Despite the rapid development of medicine and pharmacy, chronic obstructive pulmonary disease remains an unsolved problem of modern healthcare.
The term COPD is the product of many years of work by experts in the field of diseases of the human respiratory system. Previously, diseases such as chronic obstructive bronchitis, simple chronic bronchitis and emphysema were considered in isolation.
According to WHO forecasts, by 2030 COPD will take third place in the structure of mortality worldwide. At the moment, at least 70 million people on the planet suffer from this disease. Until the proper level of measures to reduce active and passive smoking is achieved, the population will be at significant risk of this disease.
What it is?
COPD is considered a fairly serious disease of the bronchopulmonary system, which greatly impedes the natural function of a person’s breathing. Its development occurs due to long-term damage to the lungs, for example, from tobacco smoke. Most often, this disease is diagnosed in adult patients whose age has exceeded 40 years. Doctors say that COPD usually combines the features of two diseases:
- Chronic bronchitis. In this condition, the bronchi are in a state of permanent inflammation, which is accompanied by hyperkrinia (a term meaning increased mucus production). As a result, there is a thickening of the walls of the bronchi and a natural narrowing of the lumen of the airways (obstruction). This condition significantly complicates the breathing process.
- Emphysema. This disease is characterized by damage to the walls of the alveoli, as well as loss of elasticity. As a result of such pathogenic changes, the useful area of the lungs for the exchange of gases (saturation of the blood with oxygen and removal of carbon dioxide from it) is reduced. Due to insufficient oxygen supply to the bloodstream, shortness of breath develops, and it is perceived by the patient as a feeling of lack of air.
Sometimes the illness takes the form of one of these conditions. It is not possible to predict the course of the disease in advance.
COPD progresses over time, since today it is not possible to completely stop the processes of damage to lung tissue. Nevertheless, doctors are able to somewhat slow down the destruction of the alveoli, as well as improve the well-being of a patient with this diagnosis.
Diagnostics
The disease mainly affects people over 50 years of age who smoke or have previously smoked (smoking experience is more than 20 pack-years). COPD can be suspected by taking a medical history, but spirometry (a test of external respiratory function) is necessary to confirm the diagnosis. The main symptom is progressive shortness of breath. It is usually accompanied by a cough with sputum and attacks of suffocation. Cough, as a rule, either precedes shortness of breath or appears simultaneously with it. The sputum is pale gray in color and is coughed up in the morning, but may be coughed up during the day.
Perennial cough with sputum and mild shortness of breath are characteristic of the bronchitis type of COPD. In the emphysematous type of COPD, on the contrary, a rare cough with scant sputum and severe shortness of breath are bothersome. A change in the nature of sputum from mucous (pale gray) to purulent indicates the addition of an infection - acute bacterial bronchitis. Wheezing and asthma attacks are the result of bronchospasm or narrowing of the airways due to inflammation. COPD in close relatives means that the disease may be due to alpha-1 antitrypsin deficiency, especially if symptoms first appeared before age 50. Hemoptysis is usually caused by an acute bacterial infection (bronchitis or pneumonia), but lung cancer must be excluded. If the disease began with progressive shortness of breath against the background of bronchial asthma, especially in a non-smoker, chronic asthmatic bronchitis is likely.
With the bronchitis type of COPD there are usually no complaints at rest. Over time, hypoxemia (decreased oxygen levels in the blood) inevitably develops, which leads to changes in the heart (cor pulmonale) and heart failure (which manifests itself, in particular, as edema).
With COPD, especially severe ones, there may be complaints that are not directly related to damage to the respiratory system: fatigue, weight loss, loss of appetite. Sleep disturbances and mental disorders are also possible: depression, problems with concentration and memory.
Causes of the disease
Doctors are confident that the main reason for the development of COPD is the presence of nicotine addiction in a person. After all, constant inhalation of tobacco smoke for many years leads to irritation of the respiratory tract and destruction of elastic fibers in the alveoli of the lungs. Smoking is considered the main factor in the development of the disease in 80-90% of cases. In non-smoking patients, the disease may occur due to occupational hazards, in particular when working in the mining industry. Dusts containing cadmium and silicon are considered especially harmful to the lungs.
There are cases of COPD in people who do not have a nicotine addiction, as well as those who are far from hazardous industries. They probably develop the disease due to an unfortunate combination of several risk factors and a certain individual predisposition.
