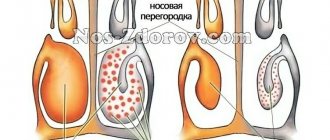
In fact, this organ is a pair, that is, there are two nasal cavities. They are separated from each other by the nasal septum. Each nostril opens at the front, and at the back it is connected to the nasopharynx by special openings. However, it so happened that these two departments are combined in speech under the name “nasal cavity”.
Its structure is more complex than it seems to an ignorant person. The walls of the nasal cavities, the bottom and roof of the cavity are rigid due to bone, cartilage and connective tissue of high density. It is because of this structural feature that the cavity does not collapse when inhaling.
Each nasal cavity is divided into two parts: the vestibule is the expanded area immediately behind the nostrils, and the respiratory cavity is a narrowed part located immediately behind the vestibule. The epidermis, which lines the cavity from the inside, contains a lot of hair follicles, as well as sweat and sebaceous glands. Why exactly is the nasal cavity lined this way? Its functions are cleansing, increasing humidity and air temperature, which is why it is so richly covered with blood vessels. Hairs can trap large particles in the inhaled air.
In the vestibule, the multilayered one belongs to the non-keratinizing type, then it becomes multirowed cylindrical ciliated, and goblet cells begin to appear in it. The epithelium becomes part of the mucous membrane lining the respiratory part of the nasal cavity.
The lamina propria of the mucous membrane here is adjacent to the periosteum or perichondrium, depending on whether this mucous membrane covers bone or cartilage. The basement membrane, which separates the respiratory epithelium from the lamina propria, is much thicker than in most other types of epithelium.
The epithelial surface is moistened with mucus, which is also produced by glands from the lamina propria. Up to 500 ml of mucus is produced per day. The latter mixes with particles of dirt and dust that stick to it, and thanks to the cilia, it moves to. Cleansing the nasal cavity largely depends on the condition of the cilia; if they have suffered from illness or injury, this process can be greatly disrupted.
In some places near the vestibule there are lymphatic follicles that perform an immune function. In the lamina propria of the nasal mucosa there are many plasma cells and lymphocytes, and sometimes granular leukocytes are also found. They “protect the borders” of the body, protecting us from invasions, because the nasal cavity often becomes the gateway to infections.
However, the cavity “works” not only with air; on the upper part of the walls, as well as the roof of the rear part of each area, there are special cells that make up the organ of smell.
There are two olfactory zones, one in each nasal cavity. The mucous membrane there forms a special organ, thanks to which we are able to smell. The peculiarity of this sensory organ is that the bodies of neurons there are located on the surface, which makes them truly vulnerable. Therefore, with injuries to the nose or chronic diseases, a person may lose their sense of smell. We lose another approximately one percent of our sense of smell for every year of life, which is why this important sense is so often impaired in older people.
Along the side plate of each cavity there are three bone plates, one above the other, like small shelves. They are slightly curved downwards, which is why they are called turbinates.
Also associated with the nasal cavity are those found in the bone cavities. The largest is located in the smaller sinuses - in the frontal, ethmoid and sphenoid bones. They are the ones that fill with mucus and sometimes pus during sinusitis. In this case, medications are prescribed that cause the patency of the sinuses to increase.
The nasal cavity is complex, because it must protect us, prepare air for the lungs and carry out the sense of smell.
The importance of the mucous membrane comes down to its protective function. If the largest dust particles are retained by a thick “picket fence” of hair on the vestibule of the nose, then the medium ones settle on the ciliated epithelium of the mucous membrane. His cilia seem to snatch dust particles from the inhaled air and, with oscillatory movements, move them towards the nasopharynx, from where they either enter the esophagus, which is not at all scary, or are simply cleared out. In addition, the mucous membrane contains many nerve endings, touching which dust particles cause sneezing, which can sweep away all the “garbage” from the upper respiratory tract.
Goblet cells and numerous glands closely monitor the humidity of the air, increasing secretion if it is dry and requires moisture. It is also important that the secreted mucus contains substances such as lysozyme, mucin, etc., which kill pathogenic microflora. It should be noted that when irritating substances enter the nose, the flow of tears into the nasal cavity through the nasolacrimal duct increases. This is necessary to dilute the irritating substance and its further removal.
The submucosal layer plays the role of an air conditioner due to its venous plexuses. If the air we inhale is cold, the veins expand, the amount of “hot” (about 37°C) blood in them increases, the mucous membrane warms up, and heat transfer to the air increases. If the air is too warm, the diameter of the vessels decreases, the mucous membrane “cools down” a little, after which it can take heat from the incoming air stream, cooling it somewhat.
Let us denote one more function—the resonator function. It turned out that the air-filled paranasal sinuses act as a resonator. And here is the proof: with a runny nose, although conduction through the nose may not be completely disrupted, swelling of the mucous membrane changes the volume of the sinuses, causing the voice to change its usual timbre, differing in some dull tones.
So, let’s summarize and list the functions of the nasal mucosa and nasal cavity
:
- Conducting air
from the external environment of the body to the nasopharynx and in the opposite direction. - purification
from large and medium-sized dust particles. - humidification
, dilution of chemical irritants. - Partial disinfection
. - Thermal correction
of inhaled air. - Reflexive call of protective actions
(from sneezing to temporary respiratory arrest). - Participation in lightening the mass of the skull
by filling the paranasal sinuses with air. - Resonator function
. - Olfactory function
. The nasopharynx belongs to the upper respiratory tract, although the rest of the pharynx also indirectly belongs to them, because the air passes through them before entering the larynx.
The nasal cavity is the beginning of the human respiratory tract. This is the air channel that connects the nasopharynx with the external environment. The nasal cavity houses the olfactory organs; in addition, the incoming air is warmed and purified here.
Drying of mucous membranes
At first glance, it may seem that the problem of dry epithelial cover is not worth special attention, but this is not so. Drying of the ciliated epithelium can lead to disruption of the cilia and, as a result, stagnation of secretions in the nose. This threatens the disease becoming chronic, as well as the development of rhinitis and sinusitis.
There are a number of proven remedies to eliminate dryness in the nasal cavity:
- Salt solutions. The positive effect of isotonic solutions (0.9% sodium chloride) has been proven by numerous clinical trials, diluting secretions, moisturizing the epithelium and restoring the functioning of cilia. The most popular drops and sprays are Dolphin, Humer, AquaMaris.
