With FPN, the fetus experiences oxygen starvation. There is a delay in its growth and development. The likelihood that an unborn child will suffer from intrauterine infections and harmful metabolic products increases significantly. Violation of the hormonal function of the placenta can cause premature birth and the occurrence of various anomalies in labor.
The consequences of placental insufficiency can be dire. FPN can lead to fetal death. If a child is born, then his adaptation to the world around him will be much more difficult than that of an absolutely healthy baby.
In addition, the newborn may have congenital anomalies (for example, hip dysplasia, torticollis), and encephalopathy. He will be more susceptible to intestinal and respiratory infections.
About the placenta
The placenta is a temporary organ that is formed exclusively during pregnancy (from 16 weeks) and performs a number of essential functions necessary for the successful development and growth of the unborn child. First of all, the placenta carries out gas exchange - oxygen is delivered from the mother’s blood through the utero-placental-fetal system to the unborn baby, and, on the contrary, carbon dioxide comes from the fetal circulatory system into the woman’s bloodstream.
The placenta is also involved in delivering nutrients to the fetus that are necessary for its growth. In addition, the placenta plays the role of an endocrine organ during gestation and synthesizes a number of hormones, without which the physiological course of pregnancy would be impossible (progesterone, placental lactogen, estrogens, hCG and others).
But do not forget that the placenta easily allows harmful substances (nicotine, alcohol, drugs) to pass through, which adversely affect the fetus.
Functions of the placenta during pregnancy
The placenta (fetal place) is the organ that connects the child with the mother’s body. The fetal place is formed at 14-16 weeks. In the early stages of pregnancy, all the functions of the placenta are performed by the chorion (one of the membranes of the fertilized egg).
The shape of the placenta resembles a round, flat disc. It is penetrated by blood vessels through which nutrients flow to the fetus. By the time the baby is born, the fetal place weighs about 500 g and reaches a diameter of up to 16 cm.
Normally, the placenta is attached to one of the walls of the uterus. In some cases, the fetal place drops too low and reaches the cervix, blocking the internal os. During pregnancy, the placenta may migrate and rise higher to the fundus of the uterus. Placenta previa is a condition in which the fetal site remains at the level of the cervix after 32 weeks. In this situation, the birth of a child is only possible through a caesarean section.
Functions of the placenta:
- supply of nutrients to the fetus;
- gas exchange (passage of oxygen and removal of carbon dioxide);
- protection from the penetration of hazardous substances (medicines, maternal antibodies);
- synthesis of progesterone and other hormones.
If the placenta does not perform its functions, it is said to be insufficient. Why does this pathology develop during pregnancy?
What is fetoplacental insufficiency
Placental insufficiency (synonym - fetoplacental insufficiency) is a complex symptom complex that is caused by morphological and functional changes in the placenta (that is, its functions and structure are disrupted).
Fetoplacental insufficiency of the fetus is nothing more than a disorder of blood flow in the mother-placenta-fetus system. In the case of significant and progressive these disorders, placental insufficiency leads to delayed development of the fetus, and in especially severe cases it causes intrauterine hypoxia and even death.
Classification
Placental insufficiency is classified according to several criteria:
Depending on the moment and mechanism of development:
- primary, which is diagnosed before 16 weeks of gestation and is caused by a violation of the process of implantation and/or placentation;
- secondary, which arose when the placenta was already formed, that is, after 16 weeks under the influence of external factors affecting the fetus and placenta;
Depending on the clinical course:
- acute, usually associated with either placental abruption of a normal or low-localized placenta, usually develops during childbirth, but can occur at any stage of gestation;
- chronic placental insufficiency occurs at any time of gestation and is divided into compensated, when there are metabolic disorders in the placenta, but there are no circulatory disorders in the mother-placenta and fetus-placenta systems, which is confirmed by Doppler studies, and decompensated placental insufficiency, which is said to progress pathological process in the fetus-placenta-mother system (confirmed by Doppler).
In turn, the decompensated form of pathology is divided into several degrees of placental insufficiency (see also degree of placental maturity):
- 1a degree, when there is a violation of blood flow only in the uteroplacental circle;
- 1b degree, when there is a circulatory disorder only in the fetal-placental circle;
- 2nd degree - circulatory disorders occurred in both circles, but they do not exceed critical values;
- 3rd degree – a condition that threatens the life of the fetus, since the level of disorders in the fetal-placental circle has reached a critical limit.
In addition, it is known that in 60% or more cases, placental insufficiency leads to intrauterine growth retardation of the baby, so it is divided into:
- fetoplacental insufficiency with IUGR;
- fetoplacental insufficiency, fetal development delay is not detected.
Forms of the disease
There are several varieties and classifications of the disease. For example, FPN is divided into chronic and acute forms, as well as compensated and decompensated varieties.
The acute form of insufficiency is characterized by serious disruptions in blood flow, which entails intrauterine death of the fetus. It is not possible to prevent such developments. The chronic form of FPN is characterized by long-term development, but the main cause of the disorders remains the same - deviation of blood circulation in the placenta.
A compensated or secondary variety has a positive prognosis. The intrauterine development of the fetus does not undergo changes, and it adapts to disturbances in the female body. This arrangement is possible in cases where the compensatory characteristics of the mother’s body are fully manifested.
The decompensated type of pathology does not entail a risk factor for death, but the problem leads to serious changes in the fetus, which in turn can provoke acute oxygen deficiency and developmental delay (physiological or psychological). Absolute PN is more dangerous than relative PN.
Pathology is also classified according to degrees: insufficiency of 1st degree (1a) is the highest indicator, then there is an anomaly of 2nd degree, etc.
Causes
The causes of placental insufficiency of the fetus are very diverse and can be conditionally divided into 2 groups:
- endogenous, that is, acting from within the body (for example, genetic and hormonal factors, or deficiency of decidua enzymes or bacterial and/or viral infections);
- exogenous – make up a larger number of factors affecting the fetal-placental blood flow “from the outside”.
So, there are 5 main groups of reasons leading to the development of this pathological condition:
Social, everyday and/or natural circumstances
This group of factors includes both exposure to unfavorable external factors (radioactive radiation, gas pollution, electromagnetic radiation), which can affect the reproductive cells even before pregnancy, as well as poor nutrition, stressful situations, occupational hazards, excessive physical activity, and the use of household chemicals . In addition, social factors include smoking, abuse of alcoholic beverages, drugs, and excessive consumption of strong coffee or tea.
Complicated course of the gestation period
First of all, it is worth mentioning gestosis, which in 32% of cases leads to the development of placental insufficiency and the threat of termination of pregnancy (50 - 77%). Also contributing to the occurrence of the described pathological process can be postterm pregnancy or pregnancy with more than one fetus, placenta previa and antiphospholipid syndrome, Rh-conflict pregnancy and genitourinary infections, the woman’s age (over 35 and under 18 years).
Pathology of the reproductive system currently or in history
This group of factors includes tumors of the uterus and ovaries, menstrual irregularities, multiple births, and especially abortions, fetal death during pregnancy or a history of the birth of hypotrophic children, recurrent miscarriage and premature birth, infertility and inflammatory processes of the genital organs.
