Main symptoms:
- Apathy
- Pallor
- Headache
- Jaundice
- Ammonia smell from breath
- Circulatory disorders
- Dehydration
- Osteoporosis
- Reduced blood clotting
- Loss of appetite
- Vomit
- Extreme thirst
- Weakness
- Nausea
- Increased urine output
- Frequent night urination
Renal failure means a syndrome in which all functions relevant to the kidneys are disrupted, resulting in a disorder of various types of metabolism in them (nitrogen, electrolyte, water, etc.). Renal failure, the symptoms of which depend on the course of this disorder, can be acute or chronic, each of the pathologies develops due to the influence of different circumstances.
Online consultation on the disease “Kidney failure”.
Ask a question to the specialists for free: Urologist.
- Description of the disease
- Causes of kidney failure
- ARF: symptoms
- OPN: forecast
- CRF: symptoms
- CRF: prognosis
- Diagnostics
- Treatment
general description
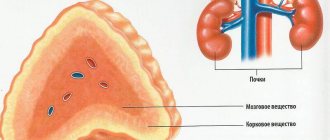
The main functions of the kidneys, which in particular include the functions of removing metabolic products from the body, as well as maintaining the balance in the acid-base state and water-electrolyte composition, directly involve renal blood flow, as well as glomerular filtration in combination with the tubules. In the latter version, the processes consist of concentration ability, secretion and re-absorption.
What is noteworthy is that not all changes that may affect the listed variants of the processes are the obligatory cause of subsequent pronounced disturbances in kidney function; accordingly, any disturbance in the processes cannot be defined as renal failure, which interests us. Thus, it is important to determine what renal failure actually is and on the basis of what specific processes it is advisable to distinguish it as this type of pathology.
So, by renal failure we mean a syndrome that develops against the background of severe disturbances in renal processes, in which we are talking about a disorder of homeostasis. Homeostasis generally refers to the maintenance at a level of relative constancy of the internal environment characteristic of the body, which in the variant we are considering is attached to its specific area - that is, to the kidneys. At the same time, azotemia (in which there is an excess of protein metabolic products in the blood, which includes nitrogen), disturbances in the body’s general acid-base balance, as well as disturbances in the water-electrolyte balance, become relevant in these processes.
As we have already noted, the condition we are interested in today can arise against the background of the influence of various causes; these causes, in particular, are determined by what type of renal failure (acute or chronic) we are talking about.
Renal failure, the symptoms of which in children manifest themselves similarly to those in adults, will be discussed below in terms of the course of interest (acute, chronic) in combination with the reasons that provoke their development. The only point that I would like to note against the background of the commonality of symptoms is that in children with a chronic form of renal failure, growth retardation, and this connection has been known for quite a long time, noted by a number of authors as “renal infantilism.”
The actual reasons that provoke such a delay have not been fully elucidated, however, the loss of potassium and calcium against the background of effects provoked by acidosis can be considered as the most likely factor leading to it. It is possible that this also occurs due to renal rickets, which develops as a result of the relevance of osteoporosis and hypocalcemia in the condition under consideration in combination with the lack of conversion to the required form of vitamin D, which becomes impossible due to the death of renal tissue.
Kidney structure
Kidney failure: causes
- Acute renal failure : Shock kidney. This state is achieved due to traumatic shock, which manifests itself in combination with massive tissue damage, which occurs as a result of a decrease in the total volume of circulating blood. This condition is provoked by: massive blood loss; abortions; burns; a syndrome that occurs against the background of crushing muscles with their crushing; blood transfusion (in case of incompatibility); debilitating vomiting or toxicosis during pregnancy; myocardial infarction.
- Toxic kidney. In this case, we are talking about poisoning that occurred due to exposure to neurotropic poisons (mushrooms, insects, snake bites, arsenic, mercury, etc.). Among other things, intoxication with radiopaque substances, medications (analgesics, antibiotics), alcohol, and narcotic substances is also relevant for this option. The possibility of acute renal failure in this variant of the provoking factor cannot be ruled out, given the relevance of professional activities directly related to ionizing radiation, as well as heavy metal salts (organic poisons, mercury salts).
