When reading books written in the nineteenth century, we often encounter romantic characters suffering from consumption. The disease that we call tuberculosis today was in those days considered the result of a broken heart and a delicate mental organization. Doctors did not yet know about its contagiousness, therefore, they mainly recommended that patients travel to a warm climate, a healthy lifestyle and exercise in the fresh air.
Over two hundred years, medicine has made great progress, and now tuberculosis has almost left developed countries. However, our planet is large, and according to WHO, this disease is one of the ten leading causes of death worldwide. The disease is most common in developing countries, where there are few options for preventing and treating tuberculosis.
What are the symptoms of tuberculosis?
Some people become infected with Koch bacilli (the bacteria that causes tuberculosis) but do not experience symptoms. This condition is known as latent tuberculosis. The disease can “sleep” for many years before the latent form of the disease turns into an open one.
Active tuberculosis (as its open form is also called) has many symptoms. Most often they are associated with the respiratory system and are manifested by a prolonged cough with blood, sputum or mucus. A sick person may experience pain when coughing or even breathing normally. Other symptoms may include:
- unexplained fatigue
- elevated temperature
- night sweats
- loss of appetite
- weight loss
- enlarged lymph nodes
- "feverish" blush
Although tuberculosis usually affects the lungs, it can also develop in other organs - the kidneys, spine, bone marrow and brain. Symptoms will vary depending on the location of the lesion. For example, kidney tuberculosis can manifest as blood in the urine.
How dangerous is this disease for the patient’s health?
Pulmonary tuberculosis always leaves behind irreversible consequences, regardless of the patient’s age. The fact is that once the bacillus enters the respiratory tract, it begins to destroy lung tissue, namely, to kill specialized cells that saturate the blood with oxygen, which, like nerve cells, are not restored. After the death of the lung tissue, the body puts in its place a “patch” of ordinary connective tissue, incapable of performing the function of breathing, and also low-elastic, which leads to a decrease in the mobility of the lungs and a significant decrease in oxygen exchange. These scars on the lungs remain for life and are clearly visible on fluorographic photographs.
In addition to the fact that tuberculosis directly destroys the lungs, it also has a depressing effect on the entire body as a whole, since the waste products of the bacilli are extremely toxic.
Also, many people believe that pulmonary tuberculosis, skin tuberculosis or bone tuberculosis are different diseases. In fact, this is one and the same disease, caused by one pathogen that can affect any human tissue. It doesn’t matter what form the patient initially suffered from, in any case, tuberculosis can develop and then spread to other organs, including the brain, especially during an exacerbation.
Who is at greatest risk of contracting tuberculosis?
According to WHO, more than 95% of all tuberculosis-related deaths occur in low- and middle-income countries. People with long-term alcohol, nicotine or drug addiction are usually more prone to open forms of tuberculosis - as are those whose immune systems are weakened for one reason or another. Thus, tuberculosis is very dangerous for HIV-positive people.
Other risk factors for developing active tuberculosis:
- diabetes
- end stage kidney disease
- malnutrition (including eating disorders such as anorexia)
- some types of cancer
Medicines that suppress the immune system can also put people at risk of developing active TB. These include drugs that people take to prevent organ transplant rejection.
There are other medications that increase the risk of getting tuberculosis . They are used to treat the following diseases:
- cancer
- rheumatoid arthritis
- Crohn's disease
- psoriasis
- lupus
Traveling to regions with high incidence rates also increases the risk of contracting tuberculosis. Moreover, interestingly, from the point of view of the World Health Organization, some regions of Russia and other countries of the former Soviet Union are considered dangerous for tourists.
Other regions with high incidence rates:
- Sub-Saharan Africa
- India
- Mexico and other Latin American countries
- China and a number of other Asian countries
- islands of southeast asia
- Micronesia
However, not everything is going smoothly in the first world countries either. Homeless people, people in prison, and people with low incomes continue to be at high risk of contracting open TB.
Features of closed form tuberculosis
Today this disease is very common. According to the World Health Organization, at least a third of the world's population is infected with tuberculosis bacteria, with no more than 10% of those infected developing active tuberculosis.
The tuberculosis bacillus, having entered the human body, begins to affect the tissues of the respiratory organs or lymphatic system.
Since it is located inside the tubercle and does not break out beyond its limits, the lesion gradually begins to heal, but a compaction appears on the tissue. This is the first stage. But if the infection enters the patient’s blood, then multiple lesions are already formed. This is the second stage.