Clinical picture
Clinical manifestations of placental insufficiency depend on its form. In the case of the development of chronic compensated placental insufficiency, there are no characteristic symptoms of the disease, and the diagnosis is established only by ultrasound and Doppler ultrasound.
If there is acute or chronic decompensated placental insufficiency, then obvious clinical signs appear, primarily those that indicate the development of intrauterine fetal hypoxia.
- At first, the pregnant woman feels frequent and erratic movements of the fetus, and the doctor notes an increase in its heart rate (tachycardia).
- In the future, in the absence of treatment, movements become less frequent (normally, after 28 weeks of gestation, the expectant mother should feel at least 10 movements of the unborn baby per day), and bradycardia (decreased heartbeat) occurs.
As a rule, placental insufficiency is accompanied by gestosis and the threat of miscarriage, which is not only the cause of its occurrence, but also a consequence (the production of hormones by the placenta is disrupted).
- In the first trimester, the threat of miscarriage can result in a miscarriage or a frozen pregnancy.
- At a later date, due to the permanent threat of miscarriage, pregnancy often ends in premature birth,
- In the third trimester, due to impaired hormone-producing function of the placenta, pregnancy may be carried to term, which aggravates fetal hypoxia.
In addition, a disorder of the endocrine function of the placenta leads to the development of insufficiency of the vaginal epithelium, which creates favorable conditions for the activation of opportunistic vaginal microflora and the development of colpitis. Inflammatory processes in the vagina contribute to infection of the membranes, which can lead to chorioamnionitis and intrauterine infection of the baby.
In addition to the failure of the hormonal function of the placenta, fetoplacental insufficiency causes pathology and excretory function, as a result of which oligohydramnios develops, and in some cases (fetal hemolytic disease or maternal diabetes mellitus) polyhydramnios.
But the most characteristic manifestation of decompensated placental insufficiency is delayed fetal development, which is facilitated by progressive hypoxia. Clinically, developmental delay of the unborn child is established according to external obstetric examination (measuring the size of the abdomen).
Indicators such as the height of the uterine fundus and abdominal circumference lag behind the current stage of pregnancy. The form of intrauterine developmental delay of the unborn child is determined by ultrasound.
- The symmetrical form is characterized by a proportional lag in the weight and length of the fetus, that is, all indicators are reduced to one degree or another.
- Evidence of an asymmetrical form of developmental delay is a disproportionate lag in development of the fetus, that is, the baby’s body length is within normal limits, but its weight is reduced due to a decrease in the circumference of the chest and abdomen (due to a decrease in subcutaneous fatty tissue and a lag in the growth of parenchymal organs: lungs, liver and others).
Fetoplacental insufficiency: a problem of modern obstetrics
Fetoplacental insufficiency (FPI) is a symptom complex in which various disorders occur, both from the placenta and from the fetus, due to various diseases and obstetric complications. The variety of variants of manifestation of FPN, the frequency and severity of complications for the pregnant woman and the fetus, the predominant violation of one or another function of the placenta depend on the duration of pregnancy, the strength, duration and nature of the influence of damaging factors, as well as on the stage of development of the fetus and placenta, the degree of expression of compensatory and adaptive capabilities "mother-placenta-fetus" system.
Causes of FPN
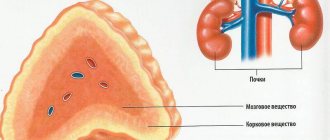
FPN can develop under the influence of various reasons. Disturbances in the formation and function of the placenta can be caused by diseases of the heart and vascular system of the pregnant woman (heart defects, circulatory failure, arterial hypertension and hypotension), pathology of the kidneys, liver, lungs, blood, chronic infection, diseases of the neuroendocrine system (diabetes mellitus, hypo- and hyperfunction thyroid gland, pathology of the hypothalamus and adrenal glands) and a number of other pathological conditions. FPN in anemia is caused by a decrease in the level of iron both in the maternal blood and in the placenta itself, which leads to inhibition of the activity of respiratory enzymes and the transport of iron to the fetus. In diabetes mellitus, metabolism is disrupted, hormonal disorders and changes in immune status are detected. Sclerotic vascular damage leads to a decrease in the supply of arterial blood to the placenta. An important role in the development of FPN is played by various infectious diseases, especially those occurring in an acute form or worsening during pregnancy. The placenta can be affected by bacteria, viruses, protozoa and other infectious agents.
Of no small importance in the formation of FPN is the pathology of the uterus: endometriosis, myometrial hypoplasia, malformations of the uterus (saddle-shaped, bicornuate). Uterine fibroids should be considered a risk factor for FPN. However, the risk of FPN varies among pregnant women with uterine fibroids. The high-risk group includes primiparas aged 35 years and older with a predominantly intermuscular location of large myomatous nodes, especially when the placenta is localized in the area where the tumor is located. The group with a low risk of FPN consists of young women under 30 years of age without severe extragenital diseases, with small myomatous nodes, predominantly subperitoneal, in the fundus and body of the uterus.
Among the complications of pregnancy that most often accompany FPN, the leading place is occupied by gestosis. The threat of miscarriage should be simultaneously considered both as a cause and as a consequence of FPN. Due to the different etiology of FPN when there is a threat of miscarriage, the pathogenesis of this complication has different options, and the prognosis for the fetus depends on the degree of development of protective-adaptive reactions. With a low location or placenta previa, vascularization of the subplacental zone is reduced. The thinner wall of the lower segment of the uterus does not provide the necessary conditions for sufficient vascularization of the placental bed and its normal functioning.
Relatively often, with this pathology, placental abruption occurs, accompanied by blood loss. Multiple pregnancy represents a natural model of FPN as a result of inadequate provision of the needs of two or more fetuses. The basis of FPN in isoserological incompatibility of the blood of mother and fetus most often lies in the processes of impaired maturation of the placenta. The fetus develops anemia and hypoxia, developmental delay occurs due to disturbances in protein synthesis processes and decreased enzyme activity. The functional state of the placenta is largely determined by the degree of its development in accordance with the gestational age and the preservation of protective and adaptive mechanisms. Matching the maturity of the placenta to the gestational age is one of the most important conditions for ensuring adequate development of the fetus and its protection. There is no doubt that the late age of a pregnant woman (over 35 years old) or, conversely, young age (under 17 years old), a burdened medical history (abortions, inflammatory diseases), bad habits, exposure to adverse environmental factors, poor nutrition, social vulnerability and household instability are also contribute to complicated formation of the placenta and disruption of its function [1].
Clinical practice and scientific research results indicate the multifactorial nature of FPN. In this regard, it is almost impossible to identify any single factor in the development of this complication. The listed pathological conditions do not equally influence the development of FPN. Most often, several etiological factors are involved in the development of this pathology, one of which may be leading. Pathological changes that occur during FPN lead to a decrease in uteroplacental and fetoplacental blood flow; decreased arterial blood supply to the placenta and fetus; limitation of gas exchange and metabolism in the fetoplacental complex; disruption of placental maturation processes; decreased synthesis and imbalance of placental hormones. All these changes suppress the compensatory-adaptive capabilities of the “mother-placenta-fetus” system, slow down the growth and development of the fetus, cause a complicated course of pregnancy and childbirth (threat of premature termination of pregnancy, gestosis, premature and late birth, labor anomalies, premature placental abruption and etc.) [5].