- Essential oils are best taken by inhalation, dissolving a few drops in water. The moisturizing and bactericidal effect of fir, mint, and eucalyptus oils is known. It is not recommended to drip directly into the nose to avoid burns.
- Nasal ointments (neutral, without medicinal substances) create a general moisturizing effect. Pinosol ointment and Oxolinic ointment have proven themselves well.
- When applied regularly, baby oil softens the skin and reduces the feeling of dryness.
If drying out of the epithelium occurs when taking intranasal medications, you should change them to alternative ones with a different active ingredient or stop using them altogether.
The main consequences of using vasoconstrictor nasal drops include disruption of the integrity of the mucous membrane, the onset of drug-induced rhinitis, and bleeding. Measures for rehabilitation of the mucous membrane are known: this is hydration and strengthening of blood vessels.
Since sudden cessation of taking vasoconstrictor nasal medications causes “withdrawal syndrome,” first of all, doctors recommend replacing them with alternative nasal medications (homeopathic, seawater-based, with natural oils), then physiotherapy.
You can also resort to traditional medicine methods that have already been tested for centuries.
The simplest composition of a spray or drops based on sea water is a saline solution with an active substance concentration of about 9 g/l (isotonic) or 20 g/l (hypertonic).
The action of preparations based on sea water is based on the property of salt to retain moisture. The advantages of these products are environmental friendliness, possibility of use during pregnancy and lactation, applicability in early childhood, non-addiction.
The spray form allows you to evenly distribute the product throughout the sinuses and the entire nasopharynx.
Sea water has the following qualities:
- antibacterial effect;
- moisturizing the mucous membrane;
- reduction of swelling;
- acceleration of tissue regeneration;
- local strengthening of immunity.
The therapeutic effect of nasal sprays and drops occurs within 5 seconds after use and lasts for 4 hours.
Reliable drugs include a series of nasal rinses in the form of drops and sprays of the Aqualor brand.
It has remedies used for sinusitis, rhinitis, adenitis, and therefore can be an adequate replacement for vasoconstrictor drops.
When spraying the drug onto the irritated mucous membrane, a burning sensation is observed due to exposure to salt, which goes away within 2 minutes.
You can also use sprays based on sea water - “Aquamaris” and “Quix”.
Regardless of the drug chosen, irrigation of the nasal mucosa must be done 4 times a day for 7 days.
Diseases of the nasal cavity - MedAnswer
There are many diseases affecting the nasal cavity, nasopharynx and paranasal sinuses.
They can have a very different nature, mechanism of formation, nature of flow and degree of danger. Almost every person has encountered at least one of them during their life.
The identification and treatment of these diseases is carried out by an otolaryngologist or, as he is also called, an ENT specialist.
Development of nasal diseases
Depending on the location of the pathological process, diseases of the nose and paranasal sinuses have certain differences. They can be divided into three categories:
- diseases of the external nose;
- diseases of the nasal cavity;
- diseases of the paranasal sinuses.
In addition, these processes can affect the brain, causing intracranial complications.
The nature of the runny nose
The symptoms of many diseases occurring in the nasal and sinus cavities are similar. In this regard, it is difficult to independently determine the diagnosis; to accurately determine the nature and localization of the disease, professional diagnostics using special equipment is required. The method of treatment will depend on this, since the disease can be:
- infectious disease of a bacterial, viral or fungal nature;
- inflammation of the mucous membrane caused by trauma of a mechanical, chemical, thermal and other nature;
- allergic reaction to respiratory irritants (pollen, dust, wool, etc.);
- complications of other diseases, including those not related to the respiratory system;
- expression of oncological changes in some areas.
Of course, with such a range of causes and characteristics, there can be no single treatment. It is also clear that eliminating the symptoms of such diseases is not only insufficient, but also unlikely.
Self-medication can aggravate the situation, for example, if you treat allergic symptoms with certain folk remedies, or treat a viral infection with antibacterial drugs.
The apparent simplicity and obviousness of the pathological processes occurring in the nose is extremely deceptive. Neglecting the treatment of these diseases, underestimating them, is very dangerous. A runny nose alone can be of the following types:
- spicy;
- chronic;
- chronic atrophic;
- chronic hypertrophic;
- vasomotor allergic;
- ozena.
How to distinguish one from the other, and what means of treatment to choose, should be determined by a specialist, especially since a runny nose is not always an independent problem; it often indicates the presence of another ENT disease.
Various types of sinusitis, for example, can lead to life-threatening complications.
Paying timely attention to a symptom such as a runny nose will help identify the disease at an early stage and cure it, using less effort and with the greatest effectiveness.
General symptomatic picture
Many diseases of the nose and paranasal sinuses have similar symptoms. This is due to the fact that the mucous membrane is affected first. Her reaction to the pathological process is identical - she intensifies her work, sometimes undergoing some changes. As a result, a person experiences:
- intense secretion of mucus from the nose;
- violations of the respiratory function of the nose;
- development of swelling of the nasal mucosa;
- swelling of the face;
- general malaise, painful state of the body;
- sometimes (especially in the acute form) body temperature may rise;
- nasal (sometimes ear) congestion, voice changes, nasal sound;
- headaches (less often toothaches);
- disturbances of appetite, sleep;
- complete or partial loss of smell, etc.
Symptoms, depending on the type of ENT disease, may have some differences or characteristic features. However, from the overall picture it is clear that relying only on it, it is almost impossible to determine the disease.
Such manifestations occur in colds, acute respiratory viral infections, sinusitis and many other diseases. To make a diagnosis, computer and magnetic resonance imaging are used, as well as laboratory tests, allergy tests, etc.
Based on the duration and frequency of symptoms, all diseases can be divided according to the degree of development into:
- primary;
- spicy;
- chronic.
As a rule, recently appeared, moderately severe symptoms indicate the primary stage, pronounced symptoms lasting about three weeks indicate an acute form, and those recurring 3 to 4 times a year indicate a chronic form of the disease.
Types of nasal diseases and their treatment
All diseases of the nasal region can be divided into diseases of the organ itself and the internal cavities and sinuses. Diseases of the nose are easier to treat, since local remedies are available, and bring fewer internal complications, but often have a visual manifestation.
