When should you have your tonsils removed? Types of tonsillectomy. Features of the postoperative period.
Tonsillectomy is an operation that has been performed frequently and for a very long time. The first mentions of excision of the tonsils are mentioned in ancient Greek and Roman sources, which are already nearly 3,000 years old.
Today, every 8 inhabitants of planet Earth have had their tonsils removed, and two thirds of these people underwent the operation in childhood. Why is this type of surgical intervention “put on stream”? How necessary is it? What are the indications for tonsillectomy, what happens after it? It's worth trying to find answers to these questions.
Laser and radio wave tonsillectomy: indications
Tonsillectomy is a medical term of Latin and Greek origin. Tonsilla (Latin) means “tonsil”, and ἐκτομή (Greek) means “removal”. This is an operation during which the surgeon, using one of the practiced methods, removes the patient’s tonsils (palatine tonsils) along with the connective capsule.
Tonsillectomy.
Modern medicine knows several methods for removing tonsils:
- scalpel, scissors and wire loop
- electrocoagulation
- cryodestruction
- CO2 laser
- ultrasound
- radiofrequency ablation
Chronic tonsillitis is a rather severe, unpleasant disease, and sometimes difficult to cope with. And there is no other choice but to remove the organ, which is a constant source of infection.
IMPORTANT: Previously, tonsillectomy was done en masse. And not only for patients with chronic inflammation of the tonsils, but also for prevention. The operation was considered easy and little traumatic, and the tonsils were considered a rudimentary organ. Today, their role in the formation of human immunity has become obvious, so surgery is performed only in extreme cases, if there are clear indications.
These include:
- Chronic tonsillitis with frequent relapses (frequent tonsillitis). This is considered tonsillitis, which worsens more often than 4 times a year, for 2-3 years.
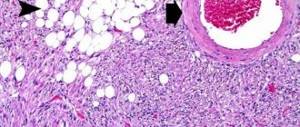
- Chronic tonsillitis, which has turned into a decompensated form. With this, the tonsils not only become inflamed, but a number of irreversible destructive changes occur in them. The infection from them spreads to nearby organs. The source of infection is growing.
- Complications of the disease appear in the form of allergization of the body, cardiovascular pathologies, diseases of the kidneys, joints, and endocrine glands.
- The tonsils grow to such an extent that they interfere with breathing (apnea, sleep apnea) or swallowing.
- A peritonsillar abscess, phlegmon, and other purulent complications occurred.
- Measures of conservative treatment of chronic tonsillitis were taken, but they did not produce results.
Indications for tonsillectomy.
IMPORTANT: It is advisable to perform a tonsillectomy during a period of remission, when the tonsils are relatively calm. In the presence of purulent complications or in other cases of surgery during an exacerbation, the patient is prescribed high doses of antibacterial drugs.
But there are people for whom tonsillectomy performed by any method is strictly contraindicated. These are patients with chronic tonsillitis with:
- leukemia, other serious blood diseases
- abnormalities of the vessels of the pharynx
- pulmonary tuberculosis in open form
- diseases of the heart, kidneys, liver, lungs, in which irreversible changes have occurred in these organs (stage of decompensation)
- severe forms of neuropsychic pathologies
- severe form of diabetes mellitus
Tonsillectomy is not performed temporarily, but is postponed to a more favorable time for:
- ARVI and influenza
- exacerbation of chronic diseases identified in the patient
- ketonuria in diabetics
- dental caries
- menses
IMPORTANT: Before the operation, a patient with chronic tonsillitis visits an ENT specialist, a therapist, and medical specialists as necessary, and also undergoes a clinical and blood biochemistry test, a coagulogram, and a urine clinic.
Laser tonsillectomy
Instead of a scalpel or scissors in ENT practice, I use lasers (diode or carbon dioxide) as a surgical instrument.
Laser tonsil removal.