- Acute infectious kidney. This condition is accompanied by the impact of infectious diseases on the body. So, for example, an acute infectious kidney is an actual condition in sepsis, which, in turn, can have a different type of origin (primarily anaerobic origin is relevant here, as well as an origin against the background of septic abortions). In addition, the condition in question develops against the background of hemorrhagic fever and leptospirosis; with dehydration due to bacterial shock and infectious diseases such as cholera or dysentery, etc.
- Embolisms and thromboses relevant to the renal arteries.
- Acute pyelonephritis or glomerulonephritis.
- Obstruction of the ureters due to compression, the presence of tumor formation or stones in them.
It should be noted that acute renal failure occurs in about 60% of cases as a result of injury or surgery, about 40% occurs during treatment in medical institutions, and up to 2% during pregnancy.
- Chronic renal failure: Chronic form of glomerulonephritis.
- Secondary kidney damage caused by the following factors: arterial hypertension;
- diabetes;
- viral hepatitis;
- malaria;
- systemic vasculitis;
- systemic diseases affecting connective tissues;
- gout.
Leadership in the positions of the causes provoking the development of chronic renal failure syndrome is assigned to chronic glomerulonephritis and the chronic form of pyelonephritis.
Kidney failure: causes
Etiology
Etiology of prerenal acute renal failure
Prerenal acute renal failure can develop in conditions that are accompanied by a decrease in cardiac output (pulmonary embolism, heart failure, arrhythmia, cardiac tamponade, cardiogenic shock). Often the cause is a decrease in the amount of extracellular fluid (with diarrhea, dehydration, acute blood loss, burns, ascites caused by cirrhosis of the liver). May occur due to severe vasodilation that occurs during bacteriotoxic or anaphylactic shock.
Etiology of renal acute renal failure
Occurs due to toxic effects on the renal parenchyma of fertilizers, poisonous mushrooms, copper salts, cadmium, uranium and mercury. Develops with uncontrolled use of nephrotoxic medications (antitumor drugs, a number of antibiotics and sulfonamides). X-ray contrast agents and the listed drugs, prescribed in the usual dosage, can cause renal acute renal failure in patients with impaired renal function.
In addition, this form of acute renal failure occurs when a large amount of myoglobin and hemoglobin circulates in the blood (with severe macrohemaglobinuria, transfusion of incompatible blood, prolonged compression of tissue during injury, drug and alcohol coma). Less commonly, the development of renal acute renal failure is caused by inflammatory kidney disease.
Etiology of postrenal acute renal failure
It develops when there is a mechanical disturbance in the passage of urine due to bilateral obstruction of the urinary tract by stones. Less commonly occurs with tumors of the prostate gland, bladder and ureters, tuberculous lesions, urethritis and periurethritis, dystrophic lesions of the retroperitoneal tissue.
In severe combined injuries and extensive surgical interventions, acute renal failure is caused by several factors (shock, sepsis, blood transfusion, treatment with nephrotoxic drugs).
Acute renal failure: symptoms
Acute renal failure, which we will further abbreviate to the abbreviation ARF, is a syndrome in which there is a rapid decrease or complete cessation of kidney functions, and these functions can decrease/stop in one kidney or in both at the same time. As a result of this syndrome, metabolic processes are sharply disrupted, and an increase in products formed during nitrogen metabolism is noted. Relevant disorders of the nephron, which is defined as a structural renal unit, in this situation arise due to a decrease in blood flow in the kidneys and, at the same time, due to a decrease in the volume of oxygen delivered to them.
The development of acute renal failure can occur either within literally a few hours or within a period of 1 to 7 days. The duration of the condition that patients experience with this syndrome can be 24 hours or more. Timely seeking medical help with subsequent adequate treatment can ensure complete restoration of all functions in which the kidneys are directly involved.
Turning, in fact, to the symptoms of acute renal failure, it should initially be noted that in the overall picture in the foreground there is precisely the symptomatology that served as a kind of basis for the occurrence of this syndrome, that is, from the disease that directly provoked it.
Thus, we can distinguish 4 main periods that characterize the course of acute renal failure: the shock period, the period of oligoanuria, the recovery period of diuresis in combination with the initial phase of diuresis (plus the polyuria phase), as well as the recovery period.
The symptoms of the first period (mostly its duration is 1-2 days) are characterized by the already noted above symptoms of the disease that provoked the OPS syndrome - it is at this moment in its course that it manifests itself most clearly. Along with it, tachycardia and a decrease in blood pressure are also noted (which in most cases is transient, that is, soon stabilizing to normal levels). Chills occur, pale and yellow skin is noted, and body temperature rises.
