Laryngotracheitis is a process accompanied by combined lesions in the area of the larynx and trachea. Its appearance is caused by the presence of infection in the body. The picture is traditionally accompanied by a large number of manifestations that require immediate consultation with a doctor and competent therapy. When the disease is laryngotracheitis, symptoms and treatment in adults are closely related.
Causes and symptoms of damage in adults
Traditionally, the development of the disease occurs in childhood, although in some situations the pathology affects adult patients. The causes and symptoms often have a close relationship with ARVI and act as its complications in the event of a noticeable decrease in immune defense. In practice, laryngitis and tracheitis can occur separately, but often go hand in hand, accompanied by a similar clinical picture.
The key causative factors for the occurrence of laryngotracheitis are the following:
- bacterial processes, in particular – staphylococci, streptococci, tuberculosis;
- mycoplasma diseases;
- herpes and similar viruses;
- allergic reactions from the body;
- influence of chemical agents.
In the case of laryngotracheitis, symptoms and treatment in adults are related. The following nuances act as provocateurs and causative agents of the progression of the disease:
- excessive inhalation of air filled with dust and gases;
- excessively loud singing;
- “friendship” with alcohol, tobacco products;
- hypothermia of the legs and body as a whole.
Since the causes and symptoms of the disease are closely related to each other, the following manifestations can be distinguished:
- a sharp increase in body temperature;
- sore throat;
- discomfort in the chest area;
- dry cough accompanied by pain;
- during the manifestation of the cough reflex, pain in the chest becomes increasingly stronger;
- attacks occur during laughter, deep breathing;
- there is a slight discharge of sputum of increased thickness and viscosity;
- hoarseness in the head and excessive hoarseness;
- discomfort in the larynx, accompanied by dryness and burning.
As a result, the acute process becomes chronic. Its symptoms are expressed in the following phenomena:
- violation of speech and voice options;
- attacks of cough syndrome;
- frequent vocal fatigue.
Thus, there are many reasons for the appearance of the disease and the symptoms of its manifestation.
Acute stenosing laryngotracheitis: description and symptoms
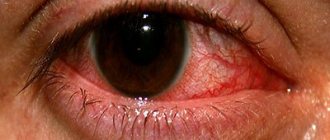
Acute stenosing laryngotracheitis traditionally affects the mucous membrane. You can become infected with it through airborne droplets during coughing, sneezing, or talking with a sick person. There is less risk of infection from household exposure. The development of pathology occurs 2-3 days after the onset of an acute respiratory disease; more often, the first symptoms make themselves felt at night. They are manifested by a rough cough, noisy breathing with whistling, shortness of breath, hoarseness, deterioration in general condition, including increased body temperature. There are signs of an inflammatory process in the upper respiratory tract. This is a runny nose, cough, redness.
Stenosis occurs in several forms, each of which is assigned a specific stage:
- Grade 1 does not imply any signs of insufficient breathing options;
- 2nd degree implies the manifestation of symptoms of deficiency in the form of pale skin, rapid heartbeat;
- 3rd degree is characterized by severe respiratory failure with persistent pallor of the skin, blue discoloration, and a feeling of fear;
- Stage 4 is accompanied by cessation of breathing and loss of consciousness.
Acute stenosing laryngotracheitis can occur in an uncomplicated, complicated, recurrent, descending form. Depending on this, therapeutic tactics are selected.
Features of the development of pharyngotracheitis in adults and children: symptoms and treatment methods
Pharyngitis and tracheitis are diseases that develop as localized inflammation.
But with a strong decrease in immunity or the presence of irritating factors, the inflammatory process affects both areas - the trachea and pharynx. In children and adults, acute pharyngotracheitis most often develops during the epidemic season under the influence of pathogenic microorganisms - bacteria, viruses and fungi, and also as a complication of other ENT diseases.
With pharyngotracheitis, the epithelium of the trachea and pharynx swells and becomes much redder. The tonsils become enlarged and the glands begin to produce much more secretion than usual. All this leads to a narrowing of the respiratory lumen, which is especially dangerous for young children.