Risk factors
Your risk of developing COPD increases if you:
- Indoor air pollution, including due to the use of solid fuels for heating or cooking. Aggressors can be fumes from paint, cleaning products, aerosol cosmetics and perfumes.
- Living in areas with polluted air.
- The presence of dust and all kinds of chemicals in the workplace.
- Frequent diseases of the bronchopulmonary system in childhood.
- Passive smoking (especially in childhood).
- Post-adenoviral infection.
- Chronic bronchitis.
- Over 40 years of age and male.
- Lack of vitamin C.
- Birth before term (COPD is more often diagnosed with a history of prematurity). Also, a risk factor may be low birth weight and other factors that negatively affect lung growth during fetal development or in childhood.
- Low income level, when there is no opportunity to resort to effective methods of preventing COPD.
Doctors are confident that the development of COPD can be prevented in the vast majority of cases. Reducing the prevalence of smoking is an important step in preventing this disease.
Risks and groups of COPD
When developing the risk classification for COPD, we were based on conditions and indicators collected in large-scale clinical studies (TORCH, UPLIFT, ECLIPSE):
- a decrease in spirometric parameters is associated with the risk of death of the patient and the recurrence of exacerbations,
- hospital stay caused by an exacerbation is associated with poor prognosis and a high risk of death.
For different degrees of severity, the prognosis of the frequency of exacerbations was calculated based on the previous medical history. Table "Risks":
| GOLD 1-4 Severity | Frequency of exacerbations (per year) | Mortality within 3 years, % | Hospitalization (per year) |
| Lightweight | 0,5 | , | , |
| Moderate | 1 | 11 | 0,2 |
| Heavy | 1,5 | 15 | 0,3 |
| Extremely heavy | 2 | 24 | 0,5 |
There are 3 ways to assess the risk of exacerbation:
- Population - according to the classification of the severity of COPD based on spirometry data: with grades 3 and 4, high risk is determined.
- Personal history data: if in the past year there have been 2 or more exacerbations, then the risk of subsequent ones is considered high.
- The patient's medical history at the time of hospitalization, which was caused by an exacerbation in the previous year.
Next, an integral comprehensive approach to assessing COPD in each individual patient is carried out (see below).
Symptoms of chronic obstructive disease
COPD is characterized by a slow onset, the disease makes itself felt very gradually, so it can be difficult to identify it in a timely manner. The most common primary signs of the disease:
- Chronic cough. This symptom is essentially a defense mechanism. Its appearance is associated with exposure to an irritant, for example, cigarette smoke, mucus and phlegm. If coughing does not disappear within two months, it may well signal the development of COPD.
- Excessive mucus production. It is hypercrinia that is the second early sign of COPD. Our bronchi produce mucus to protect the respiratory system so that irritants and germs do not enter the lungs. In addition, it is necessary to maintain moisture in the respiratory tract. But if the bronchopulmonary system is constantly exposed to irritants, mucus synthesis increases.
- Dyspnea. This is a symptom in which a person feels a lack of oxygen. At first, this unpleasant sensation appears only after physical exertion, but over time it becomes more permanent and disrupts a person’s full activity.
The appearance of the described signs, even if they do not bother the person too much, should be considered as a reason for an unscheduled consultation with a doctor. To begin with, you can contact a therapist, but it is better, if possible, to immediately make an appointment with a pulmonologist.
Other symptoms of COPD include:
- A feeling of tightness in the sternum.
- More frequent acute respiratory infections and acute respiratory viral infections.
- Audible wheezing.
- Painful sensations in the sternum.
- The appearance of blood streaks in the sputum.
- Weight loss.
- Swelling of the legs.
COPD can occur with periods of almost complete well-being, followed by outbreaks of exacerbations and a sharp worsening of the symptoms of the disease. External irritants, as well as infectious agents, can provoke an exacerbation.
Laboratory and instrumental studies
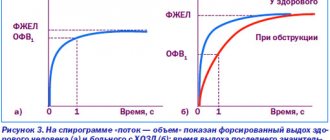
The only reliable criterion for COPD is disturbances detected during spirometry (a study of external respiratory function). Any changes in spirometric indicators, both for the better and for the worse, however, do not mean anything until they are confirmed by repeated studies. In bronchial asthma, unlike COPD, obstructive disorders are reversible.
The functional reserve of the lungs is assessed using stress tests with examination of the function of external respiration and gas exchange. In addition, stress tests make it possible to determine what causes poor exercise tolerance: impaired gas exchange or ventilation, or cardiovascular pathology. In patients with COPD, the limiting factor is often cardiovascular pathology.