The next, second period (oligoanuria, duration is generally about 1-2 weeks), is characterized by a decrease or absolute cessation of the process of urine formation, which is accompanied by a parallel increase in residual nitrogen in the blood, as well as phenol in combination with other types of metabolic products. What is noteworthy is that in many cases it is during this period that the condition of most patients improves significantly, although, as already noted, there is no urine. Later, complaints of severe weakness and headache appear; patients’ appetite and sleep worsen. Nausea with accompanying vomiting also appears. The progression of the condition is indicated by the smell of ammonia that appears during breathing.
Also, in acute renal failure, patients experience disorders associated with the activity of the central nervous system, and these disorders are quite diverse. The most common manifestations of this type are apathy, although the opposite option is not excluded, in which, accordingly, patients are in an excited state, having difficulty navigating the environment that surrounds them; a general confusion of consciousness can also be a companion to this state. In frequent cases, convulsive seizures and hyperreflexia are also observed (that is, revival or strengthening of reflexes, in which, again, patients are in an overly excitable state due to an actual “shock” to the central nervous system).
In situations where acute renal failure occurs against the background of sepsis, patients may develop a herpetic-type rash concentrated in the area around the nose and mouth. Skin changes in general can be very diverse, manifesting both in the form of urticarial rash or fixed erythema, and in the form of toxicoderma or other manifestations.
Almost every patient experiences nausea and vomiting, and somewhat less frequently, diarrhea. Especially often, certain digestive phenomena occur in combination with hemorrhagic fever along with renal syndrome. Lesions of the gastrointestinal tract are caused, first of all, by the development of excretory gastritis with enterocolitis, whose nature is defined as erosive. Meanwhile, some of the current symptoms are caused by disturbances arising from the electrolyte balance.
In addition to the listed processes, there is the development of edema in the lungs, resulting from increased permeability, which the alveolar capillaries have during this period. It is difficult to recognize it clinically, so diagnosis is made using an x-ray of the chest area.
During the period of oligoanuria, the total volume of urine excreted decreases. So, initially its volume is about 400 ml, and this, in turn, characterizes oliguria; then, with anuria, the volume of urine excreted is about 50 ml. The duration of oliguria or anuria can be up to 10 days, but some cases indicate the possibility of increasing this period to 30 days or more. Naturally, with protracted manifestations of these processes, active therapy is required to maintain human life.
During the same period, anemia becomes a constant manifestation of acute renal failure, in which, as the reader probably knows, hemoglobin decreases. Anemia, in turn, is characterized by pale skin, general weakness, dizziness and shortness of breath, and possible fainting.
Acute renal failure is also accompanied by liver damage, and this occurs in almost all cases. As for the clinical manifestations of this lesion, they consist of yellowness of the skin and mucous membranes.
The period during which there is an increase in diuresis (that is, the volume of urine formed within a certain time period; as a rule, this indicator is considered within 24 hours, that is, within the framework of daily diuresis) often occurs several days after the end of oliguria/anuria. It is characterized by a gradual onset, in which urine is initially excreted in a volume of about 500 ml with a gradual increase, and only after, again, gradually, this figure increases to about 2000 ml or more per day, and from this moment we can talk about the beginning of the third period of OPN.
From the third period, improvements in the patient’s condition are not immediately observed; moreover, in some cases the condition may even worsen. The polyuria phase in this case is accompanied by weight loss of the patient; the duration of the phase is on average about 4-6 days. There is an improvement in the appetite of patients; in addition, previously relevant changes in the circulatory system and the functioning of the central nervous system disappear.
Conventionally, the beginning of the recovery period, that is, the next, fourth period of the disease, marks the day of normalization of urea or residual nitrogen levels (which is determined based on the relevant tests), the duration of this period ranges from 3-6 months to 22 months. During this period of time, homeostasis is restored, renal concentration function and filtration improve, along with an improvement in tubular secretion.
It should be taken into account that over the next year or two it is possible that signs indicating functional failure in certain systems and organs (liver, heart, etc.) will persist.
Symptoms
At the initial stage, the symptoms of acute renal failure are very similar to the symptoms of diseases or conditions that led to acute renal failure. These are symptoms of poisoning, shock, illness.
Along with this, with the further development of the syndrome, the patient begins to notice that the amount of urine excreted per day decreases sharply. Thus, oliguria develops first, and soon anuria.