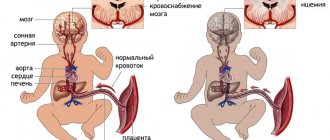
As a result of exposure to damaging factors and the implementation of pathogenetic mechanisms leading to FPN, fetal hypoxia naturally develops. At its initial stages, vasopressor factors are activated in the fetus, the tone of peripheral vessels increases, tachycardia is noted, the frequency of respiratory movements increases, motor activity increases, and cardiac output increases.
Further progression of hypoxia leads to the replacement of tachycardia by bradycardia, arrhythmia appears, and cardiac output decreases. The adaptive response to hypoxia is the redistribution of blood in favor of the brain, heart and adrenal glands with a simultaneous decrease in blood supply to other organs. At the same time, the motor and respiratory activity of the fetus is inhibited [5].
Classification of FPN
It is advisable to classify FPN taking into account the state of protective-adaptive reactions into compensated, subcompensated, decompensated [3].
The compensated form of FPN is characterized by the initial manifestations of the pathological process in the fetoplacental complex. Protective and adaptive mechanisms are activated and experience a certain tension, which creates conditions for the further development of the fetus and the progression of pregnancy. With adequate therapy and management of labor, the birth of a healthy child is possible.
The subcompensated form of FPN is characterized by an increase in the severity of the complication. Protective-adaptive mechanisms are under extreme stress (the capabilities of the fetoplacental complex are practically exhausted), which does not allow them to be implemented sufficiently for an adequate course of pregnancy and fetal development. The risk of complications for the fetus and newborn increases.
In the decompensated form of FPN, there is overstrain and disruption of compensatory-adaptive mechanisms, which no longer provide the necessary conditions for further normal progression of pregnancy. Irreversible morphofunctional disorders occur in the fetoplacental system. The risk of developing severe complications for the fetus and newborn (including their death) increases significantly. The clinical picture of FPN manifests itself in violations of the basic functions of the placenta.
Intrauterine growth restriction
Changes in the respiratory function of the placenta are mainly indicated by symptoms of fetal hypoxia. In this case, the pregnant woman first pays attention to the increased (erratic) motor activity of the fetus, then to its decrease or complete absence. The most characteristic sign of chronic FPN is intrauterine growth retardation. The clinical manifestation of intrauterine growth retardation is a decrease in the size of the pregnant woman’s abdomen (abdominal circumference, height of the uterine fundus) compared to the normative indicators characteristic of a given period of pregnancy.
With a symmetrical form of intrauterine growth retardation, which develops from the early stages of pregnancy, there is a proportional lag in the length and weight of the fetus. At the same time, quantitative indicators of fetometry have lower values compared to individual fluctuations characteristic of a given stage of pregnancy.
The asymmetric form of intrauterine growth retardation is characterized by disproportionate development of the fetus. This form most often occurs in the second or third trimester of pregnancy and is manifested by a lag in fetal body weight with its normal length. The size of the abdomen and chest of the fetus is predominantly reduced, which is associated with a lag in the development of parenchymal organs (primarily the liver) and subcutaneous fatty tissue. The dimensions of the fetal head and limbs correspond to the indicators characteristic of this stage of pregnancy.
Placental dysfunction
A reflection of violations of the protective function of the placenta when the placental barrier is weakened is intrauterine infection of the fetus under the influence of pathogenic microorganisms penetrating the placenta. It is also possible for various toxic substances to penetrate the placental barrier, which also have a damaging effect on the fetus.
A change in the synthetic function of the placenta is accompanied by an imbalance in the level of hormones it produces and a decrease in protein synthesis, which is manifested by intrauterine growth retardation, hypoxia, and pathology of uterine contractile activity during pregnancy and childbirth (long-term threat of premature termination of pregnancy, premature birth, labor abnormalities).
Prolonged and frequent increase in myometrial tone leads to a decrease in arterial blood flow to the placenta and causes venous stagnation. Hemodynamic disorders reduce gas exchange between the body of the mother and the fetus, which makes it difficult for the fetus to receive oxygen and nutrients, remove metabolic products, and contributes to an increase in fetal hypoxia.
Disruption of the endocrine function of the placenta can also lead to post-term pregnancy. A decrease in the hormonal activity of the placenta causes dysfunction of the vaginal epithelium, creating favorable conditions for the development of infection, exacerbation or the occurrence of inflammatory diseases of the urogenital tract. Against the background of a disorder of the excretory function of the placenta and amniotic membranes, a pathological amount of amniotic fluid is observed - most often oligohydramnios, and in some pathological conditions (diabetes mellitus, edematous form of hemolytic disease of the fetus, intrauterine infection, etc.) - polyhydramnios.
Diagnostics of FPN
At the initial stage of development of FPN, the listed clinical signs may be weakly expressed or absent. In this regard, methods of laboratory and instrumental dynamic monitoring of the state of the fetoplacental complex in a high-risk group for the development of FPN become essential. The dominant position in the clinical picture may be occupied by signs of the underlying disease or complication in which FPN developed. The severity of FPN and violations of compensatory and adaptive mechanisms are directly dependent on the severity of the underlying disease and the duration of its course. FPN acquires its most severe course when pathological signs appear during pregnancy up to 30 weeks or earlier. Thus, the most complete information about the form, nature, severity of FPN and the severity of compensatory-adaptive reactions can be obtained from complex dynamic diagnostics [2].
Taking into account the multifactorial etiology and pathogenesis of FPN, its diagnosis should be based on a comprehensive examination of the patient. To establish a diagnosis of FPN and identify the causes of this complication, significant attention should be paid to the correct collection of anamnesis. During the interview, the patient’s age (late or young age of a primiparous woman), her health characteristics, previous extragenital, neuroendocrine and gynecological diseases, surgical interventions, the presence of bad habits are assessed, and her profession, conditions and lifestyle are clarified.
Information about the characteristics of menstrual function, the period of its formation, the number and course of previous pregnancies is of great importance. Menstrual dysfunction is a reflection of the pathology of the neuroendocrine regulation of reproductive function. It is important to assess the course of the current pregnancy, the nature of obstetric complications and, most importantly, the presence of diseases against which pregnancy develops (arterial hypertension or hypotension, pathology of the kidneys, liver, diabetes mellitus, anemia, etc.). You should pay attention to the complaints of a pregnant woman: an increase or suppression of fetal motor activity, pain in the lower abdomen, increased tone of the uterus, the appearance of atypical discharge from the genital tract, which may be accompanied by an unpleasant odor and itching.