Removing tonsils with a laser is considered a gentle method, since the laser beam simultaneously:
- destroys pathological tissues
- coagulates (“cauterizes” small blood vessels, thereby reducing the risk of wound infection or severe bleeding)
To perform a laser tonsillectomy, there is no need to hospitalize the patient. The operation is performed on an outpatient basis. The patient is given local anesthesia. Recovery after intervention is usually quick.
Radio wave tonsillectomy
Another modern method of removing tonsils is radio wave. Human palatine tonsils are 70-90% water. The scalpel electrode gives them a radio signal, which evaporates this water. In this way, pathological tissues are dissected. Wherein:
- nearby tissues and organs are not damaged
- thermal effect on tissue is minimal
- blood vessels and nerve endings are coagulated, making the method practically bloodless, pain after the intervention is minimal
- no scar is formed after radio wave tonsillectomy
The operation can be performed using the radio wave method both under general anesthesia and with local anesthesia.
Indications for tonsillectomy
Tonsils are formations of lymphoid tissue located on the mucous membrane of the mouth in the nasopharynx area. If desired, you can view them in the mirror. The organ has an almond shape, which is how it got its name.
The tonsils have a porous structure; they are penetrated by lacunae in which protective lymphocytes mature. The function of the organ is to create local immunity that prevents dangerous bacteria from entering the body. Microbes settle on the surface of the tonsils, accumulate and cause inflammatory processes. This disease is called tonsillitis. It occurs in acute or chronic form. Tonsillitis most often affects children whose immune system is not fully developed.
Symptoms of inflammation of the tonsils are:
- pain and sore throat;
- enlarged lymph nodes;
- temperature increase;
- weakness, fatigue, loss of appetite;
- the tonsils increase in size and become covered with foci of purulent plaque.
With frequent inflammation, tonsillitis becomes chronic. It is an active source of infection. With purulent discharge, toxins regularly enter the bloodstream and poison the body.
Bacteria cause diseases of internal organs - heart, kidneys, joints and nearby - ears, nose, eyes. Rhinitis, otitis and conjunctivitis are constant companions of chronic pathology of the tonsils. The affected tissue changes the shape of the tonsils, they increase in size. This disrupts normal breathing, swallowing, and changes the voice.
After examination and tests, the otolaryngologist prescribes conservative treatment. If it does not give a positive result and the disease returns, a tonsillectomy is prescribed under general anesthesia or local anesthesia.
Indications for surgery:
- relapses of tonsillitis more than 5 times during the year;
- signs of a decompensated stage of the disease - there are complications in the heart, joints, kidneys;
- severe sore throat and an allergic reaction to the main groups of antibiotics used to fight the disease;
- proliferation of lymphoid tissue causes sleep apnea syndrome - breath holding;
- constant intoxication of the body, leading to decreased immunity;
- spread of inflammation to other tissues;
- ineffectiveness of conservative treatment.
To perform a tonsillectomy, a period is selected when there are no signs of obvious exacerbation.
Bilateral tonsillectomy: progress of the operation
Despite the existence of modern, less traumatic methods, removal of tonsils with a scalpel or scissors is still practiced.
- Before the operation, the patient's blood is examined. Since tonsillectomy with a scalpel is far from a bloodless method, it is necessary to make sure that the person being operated on does not have problems with blood clotting. A coagulogram is performed.
- Next, the method of pain relief is determined. For adults and children over 12 years of age, a double scalpel tonsillectomy is usually performed under local anesthesia. For children, general anesthesia is chosen, firstly, because the pain during the operation is a great stress for them, and secondly, they will not be able to sit still. Before using a particular type of anesthesia, check whether the patient is allergic to it.
- During the operation, the patient sits or lies. Manipulations begin as the anesthesia takes effect. For local treatment – after 5-10 minutes.
- The palatine tonsils are pulled back with clamps and cut off with a scalpel, scissors and a special loop. After cutting off the tonsils, apply cotton balls to the bleeding vessels and press them tightly. This is usually enough to stop the bleeding. Those vessels from which bleeding is profuse are tied with silk thread.
- When the bleeding has stopped, the operation is considered complete.
Removal of the glans with a scalpel.
IMPORTANT: The duration of a tonsillectomy with a scalpel is 30 minutes - 1 hour.