If obstructive disorders are identified, spirometry is usually supplemented by determining sensitivity to bronchodilators: for this, the patient is given a few breaths through the inhaler and the study is repeated. However, the response to a single use of bronchodilators does not always reflect their effectiveness, and low sensitivity to bronchodilators during spirometry does not mean that their long-term use will not improve the patient's condition. Therefore, regardless of the response detected by spirometry, you should not refuse a trial of bronchodilator treatment.
A chest x-ray can help diagnose emphysema. Its most important symptom is overinflation of the lungs. Bullae may be detected in the upper lobes and focal increases in the transparency of the lung fields. X-rays only approximately characterize the severity of emphysema and are most informative in severe forms of the disease. Computed tomography (CT) is much more sensitive in detecting changes such as small bullae. However, neither radiography nor CT replaces the key diagnostic method - spirometry.
During the initial examination, sputum microscopy, a general blood test with determination of the leukocyte formula, electrocardiography (ECG) and often echocardiography (ultrasound examination of the heart) are also advisable. In addition, if alpha1-antitrypsin deficiency is suspected, its level in the serum is determined, and if chronic asthmatic bronchitis is suspected, skin tests with allergens are performed and the level of IgE in the serum is determined.
Classification
Regardless of the scenario in which COPD develops, doctors identify 4 or 5 main sequential stages of its progression. At first, when the disease has not yet manifested itself, they speak of pre-disease or zero stage. In this case, the person is at risk, exposed to prolonged exposure to pathogenic factors and already suffers from cough with sputum or shortness of breath. But lung function remains intact.
The development of the disease itself has 4 stages:
- First or easy.
- Second or medium (sometimes the term moderate is used).
- The third or heavy.
- The fourth or extremely severe.
The choice of the right treatment directly depends on the stage of the disease. With early diagnosis of the disease, there is a chance to stop the course of pathological processes and prolong the patient’s life for a long period.
Easy stage
At the first stage of development of the disease, the patient himself may not yet notice any symptoms of impaired pulmonary function. It is only possible to have a chronic cough and sputum production. Nevertheless, a correctly conducted examination allows you to make a diagnosis; by analyzing the external respiratory function (ERF), the doctor can detect a slight decrease in airway patency.
Average
At the second stage of development of the disease, the patient can independently pay attention to the presence of unpleasant symptoms of illness and seek medical help. The reason for a visit to the doctor is increased symptoms of shortness of breath, which begins to reduce the quality of life. A cough with sputum production is also usually observed. The FVD study shows:
- Decreased airway patency.
- Decreased forced expiratory volume (more than 50%, but less than 80% of normal).
If COPD is diagnosed at the middle stage of development, there is every chance to slow down its development. But it is most often possible to identify the disease only with a certain awareness of the patients.
Heavy
If COPD reaches the third stage of development, the patient’s life becomes much harder:
- Shortness of breath increases and interferes with even simple everyday activities. The patient even has to stop to rest during an ordinary walk. Of course, the ability for self-care, movement, and work activity decreases.
- The frequency of exacerbations of the disease, which require prolonged outpatient or inpatient treatment, is increasing. During an exacerbation, deterioration in well-being is recorded for at least two days in a row, which occurs suddenly and is accompanied by increased cough and shortness of breath, as well as an increase in the volume of sputum produced. During such a period, the patient needs special therapy.
- Right ventricular heart failure may develop.
Patients with stage 3 COPD may be assigned a second disability group.
Extremely heavy
At stage 4 COPD, exacerbations of the disease become life-threatening for the patient. The patient has:
- Extremely severe bronchial obstruction develops.
- Dyspnea is present at rest, increasing in the supine position.
- A condition called cor pulmonale occurs, in which the volume of the heart increases and the walls of the right ventricle stretch. This condition leads to pain in the chest, tachycardia, rapid breathing and bluish skin. Swelling of the arms and legs is observed.
In extremely severe cases of COPD, patients may need constant outside care, as well as systematic assistance from others. The first disability group can be established.