During an objective examination, the state of uterine tone is assessed by palpation. The height of the uterine fundus and abdominal circumference are measured and compared with the body weight and height of the pregnant woman, as well as the specified gestational age. Such measurements are important and at the same time the simplest indicators for diagnosing intrauterine growth retardation, oligohydramnios and polyhydramnios. During an external examination of the genital organs and when examining using mirrors, it is necessary to pay attention to the presence of signs of inflammation, the nature of discharge from the genital tract, and to take material from the vaginal wall, from the cervical canal and from the urethra for microbiological and cytological examination [2].
During an echographic examination, the size of the fetus is determined (the size of the head, torso and limbs) and compared with standard indicators characteristic of the expected gestational age. The basis of ultrasound diagnostics to clarify the correspondence of fetal size to the expected gestational age and to identify intrauterine growth retardation is the comparison of fetometric indicators with normative data. An indispensable condition is the assessment of the anatomical structures of the fetus to identify abnormalities of its development. An echographic examination also includes placentography. In this case, the localization of the placenta, the thickness of the placenta, the distance of the placenta from the internal os, the correspondence of the degree of maturity of the placenta to the gestational age, pathological inclusions in the structure of the placenta, the location of the placenta in relation to myomatous nodes or the scar on the uterus are determined. During the study, the volume of amniotic fluid, the structure of the umbilical cord and the location of the umbilical cord loops are assessed [4].
Doppler ultrasound is a highly informative, relatively simple and safe diagnostic method that can be used for comprehensive dynamic monitoring of the state of blood circulation in the “mother-placenta-fetus” system after 18–19 weeks of pregnancy, since by this time the second wave of cytotrophoblast invasion has completed. The nature of hemodynamics in the umbilical cord arteries allows us to judge the state of fetoplacental blood flow and microcirculation in the fetal part of the placenta. To diagnose disturbances in uteroplacental blood flow, studies are performed in the uterine arteries on both sides [4].
An important component of a comprehensive assessment of the fetal condition is cardiotocography (CTG), which is a method of functional assessment of the fetal condition based on recording the frequency of its heartbeats and their changes depending on uterine contractions, the action of external stimuli or the activity of the fetus itself. CTG significantly expands the possibilities of antenatal diagnosis, allowing one to resolve issues of rational pregnancy management tactics.
The final tactics for managing the patient should be developed not only on the basis of an assessment of individual indicators of the state of the fetoplacental complex, but also taking into account the individual characteristics of a specific clinical observation (term and complications of pregnancy, concomitant somatic pathology, results of an additional comprehensive examination, condition and readiness of the body for childbirth, etc.) .d.).
Treatment of pregnant women with FPN
If FPN is detected, it is advisable to hospitalize a pregnant woman in a hospital for in-depth examination and treatment. An exception may be pregnant women with a compensated form of FPN, provided that the treatment initiated has a positive effect and there are the necessary conditions for dynamic clinical and instrumental monitoring of the nature of the course of pregnancy and the effectiveness of the therapy. The leading place in the implementation of therapeutic measures is taken by the treatment of the underlying disease or complication in which the FPN occurred. At present, unfortunately, it is not possible to completely rid a pregnant woman of FPN using any therapeutic interventions. The means of therapy used can only help to stabilize the existing pathological process and maintain compensatory and adaptive mechanisms at a level that allows for the continuation of pregnancy until the possible optimal date of delivery.
The basis of treatment for placental insufficiency is measures aimed at improving uteroplacental and fetoplacental blood flow. Drugs used for this purpose dilate blood vessels, relax the muscles of the uterus, and improve the rheological properties of blood in the “mother-placenta-fetus” system [2].
Treatment of FPN should be aimed at improving uteroplacental and fetoplacental blood flow; intensification of gas exchange; correction of rheological and coagulation properties of blood; elimination of hypovolemia and hypoproteinemia; normalization of vascular tone and contractile activity of the uterus; strengthening antioxidant protection; optimization of metabolic and metabolic processes. A standard treatment regimen for FPN cannot exist due to the individual combination of etiological factors and pathogenetic mechanisms for the development of this complication. The selection of drugs should be carried out individually and differentiated in each specific observation, taking into account the severity and duration of the complication, etiological factors and pathogenetic mechanisms underlying this pathology. The dosage of drugs and the duration of their use require an individual approach. Attention should be paid to correcting the side effects of certain medications.
In the pathogenesis of placental insufficiency, as well as in gestosis, the main thing is endothelial dysfunction. There are three endothelial systems: mother, placenta and fetus. Therefore, the processes occurring in the vascular-platelet unit during placental insufficiency are similar to those that occur during gestosis. And this leads to metabolic disorders in the “mother-placenta-fetus” system and to fetal malnutrition.
The need for magnesium during pregnancy increases 2–3 times due to the growth and development of the fetus and placenta. Magnesium, which is involved in more than 300 enzymatic reactions, is essential for fetal growth. Magnesium ions are involved in the synthesis of DNA and RNA. A successful combination of magnesium with pyridoxine, which ensures protein metabolism, being a cation in more than 50 enzymatic reactions, participating in the synthesis and absorption of amino acids, promotes the formation of hemoglobin in red blood cells, which is especially important for the growing embryo and fetus. Therefore, in the presence of placental insufficiency and fetal malnutrition, it is most advisable to use magnesium preparations.
Magnesium (Magne B6® forte) has a positive effect on the uteroplacental circulation, therefore its use is indicated for the treatment of placental insufficiency and fetal malnutrition. A parallelism has been established between the concentration of magnesium in the blood serum, in the myometrium, and in the placenta.
Magne B6® forte also goes well with angioprotectors, angioactive agents (Trental, Curantil, Mildronate, Actovegin, etc.), with antioxidants - vitamins E, C, group B, etc.
When treating threatened miscarriage and placental insufficiency, magnesium therapy can be combined with the use of vitamin E and other antioxidants, Mildronate, Actovegin, calcium channel blockers (verapamil), Eufillin, Papaverine, Dibazol, No-shpa, antihistamines, physiotherapeutic methods of treatment ( central electroanalgesia, inductotherapy of the perinephric region, hydroionization, etc.).
Treatment for FPN begins and is carried out in a hospital for at least 4 weeks, followed by its continuation in the antenatal clinic. The total duration of treatment is at least 6–8 weeks. To assess the effectiveness of the therapy, dynamic monitoring is carried out using clinical, laboratory and instrumental research methods. An important condition for successful treatment of FPN is that the pregnant woman adheres to an appropriate regimen: proper rest for at least 10–12 hours a day, elimination of physical and emotional stress, and a rational, balanced diet.
One of the leading pathogenetic mechanisms for the development of FPN is disturbances of the uteroplacental and fetoplacental blood flow, accompanied by an increase in blood viscosity, hyperaggregation of erythrocytes and platelets, a disorder of microcirculation and vascular tone, and arterial circulatory insufficiency. Therefore, an important place in the treatment of FPN is occupied by drugs with antiplatelet and anticoagulant action, as well as drugs that normalize vascular tone.
It should be taken into account that a periodic and prolonged increase in uterine tone contributes to impaired blood circulation in the intervillous space due to a decrease in venous outflow. In this regard, in the course of therapy for FPN in patients with symptoms of threatened miscarriage, the prescription of tocolytic drugs is justified.