Contraindications
Resection of the tonsils is not performed in all patients. There are a number of restrictions and contraindications. The surgeon makes a negative decision on tonsil removal if the patient has:
- problems with blood clotting;
- heart and kidney diseases;
- diabetes;
- acute infectious diseases;
- severe hypertension;
- tuberculosis in the active phase;
- pregnancy after 6 months.
Gynecologists and cardiologists are against tonsil removal. They believe that the operation leads to severe weakening of the body.
Tonsillectomy and postoperative period
The duration and complexity of postoperative recovery directly depends on the method of tonsil removal, as well as the type of anesthesia used during the operation.
- Immediately after the operation, the patient is taken to the ward. On the bed he is laid on his side, with a towel placed under his cheek. The fact is that in the first hours after the operation he will have profuse salivation. It is important that he does not choke.
- You cannot talk on the first day after surgery. Adults and adolescents are allowed to drink 3-4 hours after surgery; they cannot eat on this day. After 5-6 hours, children can be fed liquid food (ground porridge, for example), the temperature of which is equal to room temperature.
- On days 2-3, the postoperative patient may experience pain in the area of the tonsils and throat.
- On day 2-3, patients whose tonsils were removed with laser, liquid nitrogen and radio waves are discharged, unless complications arise (such cases are rare).
- Postoperative patients whose tonsils were removed with a scalpel are discharged on days 5-6.
After tonsillectomy, the patient lies on his side.
IMPORTANT: Complete recovery after tonsillectomy is equated to epithelization of the almond niches. It occurs 17–21 days after surgery. Then the postoperative period ends.
Tonsil removal methods
There are two methods of operation in total. They are selected depending on the degree of tissue damage:
- Tonsillotomy - partial removal of tissue. With this method of surgical intervention, healthy areas of the tonsils are not affected; they retain their functionality, protecting them from viruses and bacteria.
- Tonsillectomy - complete removal of tissue. The tonsils are cut out completely to prevent the risk of infection of neighboring organs.
Modern medicine includes several methods of performing surgery in adults and children:
- Traditional using a sharp loop of surgical wire. With this method, tonsils and nearby tissues are removed. The traditional method of resection is practically no longer used, because it has a large number of contraindications and side effects, one of which is severe bleeding.
- Cryodestruction using liquid nitrogen. It is applied to the affected areas, under the influence of which the infected tonsils die and fall off. To completely remove tonsils, several such procedures are necessary. The advantages of this method are that it does not require much time for rehabilitation, and the operation itself is painless.
- Laser removal. A special device is used to cauterize the affected tissue, thereby eliminating infected areas and preventing the risk of bleeding. Laser removal has minimal trauma and easy postoperative recovery.
- Electrocoagulation. To remove the tonsils, an electric current is directed to the affected areas of tissue. To achieve the desired result, several such procedures are carried out. There is a danger: incorrectly selected power can cause burns to the mucous membrane.
- Ultrasonic removal. This method is characterized by reduced risk of injury and absence of bleeding.
- Radio wave method. The essence of the method is to evaporate the water contained in the tonsils. To do this, a scalpel electrode is inserted into them, with the help of which a radio wave signal is supplied. Under its influence, pathological tissues are dissected.
After surgery, patients are advised to rinse their mouths and rinse their tonsils at home and in the hospital. This is necessary to prevent wound infection.
How long does the temperature last after tonsillectomy?
On the second day after tonsillectomy, the patient's temperature may rise to low-grade fever. Usually it is 37 - 37.5 degrees. This increase is associated with the healing of the postoperative wound.
- Low-grade fever, normally, lasts 7-10 days. But there are cases when the temperature does not normalize until complete epithelialization.
- If the temperature does not drop 3 weeks after surgery or longer, this is a reason to consult a doctor and get a blood test. There may have been some complications.
After a tonsillectomy, the temperature can last up to 21 days.
How long does your throat hurt after a tonsillectomy?