Diseases of the external nose
These diseases affect the outer part of the nose and adjacent areas of the skin and glands.
Unlike diseases that originate in the paranasal sinuses and nasal cavity, diseases of the external nose become noticeable immediately.
In most cases, they are accompanied by pain and discomfort and are determined visually. Using the example of the most common diseases of this type, we will consider their symptoms and treatment:
- Erysipelas. Or as it is more often called, erysipelas, is an infectious disease, expressed in swelling and redness of the affected area. In a person, the skin of the vestibule of the nose becomes inflamed.
The infection is streptococcal, introduced into the skin through microtraumas, such as cracks, scratches, scratching, etc. For treatment, antibacterial drugs are used, to which streptococci are sensitive. Antibiotics are administered intramuscularly or taken orally. A local effect on the affected area of the nose does not make sense.
- Furuncle. It occurs quite often; it is considered as a disease of the external nose if the inflamed hair follicle or sebaceous gland is located in the area of the wings of the nose, on its tip or septum.
It appears as a clearly defined lump (purulent lump) about the size of a pea. If several hair follicles or glands become inflamed at the same time, then this phenomenon is called a carbuncle. Most often, the abscess is opened surgically, after which a special bandage is applied, antibiotics or topical ointments may be prescribed.
- Rhinophyma. This is an inflammation in which there is a strong proliferation of all layers of the skin of the nose. Localized in the area of the wings and tip of the nose. It is expressed in the form of the formation of tubercles, greatly changing the outline of the nose and face as a whole. With a significant degree of hypertrophy, it can stretch out and hang down, interfering with normal respiratory function and food intake. Surgery is used as treatment.
Diseases of the nasal cavity
There are a huge number of them. They affect the mucous membrane, bone and muscle structures, nasal septum, blood vessels, etc.
Diseases are of a very different nature, can be caused by a variety of reasons and require an individual approach to treatment.
Depending on the type of disease, classical therapy or surgery may be used. Sometimes drug treatment is prescribed in the postoperative period.
Modern surgical methods, as a rule, are minimally invasive, low-traumatic, and do not require long-term recovery. Some can even be performed on an outpatient basis. Drug therapy is prescribed individually. Here are just a few diseases that fall into this category:
- nasal polyps;
- rhinitis;
- nose bleed;
- nasal injuries;
- chemical burn;
- synechiae of the nasal cavity;
- hematoma of the nasal septum;
- deviated nasal septum;
- foreign bodies in the nasal cavity.
Any of these diseases can and should be treated. It is better to do this after consulting a doctor. Even the use of folk remedies should be coordinated, since in some cases they can cause harm rather than benefit.
Neglecting treatment for even a seemingly simple runny nose can lead to the development of more serious diseases, and those, in turn, to dangerous complications.
Many pathological processes in the paranasal sinuses arise precisely as a result of untreated diseases of the nasal cavity.
Diseases of the paranasal sinuses
When talking about this category of diseases, sinusitis is first of all assumed. In fact, sinusitis in Latin means inflammation of the sinuses. Sinusitis occurs due to inflammation of the mucous membrane of one or more paranasal sinuses. Depending on which of them the inflammatory process develops, diseases such as:
- frontal sinusitis;
- sinusitis;
- ethmoiditis;
- sphenoiditis
They arise for several reasons. For example, nasal polyps can be both a consequence of inflammation of the paranasal sinuses and its cause. Frequent and/or untreated respiratory diseases can also cause inflammation.
Types of sinusitis
There are sinusitis of an allergic nature, as well as those caused by a bacterial, viral or fungal infection. Favorable conditions for the development of sinusitis occur with various injuries and curvatures of the nasal septum.
- Frontit. This disease is an inflammation of the frontal paranasal sinus. Under the influence of one of the possible causes, inflammation of the mucous membrane occurs.
Mucus begins to accumulate in the sinus, which is eliminated through the nasal passages. Thus, one of the symptoms of frontal sinusitis appears - a runny nose.
Another characteristic feature of this disease is headache predominantly in the frontal lobe. When the head is tilted forward, the pain intensifies.
The acute form is often accompanied by increased body temperature and general weakness.
At the initial stages, conservative therapy is used; in case of a more severe form of the disease, as well as in case of ineffectiveness of previous treatment, surgical intervention is prescribed.
- Sinusitis. A fairly common disease, which is an inflammation of the mucous membrane of the maxillary (maxillary) sinus.
The symptoms are similar to the previous case; to them you can add toothache, which is uncharacteristic of frontal sinusitis. As a rule, pain occurs in the upper jaw area.
In addition, pressing pain in the forehead, intensifying as purulent accumulations in the sinus increase.
Sinusitis can be treated either conservatively or by puncture, followed by drainage and treatment of the affected cavity. First of all, the goal of therapy is to relieve swelling of the mucous membrane, drain pus from the sinuses, and stop the inflammatory process. Various physiotherapeutic procedures are actively used in the treatment of sinusitis.
- Ethmoiditis. Inflammation of the ethmoid labyrinth is called ethmoiditis. It occurs for the same reasons as other sinusitis, the symptomatic picture is also identical.
However, ethmoiditis is dangerous due to its complications due to the location of the ethmoid labyrinth itself. In close proximity to it are the orbit, anterior cranial fossa, and ethmoidal arteries.
Damage to these anatomical structures is very dangerous.
Vasoconstrictors, antibacterial, anti-inflammatory and antifungal drugs are used for treatment, as with other sinusitis.
Also often after surgery, sinus rinsing using special solutions is prescribed.
- Sphenoiditis. This is an inflammation of the mucous membrane of the sphenoid sinus. Its location is characterized by the proximity of the pituitary gland, carotid artery, and optic nerve. It is natural that when complications arise, these structures are under threat.
It is advisable to identify the disease as early as possible.
Its presence is indicated by such characteristic symptoms as a headache in the back of the head, while mucous discharge (runny nose) is often absent due to the fact that in this case the mucus flows mainly along the back wall of the nasopharynx.
The principle of treatment is generally the same as in the previous case. The doctor selects drug treatment on an individual basis and, if necessary, prescribes surgery. Self-treatment of sphenoiditis, like other sinusitis, with folk remedies is ineffective, undesirable, and sometimes downright dangerous.
Did the article help you?