Thus, placental insufficiency develops during complicated pregnancy, which requires treatment and preventive measures aimed at reducing obstetric pathology. The problem of treating placental insufficiency remains unsolved, so correction of disorders should be better started before pregnancy, which can reduce the incidence of complications in pregnancy, the fetus and the newborn.
Literature
- Fedorova M.V. Placental insufficiency // Obstetrics and gynecology. 1997. No. 6. pp. 40–43.
- Serov V.N. Diagnosis and treatment of placental insufficiency // Breast cancer. 2008. pp. 35–40.
- Kuzmin V.N., Adamyan L.V., Muzykantova V.S. Placental insufficiency in viral infections // M.: 2005. P. 103.
- Shapovalenko S.A. Complex diagnosis and treatment of placental insufficiency in pregnant women at different stages of gestation // Vestnik Ros. Association of Obstetricians and Gynecologists. 2001. No. 2. P. 437.
- Salafia CM Placental pathology and fetal growth restriction // Clin.Obstet.Gynecol. 2007. 40. 7409 RU.MPG.11.02.11.
V. N. Kuzmin , Doctor of Medical Sciences, Professor
MGMSU , Moscow
Contact information for authors for correspondence
Buy an issue with this article in pdf
Diagnostics
Diagnosis of fetoplacental insufficiency begins with collecting anamnesis and complaints. The nature of the menstrual cycle, the presence of pregnancies in the past and their outcome, previous and existing extragenital diseases are clarified. Then a general and external and internal obstetric examination is carried out, during which the woman’s body weight and height, abdominal circumference and fundus height are measured, the tone of the uterus and the condition of the cervix (immature, ripening or mature) are assessed. In addition, during an internal gynecological examination, the doctor evaluates vaginal leucorrhoea, the presence/absence of bleeding and takes a smear for vaginal microflora. If necessary, tests for hidden sexually transmitted infections using the PCR method are prescribed.
Laboratory research methods are important:
- blood for clotting;
- UAC and OAM;
- blood biochemistry (total protein, alkaline phosphatase, glucose, liver enzymes);
- placental lactogen and oxytocinase;
- urine to determine the amount of estriol excreted.
The last 2 tests are necessary to assess the hormone-producing function of the placenta.
The leading place in the diagnosis of the described pathological syndrome is occupied by instrumental research methods:
Ultrasound of the uterus and fetus
When performing an ultrasound, the dimensions of the unborn child are assessed (circumference of the head, abdomen and chest, length of the limbs), which are compared with normal values for a given gestational age, which is necessary to confirm the presence of delayed fetal development. The anatomical structures of the fetus are also carefully assessed for congenital anomalies. In addition, the placenta, its thickness and location, relationship to the internal os and pathological structures (myoma nodes and postoperative scar) are assessed. Thinning or thickening of the placenta, as well as the presence of pathological changes in it (calcifications, infarctions, cysts, etc.) indicate the presence of its insufficiency. During an ultrasound scan, it is important to assess the degree of maturity of the placenta:
- zero – homogeneous placenta with a smooth “maternal” surface (chorionic plate);
- the first is a homogeneous placenta with small echogenic areas, the “maternal” surface is tortuous;
- second - echogenic areas become more extensive, the convolutions of the “maternal” surface go deep into the placenta, but do not reach the basal layer;
- the third is the penetration of the convolutions of the “maternal” surface to the basal layer, which form circles, and the placenta itself acquires a pronounced lobular structure.
If the 3rd degree of maturity is determined at a gestation period of less than 38 weeks, they speak of premature aging or maturation of the placenta, which also confirms its insufficiency. The amount of amniotic fluid is also determined (the amniotic fluid index is calculated) and the presence/absence of low or polyhydramnios (evidence of a violation of the excretory function of the placenta).
Even more interesting:
What is Unidox prescribed for?
Treatment of FPN
With the development of fetoplacental insufficiency, the main goal of treatment is to prolong pregnancy and adequate and timely delivery. Pregnant women with decompensated and acute forms of placental insufficiency, with detected fetal developmental delay and when diagnosing disorders of the functional state of the fetus based on the results of CTG, ultrasound and Doppler sonography are subject to mandatory hospitalization.
- Pregnant women are recommended to get enough sleep (at least 8 hours a day) and a healthy, balanced diet. Walking in the fresh air is no less necessary. It is also necessary to give up bad habits.
- To normalize blood flow in the placenta-fetus system, drugs are prescribed that improve tissue metabolism (Actovegin intravenous drip with 5% glucose, then in tablets, ascorbic acid, tocopherol, troxevasin), rheocorrectors (reopoliglucin, rheosorbilact, infucol), antispasmodics and tocolytics (but -spa, ginipral, magnesium sulfate, magne-B6).
- The administration of aminophylline and a glucose-novocaine mixture by intravenous infusion is indicated.
- To improve the rheological properties of the blood, antiplatelet agents (curantil, trental) and anticoagulants (fraxiparin, clexane - low molecular weight heparins) are prescribed, which “thin” the blood, improve placental-fetal blood flow and prevent the development of pathological formations in the placenta.
- The administration of drugs that improve blood circulation in the brain (nootropil, piracetam) and calcium channel blockers (Corinfar) to reduce uterine tone is indicated.
- In order to normalize metabolism in the placenta, it is recommended to take hormonal drugs (utrogestan, duphaston), vitamins (folic acid, cocarboxylase, ATP) and iron supplements, especially when anemia is detected (sorbifer, tardiferon, see iron supplements for anemia).
- To restore gas exchange in the fetal-placental system, oxygen therapy with humidified oxygen and antihypoxants (cytochrome C, Cavinton, Mildronate) are prescribed. Taking sedatives to relieve brain excitability (motherwort, valerian, glycine) is also indicated.
Treatment for placental insufficiency in a hospital setting should last at least 4 weeks, followed by outpatient treatment. The entire course takes 6 – 8 weeks. The effectiveness of treatment is assessed using CTG, ultrasound scanning of the fetus and placenta and Doppler sonography.
What to do for prevention
Prevention is the most important part during pregnancy. Such measures should be started even before the moment of conception in order to exclude most complications, including the threat of developing FPN. Preventive measures are prescribed by a specialist, but the patient has the right to carry them out independently, but after consultation.
To eliminate the risk factor for pathology, the following measures should be taken:
- Lead a healthy lifestyle.
- Stop sexual intercourse in the third month of pregnancy or as directed by a specialist.
- It is recommended to give up alcohol and tobacco products two months before conception. If you use drugs, you should undergo rehabilitation.
- Stabilize the diet. Priority should be vegetables and fruits, steamed food.
- Walk outdoors for at least 30 minutes every day. Ventilate the room.
- If your work activity involves chemical or toxic substances, it is recommended to change jobs or take early maternity leave.
- Eliminate factors contributing to the deterioration of the psycho-emotional plan. Avoid stressful situations without conflict.
- Take fortified preparations containing vitamin E.
- Visit your doctor promptly on the appointed days.
- If any deviations occur, immediately carry out diagnostics.