Symptom severity
For COPD typing, specially developed, valid questionnaire methods are used: MRC - “Medical Research Council Scale”; CAT, COPD Assessment Test, developed by the global initiative GOLD - COPD Assessment Test. Please mark the score from 0 to 4 that applies to you:
| M.R.C. | |
| 0 | I feel shortness of breath only during significant physical activity. load |
| 1 | I feel short of breath when accelerating, walking on level ground, or when ascending a hill |
| 2 | Because I feel short of breath when walking on a flat surface, I begin to walk slower compared to people of the same age, and if I walk at my usual pace on a flat surface, I feel my breathing stop. |
| 3 | When I cover a distance of about 100 m, I feel like I’m out of breath, or after a few minutes of calm walking |
| 4 | I can't leave my house because I feel short of breath or out of breath when getting dressed/undressed. |
Take the test and evaluate how your lung disease is progressing:
| SAT | ||||
| Example: I'm in a good mood | 0 1 2 3 4 5 | I am in a bad mood | Points | |
| I don't cough at all | 0 1 2 3 4 5 | Cough is constant | ||
| I don't feel any phlegm in my lungs at all. | 0 1 2 3 4 5 | I feel like my lungs are filled with phlegm | ||
| I don't feel any pressure in my chest | 0 1 2 3 4 5 | I feel very strong pressure in my chest | ||
| When I go up one flight of stairs or go up, I feel short of breath | 0 1 2 3 4 5 | When I walk up or climb one flight of stairs, I feel very short of breath | ||
| I do my housework calmly | 0 1 2 3 4 5 | I find it very difficult to do housework | ||
| I feel confident leaving the house despite my lung disease | 0 1 2 3 4 5 | Unable to confidently leave home due to lung disease | ||
| I have a restful and restful sleep | 0 1 2 3 4 5 | I can't sleep well because of my lung disease | ||
| I'm quite energetic | 0 1 2 3 4 5 | I'm out of energy | ||
| TOTAL SCORE | ||||
| 0 — 10 | The impact is negligible | |||
| 11 — 20 | Moderate | |||
| 21 — 30 | Strong | |||
| 31 — 40 | Very strong | |||
Test results: CAT≥10 or MRC≥2 scale values indicate significant severity of symptoms and are critical values. To assess the strength of clinical manifestations, one scale should be used, preferably CAT, because it allows you to most fully assess your health status. Unfortunately, Russian doctors rarely resort to questionnaires.
Clinical forms
When COPD develops to the third stage, doctors can determine 2 types of clinical picture of the disease:
- Emphysematous. In such patients, shortness of breath is more pronounced, and bronchial obstruction is not too obvious. Severe hyperventilation of the lungs is recorded. The emphysematous type of the disease is considered more favorable; cor pulmonale can develop only in old age.
- Bronchitic. With this variant of the disease, cough is the predominant symptom, and shortness of breath is not so pronounced. Severe bronchial obstruction and severe cyanosis are recorded. Cor pulmonale can develop at an early age and subsequently lead to death.
Identification of two clinical forms of COPD is necessary to obtain a preliminary prognosis for the further development of the disease. In some cases, the emphysematous and bronchitis types of the disease are combined.
Content
- 1 Preventive measures 1.1 Smoking control measures
- 1.2 Combating professional factors
- 2.1 Bronchodilators 2.1.1 β2-agonists
How is the diagnosis made?
When seeking medical help, a pulmonologist first of all carries out:
- Assessing the patient's appearance. Already an analysis of the patient’s behavior and the reactions of his respiratory system to the conversation allows us to draw certain conclusions regarding the diagnosis. In severe cases of COPD, the patient purses his lips into a “tube” and takes a forced position.
- Assessment of skin color. In particular, a grayish-blue tint to the skin indicates hypoxemia (insufficient oxygen in the blood), and the presence of acrocyanosis (blueness of the nasolabial triangle, fingers and toes, etc.) may indicate heart failure.
- Examination of the sternum. In severe COPD, the chest becomes deformed, inactive during breathing and significantly expanded in the lower sections. When breathing, active muscle tension occurs, as well as retraction of the lower intercostal spaces.
- Tapping the sternum. During such manipulation, the doctor may pay attention to the lowering of the lower borders of the lungs, as well as a boxy percussion sound.
- Listening to the lungs. Breathing may be harsh or weakened, accompanied by dry wheezing.
To make an accurate diagnosis of COPD, additional studies are required to determine the functioning of the bronchopulmonary system.
Instrumental diagnostics
To identify COPD, including in the early stages of development, the following can be performed:
- Study of the characteristics of external respiration. This diagnostic method helps to detect airflow limitation even in patients without shortness of breath, with the initial stage of the disease.
- Radiography. This diagnostic method mainly helps to exclude other diseases (for example, cancer or tuberculosis), as well as to identify complications in a timely manner.