Let us know about it - rate it
Source: https://medotvetu.ru/%D0%B7%D0%B0%D0%B1%D0%BE%D0%BB%D0%B5%D0%B2%D0%B0%D0%BD%D0%B8 %D1%8F-%D0%BD%D0%BE%D1%81%D0%BE%D0%B2%D0%BE%D0%B9-%D0%BF%D0%BE%D0%BB%D0%BE %D1%81%D1%82%D0%B8.html
Facilities
There are different treatment methods, from folk remedies to medical treatment. Before choosing any remedy, it is best to consult with a specialist or your doctor.
However, in most cases, according to doctors, the cause of dryness should first be determined.
For example, if it is caused by dry indoor air, you should increase the humidity level using an air conditioner or an electric fountain. It is even permissible to place bowls with clean water on the windowsills. In addition, you need to drink up to 1.5 liters of fluid daily.
If the reasons for the constant drying of the nasal mucosa lie in an allergic reaction, you need to determine it by passing tests and get rid of the allergen. Dry nose can be relieved using various remedies, both folk and medical.
Medications for dry nose
It is best to seek medical advice immediately so that the disease does not become chronic.
Pharmacies have different products to suit every taste and budget. Most often, there are various drops and sprays that help reduce itching and effectively fight infections and bacteria.
Vitaon balm helps to moisturize the sinuses well.
These are products such as Aqua Maris, Pinosol. It is best to use products that are oil-based and do not contain corticosteroids, i.e. drying substances. Among the ointments, we can distinguish Spasatel, Pinosol, Traumeel S. They gently and carefully moisturize the nasal mucosa.
Vitaon balm helps a lot. It softens the nasal mucosa deep inside, helps fight its cracking, and heals well.
ethnoscience
Since ancient times, proven folk remedies have come to us that can help with many problems that a person faces during his life:
- To moisturize your nose, you can use water with silver ions.
- At night you can also use aloe juice. They are good for nose drops, just like Kalanchoe or carrot juice.
- Inhalations with herbal components have a good effect.
- A mixture of tea tree, grape and olive oils. Apply this mixture to each nostril daily.
- Tea with honey or lemon is beneficial at later times of the day. Tea, if desired, can be replaced with warm milk.
- Inhalation is an effective method of moisturizing the mucous membrane. It can be done using various saline solutions or herbal infusions. Inhalations are a popular way to combat this problem. Various oils and solutions can be used to carry them out. The widely known eucalyptus is often used for these purposes in the form of oil.
- Doctors consider sinus irrigation to be an effective option. Sea salt works great for this. It kills all infection and fights viruses.
All the remedies described help eliminate unpleasant symptoms and increase immunity.
During treatment you need to drink a lot of water. It must be cleaned first. In addition, you need to monitor the air humidity in the room. If necessary, you should use sprays.
These methods will answer the question of how to remove dry nose forever if it is caused by non-painful reasons.
If home treatment does not help, you should immediately consult a doctor. He will conduct a diagnosis and be able to prescribe the necessary procedures. Prescribe more serious medications. You should not self-medicate. It is worth noting that if the disease is ignored, pus may form or bleeding may occur.
Symptoms and signs of mucosal inflammation
Inflammation of the nasal mucosa manifests itself in different ways, but most often patients complain of heavy nasal discharge, congestion and sneezing. Since the same symptoms appear with a common cold, many people ignore the disease or self-medicate.
But if the therapy is chosen incorrectly, there is a possibility of developing pathological processes leading to the appearance of eczema, furunculosis or sinusitis.
Currently, doctors classify the disease according to specific symptoms characteristic of a particular type of rhinitis.
Infectious rhinitis
Damage to the nasal mucosa occurs due to various viruses entering the body. Most often, microorganisms of the genus Microplasma and Candida act as the primary source. Infectious inflammation of this kind is always accompanied by an increase in body temperature and severe weakness; patients often complain of a burning sensation in the nose area. With such a lesion, profuse nasal discharge appears, having a transparent or white tint.
Vasomotor rhinitis
The peculiarity of such a lesion is that it is not accompanied by a runny nose, but the person will suffer from severe congestion, which occurs mainly in the morning. In rare cases, vasomotor rhinitis is accompanied by copious watery discharge and frequent sneezing.
Allergic rhinitis
With such a lesion, the patient will suffer not only from heavy discharge and sneezing, but also from itching in the nose and increased tearing of the eyes.
This type of disease is most often diagnosed in the spring and summer. Experts assure that at the initial stage, damage to the nasal mucosa always occurs in an acute form, but in the absence of timely and competent treatment, the disorder can transform into a chronic form of the disease.
Chronic rhinitis is dangerous because it will complicate the patient’s life at certain intervals, while the symptoms of the disease will not go away for a long time.
Why is the mucous membrane in the nose damaged?
The nasal mucosa can be injured under the influence of various negative factors. Usually the cause is the incorrect use of nasal drops with a vasoconstrictor effect for too long. These substances dry out the nasal cavity, disrupt the microflora, causing a medicinal form of a runny nose. The disease causes constant swelling in the nose, which can only be relieved by administering a new dose of medication. At the same time, the surface becomes thinner, and it is no longer possible to refuse the drops without special medical care. So, in the end, surgery of varying volumes of intervention may be required to restore nasal breathing.
Other reasons include:
- constant inhalation of dirty air, for example, when working in a chemical production plant, weaving factory, etc.;
- entry of a foreign body into the nasal cavity;
- addiction;
- inhalation of scalding steam;
- curvature of the nasal septum, which provokes a narrowing of the nasal passages and complications of the correct outflow of produced secretions, as a result, the development of ENT pathologies;
- chronic diseases of the kidneys, heart, blood vessels, thyroid gland.
Temporary symptoms of damage to the nasal cavity are observed after surgery. They also occur as a result of taking drugs that burn the inner lining of the nose.
Hypertrophic rhinitis
Hypertrophic rhinitis is a polyetiological disease that can progress over a long time. It is a thickening of the nasal mucosa and hyperplasia of the tissues underneath, replacement of the epithelium with connective tissues. The causes of this pathological growth include:
- frequent recurrences of the runny nose - more than 3 - 5 cases in one year;
- congenital or acquired disorders of the structure of the nasal passages, injuries to the facial skeleton, which ultimately lead to impaired mucus discharge and stagnation;
- exposure to negative environmental factors - long-term stay in places with too low or high temperatures, inhalation of gases, dust, work in hazardous industries;
- heart and vascular diseases - hypertension, atherosclerosis provoke problems with the supply of a sufficient amount of blood with nutritional components to the nasal mucosa, which ultimately leads to tissue hypoxia;
- other pathologies of the nasopharynx are polyps, cysts, adenoids; all diseases cause persistent swelling and tissue hypertrophy in the nasal passages.