All of the above preventive measures will help prevent unnecessary complications, including placental insufficiency. The rest of the recommendations are prescribed by the specialist at his own discretion and based on the current condition of the patient, the course of pregnancy, and risk factors.
Doctor's commentary on the consequences of placental insufficiency:
Management of childbirth
Delivery through the natural birth canal is carried out in the presence of a favorable obstetric situation, a mature cervix and compensated placental insufficiency. Childbirth is recommended to be performed with pain relief (epidural anesthesia). If weakness of labor occurs, stimulation is carried out with prostaglandins, and in the second period, obstetric forceps are applied or vacuum extraction of the fetus is performed.
Early delivery (up to 37 weeks) is indicated in the absence of positive dynamics according to ultrasound (fetometric indicators of the fetus) and Dopplerography after 10 days of therapy, as well as in cases of diagnosed fetal malnutrition. If the cervix is immature, delayed fetal development with disorders of its functional state is diagnosed, as well as a complicated obstetric history, age 30 years or older, a cesarean section is performed.
Consequences of FPN
Pregnancy occurring against the background of placental insufficiency, as a rule, leads to the development of the following complications:
- placental abruption
- post-term pregnancy;
- high risk of intrauterine fetal death
- developmental delay or malnutrition of the fetus and the birth of a low birth weight baby;
- intrapartum fetal hypoxia leading to cerebrovascular accident in the newborn;
- respiratory pathology (pneumonia and pneumopathy);
- neurological status disorders;
- intestinal disorders;
- tendency to colds;
- fetal malformations.
Placental insufficiency (or as it is also called fetoplacental insufficiency (FPI)) is one of the most common complications of pregnancy.
Placental insufficiency refers to dysfunction of the placenta that occurs under the influence of various factors. With this disorder, the fetus does not receive enough oxygen and development of FGR (fetal growth retardation) is possible.
Types of placental insufficiency
Placental insufficiency in time and mechanism of occurrence is:
- Primary - occurs before 16 weeks of pregnancy and is associated with disturbances in the processes of implantation and placentation.
- Secondary - develops against the background of an already formed placenta (after the 16th week of pregnancy) under the influence of factors external to the fetus and placenta.
Placental insufficiency can be:
- Compensated placental insufficiency is when the processes in the placenta are disrupted, but there are no disturbances in the mother-placenta-fetus system.
- Decompensated placental insufficiency is when irreversible disorders occur in the fetoplacental system that do not provide the necessary conditions for the further normal development of pregnancy.
Types of placental insufficiency according to the presence of FGR (fetal growth retardation): placental insufficiency without FGR and placental insufficiency with FGR.
Chronic and acute placental insufficiency
Acute placental insufficiency is most often associated with abruption of a normal or low-lying placenta and occurs mainly during childbirth. Acute placental insufficiency is observed much less frequently than chronic placental insufficiency.
Chronic placental insufficiency can occur at various stages of pregnancy, especially in women at high risk.
Factors that provoke the appearance of placental insufficiency during pregnancy include:
- primiparous women over 35 years of age and under 18;
- malnutrition, psycho-emotional overload;
- Iron-deficiency anemia;
- endocrine diseases (diabetes mellitus, thyroid diseases), diseases of the cardiovascular system (heart defects, hypertension), kidneys, lungs;
- sexually transmitted infections, as well as menstruation disorders, miscarriage, past abortions;
- chronic gynecological diseases - endometriosis, uterine fibroids, abnormalities of the reproductive system (uterine malformations).
- diseases during real pregnancy (preeclampsia, threatened miscarriage, multiple pregnancies, abnormalities in the location and attachment of the placenta, infections, including urogenital ones.
Types of disease
Conventionally, doctors distinguish four types of pathology. This division is very arbitrary - sometimes even the attending physicians themselves can neglect it:
- primary placental insufficiency. Usually formed in the first trimester of pregnancy. Unfortunately, it may go unnoticed - especially in the case when the doctor did not find any obvious disorders/pathologies during the examination;
- secondary placental insufficiency. It often appears at a later stage - usually the end of the second/beginning of the third trimester. The doctor can easily recognize such a pathology during a routine examination of the patient;
- acute placental insufficiency. This pathology is characterized by a sharp disruption of the uteroplacental blood flow due to detached placenta and the resulting hematoma. As a result, the fetus may experience acute hypoxia, which in some cases can lead to its death. In this condition, the pregnant woman needs urgent hospital treatment;
- chronic placental insufficiency. With this pathology, blood circulation in the “children's place” is gradually disrupted, due to the fact that it gradually loses the ability to adapt to new conditions due to disruption of cellular metabolism.
Diagnosis of placental insufficiency
Pregnant women at risk for the development of placental insufficiency require regular monitoring. During the examination, the doctor will pay attention to the following signs:
- height and weight of the pregnant woman;
- abdominal circumference, uterine fundus height (UFH) (if the difference in the numerical value of the gestational age and UFH, expressed in centimeters, is more than three, we can talk about the presence of FGR; this criterion allows us to identify about 50% of pregnancies complicated by FGR);
- uterine tone (uterine tone is increased when there is a threat of miscarriage);
- presence of bloody discharge from the genital tract;
- the number of fetal movements and the nature of the heartbeat (changes in heart rate).
Three main methods are used for diagnosis: ultrasound, Doppler and cardiotocography (CTG).
In the second and third trimesters of pregnancy, during ultrasound screening (20–24 weeks and 30–34 weeks), as well as for additional indications, ultrasound fetometry and Doppler examination of blood flow in the arteries and veins of the mother-placenta-fetus functional system are performed.
When performing an ultrasound, in addition to fetometry, which makes it possible to establish a diagnosis of FGR, the diagnostician pays attention to the condition of the placenta, the size of the fetus, and the amount of amniotic fluid:
- determination of the location of the placenta, placental thickness and structure (degree of maturity, presence of edema, expansion of intervillous spaces, etc.). In the presence of fetoplacental insufficiency, according to ultrasound data, a decrease or increase in the thickness of the placenta by more than 5 mm is noted, in contrast to the normal indicators for the corresponding period. In the placenta itself, signs of “premature aging” are observed, as evidenced by the deposition of calcium salts;
- determining the size of the fetus (head, torso and limbs) and comparing them with standard indicators characteristic of the expected gestational age. A reliable sign of fetal growth restriction is the discrepancy between the size of the fetus and the actual period of pregnancy.
- detection of oligohydramnios or polyhydramnios (calculation of the AF index).
Doppler measurements are performed to assess the state of blood flow in the vessels of the umbilical cord, uterus and fetal brain. CTG is performed to assess fetal cardiac activity.
Placental insufficiency in the miscarriage clinic
B
Women with recurrent miscarriage constitute a risk group for the development of placental insufficiency, leading to malnutrition and chronic intrauterine hypoxia of the fetus. According to modern concepts, with the development of hypoxia, it is the fetus that induces premature birth, while normalization of the intrauterine state of the fetus can lead to successful prolongation of pregnancy.