Sore throat after tonsil removal occurs immediately or the next day. It can get into your ears. The most intense pain sensations occur until the 6th day after surgery. By the second week, the tonsil niches are completely cleared of plaque, and by the end of the third week they are completely covered with new epithelium. By this time, the pain usually goes away.
Sore throat is a feature of the postoperative period after tonsillectomy.
Bleeding after tonsillectomy
Bleeding most often occurs in patients after removal of the tonsils with a scalpel. It occurs in 1-8% of adults and 3-6% of children, and is usually associated with:
- errors in the operation
- structural features of blood vessels
- poor blood clotting
Typically, this type of complication occurs immediately after tonsillectomy. It is dangerous for two main reasons, which are:
- blood loss
- risk of choking on blood (especially in children)
Doctors decide what measures to take to stop the bleeding and restore the patient’s blood, based on the severity of his condition.
IMPORTANT: A week after the operation, the patient may release small amounts of blood from the healing niches of the palatine tonsils. Most likely, this bleeding is associated with mechanical damage to the mucous membrane during food intake.
Complications after tonsillectomy
Other complications after tonsil removal include:
- inflammation due to infection
- scars on the palate and palatine arches
- hyperplasia of the nasopharyngeal and lingual tonsils
- acetonemia in children
- pharyngitis and sore throat
These complications are extremely rare, provided that tonsillectomy was performed according to indications and with adequate preoperative preparation.
Tonsillectomy: before and after.
How is recovery after tonsil removal?
Tonsillectomy is an operation that has been used for about 3,000 years. It is indicated for: chronic tonsillitis, adenoiditis, airway obstruction.
Before surgery, the patient is prepared (biological material is taken for testing and examined). There are 2 methods of pain relief: local anesthesia and general anesthesia. This is followed by recovery after removal of the tonsils.
During this period, you must follow all the rules. The timing of final recovery depends on this.
What can you eat after tonsil removal?
For the first 6-7 hours there is no need to eat. Then you can eat the food in liquid form (broth, jelly, cream). From the second day, diets (“zero” or “surgical”) are prescribed. They have a gentle diet.
It is necessary to select easily digestible foods. Allowed: broth, porridge (mashed through a sieve), fish puree, jelly, cream and jelly. From the third day you can introduce: puree soup, pureed cottage cheese, baked apples, porridge with milk.
During rehabilitation after tonsil removal, you must adhere to some general rules regarding nutrition:
- Food and drink should be cold.
- Eat more protein foods.
- Avoid salt and spices when cooking.
- Take meals in small portions throughout the day.
- Drink plenty of water and not hot.
- Avoid citrus fruits.
- Peel fruits and vegetables.
- Eliminate alcohol and sweets.
Nutritional rules should be followed until recovery.
Therapeutic procedures after surgery
3-4 days after surgery to remove adenoids and tonsils, the patient is discharged home. However, the treatment does not stop there.
There are regulations and detailed instructions that must be strictly followed:
- Follow a diet.
- Reduce the load on the ligaments (do not talk loudly).
- Reduce physical activity.
- Take medications prescribed by your doctor.
- Gargle more often.
These procedures will help speed up your recovery.
Consequences of tonsillectomy. Is it possible to have a sore throat after a tonsillectomy?
A positive consequence of removing the tonsils is getting rid of chronic tonsillitis and frequent sore throats. It turns out that if you remove the tonsils, there will be no sore throats? In general terms, yes. But immediately after surgery, a complication is possible, which doctors call “postoperative sore throat.” It manifests itself as pharyngitis (inflammation of the throat mucosa), inflammation of the palate, and lymphadenitis.
Many experts see the lack of a barrier between the environment and the human respiratory system, the role of which was played by the tonsils, as a negative consequence of tonsillectomy. According to statistics, bronchitis as a complication of ARVI is more common in people after tonsillectomy.
Recovery after tonsillectomy – rehabilitation. Nutrition after tonsillectomy: diet
In the first hours after surgery, while blood is bleeding from the wounds, the patient is recommended to lie on his side. When the bleeding stops, you can turn over and stand up. If there are no complications, you can return to normal life immediately after discharge from the hospital.
