Perforated otitis in humans occurs as a complication of the acute purulent form of this disease. In this case, patients experience a violation of the integrity of the eardrums, which separate the middle and outer ears. As a result, people experience deafness along with hearing loss and impaired perception of sounds. This disease is dangerous. Against this background, a secondary infection may occur, which occurs due to perforation of the membrane.
Membrane rupture most often occurs in the lower quadrant. This is a triangular slit, its edges are uneven, and pus can come out of it. If this happens, the doctor will take a small amount of liquid for bacteriological analysis in order to determine the causative agent of the disease and select antibacterial therapy. The larger the perforation, the more impaired the hearing. A sharp pain in the ear may indicate a ruptured eardrum.
Otitis can be characterized as follows:
- Sudden onset of illness, body temperature rises to 39 degrees.
- Pain in the ear, radiating to the temple and teeth on the affected side.
- Hearing loss and tinnitus.
- General weakness and malaise.
The main reasons for the development of pathology
Factors that provoke perforated otitis media may be the following:
- Chronic inflammation in which discharge accumulates in the ear cavity, which affects the eardrum, causing its rapid thinning.
- Foreign objects that have a traumatic effect.
- Infectious migration from nearby organs: from the oropharynx, maxillary sinuses, nasal passages, and so on.
- Improper execution of medical procedures.
- Presence of traumatic injuries to the skull.
- The introduction of infection through the bloodstream during influenza, scarlet fever, and more.
Now we will find out how in modern clinics a diagnosis is made within the framework of such a disease.
Diagnosis of the disease
Diagnosis of perforated otitis is carried out using otoscopy, which is performed by a specialist. It is a painless, simple procedure in which a plastic or metal funnel is inserted into the external auditory canal, and the auricle is pulled upward to align the ear canal and the eardrum is visually inspected.
Its rupture most often occurs in the lower quadrant. If present, the doctor takes a small amount of liquid for bacteriological analysis to determine the origin of the causative agent of the disease and select antibacterial treatment. The larger the size of the perforation, the more significantly the patient’s hearing is impaired.
Now let’s find out what signs indicate the appearance of this disease in the body.
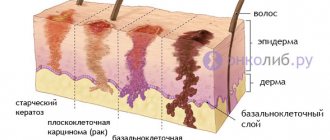
Features of the anatomy of the auditory organ
The human auditory organ consists of three sections: external, middle and internal. Each of them is capable of undergoing an inflammatory process, but most often the outer ear suffers due to openness and vulnerability to bacterial agents.
The structure of this department, at first glance, is quite simple. All elements of the outer ear, due to their special shape, are designed to absorb sound waves from the outside, amplify them as much as possible and transmit them to the eardrum, from where the vibrations enter the middle section.
- The auricle is cartilage covered with skin and soft tissue. Its shape serves to capture sounds from different directions, as well as amplify them. At the bottom of a kind of “amphitheater” formed by the auricle there is a hole leading into the ear canal.
- The auditory canal serves to pass sound to the eardrum, where it actually ends. On average, its length in an adult is about 2.5 cm, and its diameter is up to 1 cm. The skin lining the surface of the ear canal is penetrated by sebaceous and sulfur glands, the task of which is to moisturize the “tunnel”, attract dust and prevent bacteria penetrate to the middle ear.
- The eardrum is the boundary between the middle and outer ear. The membrane not only transmits sound vibrations to the auditory ossicles, but also serves as a kind of mechanical barrier for bacteria that have penetrated the organ.
Purulent otitis media and its symptoms
Purulent perforated otitis is characterized by:
- Sharp and very severe pain.
- Weakening or loss of hearing on the affected side.
- The discharge of pus with an unpleasant odor mixed with blood from the area of the sore ear.
- Ringing, noise and discomfort.
- Dizziness and nausea.
- Pain subsides as a result of fluid draining from the ear.
