In patients who have suffered from kidney disease for a long time, chronic renal failure (CRF) gradually develops. This is a severe painful condition that is characterized by the inability of the kidneys to function as a filter in the human body. Unfortunately, chronic renal failure cannot be completely cured, but modern medicine has methods to stop the development. A patient with chronic renal failure is forced to constantly be monitored by a nephrologist and undergo courses of therapy.
HPN: What is this?
The diagnosis of chronic renal failure is made to a patient who has had kidney dysfunction for more than 3 months. As pathology develops, the kidneys lose their ability to eliminate toxins from the human body, resulting in intoxication. The lack of qualified assistance leads to disruption of the natural chemical balance of the body and death. Often, chronic renal failure is a consequence of untreated ailments and inflammation of the urinary system, surgical interventions or injuries.
Pathogenesis of the disease and causes of occurrence
In nephrology, the wording of chronic kidney disease has been replaced by “chronic kidney disease.” The pathogenesis of CKD is expressed in the progressive death of nephrons (working units of the kidney), followed by replacement of the renal parenchyma with connective tissue. As a result, the organ cannot cope with filtering and excretory functions, and toxic substances accumulate in the body. The leader among the causes of this pathology is acute renal failure. Any inflammatory process in the urinary system can lead to organ failure. Etiology of the disease:
Liver cirrhosis may be a risk factor for the development of kidney pathology.
- obesity;
- urolithiasis disease;
- diabetes;
- cirrhosis of the liver;
- congenital features of the development of the urinary system;
- alcohol and drug poisoning;
- chemical intoxication;
- diseases of the cardiovascular system;
- systemic autoimmune diseases;
- various kidney diseases.
Causes
Kidney failure is divided into acute and chronic. Acute renal failure (ARF) occurs as a result of various causes, which can be divided into three groups:
1. Causes of blood supply to the kidneys - various shock conditions (allergic shock, severe bleeding, obstruction of the renal artery or vein) “stop” the blood flow to the kidneys, and they cannot perform their normal functions.
2. Causes in the kidneys themselves - here most often there are various diseases that damage the parenchyma (working tissue) of the kidney, as well as a number of toxic (including medicinal) damage to the kidneys.
3. The causes lie in the urethra, bladder and urethra - these are relatively rare pathological conditions that completely block the output of urine.
Acute renal failure is characterized by a cessation of urine output (oliguria or anuria) and occurs relatively quickly: from several hours to several days. Most often, it is reversible (i.e., it is a treatable condition) and usually occurs in several stages:
• manifestation phase of the cause of kidney damage;
• oliguric and anuric phase;
• polyuria;
• recovery stage.
Chronic kidney failure (CRF) develops slowly and gradually and is the final stage of various diseases that irreversibly damage the kidneys and all their functions. The electrolyte and acid-base balance in the body is disturbed, the concentrations of nitrogenous bodies formed as a result of protein metabolism in the body increase, the production of red blood cells and the exchange of minerals in the bones are disrupted.
CKD is the final stage of kidney damage that occurs as a result of various diseases. Most often these are: diabetes mellitus, long-term untreated hypertension (“high blood pressure”), glomerulonephritis, vasculitis, autoimmune systemic diseases, pyelonephritis, drug-induced or toxic interstitial nephritis, congenital kidney malformations, etc.
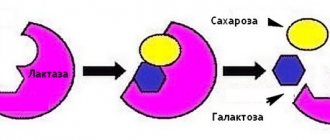
By their mechanism, all these diseases slowly and gradually destroy the main “working” unit of the kidney, called the nephron. Each kidney contains about 1.2 million nephrons. The processes of filtration and blood resorption occur in the nephron. With the destruction of nephrons, there is a progressive decrease in glomerular filtration and, accordingly, a progressive increase in the concentration of excess (toxic to the body) waste nitrogen-containing substances and fluid retention.
CRF progresses gradually over a long period of time. Conventionally, the evolution of the disease is divided into several stages:
• Long stage of compensation. At this stage, the “patient” usually does not suspect the presence of the disease. The kidneys have partially lost their functionality, but the levels of nitrogen-containing bodies in the blood (creatinine and urea) have not yet increased. At this stage, the excretory system is still coping with its tasks.
• Stage of compensated retention. At this stage, the values of nitrogen-containing substances in the blood rise above normal (that is, “azotemia” occurs, which is literally translated as “nitrogenous bodies in the blood”, creatinine values increase, but do not exceed 530 µmol/l). The patient does not yet have any complaints caused by uremia. Uremia depends on very high levels of urea, creatinine and other nitrogen-containing substances in the blood. During this phase, other active nephrons work with renewed vigor.
• Stage of severe renal failure. Here the creatinine level rises above 530 µmol/L, and when it reaches 710 mmol/L, symptoms associated with high concentrations of urea in the blood and tissues occur. At this stage, the compensatory capacity of the excretory system is almost exhausted.
• Terminal stage. This is the final stage of chronic renal failure, in which creatinine exceeds 880-890 µmol/l, and the symptoms of uremia no longer respond to conservative treatment. The only effective treatments at this stage are dialysis or kidney transplantation.
Symptoms of the pathological condition
CRF and CKD always act as a complication as a result of another disease. If you notice one or more symptoms, the patient should immediately consult a doctor.