The disease has a severe course, but responds well to treatment, provided that timely medical attention is sought. If tracheitis accompanied by pharyngitis is not treated, it becomes chronic or causes severe complications.
Diagnosis and treatment of acute and chronic pharyngotracheitis
Causes of pharyngotracheitis
Any viral, bacterial or fungal infection can cause pharyngotracheitis. Typically, infection occurs through airborne droplets, household or contact, and in the vast majority of cases the causative agent is viral microorganisms.
Therefore, pharyngotracheitis often occurs as a secondary disease accompanying influenza, adenoiditis, otitis media, prolonged rhinitis and other respiratory infections that affect the nasopharynx.
Important! Even when an infection penetrates the mucous membrane of the pharynx, an inflammatory process does not always develop. This requires minor provoking factors - hypothermia, stress, chronic fatigue.
The causes of bacterial pharyngotracheitis are staphylococci, Klebsiella, streptococci, Proteus, pneumococci. They penetrate the respiratory tract and cause a strong inflammatory reaction. Bacterial microorganisms penetrate the mucous membrane of the pharynx and trachea from other foci of inflammation during sore throat, sinusitis, purulent otitis, meningitis and other infectious pathologies of internal organs.
Various irritating factors can provoke inflammation:
- bad habits;
- contaminated air;
- inhalation of chemical fumes;
- allergic rhinitis;
- spicy food.
The disease occurs with a strong decrease in immunity, which is provoked by endocrine disorders, exacerbation of chronic pathologies, physical fatigue, taking cytostatics and immunosuppressants.
Types and forms of the disease
Depending on the course of the inflammatory process, otolaryngologists distinguish two forms of the disease. Acute pharyngotracheitis is characterized by rapid development, rapid increase in symptoms, and high fever. The disease usually lasts no more than 10 days, but the first improvements are observed already on the 3-4th day of properly selected therapy.
If you choose the wrong medications or refuse medical care, the disease becomes chronic.
The chronic process does not have pronounced symptoms, and during the period of remission it does not manifest itself at all.
With an exacerbation, blurred signs of the inflammatory process appear, which are also characteristic of other pathologies. Therefore, chronic pharyngotracheitis is often confused with the common cold, ARVI or acute respiratory infections.
Based on changes in the mucous membrane, three types of disease are distinguished:
- Catarrhal - characterized by redness and swelling of the pharynx, responds well to therapy.
- Hypertrophic - due to severe inflammation of the mucous membranes of the trachea and pharynx, the size increases greatly, the blood vessels dilate, and a large amount of fluid accumulates between the cells.
- Atrophic - with a protracted course of the disease, the epithelium becomes depleted, becomes dry and becomes crusty. Has the most unfavorable outcome.
They also distinguish the type of pharyngotracheitis depending on its origin - viral, fungal, bacterial, traumatic, allergic and others. Only a doctor is able to determine the type and form of pathology, and this allows him to select the most appropriate treatment.
Symptoms and manifestations of pharyngotracheitis in children and adults
Acute and chronic pharyngotracheitis have different symptoms. In acute inflammation, clear signs are observed that significantly worsen the patient’s condition and reduce performance.
The first symptoms of the disease resemble a cold. There is a slight sore throat, periodic cough, runny nose, and body temperature rises. In just a day they grow rapidly.
Characteristic symptoms of acute pharyngotracheitis:
- scratching pain in the throat;
- pain in the neck and chest;
- difficulty breathing, shortness of breath;
- painful cough;
- red rash in the oropharynx (more often in children);
- wheezing when breathing;
- general weakness;
- high body temperature;
- compaction of nearby lymph nodes.
In childhood, attacks of dry cough are especially severe and cause suffocation. That is why children with an acute form of the disease must be hospitalized, otherwise pharyngeal spasms can lead to respiratory arrest and death of the child.
Important! Prolonged coughing attacks that last more than half an hour can trigger the development of heart failure.
Symptoms of chronic pharyngotracheitis appear only during exacerbations, but do not bother the patient so much. Typically, an exacerbation does not cause a rise in temperature and has almost no effect on the general condition.
Characteristic symptoms are sore throat, mild cough, and slight discomfort in the throat. Atrophic pharyngotracheitis is accompanied by constant dry throat and painful sensations when swallowing.
Moreover, these symptoms can be painful not only during an exacerbation, but also during remission.
Diagnosis of the disease
If the symptoms described above appear, you should contact an otolaryngologist to confirm the diagnosis and get recommendations.
Diagnosis of pharyngotracheitis includes the following methods:
- Anamnesis collection.
- Pharyngoscopy.
- General blood analysis.
- Blood chemistry.
- Sputum culture tank.
- PCR research.
In case of chronic inflammation, additional studies are necessary - an immunogram, allergy tests, blood tests for rheumatoid factor and consultations with various specialists. Only a complete examination of the body will reveal what could provoke the transition of acute inflammation into a chronic course.
Features of treatment of pharyngotracheitis in children: medication, antibacterial, physiotherapy
Treatment of pharyngotracheitis in children should begin as early as possible to avoid undesirable consequences. Infants undergo therapy in a hospital setting, and adults and children after 3 years of age, subject to a mild course of the disease, can treat acute pharyngotracheitis at home. The doctor selects medications based on the causative agent of the infection, after receiving test results.
For a viral infection, antiviral agents are required:
Important! Antiviral drugs are prescribed by the attending physician, since only a specialist is able to adequately assess the child’s condition, select age-appropriate medications and correctly calculate the dosage.
For bacterial infections, antibiotics are indicated. Infants and young children are prescribed antibiotics for intramuscular injection to protect the gastrointestinal tract from their negative effects. If injection antibiotics are contraindicated and at an older age, tablets or suspensions can be used.
The most effective antibiotics for pharyngitis:
- Ceftriaxone.
- Cefazolin.
- Amoxiclav.
- Flemoxin.
- Suprax.
- Pantsef.
- Augmentin.
To support the functioning of the gastrointestinal tract and prevent the development of dysbiosis, the treatment regimen includes drugs containing beneficial bacteria - Bifidumbacterin, Linex, Bifiform, Acipol.
To reduce pain and fever:
In the treatment of pharyngotracheitis, inhalations play an important role. Drugs such as Berodual, Pulmicort and Atrovent are necessary to prevent laryngeal spasms and coughing attacks. They are used in short courses of 3-5 days and are canceled immediately after the condition improves.
To thin sputum and treat cough, inhalations with Lazolvan or Ambrobene are necessary. For antibacterial infections, inhalations with Fluimucil or Gentamicin are prescribed, if systemic antibiotics can be avoided.
You can take the following orally to treat dry cough:
- Gedelix.
- Gerbion.
- Erespal.
- Mukaltin.
- Overslept.
- Licorice root syrup.
- Marshmallow syrup.
When treating children after 3-4 years of age, gargling with a decoction of chamomile, calendula or sage is added to the treatment regimen. From pharmaceutical products you can use Furacilin, OKI, Rotokan, a weak solution of potassium permanganate or hydrogen peroxide.
After 4 years, you can use tablets and lozenges for resorption: Doctor MOM, Sage, Faringosept and Lizobakt. Sprays are prescribed with caution, as they can provoke asthma attacks. The most commonly used are Miramistin, Tantum Verde, Panavir, Ingalipt.
Treatment includes physiotherapy:
- Electrophoresis with aminophylline, lidase, potassium iodide.
- Ultraviolet irradiation.
- Inductothermy.
- SMT.
- Phonophoresis.
At home, the child must be given warm, frequent drinks. This could be tea, fruit drink, heated milk or chamomile decoction. The patient's room should be regularly wet cleaned and frequently ventilated, but without drafts.
How to treat pharyngotracheitis in adults?
Treatment of pharyngotracheitis in adults follows the same scheme as in children. The main difference is that they are prescribed stronger drugs, which are prohibited or undesirable to take at an early age.
What medications are suitable for adults:
- Antibiotics – Amoxicillin, Clarithromycin, Amoxiclav, Flemoclav.
- Antiviral - Antigrippin, Rimantadine, Kagocel, Ingavirin.
- Antifungals - Levorin, Fluconazole, Ketoconazole.
- Antipyretics – Paracetamol, Next, Ibuprofen, Acetylsalicylic acid.