- HRCT or high-expansion computed tomography. Such a study allows us to examine the exact structure of the lung tissue, as well as the characteristics of the condition of the small bronchi.
- ECG - electrocardiography. This diagnostic method allows timely replacement of the development of cor pulmonale.
- EchoCG - echocardiography. This test is necessary to detect pulmonary hypertension and other heart complications.
- Step test. This is what is called a stress test; it is the one that most often helps to identify disorders at the initial stage of COPD, when negative symptoms arise only during physical activity.
- Bronchoscopy, sometimes in combination with a biopsy of the bronchial mucosa. This analysis makes it possible to distinguish COPD from other possible ailments.
- Study of blood gas composition.
- Complete blood count (CBC), immunogram, coagulogram.
- Cytological and cultural examination of sputum.
The exact list of necessary studies to identify COPD is determined by a pulmonologist on an individual basis.
Treatment of COPD
Treatment of COPD is a long and consistent process under the supervision of doctors. Control is carried out during visits to the doctor or online consultations via Skype. The goal of a COPD treatment program is to reduce the number of exacerbations, improve respiratory function, and quickly cope with exacerbations.
Skype consultations
Online consultations save our patients time and effort. The patient sends tests and CT scans to the clinic. Then, at a pre-agreed hour, the pulmonologist who is treating you gets in touch via Skype. If during a consultation via Skype the doctor understands that an examination is required to correct treatment, then you will be invited to an appointment.
Calling a doctor to your home
For severe patients with COPD, the service Call a pulmonologist to your home is offered. Viktor Aleksandrovich Samoilenko consults at home, pulmonologist, candidate of medical sciences, nominee of the National Award for the best doctors of Russia “Calling”, student of the academician of the Russian Academy of Sciences, prof. Chuchalina A.G. During the on-site consultation, the doctor will adjust the treatment, change oxygen therapy regimens, and make new prescriptions.
Hospitalization
If it turns out that only a pulmonology hospital is required for treatment, then we will organize URGENT hospitalization in a pulmonology hospital. We will monitor the treatment together with our colleagues at the hospital.
"Day hospital"
In the “Day Hospital” we fight exacerbations of COPD with intravenous injections in combination with intensive nebulizer therapy. Two to three days of intensive treatment will lead to improved health. When breathing is restored, it will be possible to prescribe basic therapy.
How is it treated?
Unfortunately, it is not possible to completely restore the normal functioning of the bronchopulmonary system in COPD. Treatment is aimed at:
- Prevention of progression of the disease.
- Reducing the severity of unpleasant symptoms.
- Increased exercise tolerance.
- General improvement in quality of life.
- Prevention and treatment of complications.
- Prevention of exacerbations.
- Decrease in mortality rate.
Regardless of the stage of the disease, therapy should be exclusively comprehensive.
General recommendations
All patients with COPD first need to exclude the influence of aggressive factors on the respiratory system. Most often, quitting smoking becomes a mandatory step, since it is nicotine addiction that contributes to the development of the disease. But in addition, it is very important to try to reduce the amount of dust in your home and not go outside when there is an increased level of air pollution.
For successful treatment of COPD it is also worth:
- Avoid illnesses (infections can provoke an increase in negative symptoms): wash your hands, do not visit crowded places, get vaccinated against the flu if your doctor advises it, strengthen your immune system, etc.
- Develop healthy eating habits, in particular, organize a balanced menu that saturates the body with all the nutrients it needs, and also refuse frankly unhealthy foods.
- Organize regular physical activity as recommended by your doctor. Any training should be started gradually.
- Do breathing exercises.
Patients with COPD need to constantly communicate with their own doctor. In addition, they are recommended to attend support groups or a psychotherapist to prevent and eliminate depressive and anxiety conditions.
Since most often death in COPD occurs due to acute respiratory failure, blood oxygen saturation plays an important role in therapy. For this purpose, oxygen therapy is indicated for patients. Such procedures really help reduce the mortality rate; they are prescribed to patients with severe hypoxemia (based on blood gas studies).
Drug treatment
The basis of drug therapy for COPD is the use of bronchodilators. Such medications affect the tone of the bronchial muscles and are quite effective in eliminating obstruction. They can be used for inhalation therapy. The doctor may prescribe:
- Short acting bronchodilators. Such medications are the drugs of choice; they are used at intervals of 4-6 hours to reduce negative symptoms, as well as when the ability to perform physical activity is limited.
- Long-acting bronchodilators. Such medications can be combined with the previous group of medications if they do not provide sufficient effect.
