilitation and lifestyle restoration
To prevent a relapse and return to your normal lifestyle, you need to eat right and saturate your body with useful vitamins and microelements. You should wear only orthopedic shoes and do not lift heavy objects. Swimming has a beneficial effect on the musculoskeletal system.
You can't do without figure correction. It is necessary to reduce body weight and maintain weight within normal limits to avoid bone injury.
Main types and symptoms of osteochondropathy, their diagnosis and treatment
Each type of disease is characterized by its own symptoms, but some signs are common:
- Pain – constant or occurring with certain movements.
- Swelling over the affected area without signs of inflammation.
- Changes in posture and gait, the appearance of lameness.
- Violation of cellular nutrition of muscles, decrease in their tone.
- Due to the weakening of the bone structure, fractures easily occur not only after physical exertion, but also from the patient’s own weight.
Osteochondropathy of the femoral head (Perthes disease)
The disease is more often found in boys aged 4–13 years, and occurs after injury.
There are the following stages of the disease:
- Necrosis (death) of bone tissue. X-ray shows the presence of osteoporosis.
- Changes in the shape of the head of the femur, its flattening, resulting from its fracture after loading.
- Fragmentation is the gradual resorption of compressed and dead spongy bone tissue.
- Osteosclerosis is the regeneration of a flattened head with proper treatment.
- Deforming arthrosis – occurs in the absence of timely treatment; the head of the femur is deformed, its functions are impaired.
The onset of the disease is hidden, without any symptoms. Later, patients complain of pain in the hip joint, radiating to the knee joint. The pain goes away overnight, so patients do not immediately seek help. Restrictions in hip movement gradually appear, and the muscles of the limb slightly atrophy. Laboratory examination does not reveal any abnormalities.
An important role in diagnosing the disease is played by an x-ray of the hip joint, performed in two projections. Depending on the stage of development of the pathological process, osteoporosis, deformation, and a decrease in the size of the femoral head are detected on the x-ray.
Treatment for Perthes disease is long-term, sometimes about five years. The choice of treatment method depends on the stage of development of the disease. Two types of treatment are used:
- Conservative – consists of maintaining bed rest, unloading the hip joint using the cuff traction method. They also carry out massage and physiotherapeutic procedures (electrophoresis, UHF, paraffin baths).
- Surgical - its methods depend on the stage of the disease and the degree of deformation of the femoral head. After the operation, rehabilitation of patients in rehabilitation centers and balneological resorts is mandatory.
Osteochondropathies of the spine
- Osteochondropathy of the vertebral bodies (Calvé's disease) - affects the lower thoracic or upper lumbar vertebra in boys 7–14 years old. Signs of the disease are increasing pain in the area of the affected vertebra; X-ray examination reveals flattening of the vertebral body with its simultaneous expansion.
Treatment is non-operative, patients are prescribed bed rest, the spine is fixed using a plaster corset (plaster bed). Later, corrective gymnastics and wearing a reclining corset are prescribed. Treatment lasts from two to five years. If the vertebral deformity progresses, surgery is performed.
- Osteochondropathy of the apophyses of the vertebral bodies (Scheuermann-Mau disease) is more common in adolescents 11–17 years old. Symptoms of the disease include back pain, increased fatigue and decreased tone of the back muscles, and changes in posture. The x-ray shows scoliotic deformation of the spine, changes in the shape of the vertebrae, and a decrease in the height of the intervertebral discs.
Conservative treatment is prescribed: reclining gymnastics, swimming, underwater massage and underwater traction.
- Kümmel's disease (traumatic spondylitis) - occurs in men after injuries to the thoracic vertebra. Symptoms do not appear immediately: when the pain passes after the injury, an asymptomatic period begins, lasting from several months to several years. Then patients begin to feel pain in the thoracic spine. X-ray reveals wedge-shaped deformation of the injured vertebra, osteoporosis.
Treatment consists of following bed rest for 4 weeks, wearing a corset, and performing therapeutic exercises.
Osteochondropathies of the foot
- Köhler's disease Ι is osteochondropathy of the navicular bone of the foot. The disease is diagnosed in children 3–12 years old. Symptoms: the dorsum of the foot swells, severe pain occurs when walking. An x-ray shows deformation of the scaphoid bone and compaction of the bone structure.