The release of air from the organ indicates a complete rupture of the membrane. After its perforation, with successful drainage of fluid from the middle ear, hearing sensitivity is gradually restored. A small size of acute purulent perforated otitis media can heal on its own. In other cases, it is necessary to be treated by observing the degenerative changes in the affected membrane.
Labyrinthitis
The sequence of development of the disease allows us to distinguish 2 of its forms:
- Serous
- Purulent
Infection of the labyrinthine region in most cases occurs through the middle ear and is the result of the purulent stage of otitis media. Increased pus formation increases pressure in the tympanic cavity, stretching the membrane of the oval window. Over time, it becomes permeable to toxins accumulated in the middle ear - waste products of pathogenic flora. The so-called serous inflammation develops, which, on the part of the window membrane, increases the pressure in the labyrinthine area. Deformations of the thinnest membrane ultimately end in its rupture, which allows pathogenic microorganisms to penetrate directly into the cavity of the labyrinth. This is how the serous stage turns into a purulent stage.
Acute otitis media
This is a fairly rapid infection of the ear cavity. The clinical picture of the disease includes the presence of severe pain along with sensations of congestion and noise, decreased hearing, and the appearance of a hole in the membrane with further suppuration.
As part of the diagnosis of acute perforated otitis, otoscopy and blood test data are used. It is possible to perform an X-ray of the skull and examine the auditory tube.
General treatment of the disease is carried out with antibiotics, anti-inflammatory and antihistamines. As for local therapy, it consists of blowing out the auditory tube, and, in addition, instilling drops, introducing proteolytic enzymes, etc.
In children
Children under three years of age often suffer from acute perforated otitis media; their anatomical features contribute to this. In children, the auditory tube is much shorter and located more horizontally compared to adult patients. Their tympanic cavity is filled with a peculiar connective tissue, which predisposes to the development of inflammation in this area.
In children, the body's resistance to infections is less, and they also have a weaker immune system. Diseases such as adenoids, acute tonsillitis and adenoiditis only contribute to frequent relapses and the occurrence of otitis media.
It is extremely important to pay attention to the symptoms of the disease in time. If the baby is not yet two years old, then he will indicate pain by worrying, refusing food and crying. As part of the pressure on the ear tragus, the baby's crying will intensify, which will only confirm the diagnosis.
If this disease is confirmed in a baby, under no circumstances should water get into the ear canal. This can cause various complications, which can lead to complete hearing loss. Now let's look at the methods of therapy.
Causes
The main cause of the disease is infection: viral (adenoviral, influenza virus) or bacterial (hemophilus influenzae, Staphylococcus aureus, streptococcus, pneumococcus). Recently, fungal otitis caused by a fungal infection has become increasingly common.
Risk factors:
- Frequent rhinitis or sinusitis.
- Allergic rhinitis.
- Immunodeficiency conditions in children. Congenital or acquired deficiency of immune cells. This condition leads to a decrease in the body's protective properties and greater susceptibility to infection.
- Formula-fed children. Such children do not receive immune cells from their mother's milk, so their immunity is much lower than that of breast-fed babies.
Treatment
Treatment of an illness such as perforated otitis media should be carried out in a hospital by an otolaryngologist and may include:
- The use of a special patch for the membrane, which helps restore its integrity.
- Treatment with ear drops with a local anesthetic and antibacterial effect (we are talking about Anauran, Otofe).
- Therapy with angistamines (Tavegil, Cetrin, Loratadine).
- The use of vasoconstrictor drops that facilitate nasal breathing and promote better fluid outflow from the ear (for example, Otrivin or Naphthyzin).
- Carrying out systemic antibacterial therapy (prescribed after examination by a doctor).
- Applying a warming semi-alcohol compress to the ear.
- Surgery may be appropriate if the perforation is large or if there is no effect from previously described treatment methods.
Surgical treatment of perforated otitis involves the application of bone patches to the site of perforation. A flap of skin is taken from the area above the ear, then it is sewn with absorbable thin material around the perimeter of the ruptured membrane. Subsequently, the transplanted area will reliably take root, and hearing, in turn, will be restored.