At any stage of this form, the infected patient does not release mycobacteria into the outside world. The infection inside a person is as if in a closed jar, the walls of which do not allow it to get out.
Patients with the closed form of tuberculosis are characterized by:
- a special diagnostic test (tuberculin test) shows a positive result;
- chest x-ray does not show lung problems;
- the patient does not feel unwell;
- sputum test for tuberculosis is negative;
- bacteria already living in the body are not active.
Sometimes infected patients experience a constant feeling of weakness and pain when breathing.
What causes tuberculosis and how is it transmitted?
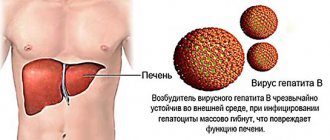
The disease is caused by bacteria called Mycobacterium tuberculosis (also known as Koch bacilli). There are several strains of pathogens, and, unfortunately, some of them have become resistant to drugs.
Koch bacilli are transmitted by airborne droplets (as is the coronavirus). When infected droplets of saliva become airborne, they can be inhaled by another person nearby. A person with tuberculosis can spread the bacteria in the following ways:
- sneezing
- cough
- talk
- singing
As we've already covered, people with a well-functioning immune system can become infected with tuberculosis but not show symptoms for many years. WHO believes that every fourth person on earth lives with a latent form of tuberculosis.
What danger does it pose to people?
If a tuberculosis bacillus gets inside the body, a person will not be dangerous. This is because microbes are not released into the environment.
Therefore, patients with the closed form of tuberculosis are not even admitted to dispensaries. They are treated at home, but always under the supervision of an experienced TB doctor.
With the help of a doctor, you can control the transition from one form of tuberculosis to another. It is also he who can refer a sick person to a hospital. This must be done without fail.
The SES must disinfect the room where such a patient was located.
This form of tuberculosis is not dangerous to others.
In this case, microbes are not released along with saliva or sputum. Thus, the infection is closed inside the body.
With the closed form of tuberculosis, transmission of the virus is impossible.
But sometimes tuberculosis in closed form can develop in the same way as in open form. This means that it has no characteristic symptoms.
In this case, the patient himself does not know that he has tuberculosis and can infect other people.
Therefore, whether a person with a closed form of tuberculosis is contagious or not is difficult to answer unambiguously. But you need to understand that when communicating with another person, the patient does not always transmit germs to him. This is only possible with weak immunity.
Most patients, in general, do not suffer from open tuberculosis, so for them it occurs only in the closed form.
How is tuberculosis diagnosed?
Skin (tuberculin) test
It is better known to us as the Mantoux reaction. The test is made with tuberculin, which, in fact, is a well-whipped cocktail of purified antigens of tuberculosis pathogens. A pronounced skin reaction at the injection site can be a sign of the immune system, which is very busy fighting tuberculosis pathogens.
The Mantoux test has no other role other than diagnostic (and it can also be wetted!).
Of course, the tuberculin test has its pros and cons (in particular, due to its not very high accuracy). But this is a cheap, fast and widely available test for diagnosing a serious serious disease. The Mantoux test is like a large sieve - it is designed to screen out “suspicious” cases in order to direct them to more specific and accurate tests.
Diaskintest works on the same principle as the Mantoux test . It is considered more accurate due to the lower rate of false positive results.
Blood analysis
If the reaction to the tuberculin test is positive (or after confirmed contact with a sick person), the doctor may prescribe more specific blood tests.
- General or biochemical blood test. Some indicators (for example, the number of leukocytes, lymphocytes and neutrophils, erythrocyte sedimentation rate) can indicate the patient's health status and the presence of an inflammatory process.
- Quantiferon test. This test shows the presence of antibodies to Mycobacterium tuberculosis in the blood, but will not provide information about which organ is affected. It will also be impossible to understand whether the disease is active or latent.
- Enzyme-linked immunosorbent assay (ELISA). It shows not only antibodies to bacteria, but also the presence of immunoglobulins. ELISA may not be entirely reliable for a number of reasons, so it is more often used to assess the effectiveness of treatment than for primary diagnosis.
- Polymerase chain reaction (PCR). This is the most accurate diagnostic method. During the study, DNA fragments of the pathogen in the blood or other biological fluids are evaluated. It also shows which organ is infected.
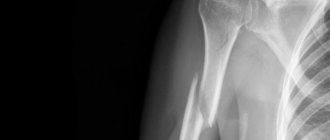
Chest X-ray (fluorography)
If the Mantoux test or blood test is positive, the person is usually sent for a chest x-ray to look for specific spots in the lungs. They are signs of infection and indicate that the body is trying to isolate pathogenic bacteria.