Sometimes therapy is needed after surgery:
- antibiotics (if an infectious complication occurs)
- antipyretics (if the temperature rises above 38-38.5 degrees)
- painkillers (especially in children if the sore throat is very intense)
A diet is recommended for all days of the postoperative period.
- It is not recommended to eat at all on the first day.
- In the first 6 days, food should be liquid, homogeneous, and at room temperature.
- For 21 days you should not eat anything that is too hot, too cold, spicy, sour, or anything that can irritate the mucous membranes of the mouth and throat.
- You need to drink the daily norm: 1.5 liters for children, 2-3 liters for adults.
In the first week after removal of the tonsils, it is recommended to eat liquid homogeneous food.
Tonsillectomy - risks of tonsil removal and recovery time
A tonsillectomy is an operation during which the tonsils are removed. It is usually performed in children or adults who have frequent episodes of tonsillitis. The intervention is performed under general anesthesia, which requires hospitalization for a day.
After surgery, the patient may experience severe pain during the first three days, which disappears as the patient recovers completely, after about 10-15 days.
What is tonsillectomy
A tonsillectomy involves the surgical removal of the tonsils, which are lymph nodes located on either side of the back of the mouth (the soft palate) and are visible to the naked eye.
They are part of the Pirogov-Waldeyer lymphatic ring, which also includes:
- Pharyngeal tonsils or adenoids. Located in the upper part of the pharynx.
- Tubal tonsils. Located around the exit into the pharynx of the Eustachian tubes.
- Lingual tonsils. Located behind the tongue on both sides.
The role of the Pirogov-Waldeyer lymphatic ring is determined by its location - it is the first “garrison” of the immune system against the invasion of any pathogens. Tonsillitis is nothing more than a failed attempt by the immune system to defend itself against such an invasion.
Often, simultaneous removal of the adenoids is performed along with a tonsillectomy.
Tonsil removal in adults and children
Tonsil removal surgery , which can be complete or partial, depending on the instructions of the otolaryngologist and surgeon, can be performed on both adults and children.
In the past, tonsil removal was performed after a certain number of repeated infections. Moreover: sometimes they did not even wait for the infection to become chronic, but removed it after the first occurrence of the disease.
In the era before antibiotics, the relevance of surgery was dictated by serious complications after streptococcal sore throat: rheumatic fever and cardiac dysfunction (carditis and heart muscle dissection).
Today, tonsil removal is carried out only in the following cases:
| Tonsil hypertrophy | Recurrent pharyngotonsillitis | Peritonsillar abscess |
| Chronic streptococcal sore throat | Suspicion of neoplasms | Hidden tonsils |
Tonsil hypertrophy : Enlarged tonsils cause symptoms such as difficulty breathing, difficulty swallowing, sleep disturbances such as snoring or sleep apnea, malocclusion of teeth, speech problems, and in children, disturbances in the growth of the face and mouth.
Recurrent infections : viral or bacterial infections of the tonsils are accompanied by symptoms such as sore throat, moderate or very high fever up to 40°C, cough, redness of the tonsils with white plaques, swollen lymph nodes, diarrhea and vomiting. In this case, tonsillectomy is indicated when infections recur at least 5 times a year.
Peritonsillar abscess : is a complication of a sore throat that does not respond to therapy and in which pus accumulates at the level of the tonsils. This makes it necessary to remove the tonsils, even if the sore throat is not recurrent.
Chronic tonsillitis : infection of the tonsils caused by beta-hemolytic streptococcus type A, which is resistant to therapy. In this case, it is useful to remove the tonsils, since beta-hemolytic streptococcus, in addition to tonsillitis, can cause problems in the joints, such as rheumatism, psoriasis and kidney or heart disease.
Suspected neoplasm : Symptoms such as neck bulges and persistent low-grade fever may be a sign of tonsil and neck tumors.
Hidden tonsils : a condition in which small white plaques form at the level of the tonsils, causing bad breath and increased salivation.