The onset of chronic renal failure is not characterized by the presence of symptoms. Often the patient learns about the disease when it has reached stage 2 and kidney function is noticeably impaired. The only specific symptom of the pathology is disturbances in urine output. The patient suffers from frequent urination, sometimes at night. As the disease progresses, urine production, on the contrary, decreases, which indicates a worsening of the disease. Symptoms of chronic renal failure:
A symptom of the disease may be morning swelling of the face.
- digestive disorders;
- dry mouth;
- a sharp decrease in the body's protective functions;
- skin hemorrhages;
- nephrogenic anemia;
- albuminuria;
- swelling of the face, especially in the morning;
- muscle twitching;
- increased fatigue;
- lack of appetite.
Causes and symptoms of chronic renal failure
Chronic renal failure (CRF) is an irreversible impairment of the functional activity of the kidneys, resulting from necrosis of their tissue and death of nephrons. It develops against the background of kidney stones, polycystic disease, chronic forms of glomerulonephritis and pyelonephritis, diabetes mellitus and other pathologies affecting the kidneys.
Symptoms of chronic renal failure:
- latent stage: there are no visible signs of pathology, test results can reveal proteinuria, sometimes absent-mindedness, lethargy and lethargy are observed;
- compressed stage: manifested by reduced density of urine with a simultaneous increase in its volume, thirst, dry mucous membranes, fatigue, increased levels of urea and creatinine;
- intermittent stage: the glomerular filtration rate decreases significantly, acidosis develops (displacement of the body’s acid-base balance), azotemia, and creatinine levels increase greatly;
- terminal stage: signs of heart failure, increasing edema, congestion in internal organs and tissues, intoxication and poisoning of the body with unremoved metabolic products appear, infectious complications, anemia are often added, a characteristic odor of ammonia appears from the mouth, vomiting, diarrhea.
Classification of the disease depending on the stage
There is a classification of chronic kidney disease that divides the development of the disease into stages. The stage is determined by measuring the glomerular blood filtration rate (GFR) and creatinine in the blood. Knowing the degree of development of the disease helps the nephrologist select effective treatment and make a prognosis for the future. The table shows the stages of chronic renal failure and the manifestations of each of them.
| Name | GFR ml/min | Creatinine level mmol/l | Clinical symptoms |
| Hidden | >90 | 0, 123 | None |
| Latent | 90—69 | 0, 123—0,176 | Indicators are the norm for older people |
| Proteinuria appears in young people | |||
| Compensated | 60—30 | 0, 177—0, 352 | Increased fatigue |
| Anemia | |||
| Muscle weakness | |||
| Dry mouth | |||
| Intermittent | 30—15 | 0, 353—0, 528 | Increased blood pressure |
| Increased urge to urinate | |||
| Severe anemia | |||
| Swelling | |||
| Terminal | <15 | >0, 528 | The nervous system is affected |
| Symptoms of body intoxication are observed | |||
| Heart failure develops |
Treatment
Women are more likely to have kidney disease than men. This is due to the physiological characteristics of the structure of the body. Carrying a child puts additional stress on internal organs. Women during pregnancy are more likely to develop the disease, which is associated with:
- an increase in blood flow to the kidneys, which can lead to overstrain and death of the glomeruli;
- disruptions in the salt absorption process, which lead to protein growth;
- bleeding disorders lead to blood clots.
During the gestation period, the likelihood of developing complications increases, since an imbalance in blood and urine parameters creates an unfavorable environment and life for the unborn child, and the mother’s health is at risk. Complications of chronic kidney disease in pregnant women:
- hypertension;
- severe swelling of the limbs;
- diuretic disorders;
- anemia and dystonia;
- placental insufficiency;
- oxygen starvation of the fetus;
- delay in fetal development;
- miscarriage, spontaneous abortion, premature birth;
- infectious and bacteriological diseases of the female genitourinary system.
Treatment of chronic renal failure is carried out by maintaining the relationship between symptoms and treatment of the disease itself.
To normalize water and salt balance it is necessary:
- Change your diet, limiting the amount of protein food to 70 g/day, giving preference to plant proteins. If the patient's life is worsened by unpleasant symptoms of stage 4 disease, protein should be less than 30 g/day. Among animal proteins, eat veal, chicken and quail eggs, and low-fat fish.
- Place restrictions on legumes, mushrooms, dairy products, nuts and other foods high in phosphorus.
- If the amount of potassium is high, you should limit potatoes, bananas, and brown bread.
- With severe swelling of the face and limbs, the daily fluid intake is 2 liters, no more. This amount includes water, tea, coffee, soups. Too much fluid can only make the situation worse.
- Salt restriction is necessary only with high blood pressure resulting from pathology.
A diet with limited protein intake is not prescribed to patients with malnutrition, low body weight, hypertension, after surgical treatment, disorders of the cardiovascular and nervous systems, as well as with a glomerular filtration rate of less than 5 ml/min.
Treatment of chronic renal failure is also accompanied by the intake of sorbents, which normalize the functioning of the digestive organs and reduce the severity of uremia. The intake of Activated Carbon, Enterosgel, Filtrum and other sorbents is indicated in the initial stages of the development of insufficiency, with a filtration rate of at least 30 ml/min.
Two drugs are used to treat anemia: Erythropoietin and Maltofer - they promote the synthesis of red blood cells and hemoglobin. The first is not used for high blood pressure and in women during menstruation. Erythropoietin is prescribed for intravenous administration, Maltofer is taken orally.