In addition, drug therapy may include the use of:
- Mucolytics. Such medications help thin the mucus and facilitate its evacuation from the bronchi.
- Antibacterial drugs. They are used to correct exacerbations of the disease.
- Inhibitors of anti-inflammatory mediators or receptors for them. Such medications effectively suppress the inflammatory process. These include Erespal, Inspiron.
- Glucocorticosteroid hormones. Such medications are used during exacerbations of the disease to relieve attacks of the disease.
The names of drugs for the treatment of COPD and their dosage are selected by the attending physician, taking into account the individual characteristics of the patient; any attempts at self-medication can lead to complications and even contribute to the progression of the disease.
How to treat using folk remedies?
The advisability of using alternative medicine should also be determined by a qualified specialist. In particular, various herbs with expectorant properties, as well as compounds that strengthen the immune system, can be used to treat COPD. Let's look at a few effective recipes:
- 1 tbsp. l. coltsfoot brew 1 tbsp. boiling water Leave the product covered until it cools, then strain and drink 3 tbsp. l. at a time with an interval of 2 hours.
- 2 tbsp. l. Icelandic moss, brew 1 liter of boiling water. After 10 minutes, strain, cool slightly and sweeten with honey. Drink as a tea just before bed.
- Brew 10 grams of anise seeds with 1 tbsp. boiling water Leave covered to infuse and strain after cooling. Drink 50 ml 4 times. in a day.
- Brew 10 grams of plantain leaves with a glass of boiling water and cool under the lid. Strain the medicine and drink it 100 ml 4 times. for a day.
- Brew 40 grams of primrose flowers with 2 liters of water. Place the container on the fire and bring the product to a boil. Boil over low heat for 2 minutes, then cover with a lid and leave to cool completely. Strain the finished medicine and take 3 tbsp. l. three times a day.
Remember that all traditional medicines can cause individual intolerance reactions. In addition, there is a risk that their use may be negatively combined with the use of medications. Therefore, the possibility of treatment at home must be discussed with your doctor.
Surgery
Surgical treatment for COPD is mostly palliative in nature - improving the quality of life of patients. It may mean:
- Removal of large bullae in patients with bullous emphysema (if the bullae cause severe shortness of breath and hemoptysis or are sources of infection).
- Reduced lung volume. Such a need may arise with severe emphysema, but this operation is rarely performed.
In principle, a lung transplant is considered a possible treatment for COPD. It is performed when respiratory function is severely reduced. But in our country such intervention is still extremely rare.
LiveInternetLiveInternet
General Description Symptoms Traditional Treatments for COPD Lifestyle and Health Program Dietary Supplements Other Treatments for COPD General Description What is COPD? Chronic obstructive pulmonary disease (COPD) is a group of serious breathing disorders that includes chronic bronchitis, asthma and emphysema, or may be a combination of two or more of these diseases. It is a progressive, irreversible and debilitating lung disease that often begins with a morning cough containing mucus and, as the disease progresses, is accompanied by shortness of breath and difficulty breathing. It is the fourth leading cause of death in the United States (according to the Center for Disease Control) and affects more than 16 million Americans. The majority of deaths (3-5 million per year) are due to cardiovascular complications of COPD. Chronic asthma (recurrent bronchospasm) is often a reaction to infection, smoke, cold air, exercise, pollen or other irritants. Other triggers for COPD are environmental pollution, chemical fumes, including most household cleaners and aerosols, dust, mold, and, of course, active or passive smoking. Miners and people who handle grain are also susceptible to chronic bronchitis. Chronic bronchitis (persistent inflammation of the bronchi) is caused by a bacterial or viral infection. It is accompanied by a chronic cough that lasts at least two to three months and discharge of mucus. Chronic bronchitis affects 9 million Americans, and this number is growing rapidly. Emphysema occurs as a result of damage to the walls that separate the tiny air sacs (alveoli) in the lungs. As this process progresses, the lungs lose elasticity and become so weak that breathing becomes difficult. Smoking is the main cause of emphysema. In addition, researchers from Columbia University Medical Center (New York) concluded that COPD and, in particular, emphysema, are associated with ingestion of foods containing nitrites. Researchers have shown that there is a correlation of emphysema with eating 14 or more servings (100g serving) of canned meat per month. So if you have COPD, one of the lifestyle changes you need to make is to stop eating hot dogs, bacon and corned beef. Symptoms of COPD • Chest tightness • Cough with mucus • Shortness of breath that worsens even with light physical activity • Fatigue • Frequent respiratory infections • Heavy breathing COPD is accompanied by shortness of breath not only when climbing stairs, but also during light exercise and even when walking