Placental insufficiency (PI) is a pathophysiological phenomenon consisting of a complex of disorders of the trophic, endocrine and metabolic functions of the placenta, leading to its inability to maintain adequate and sufficient exchange between the organisms of the mother and fetus. PN syndrome has a multifactorial nature.
Recurrent miscarriage is complicated by PN, according to the literature, in 47.6–77.3% of cases.
Professor G.M. Savelyeva identifies 3 forms of placental insufficiency:
– hemodynamic
caused by disturbances in the uteroplacental and fetal placental systems;
– placental-membrane
, characterized by a decrease in the ability of the placental membrane to transport metabolites;
– cellular-parenchymal
, associated with disturbances in the cellular activity of the trophoblast and placenta.
The division of PN according to the timing of its occurrence is also described. Primary PN is identified
up to 16 weeks, which is caused by vascular and enzymatic insufficiency due to disruption of the hormonal function of the ovaries, changes in the endo- and myometrium, somatic diseases of the woman and harmful environmental factors.
Secondary PN
is a consequence of disruption of uterine blood flow as a result of hypotension or hypertension in the mother, heart attacks, partial placental abruption, changes in the rheological properties of the blood, as well as inflammatory reactions (placentitis).
Habitual miscarriage is a multi-etiological problem, and the formation of PN occurs under the influence of several factors. These include hormonal deficiency, disorders of vascularization and endometrial reception, and vascular, thrombophilic reactions. Due to the described reasons, without corrective pathogenetic therapy, PN in patients with recurrent miscarriage is more often of a primary nature.
There are acute
and
chronic PN
. In the pathogenesis of acute insufficiency, an acute disturbance of decidual perfusion, which turns into circulatory damage to the placenta, plays an important role. This type of PN occurs as a consequence of extensive infarctions and premature detachment of a normally located placenta with the formation of a retroplacental hematoma, resulting in relatively rapid fetal death and termination of pregnancy.
Chronic PN is observed in every third woman from the high perinatal risk group. As a rule, two main ways of developing chronic PN can be clearly distinguished:
– disturbances in nutritional function or trophic insufficiency, in which the absorption and assimilation of nutrients, as well as the synthesis of the fetus’s own metabolic products, suffers;
– respiratory failure, which consists of impaired transport of oxygen and carbon dioxide.
The examination algorithm for patients with a history of miscarriage at risk for the development of PN should include:
– assessment of fetal growth and development by carefully measuring the height of the uterine fundus and the circumference of the pregnant woman’s abdomen;
– ultrasonic fetometry;
– assessment of the condition of the fetus by studying its motor activity and cardiac activity (cardiotocography, echocardiography, determination of the biophysical profile of the fetus);
– ultrasound assessment of the condition of the placenta (localization, thickness, area, volume of the maternal surface, degree of maturity, presence of cysts, calcification);
– study of placental circulation, blood flow in the vessels of the umbilical cord and large vessels of the fetus (doppler ultrasound);
– determination of the levels of hormones in the blood and specific proteins of pregnancy in dynamics (chorionic gonadotropin, placental lactogen, estriol, cortisol, trophoblastic b1-glycoprotein, placenta-specific a1-microglobulin);
– assessment of the state of metabolism and hemostasis in the pregnant woman’s body (acid-base state, enzymes AST, ALT, LDH, alkaline phosphatase, creatine phosphokinase, g-glutamine transpeptidase, volumetric oxygen transport, hemostasiogram parameters).
The basis of PN therapy is measures aimed at improving uteroplacental and fetoplacental blood flow
. Drugs used for this purpose dilate blood vessels, relax the muscles of the uterus, and improve the rheological properties of blood in the “mother-placenta-fetus” system.
Use of b-mimetics
in minimal doses it allows to normalize feto-placental blood flow, increase the saturation of fetal tissues with oxygen, eliminate acidosis and normalize biochemical parameters. Prescribing the drug hexoprenaline in a prophylactic dose of 1/4–1/2 tablet (125–250 mcg) 4–6 times a day for a long time allows to achieve sustainable relaxation of the uterus and increase blood flow in the vessels of the placenta, which is especially important in patients with recurrent miscarriage , placental insufficiency, multiple pregnancy.
We have experience in using the drugs Actovegin and Instenon in the treatment of PN in patients with miscarriage.
Actovegin
– a drug obtained from the blood of calves. Its physiological components have high biological activity (amino acids, oligopeptides, nucleosides, oligosaccharides, glycopeptides, electrolytes and some trace elements), due to which there is a powerful activation of metabolic processes at the cellular level. Under the influence of Actovegin, glucose transport and oxygen absorption in tissues improves. The absorption of large amounts of oxygen by the cell leads to the activation of aerobic oxidation processes, which increases the energy potential of tissues. It has been proven that the effects of Actovegin are most pronounced in the hypoxic nature of tissue damage.
Actovegin allows you to normalize hemodynamic parameters, increases oxygen delivery and glucose perfusion in the placenta, stimulates aerobic oxidation and has a pronounced anabolic effect on the protein metabolism of the fetus.
The recommended regimen for using Actovegin for therapeutic purposes includes starting its use with intravenous drip administration of the drug every other day 5 times at a dose of 5 ml in 250 ml of 5% glucose or saline solution. Then continue taking the drug orally, 1 tablet 3 times a day for 3–4 weeks.
In patients with recurrent miscarriage, prophylactic use of Actovegin is also possible. In this case, you can limit yourself to oral administration of the drug, 1 tablet 3 times a day for 2–3 weeks.
In case of severe PN, accompanied by chronic intrauterine fetal hypoxia, Actovegin is advisable to combine with the drug Instenon
, which leads to the normalization of fetoplacental and uteroplacental blood flow.
Instenon is a unique drug, since its effect consists of several, namely three, components.
Firstly, under the influence of hexobendin, a number of changes occur at the cellular level - the energy status of cells increases due to the activation of the utilization of glucose and oxygen through anaerobic glycolysis. This effect is very important in patients with recurrent miscarriage, since it is tissue hypoxia that leads to intrauterine growth retardation. Under the influence of hexobendine, the phenomena of tissue hypoxia are reduced or completely eliminated.
The next component of Instenon, etophylline, increases perfusion pressure in ischemic areas due to its effect on a number of organs and tissues. Myocardial metabolism is activated, which contributes to an increase in cardiac output. As a result of improved blood circulation in the renal tissue, diuresis increases, and, finally, bronchodilation develops, which also helps to increase the access of oxygen to the tissues.
The third component of Instenon - etamivan - has nootropic activity, which is expressed in an activating effect on the reticular formation of the brain, the respiratory center, and blood circulation regulation centers. This effect is also important, as it helps improve peripheral blood circulation in tissues and organs.
Instenon is administered intravenously slowly (16–20 drops per minute) at a dose of 2 ml in 250 ml of 5% glucose solution 5 times every other day. Next, it is advisable to switch to oral administration of the drug in a dose of 1 tablet 3 times a day for 2–3 weeks.