For problems with blood clotting, Clopidogrel and Aspirin are prescribed. For hypertension, medications that normalize blood pressure are used: Ramiprol, Losartan, Moxonidine, Frifon, Buetanide.
With kidney dysfunction, the metabolism of calcium and phosphorus is disrupted, which affects test results. To normalize this condition, calcium carbonate is prescribed, which does not allow phosphorus to be quickly absorbed, which increases its level. If calcium levels are insufficient, various calcium and vitamin D supplements are used.
Stabilization of the patient's condition is carried out by changing and adjusting nutrition and fluid volume, in addition, replenishment of sodium reserves is required. For this purpose, solutions of sodium, glucose, Trisamine and others are administered intravenously or intramuscularly.
For infectious underlying causes of chronic kidney disease, treatment with antibiotics and antifungal drugs is prescribed. The choice of medication is based on the results of a biochemical analysis of urine.
Hemodialysis
Chronic renal failure is treated at the last stage using an “artificial kidney”. This method is necessary when GFR decreases critically. With the help of an artificial kidney, the blood is cleared of nitrogen.
DETAILS: Urological centers in Moscow treatment of cystitis
Indications for hemodialysis:
- children and patients with diabetes mellitus with GFR less than 30 ml/min;
- GFR 10 ml/min in other patients;
- poisoning of the body with residual nitrogen;
- swelling of the lungs and brain;
- blood acidification.
This method is not used when:
- low blood pressure;
- reducing the number of blood clots;
- malignant neoplasms in the kidney;
- heart diseases;
- large-scale inflammatory lesion;
- mental disorders.
Kidney transplant
An extreme method of treating chronic kidney failure. The diseased organ is replaced with a healthy one through surgical manipulation. However, a second kidney transplant may be required if the kidney is rejected. After such an operation, the patient is prescribed hormones.
| 1. | Treatment of the underlying disease that led to uremia. |
| 2. | Mode. |
| 3. | Medical nutrition. |
| 4. | Adequate fluid intake (correction of water balance disorders). |
| 5. | Correction of electrolyte metabolism disorders. |
| 6. | Reducing the retention of end products of protein metabolism (combat azotemia). |
| 7. | Correction of acidosis. |
| 8. | Treatment of arterial hypertension. |
| 9. | Treatment of anemia. |
| 10. | Treatment of uremic osteodystrophy. |
| 11. | Treatment of infectious complications. |
| 1.1. | Treatment of the underlying disease Treatment of the underlying disease that led to the development |
Chronic renal failure in the conservative stage can still have a positive effect and even reduce the severity of chronic renal failure. This especially applies to chronic pyelonephritis with initial or moderate symptoms of chronic renal failure. Stopping the exacerbation of the inflammatory process in the kidneys reduces the severity of renal failure.
1.2. Mode
The patient should avoid hypothermia, heavy physical and emotional stress. The patient needs optimal working and living conditions. He must be surrounded by attention and care, he must be given additional rest during work, and a longer vacation is also advisable.
The diet for chronic renal failure is based on the following principles:
- limiting dietary protein intake to 60-40-20 g per day, depending on the severity of renal failure;
- ensuring sufficient calorie content of the diet corresponding to the energy needs of the body, due to fats, carbohydrates, complete provision of the body with microelements and vitamins;
- limiting the intake of phosphates from food;
- control over the intake of sodium chloride, water and potassium.
The implementation of these principles, especially the restriction of protein and phosphates in the diet, reduces the additional load on functioning nephrons, contributes to a longer preservation of satisfactory renal function, reduces azotemia, and slows down the progression of chronic renal failure. Limiting protein in food reduces the formation and retention of nitrogenous waste in the body, reduces the content of nitrogenous waste in the blood serum due to a decrease in the formation of urea (with the breakdown of 100 g of protein, 30 g of urea is formed) and due to its reutilization.
In the early stages of chronic renal failure, when the level of creatinine in the blood is up to 0.35 mmol/l and urea up to 16.7 mmol/l (glomerular filtration about 40 ml/min), moderate protein restriction to 0.8-1 g/kg is recommended, i.e. up to 50-60 g per day. At the same time, 40 g should be high-value protein in the form of meat, poultry, eggs, and milk.
When serum creatinine levels are from 0.35 to 0.53 mmol/l and urea levels are 16.7-20.0 mmol/l (glomerular filtration rate is about 20-30 ml/min), protein should be limited to 40 g per day (0.5-0.6 g/kg). At the same time, 30 g should be high-value protein, and bread, cereals, potatoes and other vegetables should account for only 10 g of protein per day.
30-40 g of complete protein per day is the minimum amount of protein required to maintain a positive nitrogen balance. If a patient with chronic renal failure has significant proteinuria, the protein content in food is increased according to the loss of protein in the urine, adding one egg (5-6 g of protein) for every 6 g of urine protein.
In general, the patient’s menu is compiled within table No. 7. The patient’s daily diet includes the following products: meat (100-120 g), cottage cheese dishes, cereal dishes, semolina porridge, rice, buckwheat, pearl barley. Particularly suitable due to their low protein content and at the same time high energy value are potato dishes (pancakes, cutlets, babkas, fried potatoes, mashed potatoes, etc.), salads with sour cream, vinaigrettes with a significant amount (50-100 g) of vegetable oil. Tea or coffee can be acidified with lemon, put
2-3 tablespoons of sugar per glass, it is recommended to use honey, jam, jam.