If the x-ray shows nothing with positive test results, most likely the person has a latent form of tuberculosis. However, a false positive test is also likely. Tuberculosis is very contagious, so annual fluorography is designed to promptly find people with an open form of tuberculosis.
Other tests
In addition to blood, tuberculosis can be indicated by analysis of sputum and mucus from the lungs. Detected mycobacteria means that the person can infect others and should wear a protective mask. Other tests (such as a CT scan of the chest, bronchoscopy, or lung biopsy) may be needed if other tests are unclear.
About carriage and infectivity
Despite the fact that the immune system has managed to cope with the inflammatory process, the remnants of Mycobacterium tuberculosis are not completely eliminated from the body, but settle in the lymph nodes. If the immune system malfunctions, the activity of mycobacteria can be activated, although only 5% of carriers develop an active form of tuberculosis. Therefore, it is so important to understand that infection does not equate to disease. No less significant is the fact that people who carry the Koch wand are not its distributors. They become dangerous to others only when the disease takes on an open form. In the saliva, sputum and other secretions of such people, active Mycobacterium tuberculosis is found, which can penetrate the body of a healthy person.
It should also be taken into account that people are not always able to independently determine whether their disease has entered the active phase, because often the onset of tuberculosis can be confused with a regular ARVI. Remaining not isolated from society, sick people spread the disease, infecting more and more people around them.
How is tuberculosis treated?
Many bacterial infections can be cured well with antibiotics in a couple of weeks, but the situation with tuberculosis is different. As a rule, when the open form is diagnosed, the medicine must be taken for six to nine months, in full course.
If you stop taking medications earlier, it is very likely that the tuberculosis infection will return, and in a form that is resistant to previous medications.
Treatment for tuberculosis can negatively affect the liver, so it is very important to regularly take biochemical blood tests and monitor the following symptoms:
- loss of appetite
- dark urine
- high fever that lasts more than three days
- unexplained nausea or vomiting
- jaundice or yellowing of the skin
- abdominal pain
If any of these symptoms appear, you should immediately consult a doctor.
Symptoms
At the beginning of the development of the pathological process, the symptoms are nonspecific and develop gradually, so the diagnosis of tuberculosis of bones and joints in the early stages is rarely established. The first symptoms include increased fatigue, irritability, decreased appetite, absent-mindedness, and an increase in temperature to low-grade levels.
Among the common symptoms found in many diseases, there are signs that you should pay attention to, namely:
- refusal of outdoor games and physical activity;
- aching or nagging muscle pain;
- limping that appears without previous injury or against the background of full health;
- enlargement of regional lymph nodes.
Further progression of the bone form of tuberculosis leads to the appearance of pronounced clinical symptoms and signs of joint damage appear.
Pus accumulates in the synovial bursa of the joints, which gradually destroys the surrounding tissue, leading to joint necrosis and the formation of fistulas. Ultimately, with delayed treatment, joint deformation and ankylosis occur. If you suspect bone tuberculosis, you must urgently seek medical help to make an accurate diagnosis.
How can you prevent tuberculosis?
Most people in high-risk areas around the world receive the TB vaccine as children, the well-known BCG vaccine.
Even if a person has not been vaccinated, the presence of pathogenic bacteria does not mean that the person will develop an active form of the disease; latent tuberculosis is more likely. To avoid its activation, the doctor may prescribe a prophylactic course of antibiotics.
Reducing the likelihood of infection also depends on people with open tuberculosis. According to statistics, each such person can infect 10 to 15 people per year if he does not take precautions. These include avoiding crowds, wearing a respirator, and social distancing.
Tuberculosis of bones
Bone tuberculosis is in second place in terms of prevalence after pulmonary tuberculosis. Every year, 300–350 thousand people die from bone tuberculosis in the world. You should not assume that tuberculosis of the bones, spine and joints is a disease that affects socially disadvantaged people. Severe illness can occur in representatives of any social circle and age (although according to medical statistics, adults get sick more often than children). In this connection, the following questions are logical: is bone tuberculosis contagious or not, what symptoms are observed during the disease, what are the measures to prevent the disease, and what modern approaches to therapy do TB specialists offer?
How is bone tuberculosis transmitted?
Infection of bone tuberculosis occurs through direct or indirect contact with a carrier of the infection. Mycobacteria that cause the disease enter a healthy body. There they spread quite quickly through the human lymphatic and circulatory systems. Together with physiological fluids, bacteria penetrate into various parts of the musculoskeletal system.