This manifestation is accompanied by symptoms of intoxication of the body - vomiting, loss of appetite. The patient becomes drowsy, his consciousness is inhibited, sometimes to the point where hallucinations and even convulsions appear.
The skin also changes - it becomes dry, pale, and small hemorrhages and swelling appear on it. The patient's breathing becomes frequent and deep. The doctor almost always listens for tachycardia in the patient, an abnormal heart rhythm and increased blood pressure are noted. Also characteristic are disorders of the digestive system - bloating and loose stools.
Acute renal failure in children has the same symptoms as in adults and also requires immediate medical intervention.
When these symptoms appear and develop, it is extremely important to start treatment promptly and adequately. Only if this condition is met in the shortest possible time, it is possible to restore diuresis and relieve the previously increasing symptoms. Full recovery occurs in six months, but may take a couple of years.
Acute renal failure: prognosis
Acute renal failure, if it does not cause death for the patient, ends with a slow but, one might say, confident recovery, and this does not indicate the relevance for him of a tendency to transition to the development of chronic kidney disease against the background of this condition.
After about 6 months, more than half of the patients reach a state of full restoration of working capacity, however, the option of limiting it for a certain part of the patients is not excluded, on the basis of which they are assigned disability (group III). In general, ability to work in this situation is determined based on the characteristics of the course of the disease that provoked acute renal failure.
Pathogenesis.
The primary response of the kidneys to many etiological factors is a decrease in cortical circulation and preglomerular vasoconstriction. They lead to a decrease in sodium reabsorption in the proximal tubules. Its concentration in the distal tubules increases, reaches the maculadensa and leads to activation of the renin-angiothesin system. Angiotensin II acts locally and increases vasoconstriction of afferent arterioles, reduces glomerular filtration and renal circulation. A vicious circle is created, cellular edema and hypoxia increase. Oliguria is promoted by impaired production of prostaglandin E and prostaglandin. These are powerful vasodilators and antagonists of the renin-angiotensin system.
New data obtained from studying the pathogenesis of oliguric acute renal failure show that, in addition to the described factors, disturbances in renal autoregulation, increased production of endogenous vasopressin, impaired ability of renal mitochondria to absorb oxygen, increased cytolytic activity of calcium, etc. are also important.
The persistence of diuresis in non-oliguric renal failure can be explained by three mechanisms. The hemodynamic function of a small number of nephrons is preserved after the initial lesion, while their resorption capacity is impaired. Nephrons lose their ability to resorb filtrate and polyuria occurs. The decrease in filtration can be generalized, but it is less pronounced than the depressed resorption capacity. Polyuria may result from a reduction in interstitial hypertonicity and the corticomedullary osmotic gradient. This increases the fractionated release of water filtered to the loop of Henle.
Diuretic phase.
The diuretic phase begins when the daily urine volume is more than 250 ml/m2 body area. The onset of this phase cannot be predicted (from 24 hours to the 60th day of oliguria). It usually develops gradually and is diagnosed not so much by polyuria as by an increase in the ratio of urea to creatinine concentrations in urine and plasma. In the early diuretic phase, large amounts of electrolytes and water are lost. This can potentiate severe hypovolemia, especially since concentrating ability has not yet been restored and the urine is hypotonic in relation to plasma. With the restoration of renal function, plasma biochemical parameters also normalize. At the same time, the patient’s clinical condition quickly improves.
Forecast.
Mortality varies and, depending on the leading pathology, is 30-65%, on average - 50%. Complications matter. The high mortality rate is explained by the inability to predict the onset of acute renal failure and the increasingly common occurrence of iatrogenic kidney damage.
Chronic renal failure: symptoms
CRF, as we will further periodically define the considered variant of the course of chronic renal failure syndrome, is a process indicating an irreversible impairment to which kidney function has been subjected for a duration of 3 months or longer. This condition develops as a result of the gradual progression of the death of nephrons (structural and functional units of the kidneys). Chronic renal failure is characterized by a number of disorders, and in particular these include disturbances in excretory function (directly related to the kidneys) and the appearance of uremia, which occurs as a result of the accumulation of nitrogenous metabolic products in the body and the toxic effects they have.