Thus, the main composition of food is carbohydrates and fats and in doses - proteins. Calculating the daily amount of protein in the diet is mandatory. When compiling a menu, you should use tables reflecting the protein content in the product and its energy value (Table 41). Table 41. Protein content and energy value of some food products (per 100 g of product)
| Product | Protein, g | Energy value, kcal |
| Meat (all types) | 23.0 | 250 |
| Milk | 3.0 | 62 |
| Kefir | 2.1 | 62 |
| Cottage cheese | 20.0 | 200 |
| Cheese (cheddar) | 20.0 | 220 |
| Sour cream | 3.5 | 284 |
| Cream (35%) | 2.0 | 320 |
| Egg (2 pcs.) | 12.0 | 150 |
| Fish | 21.0 | 73 |
| Potato | 2.0 | 68 |
| Cabbage | 1.0 | 20 |
| cucumbers | 1.0 | 20 |
| Tomatoes | 3.0 | 60 |
| Carrot | 2.0 | 30 |
| Eggplant | 0.8 | 20 |
| Pears | 0.5 | 70 |
| Apples | 0.5 | 70 |
| Cherry | 0.7 | 52 |
| Oranges | 0.5 | 50 |
| Apricots | 0.45 | 90 |
| Cranberry | 0.5 | 70 |
| Raspberries | 1.2 | 160 |
| strawberries | 1.0 | 35 |
| Honey or jam | — | 320 |
| Sugar | — | 400 |
| Wine | 2.0 | 396 |
| Sliaoch oil | 0.35 | 750 |
| Vegetable oil | — | 900 |
| Potato starch | 0.8 | 335 |
| Rice (boiled) | 4.0 | 176 |
| Pasta | 0.14 | 85 |
| Oatmeal | 0.14 | 85 |
| Noodles | 0.12 | 80 |
DETAILS: Urological treatment in Zheleznovodsk
| Product | Net weight, g | Proteins, g Fats, g | Carbohydrates, g | |
| Milk | 400 | 11.2 | 12.6 | 18.8 |
| Sour cream | 22 | 0.52 | 6.0 | 0.56 |
| Egg | 41 | 5.21 | 4.72 | 0.29 |
| Salt-free bread | 200 | 16.0 | 6.9 | 99.8 |
| Starch | 5 | 0.005 | — | 3.98 |
| Cereals and pasta | 50 | 4.94 | 0.86 | 36.5 |
| products | ||||
| Wheat groats | 10 | 1.06 | 0.13 | 7.32 |
| Sugar | 70 | — | — | 69.8 |
| Butter | 60 | 0.77 | 43.5 | 0.53 |
| Vegetable oil | 15 | — | 14.9 | — |
| Potato | 216 | 4.32 | 0.21 | 42.6 |
| Vegetables | 200 | 3.36 | 0.04 | 13.6 |
| Fruits | 176 | 0.76 | — | 19.9 |
| Dried fruits | 10 | 0.32 | — | 6.8 |
| Juices | 200 | 1.0 | — | 23.4 |
| Yeast | 8 | 1.0 | 0.03 | 0.33 |
| Tea | 2 | 0.04 | — | 0.01 |
| Coffee | 3 | — | — | — |
| 50 | 90 | 334 | ||
| It is allowed to replace 1 egg with: cottage cheese - 40 g; meat - 35 g; fish - 50 g; milk - 160 g; cheese - 20 g; beef liver - 40 g | ||||
Features in children
Pediatric chronic kidney damage has signs:
With such an illness, the child may have a stomach ache.
- Increased amount of urine excreted. Initially, the volume increases, but at stage 3, on the contrary, anuria develops (no urine). The same condition is observed at stage 4.
- Edema. The last stages of the disease are characterized by incomplete removal of fluids; as a result, children experience swelling of the ankles or face.
- Deformation of the limbs and loss of their full sensitivity.
- Abdominal pain.
- Increased pressure.
- Ammonia smell. If the child has a terminal kidney, there is a smell of urine when exhaling.
Dangerous consequences and complications
The consequences of CKD are the following pathologies:
- bone fragility;
- diseases of the cardiovascular system;
- chronic adrenal insufficiency;
- reproductive dysfunction in women;
- angiopathy;
- dysfunction of blood clotting and hematopoiesis;
- ulcers, gastritis and other diseases of the gastrointestinal tract;
- decreased libido;
- nephrotic syndrome in pregnant women;
- uremic coma;
- death.
Diagnosis of the disease
In addition to the totality of the patient’s complaints, the nephrologist will need to examine him.
Nephrology has a wide range of diagnostic measures for timely detection of pathology. A person who suspects he has kidney problems should consult a nephrologist. The doctor will conduct an examination, listen to complaints and collect a complete medical history. The final diagnosis is established after conducting a series of studies and determining the form of chronic renal failure.
What laboratory tests are needed?
To identify the disease, the following studies are used:
- General clinical urine analysis. Determines the degree of albuminuria.
- Urine culture. Determines the level of opportunistic microorganisms.
- Blood chemistry. Displays the status of the excretory system.
- Reberg-Toreev test. Thanks to this manipulation, the doctor establishes the stage of the pathology and measures GFR.
Instrumental diagnostics
Chronic renal failure is successfully diagnosed using instrumental methods:
A more detailed picture of the disease can be obtained using ultrasound.