Advantages and disadvantages of the operation
It is a common belief that people do not get sick from colds or bronchitis after having their tonsils removed; in fact, tonsillitis is not associated with these diseases, for which tonsil removal will not provide any protection.
Additionally, children and adults suffering from ear problems such as recurrent ear infections, stuffy ears, or sinusitis should not undergo tonsillectomy, but only adenoid removal.
Tonsillectomy surgery produces excellent results, but you must take into account certain disadvantages:
- Advantages: Closely related to the conditions we discussed in the previous paragraph. Thus, if you have frequent sore throats, acute or chronic, or difficulty breathing and sleep disorders, then the intervention will be beneficial because it solves these problems.
- Disadvantages: Associated with the operation, such as pain after surgery or bleeding, and improper scar formation.
Diet during recovery
Diet after surgery plays an important role in ensuring proper and rapid healing of wounds. In the first days after surgery, you should avoid solid foods as they can injure your throat. Hot drinks should also be avoided because they can cause blood vessels to dilate and increase the risk of bleeding.
Therefore, it is recommended:
- Cold and soft foods such as ice cream, especially with lemon, which, thanks to citric acid, promotes healing. However, consuming lemons in their pure form is not recommended because they are too acidic and can aggravate irritation.
- Drink cold drinks such as juices, tea, water several times a day to relieve the burning sensation and dry throat.
- Liquid foods such as pureed vegetables, vegetable broth and chicken broth, purees, baby food, semolina, but not too warm, preferably at room temperature.
- Ice cubes or popsicles to relieve pain.
Medicines
To relieve pain after surgery and to reduce the risk of bleeding, intravenous medications may be given:
- Pain relievers such as acetaminophen, alone or in combination with other analgesics.
- Antibiotics are taken for about a week after surgery to avoid infection.
- Hemostatic drugs, if the doctor deems it necessary.
- However, acetylsalicylic acid-based drugs (such as aspirin) and non-steroidal anti-inflammatory drugs such as ibuprofen or ketoprofen should be avoided because they act as anticoagulants and may cause bleeding.
Risks and complications of tonsil removal
Generally, tonsil removal does not cause any significant consequences and does not have any risks other than those associated with anesthesia and typical for any other operation.
There is, however, a rare chance that complications such as:
- Postoperative bleeding.
- Neck problems due to dislocation of the joint of the first cervical vertebrae, a condition called Grisel syndrome.
- Pharyngitis due to lack of tonsils as the first line of defense.
- Subcutaneous emphysema, which can occur if the pharyngeal muscles are damaged.
- Removing tonsils increases the risk of fluid reflux from the mouth into the nose.
These complications resolve, in any case, spontaneously within a few days. The biggest risk is bleeding, as it can lead to excessive blood loss and very serious systemic complications.
Source: https://sekretizdorovya.ru/publ/tonzillehktomija_riski_udalenija_mindalin/20-1-0-791
Tonsillectomy under general anesthesia: reviews
General anesthesia today is not the same as it was 10 or 20 years ago. It is non-toxic, does not cause complications, and feels like a regular night's sleep.
IMPORTANT: Many people believe that stress during surgery with general anesthesia is much more harmful than general anesthesia.
But what do people who have experienced general anesthesia during tonsillectomy say:
- Sveta: “They removed my tonsils under general anesthesia. What can I say, it was very difficult to come to my senses, I was not adequate for the whole day.”
- Irina: “Two years ago I had a tonsillectomy with general anesthesia. They gave me an injection in the ward, which made my vision blur. They took me to the operating room, put on an IV and put on a mask. There was nothing, no hallucinations, no feeling of falling. There was no withdrawal either, I just wanted to sleep. But after the anesthesia wore off, I felt a pain in my throat in all its colors.”
- Peter: “My wife, whose tonsils were removed under local anesthesia as a child, very vividly described to me all her terrible sensations. Therefore, when the doctor advised me to get rid of chronic tonsillitis quickly, I immediately chose general anesthesia. And I didn’t regret it. Everything went smoothly, the anesthesiologist was good.”