Structure
The outer side of the nose consists of the nostrils or wings, the middle part or back and the root, which is located in the frontal lobe of the face. The bones of the skull form its walls, and the palate limits it on the side of the mouth. The entire nasal cavity is divided into two nostrils, each of which has a lateral, medial, superior, inferior and posterior wall.
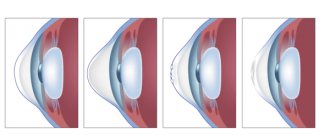
The nasal cavity is built with the help of bone, membranous and cartilaginous tissue. The whole of it is divided into three shells, but only the last of them is considered true, since it is formed by bone. Between the shells there are passages through which air passes; these are the top passage, the middle passage and the bottom passage.
On the inside of the cavity is the mucous membrane. The mucous membrane has a small thickness and performs several functions at once: it cleans and warms the air, and also helps to distinguish odors.
Moisturizing drops
Currently, pharmacies offer a huge number of moisturizing nasal drops that can moisturize a dry nasal cavity. These are medicines made from purified sea water. They contain only salts and water.
This group of medications includes the following drops and sprays:
- AquaMaris;
- Salin;
- AquaMaster;
- Aqualor;
- Marimer;
- Physiometer;
- and many others.
Additionally, read the article: “Marimer - instructions for use.”
The main advantage of these medicines is their exclusively natural origin and the complete absence of contraindications. There can be no overdose when using them. Even if you try very hard, you will not harm your health.
If you don't have enough free time to systematically rinse your nasal cavity several times a day, there is a more practical solution. You can use nasal sprays and.
When the mucous membrane of your nose dries out, the decision to moisturize it with just such medications will be absolutely correct and adequate.
Diseases of the nasal cavity - the profile of our ENT clinic
Highly qualified specialists of our clinic will conduct the necessary examination, make a diagnosis, carry out all the necessary manipulations and procedures at one of the best prices in Moscow.
| Medical service | price, rub. |
| Reduction of the nasal mucosa | 500 |
We are located at: Moscow, 5th Monetchikovsky lane, building 14, a four-minute walk from the Paveletskaya metro station (ring).
Certificates and licenses
You can make an appointment by calling the reception at +7 (495) 642-45-25. We will be glad to see you!
Make an appointment
How to moisturize the nasal mucosa
Preparations for moisturizing and rinsing the nose have no age restrictions for use. They are prescribed to infants from birth, pregnant women, and the elderly.
- Aqua Maris are moisturizing nasal drops, which are prescribed mainly in pediatrics, and an aerosol. The product is produced on the basis of sea water, which contains trace elements (calcium, magnesium, sodium, chlorine). Newborns receive 2 drops. 4 times a day. The spray is used from 1 year. Preschoolers receive 2 injections into each nostril 4 times a day. Children over 8 years old and adults are allowed to use up to 8 times daily. The drug can be used for a month.
- Aqualor - solution is available in the form of drops (Aqualor Baby) and nasal spray in a metal container. Produced from seawater from the Atlantic coast of France. The drug contains zinc, iron, copper, potassium, calcium, chlorine, sodium. The product is used 2 to 6 times a day. For calm babies, an aerosol can be used. The spray nozzle has a restrictive ring for maximum penetration into the nasal passages.
- Humer is a sterile isotonic solution made from sea water. For a baby of the first year of life, 1-2 drops are given up to 3 times a day. For a child from 1 to 7 years old, 2 drops 3-4 times a day or 1-2 injections into each nostril. The drug is used for 2-4 weeks, repeated courses are carried out at intervals of 1 month.
- Salin is a physiological solution of sodium chloride. For children with dry nasal mucosa, use under adult supervision. For infants, irrigation is carried out in a lying position. When the bottle is inverted, the drug with liquid is used in the form of drops, in a vertical position in the form of a spray. Up to 1 year, drop 1-2 drops 3 times a day, from 1 year - 3-4 sprays 2-3 times a day.
- Marimer is a hygienic product based on sea water and isotonic solution. Available in the form of intranasal aerosol and drops. Use 4 to 6 times a day according to instructions.
- Quickx - is produced on the basis of natural ocean (Atlantic) water, contains 2.6% salt. For the first few seconds after spraying, the solution may cause a burning sensation in the mucous membrane. The drug is used from 3 months. The time interval between using the liquid must be at least 8 hours.
- Dolphin – contains sea salt, soda, dry extract of licorice and rosehip. Contraindicated in children under 4 years of age, as well as in cases of complete nasal congestion. Irrigation of the mucous membrane is carried out 1-2 times a day. Duration of treatment is no more than 2 weeks.
At home, you can moisturize the nasopharyngeal mucosa using vegetable oils:
- sea buckthorn;
- grape;
- olive;
- sunflower.
Oils contain vitamins, beneficial macro- and microelements. They contain fatty acids (stearic, linoleic, oleic). Oils effectively moisturize the nasal mucosa and gently remove dried crusts without microtrauma. Promote rapid restoration of the epithelium during inflammatory or atrophic processes. The water-electrolyte balance and pH environment are regulated. The drug is applied to the epithelium using a cotton swab soaked generously in oil. You can instill 1-2 drops into the nasal passages 2 times a day.
A spray for moisturizing the nasal mucosa based on sea water, drops, and medicated oils are well tolerated by patients of all ages. They have no contraindications, with the exception of individual intolerance. There were no signs of overdose in clinical practice. The drugs can be used for both therapeutic and prophylactic purposes.
Restoring the nasal mucosa at home
First, you need to determine the reason for the irritation of the mucous membrane, and only after that begin to eliminate it. If this is a defect of the nasal septum, then therapy should be exclusively surgical. During the operation, the doctor will perform nasal plastic surgery and improve the patient's breathing ability. If the reason is a person’s professional activity, then it is worth reconsidering its feasibility. A person’s choice should fall on improving the quality of health and life.