- Ultrasound of the abdominal and pelvic organs. The examination will show physiological changes in the organs.
- Kidney biopsy. Taking and examining tissue from the diseased organ will help the doctor determine the optimal treatment regimen.
- Electrocardiography. Controls the condition of the heart.
- Chest X-ray. Sometimes chronic kidney disease occurs due to respiratory diseases, and the procedure helps eliminate this.
Treatment methods
If the development of chronic renal failure is suspected, the patient needs to consult a nephrologist and conduct laboratory tests: biochemical analysis of blood and urine, Rehberg test.
The basis for diagnosis is a decrease in the level of glomerular filtration, an increase in the level of creatinine and urea. When performing the Zimnitsky test, isohyposthenuria is detected. Ultrasound of the kidneys indicates a decrease in the thickness of the parenchyma and a decrease in the size of the kidneys. A decrease in intraorgan and main renal blood flow is detected on Doppler ultrasound of the renal vessels. X-ray contrast urography should be used with caution due to the nephrotoxicity of many contrast agents. The list of other diagnostic procedures is determined by the nature of the pathology that caused the development of chronic renal failure.
In order to begin treatment for renal failure, it must be diagnosed. The following methods are used:
- biochemical blood test, urine test (biochemical analysis can detect changes in urea and creatinine levels. Calcium, phosphorus, potassium and magnesium levels decrease or increase);
- chest x-ray;
- ultrasound examination (ultrasound);
- organ biopsy (a biopsy is done if there are problems determining the correct diagnosis);
- Reberg-Tareev test (using the Reberg-Tareev test, the excretory capacity of the kidneys is assessed. For this method, you need to take blood and collect urine);
- Doppler ultrasound (ultrasound of the kidneys checks blood circulation in the vessels);
- CT scan;
- chromocystoscopy (during chromocystoscopy, a coloring liquid is injected intravenously into a person. It gives an unusual color to the urine and allows you to examine the bladder);
- general blood test, urine test (CBC), (a general blood test can show a decreased or increased number of blood cells, hemoglobin. Protein will be present in the urine);
- magnetic resonance imaging (MRI);
- Zimnitsky test (Zimnitsky test makes it possible to find out the volume of urine excreted during the day and night. For this, the patient collects it for 24 hours);
- electrocardiography (ECG), (electrocardiography is mandatory for all patients, it allows you to find out about problems related to the heart).
Magnetic resonance imaging, ultrasound, and computed tomography are used to detect the causes of narrowing of the urinary tract.
If signs of the development of this syndrome appear, you must consult a nephrologist. Timely identification of symptoms and treatment of existing pathologies allows you to restore kidney function and prevent progression of failure.
Making a diagnosis requires collecting anamnesis and conducting a general and bacteriological analysis of urine. In addition, blood is taken from the patient for testing. Modern diagnostic tools make it much easier to identify problems related to kidney function. Commonly ordered tests include:
- Ultrasound;
- CT;
- MRI;
- Doppler ultrasound;
- chest x-ray;
- chromocystoscopy;
- biopsy;
- electrocardiography;
- urography;
- Zimnitsky's test.
Doctors are already well aware of what kidney failure is and what danger it poses. After determining the nature and severity of the pathological process as a result of a comprehensive examination, the optimal course of therapy can be selected.
It is very important for patients to listen to the recommendations of the nephrologist, since otherwise the risk of developing severe complications increases, which will significantly worsen the overall prognosis.
Effective treatment
Based on the data obtained from the research, the doctor develops the optimal and most effective treatment regimen.
Therapy for chronic kidney disease depends on the degree of development of the disease. For stages 1 and 2, treatment with medications, nutritional correction and spa treatment are acceptable. Later manifestations of pathology require an integrated approach, since other organ systems are damaged. End-stage chronic renal failure is treated exclusively with surgical methods; the doctor’s goal is to save the patient’s life.
What medications are needed?
If the disease is caused by poison toxins, then they need to be removed with sorbents.
Medicines prescribed to patients with chronic kidney disease are aimed at treating the underlying cause of the disease. If chronic renal failure is caused by an infectious disease of the urinary system, antibacterial drugs are prescribed. Given the intoxicating nature of the disease, it is important to remove the poison from the body. Enterosorbents are used for this. Glomerulonephritis and autoimmune diseases are treated with drugs based on glucocorticosteroids. Be sure to take medications that slow down the development and transition of the pathology to the next stage.
How are symptoms treated?
Treatment of chronic renal failure is aimed at symptomatic therapy:
- Anemia. To eliminate the cause, Erythropoietin is used, a drug that stimulates the production of red blood cells.
- Blood clotting disorder. Aspirin and Ticlopedin are used for treatment.
- Arterial hypertension. The pathology is treated with ACE inhibitors.
- Water and electrolyte disturbances. Carry consequences in the form of dehydration of the body. If the water-electrolyte balance is disturbed, doctors use bicarbonates, citrates and glucose.
How important is diet?
The patient's diet must include grains.
The leading clinical recommendations for the treatment of chronic renal failure are to follow a special diet. Medical nutrition contains little protein and salt, but is high in calories. A food diary is compiled jointly with a nephrologist. The main components of the diet are vegetable fats and carbohydrates: vegetables, fruits, potatoes, cereals, fish. The amount of protein is sharply limited to relieve the load on the kidneys. If the patient experiences edema, limit salt (3-5 g per day), as it slows down the removal of fluid. Sometimes special mixtures balanced in microelements are included in the diet.