At the initial stage, chronic renal failure has insignificant, one might say, symptoms, therefore it can only be determined on the basis of appropriate laboratory tests. Already obvious symptoms of chronic renal failure appear at the time of death of about 90% of the total number of nephrons. The peculiarity of this course of renal failure, as we have already noted, is the irreversibility of the process with the exception of subsequent regeneration of the renal parenchyma (that is, the outer layer from the cortex of the organ in question and the inner layer, presented in the form of the medulla). In addition to structural kidney damage against the background of chronic renal failure, other types of immunological changes cannot be excluded. The development of an irreversible process, as we have already noted, can be quite short (up to six months).
With chronic renal failure, the kidneys lose the ability to concentrate urine and dilute it, which is determined by a number of actual lesions of this period. In addition, the secretory function characteristic of the tubules is significantly reduced, and when the terminal stage of the syndrome we are considering is reached, it is completely reduced to zero. Chronic renal failure contains two main stages, this is the conservative stage (at which, accordingly, conservative treatment remains possible) and the terminal stage (in this case, the question is raised regarding the choice of replacement therapy, which consists of either extrarenal cleansing or kidney transplant procedure).
In addition to disorders associated with the excretory function of the kidneys, disruption of their homeostatic, blood purification and hematopoietic functions also becomes relevant. Forced polyuria (increased urine production) is noted, on the basis of which one can judge a small number of still surviving nephrons performing their functions, which occurs in combination with isosthenuria (in which the kidneys are unable to produce urine with a higher or lower specific gravity). Isosthenuria in this case is a direct indicator that renal failure is at the final stage of its development. Along with other processes relevant to this condition, chronic renal failure, as can be understood, also affects other organs in which, as a result of processes characteristic of the syndrome in question, changes similar to dystrophy develop with simultaneous disruption of enzymatic reactions and a decrease in reactions of an immunological nature.
Meanwhile, it should be noted that the kidneys in most cases do not lose the ability to completely excrete water entering the body (in combination with calcium, iron, magnesium, etc.), due to the corresponding influence of which adequate activities of other bodies.
So, now let's move directly to the symptoms that accompany chronic renal failure.
First of all, patients experience a pronounced state of weakness, drowsiness and general apathy predominate. Polyuria also appears, in which about 2 to 4 liters of urine are released per day, and nocturia, characterized by frequent urination at night. As a result of this course of the disease, patients are faced with dehydration, and as it progresses, with the involvement of other systems and organs of the body in the process. Subsequently, weakness becomes even more pronounced, accompanied by nausea and vomiting.
Other manifestations of symptoms include puffiness of the patient’s face and severe muscle weakness, which in this condition occurs as a result of hypokalemia (that is, a lack of potassium in the body, which, in fact, is lost due to processes relevant to the kidneys). The skin of patients is dry, itchy, excessive agitation is accompanied by increased sweating. Muscle twitching also appears (in some cases reaching cramps) - this is already caused by loss of calcium in the blood.
Bones are also affected, which is accompanied by pain, disturbances in movement and gait. The development of this type of symptomatology is caused by a gradual increase in renal failure, balance in calcium levels and reduced glomerular filtration function in the kidneys. Moreover, such changes are often accompanied by changes in the skeleton, even at the level of a disease such as osteoporosis, and this occurs due to demineralization (that is, a decrease in the content of mineral components in bone tissue). The previously noted pain in movements occurs against the background of the accumulation of urates in the synovial fluid, which, in turn, leads to the deposition of salts, as a result of which this pain, in combination with the inflammatory reaction, occurs (this is defined as secondary gout).
Many patients experience chest pain, which can also appear as a result of fibrous uremic pleurisy. In this case, when listening to the lungs, wheezing may be noted, although more often this indicates the pathology of pulmonary heart failure. Against the background of such processes in the lungs, the possibility of secondary pneumonia cannot be ruled out.
Anorexia developing with chronic renal failure can cause patients to develop an aversion to any food, also combined with nausea and vomiting, the appearance of an unpleasant taste in the mouth and dryness. After eating, you may feel fullness and heaviness in the pit of the stomach - along with thirst, these symptoms are also characteristic of chronic renal failure. In addition, patients experience shortness of breath, often high blood pressure, and frequent pain in the heart area. Blood clotting decreases, which causes not only nosebleeds, but also gastrointestinal bleeding, with possible skin hemorrhages. Anemia also develops against the background of general processes affecting the composition of the blood, and in particular leading to a decrease in the level of red blood cells, which is relevant for this symptom.