Treatment is carried out without surgery; the limb is unloaded by applying a plaster cast for one and a half months. Later – electrophoresis, wearing orthopedic shoes, therapeutic massage.
- Köhler's disease ΙΙ is osteochondropathy of the metatarsal head. Patients complain of swelling in the metatarsal bones and severe pain when walking barefoot. If the disease is not diagnosed on time, deforming arthrosis of the metatarsophalangeal joint develops.
Treatment consists of applying a plaster boot. Massage, hydrogen sulfide baths, ultrasound, mud applications, exercise therapy, and wearing orthopedic shoes are also recommended. Duration of therapy is up to three years. For deforming arthrosis, surgery is prescribed.
- Haglund-Sever disease is an osteochondropathy of the calcaneal tubercle. It occurs mainly in girls 13–16 years old. Symptoms: pain when walking, redness and swelling in the area where the Achilles tendon attaches. The treatment is conservative, the foot is provided with complete immobility, and orthopedic shoes are subsequently prescribed.
Osteochondropathies of the knee
- Osgood-Schlatter disease is an aseptic necrosis of the tibial tuberosity. The disease is hereditary and occurs in boys 13–18 years old and girls 10–11 years old; is the most common cause of knee pain in adolescents. The course of the disease is chronic, the acute period lasts up to 3 weeks, resulting in sclerosis of sparse areas of the bone. Rest, cold on the area of inflammation, and orthopedic devices to immobilize the limb are prescribed.
- Koenig's disease is a lesion of the knee joint. It most often occurs in young people aged 18 years. Patients feel swelling of the knee joint and limited mobility. The most accurate diagnosis is using MRI (magnetic resonance imaging). Treatment is surgical, arthroscopy of the knee joint is performed.
Symptoms and treatment of osteochondropathy
Osteochondropathy is the general name for bone diseases of aseptic (non-infectious) etiology, causing necrotic processes in the area of the spongy substance of the epiphyses (the end part of the tubular bone from which the joint is formed). The development of the disease leads to gradual deformation and destruction of the joint, accompanied by curvature of the affected bone. The disease can affect any bone of the skeleton, but pathology of the leg bones is more likely to develop. The hip, knee, lower leg and foot, which bear the bulk of the load during movement, are more at risk of developing pathology. Most often, osteochondropathy of bones occurs in children and adolescents aged 5 to 16 years, but sometimes this diagnosis is also made to older young people - up to 20 years.
Main causes of osteochondropathy
According to statistics, osteochondropathy constitutes approximately 2.5–3% of the total number of identified osteoarticular pathologies. Medical science has not yet identified clear reasons for the development of osteochondropathy, since this bone disease has a wide variety of forms. But most experts agree that the cause of the disease is a disruption of the normal blood supply to various parts of the skeletal system.
The lack of regeneration stimulants supplied with the blood causes a failure in the recovery processes. The bone tissue of the lower extremities in places of nutrient deficiency becomes fragile, easily susceptible to injury and deformation, and osteophytes - bone growths - develop in places of greatest load on the joint. Simultaneously with the spongy substance that makes up the head of the joint, the cartilaginous membrane surrounding it is also destroyed. As a result, the process leads to necrosis - the gradual death of osteochondral cells.
The following factors can provoke local circulatory disorders leading to the development of osteochondropathy:
- Limb injuries. During restoration (fusion) after injury to bone and cartilage tissue, partial pinching of a blood vessel may occur, leading to a limitation of the blood flow through it;
- Hormonal imbalance that occurs during the restructuring of body systems during puberty (adolescence);
- Rapid growth, leading to a deficiency in the body of phosphorus salts, calcium, and other microelements necessary to strengthen bones;
- Lagging development of the blood supply system from skeletal growth in adolescence;
- Excessive load on the bone apparatus in childhood and adolescence - sports or choreography;
- Physical inactivity is a common phenomenon among modern teenagers who are addicted to computer games and social networks, leading to stagnation of blood flow;
- Deficiency in the diet of protein necessary to strengthen the structure of muscles and osteochondral tissue;
- Lack of vitamins;
- Excess weight, which not only increases the chronic load on the joints, but also deprives them of a significant volume of blood due to the need to supply it to adipose tissue;
- Congenital anomalies of the development of the osteoarticular apparatus, such as dysplasia - underdevelopment of the joint;
- Infections of various etiologies;
- Endocrine pathologies
- Hereditary predisposition. If one of the parents has ever suffered from osteochondropathy, the likelihood of developing it in the child increases significantly.