The most difficult situations are cases where irritation of the mucous membrane began after drops with vasoconstrictor properties. Such patients cannot refuse medications because they immediately experience symptoms of a runny nose. The doctor should suggest a drug withdrawal plan. First, they gradually reduce the frequency of their use, and then completely abandon them.
Once the dependence on vasoconstrictors has been reduced, you can begin procedures to restore and strengthen the mucosa. For this purpose, folk remedies that have anti-edematous, anti-inflammatory and antiseptic properties work well:
- A decoction of chamomile, yarrow or string. 1 tbsp. l. dry chamomile or string is poured with a glass of boiling water and set to simmer on low heat for 15 minutes. After time, the composition is filtered and cooled to room temperature. This decoction should be used to wipe the nasal mucosa several times during the day. Store the decoction in the refrigerator.
- Aloe juice is mixed with an equal amount of water and 5 drops are dropped into the nostrils. Aloe is a very good remedy that improves the regeneration process, as well as promotes tissue hydration and restoration of microflora after colds.
- Peach and eucalyptus oils must be mixed in equal quantities. Cotton swabs are moistened with this composition and inserted into the nasal passages for 15 minutes. Application twice a day is sufficient for the condition of the mucous membrane to significantly improve.
Treatment methods
It will take more than one week to restore the nasal mucosa after using vasoconstrictor drugs. It is necessary to stop taking them and to alleviate the condition and switch to rinsing with saline solutions (Delufen, Aqua Maris, Salin, Humer). Functions will gradually normalize and symptoms will subside.
Subsequently, during exacerbations or new cases of rhinitis, it is recommended to use local corticosteroids, for example, mometasone or fluticasone furoate, propionate (Nasonex, Avamys, Flixonase, respectively).
To restore the nasal mucosa as a result of 1-2 degree burns, no special local measures are required. Immediately after an injury, rinsing with a light stream of cool water is indicated. If prescribed by a doctor, you can undergo a course of antibiotic therapy to prevent the addition of a bacterial infection. To reduce pain, you can use cotton swabs soaked in an analgesic (Novocaine, Lidocaine) only after consulting a doctor, as they can cause allergies. For chemical burns, treatment is carried out in a hospital. Consists mainly of antibiotic therapy and observation.
To treat damaged nasal mucosa, various forms of drugs are used:
- drops and rinsing solutions;
- ointments;
- sprays.
Among drip medications, preference is given to natural-based medications (Pinosol, Pinovit, Malavit-Rino, Vitaon), which have a complex effect and a minimum of complications. These types of nasal drops, in addition to normalizing the functions of the mucosal vessels, correct the characteristics of the secreted secretion (they dilute it, normalize the quantity), and also have an antiseptic and moderate antimicrobial effect.
It is especially convenient to restore the mucous membrane of a child with just such natural drops. For infants and children up to one year old, Nazivin (0.01%), Noxprey-Baby, Aqua Maris, Humer Spray (from 1 month) are recommended. For older children, we can recommend Delufen, Pinosol (from 2 years), Malavit-Rino (from 3 years).
An ointment based on natural oils effectively promotes the restoration of the mucous membrane. Peach and sea buckthorn, as well as rosehip, are used. Peach - helps heal after burns, has an anti-inflammatory effect, helps improve metabolism in the area of application; sea buckthorn - strengthens the vessels of the mucous membrane, normalizes their permeability. Rosehip, like peach oil, stimulates healing after burns and improves metabolism.
At the same time, the use of oxolinic or naphthalan ointment is not justified. The first has no evidence of effectiveness, the second is not indicated for the treatment of processes on the mucous membranes.
A spray, as a form of drug administration to restore damage to the internal surfaces of the nose, has a number of advantages over drops:
- more evenly distributed throughout the mucosa;
- does not leak and can be used anywhere (on the road, in transport);
- has a high dispersion, so it penetrates into tissues faster;
- the dosage of the active substance is adjusted (especially when using corticosteroids).
Most drugs in drop forms are produced in the form of sprays - Humer, Aqua Maris, Nazivin, Noxprey, Nasonex, Avamis, Flixonase.
Burnt mucous membranes can also be treated with modern hardware methods. In particular, using a laser. The method is based on the evaporation of excess capillaries of the mucous membrane and the creation of local controlled ischemia in areas of hypertrophied tissue. At the same time, the trophism of the latter naturally decreases, swelling in the nasal cavity decreases, breathing improves, and the sense of smell is restored. The method is painless, does not take much time and has minimal side effects. The advantage of laser therapy is the elimination of the pathogenetic link of rhinitis, and not the relief of symptoms.
Functions of the nose and nasopharynx
The nose consists of three parts. They all have their own characteristics. All sections are covered with a mucous membrane and the more of it, the better the air is processed.
It is important that this type of tissue is not susceptible to pathological conditions. In general, the nose performs the following functions:
- Heating cold air and preserving it;
- Cleansing from pathogens and air pollutants (using the mucous surface and hairs on it);
- Thanks to the nose, each person has his own and unique timbre of voice, that is, the organ also works as a resonator;
- Discrimination of odors by olfactory cells located in the mucosa.
Each part of the nose is structured differently and is responsible for a specific job. At the same time, the rather complex structure of osteochondral tissue allows for better processing of the incoming air flow into the lungs.
What is anemization and when is it done?
Anemization of the nasal mucosa is the artificial “bleeding” of the mucous surface of the nose. It is carried out by introducing vasoconstrictor drugs into the required anatomical area.
The main benefit of this procedure is the complete relief of swelling during inflammation. Anemization is also carried out before operations to prevent severe bleeding, for example, before puncture of the maxillary sinus.
As a means for the procedure, a composition is used, including:
- a drop of adrenaline solution with a concentration of 0.1%;
- 1 ml of ephedrine solution at a concentration of 3%.
If anemia of the deep sections is needed, the medicine is administered through a probe with an attached. The solution only takes 1-2 minutes to take effect. Indications for anemization are:
- acute, chronic runny nose;
- frontal sinusitis;
- sinusitis;
- otitis;
- inflammation of the mucous membrane as a result of hypersensitivity;
- before implementing drainage to eliminate Eustachian tube dysfunction;
- before examining the nasal cavity - after anemization, the mucous membrane becomes pale pink, making it more convenient to examine.