Late stages of chronic renal failure are accompanied by attacks of cardiac asthma. Edema forms in the lungs, consciousness is impaired. As a result of a number of these processes, the possibility of coma cannot be excluded. An important point is also the susceptibility of patients to infectious effects, because they easily fall ill with both common colds and more serious diseases, the impact of which only worsens the general condition and kidney failure, in particular.
In the preterminal period of the disease, patients experience polyuria, while in the terminal period there is predominantly oliguria (some patients experience anuria). Kidney functions, as you can understand, decrease with the progression of the disease, and this happens until they disappear completely.
Chronic renal failure: prognosis
The prognosis for a given variant of the course of the pathological process is determined largely on the basis of the course of the disease, which gave the main impetus for its development, as well as on the basis of complications that arose during the process in a complex form. Meanwhile, an important role for the prognosis is given to the phase (period) of chronic renal failure that is relevant for the patient, with the rate of development that characterizes it.
Let us highlight separately that the course of chronic renal failure is not only an irreversible process, but also a steadily progressive one, and therefore a significant prolongation of the patient’s life can only be said if he is provided with chronic hemodialysis or a kidney transplant is performed (we will dwell on these treatment options below).
Of course, cases in which chronic renal failure develops slowly with a corresponding clinical picture of uremia cannot be excluded, but these are rather exceptions - in the vast majority of cases (especially with high arterial hypertension, that is, high blood pressure), the clinical picture of this disease is characterized by the previously noted rapid progression.
Diagnosis
The main marker taken into account when diagnosing acute renal failure is an increase in the level of nitrogen compounds and potassium in the blood, which occurs with a simultaneous significant decrease in urine output (up to the complete cessation of this process). An assessment of the concentrating ability of the kidneys and the volume of urine excreted during the day is based on the results obtained from the Zimnitsky test.
An important role is also played by a biochemical blood test for electrolytes, creatinine and urea, because it is on the basis of indicators for these components that one can draw specific conclusions regarding the severity of acute renal failure, as well as how effective the methods used in treatment are.
The main task of diagnosing acute renal failure comes down to determining this form itself (that is, its specification), for which an ultrasound scan of the bladder and kidney area is performed. Based on the results of this research measure, the relevance/absence of ureteral obstruction is determined.
If necessary, to assess the state of renal blood flow, an ultrasound ultrasound procedure is performed, aimed at an appropriate study of the renal vessels. A kidney biopsy may be performed if acute glomerulonephritis, tubular necrosis, or systemic disease is suspected.
As for the diagnosis of chronic renal failure, it uses, again, urine and blood tests, as well as the Rehberg test. As a basis for confirming chronic renal failure, data indicating a reduced level of filtration, as well as an increase in the level of urea and creatinine are used. In this case, performing the Zimnitsky test determines isohyposthenuria. Ultrasound of the kidney area in this situation reveals thinning of the kidney parenchyma while simultaneously decreasing in size.
Clinic.
The severity of the syndrome varies from a mild, transient episode of oliguria to catastrophic forms with prolonged oliguria, severe electrolyte disturbances, sometimes affecting many organs and systems and requiring urgent therapeutic measures. It is necessary to differentiate between prerenal, renal - oliguric and non-oliguric, and postrenal renal failure. With a more precise diagnosis of renal failure, it is necessary to determine the type of renal lesion: acute tubular necrosis, glomerulonephritis, acute interstitial nephritis or exacerbation of chronic nephropathy. The following set of necessary studies helps to clarify the diagnosis:
1. History of previous water-salt losses, medication use, toxic effects, hypertension, nocturia and polyuria, complete anuria.
2. Objective examination: state of hydration, bladder filling, heaviness in the lumbar region, concomitant anomalies of the cardiovascular, gastrointestinal and nervous systems.
3. Determination of serum electrolytes, osmolarity, creatinine and urea levels.
4. Urine - hourly urine output, sediment, culture, osmolarity, amount of sodium, urea and creatinine.
5. Excretory urography (EUG), voiding cystography, cystoscopy, retrograde urography, echography and radioisotope scintigraphy.