Stages and symptoms of osteochondropathy
Classification of osteochondropathy by stage and stage depends on the degree of damage. Experts distinguish the following stages of osteochondropathy:
- The initial stage lasts several months and leads to the development of necrosis of osteochondral tissues;
- Moderate stage - ends with a compression fracture, in which partial destruction and wedging of bones into each other occurs. Lasts up to six months;
- The fragmentation stage lasts up to three years. At this stage, the area of bone tissue affected by the disease begins to be reabsorbed and replaced by granulation cells;
- The recovery stage after a course of therapy is individual in nature and lasts from several months to one and a half years. The shapes and structures of the affected bones are completely restored at this stage.
It takes 2-4 years from the initial stage to the recovery stage. Each type of osteochondropathy of the lower extremities has its own specific symptoms:
- Damage to the hip joint, also known as Legg-Calvé-Perthes disease, is manifested by pain in the area of damage radiating to the knee, limited dynamics of the joint, and partial atrophy of the muscles of the thigh and lower leg. The sore leg may become shorter by one and a half to two centimeters;
- When the disease is localized in the area of the tibial tuberosity, Osgood-Schlatter disease is diagnosed. It is characterized by swelling and swelling of the affected area, pain that intensifies with exercise (climbing stairs, kneeling), mild dysfunction of the knee joint;
- Disease of the navicular bone of the foot, or Keller disease 1, causes foot pain and lameness. Redness and swelling are rare;
- Osteochondropathy of the metatarsal bones (Keller's disease 2) is expressed in the shortening of the 2nd and 3rd toes, limited dynamic capabilities, redness of the skin in this area;
- Schinz's disease (osteochondropathy of the calcaneal tubercle) has a poor clinical picture, expressed in swelling and pain in the affected area.
Similar symptoms are characteristic of many osteoarticular pathologies. For proper treatment, it is important to differentiate the listed types of osteochondropathy from other diseases of the lower extremities. An experienced orthopedic surgeon will be able to make the correct diagnosis after a complete examination of the patient.
Osteochondropathy of the tibial tuberosity (Osgood-Schlatter disease)
In the scientific literature it is known as aseptic necrosis of the tibial tuberosity, tibial apophysitis, Lanelong-Osgood-Schlatter disease.
The basis of the disease is a violation of the ossification processes of the tibial tuberosity. Osteochondropathy often develops for no apparent reason, however, sometimes it is possible to establish a connection with repeated injury or increased function of the quadriceps femoris muscle (for example, during sports or ballet).
Clinic.
There is swelling and local pain in the area of the tibial tuberosity, which intensifies with palpation. Patients often say that they “…are growing a new kneecap.” Often there is a pronounced increase in the apophysis of the tibia (2 times or more). Movements in the knee joint are painful, especially after physical activity. The sharpest pain occurs when “kneeling.” An extreme degree of flexion of the limb at the knee joint is accompanied by severe pain, which often persists even at rest.
When radiographically diagnosing Osgood-Schlatter disease, it is necessary to keep in mind the many variants of normal ossification of the tibial apophysis. Most often, the apophysis ossifies in the form of a trunk-shaped process at the age of 10-13 years, but there are variants with additional small ossification nuclei. The fusion of the apophysis with the metaphysis occurs by 16-18 years.
When diagnosing, one should always take into account the discrepancy between the significant bulging of the tuberosity on clinical examination and the almost normal size of the apophysis on radiographs. Preference should be given to clinical data.
The disease lasts about a year, and sometimes several years, and ends with the restoration of the structure of the apophysis. The function of the knee joint is usually not affected.