around the room. In severe cases, the patient has great difficulty performing normal breathing. In addition, COPD can cause coughing, wheezing and chest tightness, and difficulty breathing. A team of researchers at the University of Virginia led by Dr. Benjamin Gaston found that asthma attacks can cause high levels of acidity in the lungs. Additional research has shown that the acid-base balance of a person with COPD is affected by difficulty breathing, which causes carbon dioxide (CO2), which is acidic, to build up and can rise to levels that make COPD worse. Carbon dioxide must be eliminated to maintain the body's proper pH, so the respiratory system responds to increased acidity (decreased pH) by increasing the rate and depth of breathing. The use of steroid medications helps return the pH level to normal, but steroids cannot be used long-term due to side effects, one of which is bone loss (osteoporosis). In this case, the problem can be managed using lifestyle changes and nutritional supplements, which can help stop the condition from getting worse. As part of the health program outlined below, you need to adhere to a certain diet and monitor your body's pH, for which you should buy a set of litmus indicator strips to measure urine pH (the lower the pH, the higher the acidity). Although there is no known effective treatment for COPD, lifestyle changes and nutritional supplements can be used to slow and, in some cases, partially reverse the progression of the disease. If you were recently diagnosed with COPD and started a wellness program right away, your long-term results will be much better. Below, we'll give you information about some COPD treatments you can try and a list of supplements you can take as part of your wellness program. Traditional Treatments for COPD Bronchodilators are typically the first line of defense used in medical practice. Albuterol (Proventil) is one of the most common drugs, but there are others. It is used orally and also as an inhalation dosage form. In a striking study published in the Journal of the American Medical Association, the authors concluded that medications used to treat COPD make a significant contribution to mortality from the disease. It reports on inhaled anticholinergic drugs and indicates that they lead to an increased risk of heart attacks by more than 50%, as well as an increased risk of death from cardiovascular events by more than 80%. This data is so overwhelming that if you are using one of these drugs, work closely with your doctor. Steroids can be an effective way to combat pneumonia, but they cannot be used long-term as they often have side effects - osteoporosis, stomach irritation, cataracts, bruising. For this reason, they are only intended for those who have an acute breathing problem and should only be used for a short time. Antibiotics are used when there are infections. Overuse of antibiotics can lead to other diseases, and their effectiveness decreases over time (addiction). If you are using antibiotics, be sure to also take probiotics during your antibiotic course and for a week or more afterwards to help rebuild your gut flora afterwards. Lifestyle and Wellness Program A multi-pronged approach is likely the best way to combat COPD. You can act haphazardly, taking a drug or supplement as needed, but in the long run, changing your lifestyle and diet, as well as using proper breathing techniques, relaxation techniques along with moderate exercise and taking nutritional supplements will lead to much more beneficial results. Try to understand the underlying causes of the disease, not limiting yourself to fighting the symptoms. Lifestyle changes • Stop smoking! If you smoke or are around people who smoke, stop smoking and stay away from tobacco smoke. Your recovery starts here. • Avoid scented candles and personal care products (cosmetics, perfumes, soaps, deodorants, etc.) • Do not drive during rush hour when the level of exhaust gases in the environment increases sharply • Avoid all types of aerosols and sources of strong odors. They will irritate your bronchi and aggravate your condition. These same irritants include almost all cleaning products used in your home. Use natural, non-spray products instead. You can use baking soda or vinegar. • If you have dry-cleaned clothes, air them well before putting them in the closet, otherwise you may experience headaches or other allergic reactions. • If you live in an area with high air pollution, limit your time outdoors. • Avoid people with colds, as people with COPD are much more susceptible to infection and can catch colds easily. Rhinoviruses, one of the leading causes of colds, are known to increase complications from COPD and can lead to pneumonia, a leading cause of death for people with chronic obstructive pulmonary disease. You should know that if you start coughing with greenish, yellowish or brownish sputum, then it is a bacterial infection and you should consult a doctor immediately. The cornerstone of a wellness program is strengthening your immune system. More on this later. • Eat small portions of food for several meals a day. Overloading the stomach causes pressure on the diaphragm, which leads to breathing discomfort. • If you have mold in your home or workplace, remove it or change its location. Mold is one of the main triggers of COPD symptoms. • If you have fan