There will be no complications of anemization if it is properly organized. But on the first day after the procedure, slight burning, dryness and irritation may occur. These symptoms will soon go away spontaneously.
Treatment for dry nose
There are no specific medications to treat dry nose. But it is necessary to treat dry nose. This is not only an unpleasant sensation, but in the cold season in winter it is also protection against viruses and bacteria that easily penetrate through the nasal mucosa further into the respiratory tract.
Before starting treatment, it is important to know what is causing the problem. If you know the reason, you can use simple home remedies.
Steam inhalations
Steam inhalations are often used for sore throats and nasal congestion. They also help with dry nose. The steam moisturizes the nasal mucosa well, penetrating the pores and opening them, and thus helping to increase the secretion of mucus in the nose.
Boil 3 cups of water and pour them into a wide bowl.
Lean over the bowl, covering your head with a towel, and breathe for at least 7-10 minutes.
You can add a few drops of mint essential oil to the water.
With regular use of steam inhalations, you can get rid of dry nose.
Petrolatum
Due to its moisturizing properties, Vaseline is one of the effective home remedies for dry nasal mucosa and the formation of dry crusts, including those with blood. Use only medical Vaseline.
Glycerol
Glycerin is also a good skin hydrator and can prevent and relieve dry nose. You just need to lubricate the nasal mucosa with pharmaceutical glycerin.
Vegetable and cosmetic oils
If the nose is dry, stuffy, and the formation of dry crusts, the mucous membrane can be lubricated with vegetable or cosmetic oils to moisturize it. Some of the best oils for treating dry nasal mucosa are mustard oil, almond oil and coconut oil.
Mustard oil. Mustard oil is a fatty oil. To get rid of a dry nose, simply place two or three drops of oil into each nostril and inhale slowly so that the oil moves further into the nasal passages.
In winter, lubricate your nose with mustard oil every time before going outside. This will help avoid dry nose in severe frosts.
Almond oil. Almond oil is a source of many beneficial substances: essential fatty acids, vitamin E and other vitamins, which are very useful for relieving dry nasal mucosa.
Types of diseases
There are many reasons for the development of nasal diseases. These can be not only inflammatory processes, but also traumatic conditions, neoplasms and even the specific structure of an organ. Conditionally, diseases can be divided into three groups:
- Traumatic. Such damage can be caused by domestic injuries, sports injuries, industrial injuries, or those sustained during combat operations. Injuries are divided into closed, open, and combined. Some of them can lead to deformation of the outer part of the nose. There are also situations when bone fragments are displaced or trauma to the nose leads to the formation of a septal hematoma. In such cases, treatment of nasal diseases is carried out through surgery.
- Congenital. Such pathologies include deviated septum. This phenomenon occurs in many people, and not in all cases it leads to serious problems. However, with severe deformation, the functions of the nose may be impaired. Congenital pathologies include not only a deviated septum, this category also includes fistulas, narrowed nasal passages and other anomalies. To correct such problems, a surgical method is used.
- Infectious. This category includes nasal diseases of a bacterial, fungal or viral nature. Infectious diseases are the most common. These include varieties of rhinitis, sinusitis, polyposis and other ailments.
Since infectious diseases of the sinuses are the most common, we will dwell on them in more detail.
Recovery with medications and physiotherapy
Modern medications will help restore the nasal mucosa; the following drugs are often prescribed to combat the disease:
| A drug | Photo | Price |
| Solcoseryl | From 328 rub. | |
| Panthenol | From 78 rub. | |
| Petrolatum | From 23 rub. |
It is very easy to treat the nasal mucosa with these remedies. The patient will need to soak a cotton pad with any of these medications and carefully place it in the halves of the nose, but everything is done one at a time.
The therapeutic effect time is 15 minutes; leaving the medicine for a longer time is not recommended. The procedures are performed once daily, but if necessary, the treatment must be carried out twice.
Sea buckthorn and peach oil will help soften the mucous membranes of the nasopharynx and prevent the formation of crusts.
These extracts are rich in vitamins and various microelements; they will be simply irreplaceable for injured tissues. Treatment with oils is carried out in a similar way.
Aqua Maris and Aqualor sprays have a good effect. To achieve the expected effect and moisturize the mucous membranes, you will have to use such drugs several times a day.
If the disease is in an advanced state and the nasal mucosa is quite severely affected, ointments and sprays may not help. In such cases, most specialists prescribe physiotherapeutic procedures aimed at.
It will be easy to restore the nasal mucosa for patients after a runny nose not only in a hospital setting, but also at home. It is best to warm up the nose using compresses with heated salt or sand, as well as using UV lamps.
If the patient decides to be treated in a hospital, doctors prescribe electrophoresis, special inhalations with alkaline oil solutions, as well as the use of a helium-neon laser. Regardless of which procedure is prescribed, the course of treatment is at least 10 procedures.
Swelling of the mucous membrane causes
And the most common problem with the nasal mucosa is swelling. Swelling of the nasal mucosa and paranasal sinuses underlies many diseases of the nasopharynx. How does it develop?
Infectious processes
The fundamental mechanism in the development of swelling of the nasal mucosa is considered to be infection. The ciliated epithelium is an ideal environment for the activity of pathogenic microorganisms. Viruses, bacteria and fungi penetrate with the current of inhaled air. With a normally functioning immune system and a fully functioning ciliated apparatus, all microbes are retained in the cilia and are washed out with the help of nasal secretions. Every second, thousands of different microorganisms settle in the eyelashes, and in the vast majority of cases they do not harm us.
However, when the body's defenses decrease (for example, as a result of hypothermia), microbes begin to develop in the nasal mucosa. The same outcome is possible if the viruses and bacteria that enter the nasal cavity are particularly aggressive. By the way, respiratory viruses that provoke ARVI are precisely such pathogens.
Interestingly, when the feet are hypothermic, a quick and violent reaction of the nasal mucosa is often common. This is caused by the existence of so-called reflexogenic connections between the nasal mucosa and the feet.
The inflammatory process that begins in the nasopharynx primarily leads to vasodilation, as a result, the occurrence of edema.
Allergic reaction
Swelling of the mucous membrane due to the release of histamine is the result of an allergic reaction. Many substances can act as allergens: from plant pollen to mites living in an old mattress. Despite a very special mechanism of development, allergy symptoms are very similar to the symptoms of a cold. One of the characteristic signs of allergic swelling of the nasal mucosa is itching, but it often appears with viral rhinitis. That is why doctors, and even more so the patients themselves, are not always able to quickly and accurately identify the cause of a runny nose and distinguish a common ARVI from an allergy to ragweed pollen.