Additional diagnostic procedures are as follows: in dehydrated patients - immediate rehydration with 10-20 ml/kg body weight of 0.9% NaCl and/or salt-free Humman-albumin at 0.5-1.0/kg weight per 1 hour. If diuresis is absent, administer a sterile catheter and perform a mannitol stimulation test: 0.5-1.0 kg of mass in 10-20 minutes. If urine output increases to 20 ml/h or more, tubular function is considered good and oliguria is prerenal. If unsuccessful, the mannitol test can be repeated. A necessary condition for the correct performance of the mannitol test is rapid infusion. Mannitol does not penetrate the cell, is filtered by the glomeruli and is not resorbed in the tubules. It causes osmotic diuresis, preventing the formation of casts, reduces blood viscosity and tissue resistance and increases plasma volume. Mannitol reduces the contraction of afferent arterioles and allows for an increase in renal circulation and glomerular filtration.
Contraindications to the mannitol test are complete anuria, heart failure and pulmonary edema.
Patients with normovolemia or if the mannitol test fails are prescribed furantril, Ac. ethacrynicum, which increase blood flow to the renal cortex and reduce blood flow to the juxtamedullary space, dilate the tubules and increase tubular flow through the nephron. inhibit the reabsorption of NaCl into the macula densa. Furantril and Ac. ethacrynicum are contraindicated in hypovolemia.
There are three main stages of acute renal failure: initial, oliguric and diuretic; the fourth is also accepted - restorative.
I. Initial stage. Lasts several hours. Symptoms of the underlying disease predominate, accompanied by severe hypotension and shock. Gradually, this stage passes into the early oliguric phase. Both urea and creatinine levels are not yet high. As a result of kidney damage, hyponatremia, hyperkalemia and metabolic acidosis occur. Hyponatremia often contributes to water imbalance - overhydration with improper treatment and the formation of endogenous water as a result of more intense fat catabolism. Hyperkalemia corresponds to oliguria: increases depending on protein catabolism, infection of tissue injury and metabolic azidosis. Clinical manifestations of hyperkalemia are paresthesia, paresis, muscle weakness and paralysis. The most serious changes are in the heart: muffled heart sounds, bradycardia and characteristic ECG changes: peaked T-wave, disappearance of the P-wave, PR prolongation, decomposition and disappearance of the QRS, arrhythmia and asystole. Metabolic acidosis is most often asymptomatic, but requires correction of hyperkalemia.
II. Developed acute renal failure. As a result of progressive electrolyte imbalance and accumulation of uremic toxins, clinical symptoms of acute uremia appear. Extrarenal manifestations of acute uremia, consisting of cardiovascular, gastrointestinal, neurological and hematological disorders, complicate the clinical picture. In addition to diselectrolyte disorders, hypertension (usually associated with overhydration) and increased cardiac output (with severe anemia) have a negative effect on the heart, all of which often leads to heart failure. Disturbances from the gastrointestinal tract are observed especially often and sometimes manifest as alarming symptoms. These symptoms are nonspecific and often inexplicable, expressed by lack of appetite, nausea, vomiting, hiccups, diarrhea, constipation, stomatitis, reflux esophagitis. Gastrointestinal hemorrhages associated with the presence of erosions in the gastric mucosa, peptic ulcers or colitis are often observed. Numerous disorders are observed in the nervous system. One of the early symptoms is disorientation and slow reactions. Later, irritability, hyperreflexia and convulsions appear. Moderate anemia develops when hematuria lasts more than three days; the tendency to skin hemorrhages is associated with impaired platelet function. Infections in acute renal failure are most often the cause of mortality. Respiratory infections, which are favored by hypostasis and aspiration of vomit, are especially common. Urinary tract infections are common. The phagocytic system and antibody formation are affected, the immune reactions of cells are disrupted, and resistance to antibiotics occurs as a result of their uncontrolled use. Candida infections of the skin and mucous membranes and moniliasis sepsis often develop.
A particular problem is the non-oliguric form of acute renal failure. It occurs as often as the oliguric form in patients with non-traumatic rhabdomyolysis, sepsis and hypovolemia. For drug-induced renal failure, polyuria is more typical than oliguria. Non-oliguric renal failure is a milder type of oliguric renal failure. The level of diagnostic urinary indicators and coefficients is average between the indicators for oliguric renal failure and the indicators for prerenal azotemia: for example, the ratio of urinary and plasma osmolarity in the non-oliguric form is 1.1-1.5, and urinary sodium excretion is more than with prerenal azotemia, and less than in renal renal failure.