If you have symptoms characteristic of acute or perforated otitis, you should immediately contact an otolaryngologist.
Prevention
Such measures play an important role, especially in children, since this disease, unfortunately, is prone to recurrence. So, you need:
- Correctly and promptly treat any infection along with diseases of the throat, ears and nose.
- Do not use sharp objects to clean the external auditory canals.
- Avoid exposure to excessive noise.
- Support of the body's immune system is required.
- It is important to teach your baby how to sneeze and blow his nose correctly.
- It is necessary to protect the external auditory canal from noise, for example, wearing ear protection on an airplane, sucking a lollipop during takeoff, and so on.
The inflammatory process of the middle ear will require a correct approach, and at the same time, immediate treatment. This condition does not pose a threat to the patient’s life, but it is important to follow all preventive measures in order to avoid relapses and complications of the disease.
Appointment with an ENT doctor on Saturday and Sunday for initial treatment at Bioss MC - 1,100 rubles.
Acute otitis media is an inflammation of the middle ear.
ANATOMY: The middle ear consists of the tympanic cavity and the auditory tube. Through the auditory tube, the tympanic cavity communicates with the nasopharynx. The tympanic cavity is located at the base of the temporal bone pyramid between the external auditory canal and the labyrinth (inner ear). It is lined with mucous membrane and contains a chain of auditory ossicles (hammer, incus, stapes), which transmit sound vibrations from the eardrum to the labyrinth.
Causes:
The main causative agents of AOM are pneumococcus - Streptococcus pneumoniae and Haemophilus influenzae - Haemophilus influenzae, which make up 60% of the bacterial flora. Less common is Moraxella catararhalis -3-10%, even less common is Staphylococcus aureus 1-5%. Mycoplasma pneumoniae, which can cause bullous hemorrhagic myringitis, Chlamydia trachomatis, Chlamydia pneumoniae, can play a certain role in the etiology of AOM. It is believed that up to 10% of AOM can be caused by viruses, namely: influenza and parainfluenza viruses, adeno-, rhino-, corona-, enteroviruses, respiratory syncytial viruses.
Ways of infection entering the tympanic cavity:
- Tubar (through the auditory tube from the nasopharynx)
- Hematogenous (with blood flow; rare)
- Traumatic (if the eardrum is damaged)
Factors provoking the development of the disease are:
- Hypothermia;
- Dysfunction of the auditory tube (hypertrophy of the nasopharyngeal and tubular tonsils, changes in the mucous membrane of the nasal cavity, nasopharynx in allergic and chronic rhinitis, curvature of the nasal septum, hypertrophy of the posterior sections of the nasal turbinates);
- Congenital and acquired immunodeficiency conditions;
- Concomitant severe diseases such as diabetes mellitus, bronchial asthma, rheumatic diseases, chronic renal failure;
Stages of acute otitis media
- 1. Stage of acute eustacheitis (tubo-otitis) – characterized by ear congestion, tinnitus, autophony.
- 2. Stage of catarrhal inflammation (acute catarrhal otitis media) – characterized by pain in the ear.
- 3. Stage of acute purulent inflammation (acute purulent otitis media) - characterized by the presence of mucopurulent exudate in the tympanic cavity, deterioration of general health, increased T-body, increased ear pain, ear congestion, decreased hearing in the affected ear. During acute purulent otitis, 2 periods are distinguished: - pre-perforation (the integrity of the eardrum is preserved) - post-perforation (the appearance of perforation of the eardrum,
- 4. Reparative stage (healing stage, perforation of the eardrum is closed by a scar)
Clinical manifestations and symptoms of acute otitis media:
| Complications if acute otitis media is not treated:
|
Examination program:
Additional diagnostics:
Prevention:
| Treatment: depending on the stage of acute otitis media, the following are used:
|