Hemodialysis: features of implementation
This is a procedure in which the patient's blood is passed through a special machine that contains a membrane that filters out anaphylotoxins such as C3A and C5A. End-stage renal failure is successfully treated with hardware blood purification. The procedure is carried out 3 times a week for 4 hours. Hemodialysis is prescribed if the patient:
- pronounced signs of intoxication;
- electrolyte imbalance, cerebral or pulmonary edema;
- blood acidification.
The procedure is contraindicated in the following cases:
- decompensated cardiovascular disease;
- acute inflammation of an infectious nature;
- mental disorders;
- metastatic oncology;
- hypotension;
- bleeding disorders.
Surgery
Surgery for chronic renal failure involves organ transplantation from a living or dead donor.
Doctors are forced to perform a kidney transplant if all other methods of preserving it have failed.
Kidney transplantation is a radical method used if end-stage renal failure has developed and therapy does not produce results. The donor is checked according to a number of criteria for compatibility, but there is always a risk of rejection of the transplanted kidney. Patients who survive such an operation are doomed to take hormones and cytostatics for life. This method helps prolong the patient's life.
Treatment with folk remedies
The relevance of using home recipes in therapy is determined only by a doctor. There are syndromes and pathologies for which home remedies are contraindicated, as they will cause complications and exacerbation of the disease. The success of herbal treatment depends on the stage of chronic kidney disease. Treatment with folk remedies includes taking various decoctions and tinctures of medicinal plants. The most common recipes:
- Pomegranate juice. Restores water-salt balance. You should drink a glass of juice in the morning and evening and 50 ml after meals. The duration of such treatment is 2 months.
- Flax decoction. Use a teaspoon of seeds per glass of boiling water, cook for 2 minutes over low heat. Infuse the resulting decoction for 2 hours. After cooling, take 100 ml three times a day.
- Laminaria algae. Sea kale is widely known for its beneficial properties. You need to eat 100 g per day.
Kidney failure
Renal failure is a serious complication of damage to the urinary organs, vascular pathology, in which the formation and filtration of urine decreases or completely stops. It is important that the process is not limited to changes in the kidneys themselves, but disrupts the balance of a person’s water-salt metabolism, changes the acid-base properties of the blood and the concentration of biochemical compounds dissolved in it.
Consequences can be found in all organs and systems of the body in the form of secondary damage. As kidney failure progresses, it takes on an acute or chronic form. They have differences. Therefore, pathogenesis is best considered separately.
What is acute kidney failure and how common is it?
The term “acute” refers to the rapid, even rapid development of renal dysfunction. In medical practice, it is included in the list of emergency conditions that require intensive treatment and threaten the patient’s life. The incidence of acute renal failure is 15 cases per 100,000 population.
Renal dysfunction occurs due to:
- a sharp decrease in total blood flow - prerenal damage;
- pronounced massive destruction of the nephron membrane - renal;
- sudden obstruction to the outflow of urine (obstruction) - postrenal disorders.
As a result, the patient experiences a significant decrease in urine output (oligoanuria), then complete anuria. 75% of people with such changes require urgent hemodialysis (a method of purifying the blood using an artificial kidney).
Determining the type of anuria is important for timely provision of emergency care. If there is obstruction of the urinary tract (postrenal level of damage), the patient needs emergency surgical intervention. A feature of kidney tissue is the possibility of complete recovery, therefore, with timely and complete treatment, most patients recover.
What are the causes of acute kidney failure?
The causes of acute renal failure are most often caused by:
- intoxication with poisons due to accidental poisoning or for the purpose of suicide, these include liquids from household chemicals, food industry, lead compounds, medications, bites of poisonous snakes and insects;
- a sudden decrease in blood circulation in the renal vessels during shock, collapse, acute heart failure, thrombosis and embolism of the renal artery;
- acute forms of kidney inflammation (glomerulonephritis and pyelonephritis);
- infectious diseases occurring with severe renal syndrome (hemorrhagic fever, leptospirosis);
- sudden blockage of the urinary tract with a stone, tumor - obstruction of the urinary tract;
- kidney injuries, including removal of a single kidney.
Clinical course and stages of pathology
Symptoms of renal failure determine therapeutic measures. Main manifestations:
- nausea with vomiting;
- diarrhea;
- complete lack of appetite;
- swelling of the arms and legs;
- excitement or lethargy.
Must appear:
- reduced amount or absence of urine output;
- liver enlargement.
According to the clinical course, renal failure develops in several stages.
I (initial) - characterized by the immediate cause that caused the pathology, can last several hours or days, the time of onset of the damaging factor (for example, taking poison) and the appearance of the first symptoms are taken into account, signs of intoxication are possible (pallor of the skin, nausea, vague pain in the abdominal area ).
II (oligoanuric) - the patient’s condition is assessed as severe, a characteristic decrease in the excreted volume of urine is manifested, an increase in intoxication is caused by the accumulation of end products of protein breakdown (urea, creatinine) in the blood; weakness, drowsiness, and lethargy appear due to the effect on brain cells.
Other symptoms:
- diarrhea;
- hypertension;
- increased number of heartbeats (tachycardia).
Signs of severity of renal function damage are:
- azotemia (increased amount of nitrogenous substances accumulated in the blood);
- anemia (anemia);
- addition of liver damage in the form of hepatic-renal failure.
Read more about the symptoms of kidney failure in this article.
III (restorative) - characterized by a return to the original phenomena. First, a phase of early diuresis appears, which corresponds to the clinical stage of stage II, then polyuria returns (there is a lot of urine) with the restoration of the kidneys’ ability to excrete sufficiently concentrated urine.
Against the background of normalization of biochemical blood parameters, there is an improvement in the functioning of the nervous system and heart, a decrease in high blood pressure, and a cessation of diarrhea and vomiting. Recovery lasts about 14 days.
IV (convalescent stage) - all kidney functions return to normal, it will take several months, for some people up to a year.
Chronic form
Chronic renal failure differs from acute renal failure by a gradual decrease in kidney function, death of structures, and replacement of tissue with scars with shrinkage of the organ. Its prevalence reaches from 20 to 50 cases per 100,000 population. Most often associated with a long course of inflammatory kidney diseases. Statistics show an annual increase in the number of patients by 10–12%.
What leads to the development of chronic renal failure?
The mechanism of formation of the pathology is associated with a violation of the structure of the main structural units of the kidney - nephrons.
Their number decreases significantly, atrophy and replacement with scar tissue occurs. Some glomeruli, on the contrary, hypertrophy, and similar changes in the tubules are possible. Modern research shows that the development of renal failure in such conditions is caused by an overload of “healthy” nephrons and a reduction in “sick” ones. Due to insufficient organ function provided by the residual number of glomeruli, water and electrolyte metabolism is disrupted.
The death of the glomerular apparatus is aggravated by:
- vascular damage;
- compression of the afferent arterioles by edematous tissue;
- impaired lymph circulation.
Why does chronic deficiency occur?
The most common causes of chronic kidney failure include:
- long-term inflammatory kidney diseases that destroy glomeruli and tubules (glomerulonephritis, pyelonephritis);
- congenital anomalies (polycystic disease, narrowing of the renal arteries, underdevelopment) contributing to the functional inferiority of the renal structures;
- diseases of impaired general metabolism (amyloidosis, diabetes mellitus, gout);
- systemic vascular diseases (rheumatism, lupus erythematosus, a group of hemorrhagic vasculitis, scleroderma) with simultaneous changes in renal blood flow;
- hypertension and symptomatic hypertension, which impairs blood supply to the kidneys;
- diseases accompanied by impaired outflow of urine (hydronephrosis, tumors of the underlying tract and pelvis, urolithiasis).
Among obese people, there is a widespread belief that it is possible to lose weight with the help of the hypoglycemic drug Metformin (synonyms Glucophage, Siofor, Formetin). The drug is prescribed very carefully by an endocrinologist. Negative properties include impaired renal and liver function. Self-administration is not recommended.
Types of chronic kidney failure and their classification
Different classifications of chronic kidney failure are based on:
- etiological factors;
- pathogenesis;
- degree of functional impairment;
- clinical signs.
In the Russian Federation, urologists use the Lopatkin-Kuchinsky classification. It divides pathological manifestations into 4 stages.
The latent stage of renal failure occurs without any clinical manifestations. There is normal urine output with sufficient specific gravity. In biochemical blood tests, the concentration of nitrogenous substances remains unchanged.
The earliest manifestations are detected by monitoring the ratio of kidney function during the day and at night. The disrupted circadian rhythm of urine excretion consists of an initial equalization of daytime and nighttime volumes, and then a persistent excess of the nighttime volume. When examining the patient, decreased indicators are detected:
- glomerular filtration (60–50 ml/min. with a normal level of 80–120);
- percentage of water reabsorption;
- tubular activity.
Compensated stage - the number of fully functioning nephrons decreases, but the concentration of urea and creatinine in the blood remains normal. This means that it is supported by overload of the remaining glomeruli, the development of polyuria.
Protective mechanisms ensure the removal of harmful toxins from the body due to:
- reduced concentration function of the tubules;
- decrease in glomerular filtration rate (30–50 ml/min);
- increasing urine production to 2.5 liters per day.
In this case, nocturnal diuresis predominates.
If a patient has preserved compensatory capabilities, it is necessary to take urgent measures for treatment and surgical restoration of the urine outflow tract. There is still hope for reverse development. It is impossible to completely cure the patient, but there is still a chance to transfer the disease to a more favorable latent stage. In the absence of adequate treatment, compensatory mechanisms are quickly exhausted, and a decompensated intermittent stage occurs.
The intermittent stage differs from the previous ones:
- persistently elevated creatinine and urine levels;
- the most pronounced clinical manifestations;
- exacerbations during the course of the underlying disease.
Compensatory polyuria, which contributed to the elimination of waste, is replaced by oliguria. The daily volume of urine may be normal, but the specific gravity decreases and does not change during the day. Glomerular filtration occurs at a rate of 29 to 15 ml/min.
The stage allows for periodic remissions. Although creatinine and urea levels do not normalize at this time, they remain 3-4 times higher than normal. Surgical interventions are assessed as very risky. The patient and relatives are notified. It is possible to install a nephrostomy to ensure the outflow of urine.
Terminal stage – is a consequence of untimely consultation with a doctor, the malignant course of the underlying disease. Irreversible changes occur in the body. Intoxication is caused by a high level of nitrogenous waste in the blood, a drop in glomerular filtration to 10–14 ml/min.