- For cough - Bromhexine, Codelac, thermopsis tablets.
- For resorption - Strepsils, Septolete, Faringosept, Agisept.
For inhalations and rinses, the same drugs are prescribed as for children, but in larger dosages. On average, the course of treatment lasts 7-10 days, and if all recommendations are followed, pharyngotracheitis can be cured without leaving any consequences.
Possible complications and consequences
If you delay a visit to the otolaryngologist or do not follow his recommendations, then the inflammation from acute to chronic. Frequent relapses lead to decreased immunity and frequent respiratory infections. This is especially dangerous for infants and newborns - any cold or hypothermia provokes exacerbation and inflammation of other ENT organs.
The most common complications of pharyngotracheitis:
- Bronchitis.
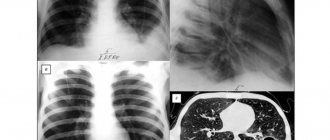
- Pneumonia.
- Angina.
- Laryngitis.
- Sinusitis.
- Otitis.
- Lymphadenitis.
Severe disease with prolonged attacks of suffocation can lead to heart failure. Therefore, after recovery, it is necessary to undergo an ECG to check the performance of the heart.
In chronic pharyngotracheitis, prolonged inflammation causes atrophy of the mucous membranes. This can cause the development of malignant neoplasms that metastasize to internal organs.
Forecast
With timely diagnosis, the disease responds well to treatment. Improvement occurs just 2-3 days after starting to take the drugs, and symptoms completely disappear after 1-2 weeks.
The prognosis is unfavorable for infants if they are not shown to a doctor when the first manifestations of the disease appear. The prognosis is also complicated if the patient has chronic pathologies and foci of infection.
Prevention of pharyngotracheitis
It is quite difficult to prevent the development of pharyngotracheitis, since too many factors can provoke the disease.
Therefore, the main way of prevention is to strengthen the immune system, for this you need to follow the following rules:
- do not abuse alcohol;
- give up cigarettes;
- harden;
- take vitamins;
- avoid sudden temperature changes;
- observe safety when working with chemicals;
- avoid contact with allergens;
- Healthy food.
You can support the functioning of the immune system and the entire body as a whole by avoiding stressful situations and physical fatigue. During epidemics, you can protect yourself from infection by avoiding crowds or wearing a medical mask.
Source: https://lor-24.ru/gorlo/osobennosti-razvitiya-faringotraxeita-u-vzroslyx-i-detej-simptomy-i-metody-lecheniya.html
Allergic laryngotracheitis and its manifestations
It is rare in adults and most often affects children under three years of age. This is due to the lack of resistance of the young body to allergens. The disease is usually classified based on the severity and stage of the lesion. In total, allergic laryngotracheitis has 4 stages of progression:
- the first is called compensated and involves the formation of a cough reflex, noisy inhalation and a “shallow” voice, its duration is in total no more than one daily period;
- the second stage involves the transition of the cough reflex into painful prolonged attacks, while the heartbeat is rapid;
- third degree implies shortness of breath, blue discoloration of the skin;
- The fourth phase of the disease is accompanied by the appearance of false croup, heavy breathing, and the likelihood of loss of consciousness increases markedly.
If, when diagnosed with allergic laryngotracheitis, the patient is not given appropriate assistance, he may die. You need to be able to make a differential diagnosis from a viral infection, since these conditions require different approaches to therapy. Symptoms of AL include the following:
- severe shortness of breath even after minimal physical exertion;
- increase in body temperature to 39 degrees;
- pale skin;
- runny nose;
- pain in the throat;
- problems with normal breathing;
- change in voice timbre;
- a cough that only gets worse over time.
An allergic disease occurs in response to a specific allergen that must be eliminated. With a lesion called laryngotracheitis, symptoms and treatment in adults are easy to determine.
Laryngotracheitis: symptoms in children
Laryngotracheitis primarily manifests itself as sudden bouts of coughing. At such moments the child breathes intermittently, noisily and restlessly. Closer to night time, these symptoms may worsen.
Symptoms of the disease:
- Hoarseness of voice.
- Blue lips and fingertips.
- Frequent attacks of shortness of breath.
Reference. The disease causes swelling in the mucous membrane of the throat. A reflex muscle spasm is possible when laryngotracheitis occurs. The glottis may become clogged with mucus.
Chronic laryngotracheitis: is it dangerous?
Chronic laryngotracheitis is a constant inflammatory process in the mucous membrane of these organs. It can have varying degrees of exacerbation and occur in various forms:
- the catarrhal type involves the appearance of slight redness, while the ligaments cannot close completely;
- hypertrophic pathology is associated with proliferation, with the development of a cough reflex and severe hoarseness;
- atrophic disease is represented by thinning of the mucous membrane, as well as changes in its structural elements.
Chronic laryngotracheitis develops during a severe condition of the respiratory tract. The main causes of development are the following lesions:
- the formation of cancerous tumors and neoplasms;
- presence of bad habits;
- physiological disorders of respiratory functions;
- systematic loads on the vocal apparatus;
- hormonal disorders and changes;
- problems in the gastrointestinal tract.
An extensive complex of forms and causative factors of the lesion has generated a large number of recommendations for the treatment of this form of the disease. However, it is much more difficult to treat, unlike the acute variety.
Classification
The severity of clinical manifestations is determined by the form of the disease and the provoking factors that caused inflammation. Pharyngotracheitis can occur in acute and chronic forms. If the disease develops suddenly and is accompanied by a severe cough, fever and sore throat, the patient is diagnosed with an acute form of the disease. Untimely and ineffective treatment of acute pharyngotracheitis can cause chronicity of pathological processes. With indolent inflammation of the trachea and pharynx, the symptoms are not so pronounced. However, with hypothermia, hypovitaminosis and a sharp decrease in immunity, relapses of inflammation occur. There are 3 types of pharyngotracheitis, which are determined by the degree of damage to the mucous membranes of the pharynx and trachea:
- catarrhal – characterized by redness and slight swelling of the ciliated epithelium in the ENT organs;
- atrophic – dystrophic changes are observed in the tissues of the respiratory tract; the mucous membrane becomes thinner and becomes covered with crusts, which provoke irritation and coughing attacks;
- hypertrophic - the ciliated epithelium slightly increases in size due to the expansion of blood vessels and swells; pathological processes in the mucous membrane stimulate the secretion of mucus in the trachea, resulting in a spastic wet cough.
The choice of drugs directly depends on the form of the ENT disease. As a rule, catarrhal inflammation of the pharynx and trachea is caused by a viral infection, which is treated with antiviral drugs. In turn, chronic forms of pathology are caused by bacterial inflammation, which can be eliminated only through antibiotics and local antiseptics.
Does the temperature increase with laryngotracheitis?
Elevated temperature with laryngotracheitis is a very common phenomenon, although there are practical cases when the disease proceeds without it. However, both children and adults need to constantly monitor this indicator. Traditionally, fluctuations in the mercury column are associated with the fact that the body is trying to fight an infectious or inflammatory process. That is, in fact, this is a very good sign, indicating the strength of the body. The general condition when fever occurs is aggravated by the following factors:
- general weakness in the body;
- the appearance of pain in the throat;
- the likelihood of vomiting;
- dry cough;
- runny nose.
In childhood, this condition is eliminated with relatively safe drugs - Nurofen, Tylenol, Efferalgan, Tsefekon, Panadol. Adults should take Paracetamol, Panadol for adults, Ibuprofen, Nimesil. Since the occurrence of high temperature is often associated with headaches, it is customary to use Spazmalgon, Ketanov, Analgin, Dexalgin.
Temperature with laryngotracheitis is quite normal, although not an obligatory sign. How many days does it last? Its duration is traditionally determined by the severity of the pathological process and its form. As a separate and independent feature, it can be added both within the acute stage and subsequently. On average, the mercury rises to 37.5 degrees and lasts for 5 days, but there are exceptions in the form of a mark of 39 degrees and a longer period. In such situations, the symptom requires immediate relief.