Treatment for swelling of the mucous membrane due to allergies is a little more complicated than for a cold. As a rule, the treatment regimen includes:
- alpha-adrenergic agonists, which constrict blood vessels and restore breathing;
- antihistamines or antiallergic drugs;
- intranasal corticosteroids (Nasonex, and others).
In addition, swelling of the nasal mucosa can be caused by injuries and other reasons.
General structure
When we talk about departments, we mean the three components of the nasal system. They differ in their structure. Moreover, for each person, some elements may differ in general, but at the same time play their role in the process of breathing and smell, as well as protection. Therefore, to simplify, the following parts are distinguished:
- Outdoor;
- Nasal cavity;
- Sinuses.
They all have common features among all people, but at the same time they also have differences. This depends on the individual anatomical characteristics, as well as on the age of the person.
Structure of the external part
The outer part is formed by the bones of the skull, cartilaginous plates, muscle and skin tissue. The shape of the external nose resembles a triangular irregular pyramid, in which:
- The apex is the bridge of the nose between the eyebrows;
- The dorsum is the surface of the olfactory organ, consisting of two lateral bones;
- Cartilaginous tissue continues the bone, forming the tip and wings of the nose;
- The tip of the nose meets the columella, a septum that forms and separates the nostrils;
- All this is covered from the inside with mucous membranes and hairs, and on the outside – with skin.
The wings of the nose are supported by muscle tissue. A person does not actively use them, and therefore they are attributed more to the facial department, which helps to reflect the emotional state of a person.
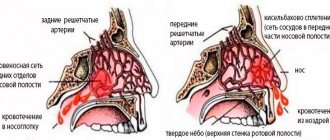
The skin in the nose area is quite thin and equipped with a large number of blood vessels and nerve endings. The columella is usually not perfectly straight and has a slight curvature. At the same time, in the area of the septum there is also a Kisselbach zone, where there is a large accumulation of blood vessels and nerve endings, almost at the very surface of the integument.
This is why nosebleeds occur most often here. Also, this area, even with minimal trauma to the nose, gives severe pain.
If we talk about the differences in this part of the olfactory organ in different people, then in adults it can differ in shape (which is influenced by past injuries, pathologies, as well as heredity), and in adults and children – in structure.
The nose is formed until about 15 years of age, although according to statistical data from researchers, the nose “matures” and grows with a person throughout life.
Newborns have a different nose from an adult. The outer part is quite small, although it consists of the same sections. But at the same time, it is just beginning to develop, and therefore children of this period often immediately pick up all sorts of inflammations and pathogens.
The olfactory organ in children cannot perform the same functions as in adults in full. The ability to warm air develops at about 5 years of age. Therefore, even in frosts of -5 - -10 degrees, the tip of a child’s nose quickly freezes.
The picture shows a diagram of the structure of the human nasal cavity
Anatomy of the nasal cavity
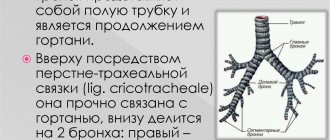
The physiology and anatomy of the nose primarily implies the internal structure in which vital processes occur. The organ cavity has its own boundaries, which are formed by the bones of the skull, oral cavity, and eye sockets. Consists of the following parts:
- The nostrils, which are the entrance gates;
- Hoan - two holes in the back of the internal cavity that lead to the upper half of the pharynx;
- The septum consists of cranial bones with a cartilaginous plate, which forms the nasal passages;
- The nasal passages, in turn, consist of walls: superior, medial internal, lateral external, and also formed by the maxillary bones.
If we talk about the departments of this area, they can be conditionally divided into lower, middle, upper with the corresponding respiratory passages. The upper passages exit to the frontal sinuses, the lower one carries the lacrimal secretion into the cavity. The middle one leads to the maxillary sinuses. The nose itself consists of:
- The vestibules are zones of epithelial cells within the wings of the nose with a large number of hairs;
- The respiratory zone is responsible for producing mucus to humidify and cleanse the air of pollutants;
- The olfactory area helps to distinguish odors due to the presence of corresponding receptors and olfactory cilia in the tissues.
In children, the internal structure is generally similar to that of an adult, but at the same time it is located quite densely due to the underdevelopment of the department. That is why this department gives frequent complications in the form.
The passages of the nose are narrow, and the structure of the mucous membrane is distinguished by a large number of blood vessels, which provokes almost immediate swelling under the influence of hypothermia, a pathogen or an allergen.
Simple and accessible information about the structure of the nasal cavity in our video:
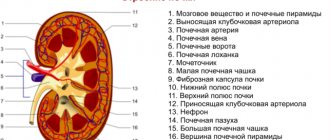
The structure of the paranasal sinuses
The sinuses are an additional device for air ventilation, which are also lined with mucous surfaces and are a natural extension of the nasal passage system. The department consists of:
- The maxillary sinuses are the largest section of this type with a wide opening that is covered by the mucous membrane, leaving only a small gap. It is precisely because of the peculiarities of this structure that all sorts of infectious lesions of this section often develop with difficult removal of “waste products”. They are located on the sides of the nose in the area of the cheeks under the eyes.
- The frontal sinus is located in the area above the eyebrows just above the bridge of the nose.
- The third largest section is the cells of the ethmoid bone.
- The sphenoid sinus is the smallest.
Each department can be affected by a specific disease, which is named accordingly. In general, pathologies of this part of the nose are called sinusitis.
The paranasal sinuses are extremely important in the structure of the nose, as they ultimately warm and moisturize the air flow coming from the outside, and also organize the sense of smell. Free cavities reduce the weight of the skull, reducing the load on the spine. In case of injury, they help soften the force of the blow, and also participate in the formation of the timbre of the voice.
At birth, a child has formed cells of the ethmoid labyrinth and the rudiments of the maxillary sinuses. Gradually, the structure of the labyrinth changes, increasing in volume. The maxillary cavities are finally formed only by the age of 12. The frontal and sphenoid sinuses begin to develop only from 3-5 years.
Visual video with diagrams of the structure and location of the paranasal sinuses: