Postmenopause is the last phase of menopause, when the female body begins to function without the participation of ovarian hormones. Since each woman has to go through the menopause and, accordingly, postmenopause, a reliable understanding of the changes taking place and their significance largely help to form the correct attitude towards this stage of life, as well as to avoid serious negative consequences for the psycho-emotional sphere.
Menopause is a long, step-by-step process of gradual completion of the reproductive function of the female body. As a result, due to the “switching off” of the ovaries, physiological infertility is formed, and the body begins to function under conditions of hormonal (estrogen) deficiency. Menopause begins long before the disappearance of menstrual function, takes a long time and occurs with individual characteristics for each woman. In fact, it can be divided into three main stages (phases): before menopause (premenopause), menopause and the period after it - postmenopause.
The majority of the ovaries begin to “prepare” for completion of work already at the age of 45; conventionally, this age limit is taken as the beginning of menopause - premenopause. At this stage, the ovaries continue to secrete hormones necessary for the body, but their quantity and ratio change, which leads to menstrual dysfunction and the appearance of the first extragenital symptoms inherent in menopause.
After the final cessation of menstrual function, the next, shortest stage begins - menopause. Menopause as a medical term means the last spontaneous menstruation. The end of menstrual function is natural and physiological, so it should not be associated with pathology. However, there is often semantic confusion with this term when “menopause” refers to its pathological course (menopause syndrome) or the entire menopause. To accurately distinguish the last menstrual period from a period after a delay, it is customary to diagnose menopause only after at least 12 months have passed since the last menstrual bleeding.
After menopause, the final phase of menopause—postmenopause—starts. It is classified into early (first five years without menstruation) and late (ten years without menstruation). Menstrual flow in postmenopause is absolutely excluded, since the ovaries no longer function and cannot cause corresponding physiological changes in the endometrium. Therefore, any postmenopausal spotting indicates a serious pathological cause.
Sometimes experts use another term – “perimenopause”. Perimenopause is not a separate period of menopause, but only combines pre- and menopause.
The identification of periods in menopause is very arbitrary and is more important for clinical practice. Only the fact of the onset of menopause and all the accompanying changes are especially significant.
Most often, menopause occurs at the age of 50, however, all generally accepted time frames for the menopause are arbitrary, as they are established statistically. In healthy women (3%), menopause can be early (before 45 years), in every fifth out of a hundred it is late (after 55 years). If a woman with premature (relative to the “norm”) or delayed menopause does not have any pathological prerequisites, she is considered healthy.
So, the causes of postmenopause coincide with those in pre- and menopause, and the only reason for all climacteric changes occurring in the body is the cessation of ovarian function.
The function of the ovaries throughout the entire reproductive stage (which lasts 30–35 years) remains virtually unchanged, with the exception of the periods of childbirth. When the ovaries form, they initially contain many follicles - small spherical formations resembling vesicles, each of which in the future can become a source of a sexually mature egg. Each menstrual cycle in one of the ovaries (more often they function alternately), 10–15 immature follicles begin to actively grow (proliferate) and change structurally, transforming into a hormonal mini-gland capable of secreting estrogens. Then nature “selects” the most viable proliferating follicle (usually the only one), which can ensure the correct maturation of a full-fledged egg, and gives it the opportunity to develop further; the remaining follicles are reduced without reaching the required degree of maturity.
The first, follicular, phase of the menstrual cycle ends with the rupture of the follicle and the release of a mature egg outside the ovary - ovulation. In the absence of fertilization, the egg dies within two days, and the second, luteal, phase starts in the ovary. The structure of the elements remaining after the death of the follicle changes, and another temporary hormonal structure is formed - the corpus luteum, which is responsible for the secretion of progesterone. The corpus luteum stops functioning and is reduced shortly before menstrual bleeding.
All events occurring in the ovaries are controlled by the central unit - the hypothalamus and pituitary gland. The maturation of the follicle and egg, respectively, occurs with the participation of follicle-stimulating hormone (FSH) of the pituitary gland, and the luteinizing hormone (LH) secreted by it actively affects the corpus luteum.
Such cyclically changing hormonal activity of the ovaries ensures not only the implementation of the reproductive function, it affects almost all the most important organs and tissues of the female body, and the completion of the hormonal ovarian function leads not only to physiological infertility, but also to general functional dysfunction.
The ovaries do not suddenly stop working. To avoid excessive stress on the body, nature has kindly programmed a long physiological transition from a state of normal estrogenic influence to its absence. Usually it is 8 – 10 years.
Postmenopause is the culmination of the menopausal period and is characterized by the greatest severity of all symptoms associated with a deficiency of estrogen influence.
Postmenopausal therapy has many directions and depends on the specific situation. For the majority, it does not go beyond symptomatic treatment and is intended to compensate for the consequences of hormonal deficiency.
What is postmenopause
Postmenopause, in fact, corresponds to the period of a woman’s life after menopause; it is the longest time stage of the menopause, as it begins a year after the last menstrual bleeding and continues until old age.
It should be recalled once again that postmenopause itself is not a pathology, since the causes of postmenopause themselves are natural and logical.
A healthy woman, as a rule, enters the postmenopausal period with good compensatory capabilities that help her cope with the negative consequences of menopause and maintain the usual rhythm of life. More often, the pathology of the postmenopausal period is associated with compensatory dysfunction, that is, when the body is simply unable to adapt to new operating conditions.
Experts often have to answer the question “what is the normal level of hormones in postmenopause,” because it is hormonal dysfunction and its degree that influence structural and functional changes and is also responsible for pathological symptoms.
All changes that occur during menopause are associated with estrogens. Age-related depletion of ovarian function provokes a pronounced estrogen deficiency, which causes disruption of the entire body.
It is incorrect to say that a woman has no estrogen at all after menopause. Estrogenic activity is recorded over many years and after the cessation of ovarian function, as well as after surgical removal of the ovaries. However, if during the reproductive pores estrogens are synthesized in the ovaries, then after the main female hormonal gland is “turned off” they are of extraglandular origin.
The most important female estrogens are estradiol, estrone and estriol. The main source of all three estrogens in a non-pregnant healthy woman is the ovaries. However, the adrenal glands and adipose tissue are also capable of producing them. Estrogens have a unique self-conversion function, thanks to which the deficiency of one estrogen is replenished at the expense of another. Thus, estradiol can be converted to estrone and vice versa. The interconversion of estrogens occurs in the tissues of different organs, and the place of their disposal is the liver.
A clear norm of hormones in postmenopause has not been established, since the quantitative change in hormones is significantly influenced by the onset and course of previous periods of menopause, as well as the presence of hormonal dysfunction during the reproductive period.
Soon after the onset of menopause, against the background of the complete absence of follicles responsible for the secretion of estrogen, the level of follicle-stimulating hormone increases significantly (10 and even 20 times). The concentration of luteinizing hormone also increases, but to a lesser extent - three times. Since it is not the ovaries, but the peripheral structures that are responsible for the synthesis of estrogen in postmenopause, their quantitative ratio also becomes different: against the background of a decrease in the concentration of estradiol, the amount of estrone increases. The androgen-estrogen ratio after menopause begins to gradually shift in favor of androgens.
Heavy discharge
According to statistics, about 28% of women suffer from fairly heavy discharge during premenopause. Such menstrual discharge is characterized by: heavy bleeding, the presence of blood clots, and a rich red color. As a result of such heavy menstrual flow, anemia may develop. This is why a woman feels:
- weakness;
- dizziness;
- nausea.
If you have such discharge, you need to see a doctor.
Popular articles:
|
Symptoms and signs of postmenopause
Extraglandular sources of estrogen continue to function actively for several years after menopause to support the functioning of estrogen-dependent organs: mammary glands, uterus, vulva and vagina. Also, other, extragenital structures - excretory, musculoskeletal, cardiovascular and others - also need estrogens in postmenopause. If the hormonal influence necessary for the normal functioning of these structures becomes insufficient, a number of pathological conditions appear.
The most “famous” symptoms of menopause (hot flashes during menopause, neurological and emotional) may also be present in postmenopause, but they no longer dominate; they are gradually replaced by urogenital, cardiovascular disorders and changes in bone and muscle tissue.
Two years after the fact of menopause is established, a complex of so-called delayed clinical symptoms of postmenopause appears:
— Urogenital disorders. The lack of proper influence on the mucous membranes of the genital tract provokes their structural changes, namely atrophy. The thinned mucous membrane of the vulva, vaginal cavity and urethra loses its strong protective properties and becomes vulnerable to mechanical injury and infectious aggression. A significant decrease in the number of lactobacilli in the vaginal microflora provokes dysbiotic local disorders and a subsequent inflammatory process.
During this period, vaginitis, cystitis, and urethritis of atrophic origin often occur. Inflammatory changes in the urethra can alter the function of the bladder sphincters and cause frequent urination and/or urinary incontinence.
Pathological discharge in postmenopause is associated with a nonspecific inflammatory process. Vaginal discharge can be serous or purulent, accompanied by severe discomfort, itching, burning, and have an unpleasant odor. Smears and cultures often reveal opportunistic flora and signs of severe dysbiosis.
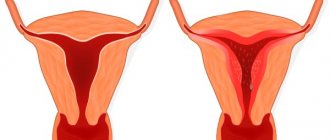
Bloody discharge in postmenopause is never consistent with the concept of physiological norm. It is necessary to differentiate between bleeding and minor sanguineous discharge against the background of mechanical action or inflammation. A woman cannot independently determine the nature of the bleeding, so she should definitely visit a specialist.
Uterine bleeding in postmenopause is usually diagnosed in the early (before 55 years) period and is associated with a pathology of benign origin. The most popular reasons are polyps and/or hyperplastic process in the endometrium. In fact, polyps are also a reflection of hyperplastic changes in the endometrium, but of a local nature, when the mucous membrane does not grow over the entire area, but locally.
Uterine bleeding in postmenopause in older (up to 65 years) age groups occurs not only on a benign basis, but also due to endometrial cancer, its frequency peaks in this age group.
— Changes in the condition of the skin and its appendages. Estrogens keep hair and nails strong and skin elastic. In the absence of proper estrogenic influence, the skin becomes dry, thins, wrinkles form, nails break more easily, and hair loses elasticity and falls out more.
Late clinical manifestations of postmenopause include:
— Postmenopausal metabolic syndrome. Arterial hypertension, atherosclerosis, disorders of lipid metabolism and glucose utilization prevail in its composition. Active complaints include: increased heartbeat, angina attacks, lability of pulse and blood pressure.
Changes in lipid metabolism provoke weight gain. As a rule, almost all women recover during menopause, even those who adhere to a diet. However, the number of kilograms gained is unequal and has an important diagnostic value: if a woman does not change her diet, but her weight increases by more than five kilograms, her metabolic disorders no longer correlate with natural ones.
— Visual, hearing and memory disorders associated with insufficient influence of estrogens on the neurological sphere.
— Changes in the structure of the musculoskeletal system. In postmenopause, muscle tone and bone structure change. Thanks to estrogens, the skeletal system during the reproductive period received a sufficient amount of calcium and other “building material”. In postmenopause, signs of osteoporosis appear when calcium does not accumulate in the bone structures, but is “washed out”, so the bones become fragile and the joints become less strong.
It should be noted that the listed changes in almost half (45%) of women experiencing menopause occur with minimal clinical manifestations and do not have a high degree of severity. A healthy woman who pays due attention to her gynecological health has a high chance of surviving menopause and, accordingly, postmenopause, calmly.
Which ob® products to use during premenopausal periods
- When the discharge becomes heavier: ob® ExtraDefence
Designed with SilkTouch™ safety wings for added protection against leaks and slippage. This means that these sanitary products are able to retain fluid that other tampons might miss, providing reliable protection during perimenopause. Tampons with wings do not change the feeling of using this hygiene product at all. With ob® ExtraDefence you don't have to worry about your tampon moving, even during restless sleep.
- When the discharge becomes thinner: ob® ProComfort®
Smooth Technology* is designed to provide an even smoother tampon surface**, while the silky SilkTouch™ coating makes insertion and removal as easy as possible. One of the symptoms of age-related premenopause may be dryness and discomfort in the vagina during menstruation and on the remaining days of the cycle. ob® ProComfort® tampons will give you comfortable insertion and provide reliable and gentle protection against leaks during this difficult period of life.>
* Smooth Technology ** compared to previous version ob® ProComfort®
Treatment
The period of premenopause itself is not considered a pathology. However, for some symptoms that cause a woman discomfort or may cause complications, the doctor may prescribe some treatment. The main indicator is a blood test for hormones. Adjustment of hormonal levels is prescribed only after a blood test for hormones. For this purpose, hormone replacement therapy is prescribed. To eliminate negative symptoms during premenopause such as pain, weakness, hot flashes, the doctor prescribes non-hormonal medications.
Indications for hormone replacement therapy
If the following points are observed:
- early onset of premenopause before age 40;
- the onset of artificial menopause (after surgery, such as removal of the ovaries);
- pathological symptoms during premenopause - hot flashes, insomnia, depression;
- the presence of changes in the genitourinary system - cystitis, colpitis, pain during sexual intercourse;
- first signs of osteoporosis.
Treatment method:
Use of estrogens
This treatment is only possible if the uterus is removed.
- estrogens are used in courses of 28 days;
- daily dose 2 mg;
- estradiol skin patch;
- cutaneous gel 0.5 mg daily;
- vaginal cream 0.5-1 mg.
Use of progesterones
- daily dosage 100 mcg;
- intrauterine device with hormone.
Combined treatment
Contains hormones such as estrogen, progesterone. Contraceptive drugs are mainly prescribed. The doctor selects the course of treatment and medications strictly individually.
Contraindications for hormone replacement therapy
- breast cancer;
- pelvic cancer;
- uterine bleeding;
- endometrial hyperplasia;
- vein thrombosis, varicose veins;
- angina pectoris;
- hypertonic disease;
- liver disease.