Signs, symptoms and complications of pharyngotracheitis
The symptoms of this disease are very unpleasant and are more local in nature than general:
- General weakness and malaise;
- Redness of the tonsils and their swelling;
- Hoarseness of voice;
- Enlarged lymph nodes;
- Sore throat when swallowing;
- Heat;
- Chills;
- Soreness and burning sensation in the throat.
Acute pharyngotracheitis begins with coughing attacks, wheezing in the throat and high body temperature. The most common reason for this is hypothermia. The chronic form does not manifest itself so clearly; it is not always taken seriously and is not treated immediately after rare coughing, mild hoarseness in the throat and squeezing sensations in the chest. These symptoms boil down to overwork or a mild cold, which is a big mistake. Chronic pharyngotracheitis weakens the immune system to almost zero and exposes the body to even greater danger in the form of many other diseases. If you do not start treatment on time and do not approach the problem seriously, you can get a bunch of complications:
- Pneumonia;
- Asthma;
- Bronchitis.
In addition, children and adults are at high risk of complications in the lymphatic system.
Laryngotracheitis: treatment of the disease, methods
If laryngotracheitis is diagnosed, treatment is carried out on an outpatient basis. A patient who is experiencing an acute process is recommended to consume a lot of liquid in the form of tea, compote, or jelly. An important role is played by etiotropic treatment, which consists of prescribing antiviral drugs:
- Remandatin;
- Umifenovir;
- Proteflazid;
- Interferon.
If we talk about the symptomatic therapeutic process, it is carried out through the use of antitussive, antihistamine medications, as well as mucolytic, antipyretic compounds. The optimal effect can be achieved using electrophoresis, inhalation, and immunomodulatory methods:
- Lycopid;
- Immunal;
- Broncho-munal.
If laryngotracheitis is diagnosed, treatment is reduced to other complexes. Vitamin C and multivitamin medications are prescribed. If the disease has progressed to the chronic stage, it is customary to use UHF therapy, electrophoresis, inhalation treatment, and massage measures. Surgical intervention is performed occasionally, in particular, in the absence of the desired result from the drug therapeutic process.
Is Berodual effective for laryngotracheitis?
Berodual for laryngotracheitis is prescribed quite often. This is a German product, produced in Italy, and has two common forms of release - drops and aerosol. The first form is mainly intended for children, offered for sale in 20 ml bottles in the form of a clear liquid that has neither color nor odor. The active ingredients of the drug are fenoterol, ipratropium bromide, and provide a bronchodilator effect. Indications for use are in the following conditions:
- bronchial type asthma;
- COPD disease;
- obstructive bronchial lesion;
- pulmonary emphysema.
Treatment with the drug Berodual for laryngotracheitis is carried out strictly under the supervision of the treating specialist and according to the dosage specified in the instructions.
The nature of laryngotracheitis
Larynx of a healthy child and a child with laryngotracheitis
Laryngitis in a child occurs when the larynx becomes inflamed. The area around the vocal cords becomes inflamed and becomes a source of pain. The disease is caused by viruses or bacteria, sometimes fungi.
The spread of inflammation to the trachea - the respiratory tube between the larynx and bronchi - occurs when measures to combat the infection are not taken in a timely manner.
Important! The downward transition of the area of insemination by infectious pathogens creates the preconditions for the development of severe infectious bronchitis and pneumonia. Allergic laryngotracheitis is no less dangerous - its complication threatens suffocation.
Therefore, treatment should begin with the appearance of the first signs of the disease.
Is Pulmicort effective for laryngotracheitis?
Pulmicort for laryngotracheitis is an inhalation agent widely used for the disease in question. It is hormonal and has an anti-inflammatory effect, especially against pulmonary obstruction and any types of bronchial lesions. It is designed for long-term therapy using a nebulizer. Immediate absorption into the mucous membranes occurs, and 1/3 of everything that the patient inhales penetrates the alveoli, which contributes to an auxiliary therapeutic result.
In comparison with classical inhalation formulations, Pulmicort for laryngotracheitis is considered the safest in terms of the occurrence of adverse reactions, therefore it is used even for the treatment of children. Adverse reactions make themselves felt only in case of intolerance to a number of components of the composition, as well as when the dose is changed upward, therefore it is necessary to strictly follow the instructions for use. Otherwise, there is a risk of encountering negative consequences in the form of depression, nervousness, candidiasis, dryness, and cough reflex.