According to our data, in 97% of patients with intrauterine growth retardation and chronic intrauterine hypoxia, it is possible to achieve an improvement in the fetal condition, of which 75% have pronounced positive dynamics. It was noted that normalization of cell metabolism, reduction or elimination of tissue hypoxia due to the use of the drugs Actovegin and Instenon has a positive effect on the condition of the fetus and prolongation of pregnancy.
A thorough analysis of the reasons that led to the development of the threat of premature birth is necessary. If infectious genesis prevails, antibacterial therapy is effective, taking into account the sensitivity of the isolated microflora to antibiotics; in case of autoimmune disorders, individual selection of antiplatelet agents
(Cardiomagnyl, dipyridamole), if necessary,
anticoagulants
under close control of a hemostasiogram, preference is given to low molecular weight heparins (enoxaparin, etc.).
, amino acid solutions are added to treatment
– infezol, levamine, alvezin, intravenous drip for a course of 5–7 injections.
Metabolic therapy is prescribed in complexes for 10–12 days with 2–3 week breaks.
In the complex of treatment, if drug therapy is insufficiently effective, courses of therapeutic plasmapheresis can be used to help normalize the rheological properties of the blood, as well as increase sensitivity to the drugs used. A pronounced positive therapeutic effect was noted during plasma substitution with solutions of hydroxyethyl starch using crystalloid and protein drugs - albumin. The course of treatment consists of 3 sessions at intervals of 2–4 days.
Summarizing the above data, it should be noted that PN during miscarriage is a multi-etiological problem that is difficult to solve during pregnancy.
In this regard, a comprehensive examination of women is necessary before the desired pregnancy occurs. Correction of identified disorders should be started in a timely manner and carried out even before conception, which is the prevention of primary placental insufficiency.
Treatment of placental insufficiency
The main goals of treatment of placental insufficiency are measures aimed at:
- improvement of uteroplacental and fetoplacental blood flow;
- prevention of intrauterine growth retardation (discrepancy between the size of the fetus and the required size at a given stage of pregnancy);
- choice of timing and method of delivery (through the natural birth canal or by caesarean section).
Drug therapy is reduced to the prescription of drugs that dilate blood vessels (such as Curantil, to improve microcirculation, eliminate hypoxia in fetal tissues and to prevent further negative changes in the placenta), tocolytics (relaxing the muscles of the uterus such as Ginipral, Magnesium Sulfate, No-spa.) , improving the properties of blood in the “mother-placenta-fetus” system, sedatives that reduce the neuropsychic agitation of the pregnant woman (tinctures of motherwort or valerian, glycine). In case of increased blood clotting, antiplatelet agents (Heparin) are used.
Symptoms
The symptoms of uteroplacental insufficiency are noticeable, difficult to miss for a healthcare professional, and some of them are easy to notice for the pregnant woman herself.
- The first symptom is the small size of the uterus compared to what should be observed in accordance with the stage of pregnancy. The doctor determines the size of the uterus by palpation, and if the height of the fundus of the uterus is insufficient, then this becomes a signal of delayed intrauterine development of the baby.
- Increase or decrease in fetal heart rate due to oxygen starvation (hypoxia). Bradycardia indicates decompensation.
- Fetal movement begins from the 16th week of pregnancy, and a woman can count how many times a day he was active. A decrease in motor activity indicates possible fetal hypoxia associated with placental insufficiency. The sign is relevant after 24 weeks.
- Bloody discharge from the genital tract of a pregnant woman is a dangerous symptom. It may indicate placental abruption due to CPRF.
- If the uterus is constantly in a state of hypertonicity due to chronic renal failure, this threatens miscarriage or premature birth.
The woman herself should note and inform the doctor that her blood pressure has increased significantly, and this increase has been observed regularly for a long time. Peripheral edema can be a signal of disturbances in the functioning of the heart and kidneys, the first sign of gestosis. The consequence of these disorders is a decrease in blood supply to the placenta and the development of chronic renal failure.
Childbirth with placental insufficiency
With a compensated form of fetoplacental insufficiency, if the fetus does not suffer from hypoxia, then the pregnant woman can give birth through the natural birth canal. In all other cases, in the presence of a viable fetus, a cesarean section is indicated.
Placental insufficiency is a serious complication of pregnancy, leading to high morbidity and mortality of the fetus and newborn. The risk of developing placental insufficiency increases significantly in pregnant women with poor nutrition, in smokers and patients who drink alcohol.
The placenta is a temporary organ that is formed only during pregnancy and performs the functions of supplying the fetus with everything necessary for healthy development. Placental insufficiency is a violation of its structure and functions. In other words, this is a disorder of blood flow in the fetus-placenta-mother system. In severe cases, it can even lead to the death of a child. So, let's learn about the causes, treatment and consequences of placental insufficiency.
Features of childbirth
If the development of the fetus occurs without deviations (compensated form of FPN), the woman is allowed to give birth naturally. In other situations, a caesarean section is performed to prevent existing complications.
It is especially worth paying attention to childbirth with a decompensated form of PN. A newborn baby may be born with a blocked pulmonary duct, which will lead to further death. To prevent this, a caesarean section is performed. But there are situations when the baby’s mother is intolerant to local anesthesia. In such situations, the operation is performed without anesthesia, but with painkillers.
Why does it occur
The causes of pathology are divided into endogenous (acting from within the body) and exogenous (acting from the outside). The latter are air pollution, radiation exposure, stress, poor nutrition, occupational hazards, and the use of aggressive household chemicals. Excessive physical activity by the expectant mother can also negatively affect the condition of the placenta. Exogenous factors of placental insufficiency include bad habits, primarily smoking of the expectant mother, drinking alcoholic beverages, and a passion for strong coffee.
As for exogenous factors, these include the age of future mothers over 35 and under 18; numerous births and abortions; ovarian tumors; history of birth of hypotrophic children; habitual miscarriage; inflammatory processes of the genital organs.
Practice shows that very often the cause of placental insufficiency is somatic diseases of the mother. We are talking about diabetes, hypertension, heart disease, blood and kidney diseases. Women with congenital pathologies of the reproductive organs, for example, a bicornuate or saddle-shaped uterus, are also at risk.
Etiology
To date, not all the causes influencing the formation of placental insufficiency are known. Disease statistics allow us to accurately identify only a few of them:
- age. The risk group includes all women under 18 years of age and after 32 years of age;
- excessive use of alcohol, tobacco or drugs;
- individual body features (such as short stature, obesity or emaciation);
- level of mental health. Fatigue, lack of sleep, breakdowns and stress have long become commonplace. The above factors could also cause placental insufficiency;
- bearing several fruits;
- chronic diseases. These can be both problems in the female part, and difficulties in the functioning of the cardiovascular system, gastrointestinal tract;
- Difficulties in pregnancy or childbirth: absence or, on the contrary, excess of amniotic fluid, bleeding wounds, risk of miscarriage.
Risk factors that provoke the development of placental insufficiency:
- long-term risk of miscarriage;
- tumors in the muscular layers of the uterus (a characteristic symptom is uterine bleeding);
- other diseases: bronchitis, tonsillitis, critical blood pressure, malformations of heart structures, etc.;
- fetal death during previous births.