Course of the terminal stage
The clinical course in the terminal stage has four forms. Otherwise, they are considered periods of pathological changes.
I - renal failure is characterized by reduced glomerular filtration to 10–14 ml/min, high levels of urea while maintaining urine output in a volume of one liter or more.
II - stage is divided into forms “a” and “b”:
- In IIa, diuresis decreases, the content of dissolved substances in the urine decreases, acidosis develops (deviation of general metabolism in the acidic direction), and the amount of nitrogenous waste in the blood test continues to increase. The important thing is that changes in internal organs are still reversible. In other words, bringing the indicators closer to normal contributes to the complete restoration of damage to the heart, lungs, and liver.
- In stage IIb, compared with IIa, disorders of internal organs are more pronounced.
III - violations reach a critical level. Against the background of severe uremic intoxication, the brain reacts with a coma, renal-liver failure develops with degeneration of liver cells (hepatocytes), decompensation of cardiac activity and arrhythmias occur due to severe hyperkalemia.
Modern methods of treatment, including peritoneal dialysis and hemodialysis to relieve intoxication, are weakly effective or ineffective.
How to detect kidney failure?
In the diagnosis of acute renal failure, urologists attach primary importance to the absence of detected urine in the bladder. This sign does not necessarily confirm anuria. It is necessary to differentiate it from acute urinary retention due to a stone, spasm, in men with prostate adenoma.
The patient's bladder is examined using a cystoscope. If overfilling is detected, acute kidney failure is ruled out. Knowledge of the previous connection with poisoning and previous diseases helps to establish the cause and determine the form.
A urine test indicates:
- hemolytic shock in case of detection of hemoglobin clumps;
- tissue crush syndrome in the presence of myoglobin crystals;
- poisoning with sulfonamides when salts of sulfonamide substances are detected.
To establish the level of kidney damage, it is necessary to conduct ultrasound, x-ray and instrumental studies. If a catheter is successfully inserted into the renal pelvis and a lack of urine output is detected, one must think about renal or prerenal forms of failure.
Ultrasound and computed tomography make it possible to determine:
- kidney size;
- disturbed structure of the pelvis and calyces;
- development of a tumor compressing the kidney tissue and ureters.
In specialized clinics, radioisotope scanning is performed, which makes it possible to judge the degree of destruction of the kidney parenchyma.
Biochemical blood tests play an important role. A mandatory comprehensive examination before prescribing hemodialysis, plasmapheresis, hemosorption in each individual case is to study the level of:
- nitrogen-containing components;
- composition of electrolytes;
- acid-base reaction;
- liver enzymes.
Chronic kidney failure must be excluded in the diagnosis of long-term ill patients with pyelonephritis, glomerulonephritis, diabetes mellitus and other concomitant pathologies.
When questioning women, attention is always paid to complicated pregnancies and the occurrence of renal pathology during childbirth. First of all, it is necessary to fully examine to exclude the latent stage of chronic failure if the patient has:
- long-term dysuric symptoms;
- lower back pain;
- unclear temperature fluctuations;
- repeated attacks of renal colic;
- urinalysis reveals bacteriuria and leukocyturia.
When identifying any renal pathology, it is necessary to study the functional capabilities of the organs, make sure that both kidneys are functioning stable and that they have a reserve supply. Urine examination using the Zimnitsky method makes it possible to identify initial signs of functional weakness based on daily urinary arrhythmia.
Add information about the work of nephrons calculations:
- glomerular filtration rate;
- creatinine clearance;
- Rehberg test results.
In case of chronic pathology, there is more time to carry out:
- radioisotope diagnostics;
- excretory urography;
- dopplerography.
How is the prognosis for the patient’s health and life assessed?
If medical care is provided to a patient with acute renal failure in a timely manner, the prognosis can be considered favorable for most patients. They recover and return to their work and normal lives. Diet restrictions will apply for about a year. However, one should take into account the impossibility of counteracting some toxic substances, lack of access to hemodialysis, and late admission of the patient.
Complete restoration of kidney function after acute failure can be achieved in 35-40% of cases; in 10-15% of patients, kidney function is partially normalized; from 1 to 3% the disease becomes chronic. The lethal outcome in acute poisoning reaches up to 20%; patients die from general sepsis, uremic coma, and impaired cardiac activity.
The course of chronic renal failure in inflammatory diseases is associated with advances in the treatment of glomerulo- and pyelonephritis. Therefore, doctors attach great importance to the timely detection and treatment of exacerbations. The development of kidney transplantation does not yet compensate for the needs of patients.
Prevention of renal failure is carried out by people who fulfill all the requirements of the attending physician regarding diet, control examinations, regular preventive courses of treatment during periods of no exacerbation and do not shy away from hospitalization during an active process. Pathology is prevented by timely surgery for urolithiasis, tumors of the urinary organs, and prostate adenoma.
Any means of treating diseases that spread to the renal structures must be treated with due attention. Problems of diabetes mellitus and hypertensive crises do not bypass the sensitive vascular network of the kidneys. Recommended measures regarding regimen and diet are the least that a person can do for his health and preservation of his kidneys.
Is there prevention?
A healthy lifestyle is the best preventative measure.
To prevent chronic kidney disease, you need to take the following measures:
- drink alcohol in limited quantities;
- undergo timely diagnosis of deviations;
- do not take medications without the consent of the doctor;
- lead a healthy lifestyle.