How to treat laryngotracheitis: folk remedies
If you are diagnosed with laryngotracheitis, folk remedies will come to the rescue:
- the onion is grated, and then the pulp is sent to boiling milk in the amount of ½ liter, filtered without boiling, and drunk in one gulp at night;
- 100 g of carrots are boiled in half a liter of milk, and then filtered and consumed a little during the day;
- in case of acute injury, it is customary to use a decoction based on dried apples, which is drunk in ½ tbsp. twice a day;
- if you lose your voice, a decoction of cabbage leaves will help; for this, take a few leaves, wash them in water and brew until completely boiled, drink the remedy 3-4 r. in a day.
For the disease laryngotracheitis, folk remedies are used quite often.
Emergency care for laryngotracheitis: procedure
Emergency care for laryngotracheitis should be provided urgently to avoid complications.
- Provide the patient with bed rest, i.e., lying down for several days.
- Give him a warm drink - fruit drinks, fresh compotes, water, weak green or black tea several times a day.
- If there are complications, call an ambulance at home.
- Provide him with proper nutrition, excluding foods that irritate the mucous membranes of the throat.
Emergency care for laryngotracheitis is the key to a quick recovery.
We looked at what the disease laryngotracheitis is, symptoms and treatment in adults. A competent approach to organizing therapy guarantees a lasting effect.
Treatment of pathology
If the above symptoms appear, the child should be immediately shown to the treating specialist. As already mentioned, in its signs, nature of development and symptoms, laryngotracheitis resembles a number of viral diseases, and you can also learn in detail about the symptoms of tracheitis, because these diseases are very similar. The doctor will make an accurate diagnosis after conducting a full-scale examination.
First of all, the child is prescribed a course of inhalations. For these purposes, a special ultrasonic inhaler is used.
Treatment can also be carried out using steam inhalation. It is imperative to take precautions so as not to harm the child: hot steam can burn the mucous membrane of the larynx and trachea. For inhalation, use sea salt or any other alkaline-containing substance recommended by a pediatrician or otolaryngologist.
If laryngotracheitis occurs in an acute form, then the doctor must prescribe antibiotic pharmacological agents. Erespal is considered very effective. The dosage and duration of treatment is determined only by the treating specialist.
When do you need to seek emergency help from specialists?
There are cases when laryngotracheitis in children is accompanied by severe symptoms that are dangerous to health. In such cases, you need to call an ambulance. So, you should seek immediate medical attention if the following symptoms occur:
- if inhalation is accompanied by an uncharacteristic noise;
- if parents hear a whistle when exhaling;
- with lack of air (excessive shortness of breath);
- when the color of the skin changes (sharp pallor);
- if during inhalation the dimple in the child’s neck sinks heavily.
Advice from Dr. Komarovsky
As you know, the leading pediatrician, TV presenter and author of books, Komarovsky, does not always agree with specialists on the issues of curing a particular disease. If we talk about childhood laryngotracheitis, Komarovsky insists that the pathology can be cured not with antibiotics, but with an appropriate regimen. The doctor advises keeping in bed, drinking plenty of warm drinks and breathing fresh air.
To prevent the infection from affecting the bronchi, you should start taking mucolytic drugs in a timely manner. Inhalations and physiological procedures should be carried out when treating advanced forms of childhood laryngotracheitis.
Features of the regime during the treatment period
Parents should remember that the cure of childhood laryngotracheitis largely depends on the correct organization of the treatment course. In addition to taking pharmacological agents and performing inhalation procedures, during the treatment period you must adhere to the following rules:
- do not perform inhalation procedures if the child has a fever;
- the temperature in the children's room should be about 22°;
- the humidity level in the room should be between 50-65%;
- the child needs to be given foot baths and plenty of warm drinks;
- it is important to strengthen the child’s immune system with vitamins through the consumption of juices, fruit drinks, for example, cranberry drinks, compotes or soda water;
- you need to follow a moderate diet;
- During the treatment period, it is imperative to exclude spicy, sour and salty foods, sugar and chocolate products.