equipment and air ducts in your home, clean them at least once a year to remove dust. Consider installing a filter to clean the system of pollen, dust, mold and other particles. • Keep indoor humidity at an optimal level of 30-55%. You can buy a device to monitor the humidity level, and if it is too high, use a dehumidifier, and if it is too low, use a humidifier. • Buy a negative ion generator. The air will be purified by adding negative ions to it, which attract positively charged microparticles of dust, fur and other irritants. This device will be especially important when your house or apartment is tightly closed and not ventilated. Diet Changes A good diet for lung disease should include fruits, vegetables, juices, high-fiber foods, fats high in omega-3 fatty acids (olive oil and flaxseed oil), fish and chicken. This diet is rich in natural anti-inflammatory substances and antioxidants, and will not overload the digestive system. One study found an inverse relationship between vegetable consumption and the occurrence of chronic bronchitis. Avoid acidic foods if you want to keep your body's pH alkaline as a way to reduce processes that can trigger a flare-up of COPD symptoms. Although, as a rule, fruits are acidic (pH <7), the reaction in the body matters, and fruits are useful in this regard, since they produce a mainly alkaline pH value in the body >7. Buy a set of litmus test strips and monitor your body's acidity by measuring your urine pH with the strips. Build a graph of pH changes depending on the time of day and date, noting any exacerbation of your condition on it. Mark points on it before and after the attack, record what you ate and drank before the attack, and see if there is a connection between these data. Many foods and lifestyle choices can trigger an attack, so you need to learn to control the situation. If your pH is low, use dietary supplements that reduce body acidity (increase pH). Monitoring your pH should be part of your daily routine, especially if you have a chronic health condition. Stop eating processed meats: hot dogs, bacon, corned beef, packaged lunches. They are prepared with nitrites, which cause an increased risk of developing COPD. Other dietary factors also contribute to this, such as a lack of vitamin C and other antioxidants. A 2007 study published in the American Journal of Epidemiology found that a high-fiber diet was very helpful in reducing the risk of COPD. Study participants who were in the group that ate any high-fiber foods had a 15% reduction in their risk of COPD, while other participants who got their fiber primarily from fruits had a 38% reduction in their risk of COPD. This result is very important, as it once again shows how important nutritional composition is for your health. Make increasing your fiber intake part of your wellness program. A study done at Johns Hopkins School of Medicine reports the need for antioxidant protection for those suffering from emphysema. A substance called sulforaphane, which is found in cruciferous vegetables such as bok choy, broccoli, Brussels sprouts, cabbage, cauliflower, kale and wasabi (Japanese horseradish), has been found to be very effective in providing this protection. The largest amount of sulforaphane is found in broccoli. This compound appears to help protect the lungs from inflammatory damage, especially in smokers. Also take advantage of the antioxidants found in colorful fruits and vegetables, such as tomatoes, peppers, carrots, etc. You can also take carotenoid supplements—lycopene, lutein, and beta-carotene—as well as bioflavonoids. Avoid the following: • Aspartame and other artificial sweeteners (found in sodas) • Dairy products – eliminate all dairy • Fast foods (use a lot of omega-6 fatty acids from soybean oil) • Meats • MSG and all additives containing MSG • Oils containing omega-6 fatty acids (canola, corn, peanut, sunflower, soy). Most omega-6 oils tend to increase inflammation. • Processed meats • Saturated fats • Snacks, cookies, crackers (soybean oil) • Soda (very acidic) • Soy proteins • Wheat - eliminate all wheat products Breathing Techniques One of the most important things you can do to mitigate COPD , is to learn healthy breathing techniques that will strengthen your lung function and keep your pH within the proper acid-base balance. Most people breathe incorrectly, and if you learn how to do this, you can significantly improve your health. Proper breathing will help maintain proper balance in the lungs between oxygen and carbon dioxide. Lack of this balance results in decreased alkalinity, which can aggravate your condition. Talk to your doctor, who can help you find the breathing system that's right for you. Long-term research shows that there are many useful respiratory systems around the world. The Chinese have long used breathing techniques to treat many diseases, and various breathing methods are also used in yoga and meditation. Exercise It may seem counterintuitive to exercise when you have breathing problems, but one study published in the journal Circulation in 2001 found, “A six-month endurance exercise program was associated with recovery of lung function after thirty years of pulmonary disease.” . Just don’t overdo it and always check the air condition for the absence of irritants in the place where you are going to exercise. Work with your doctor to choose an exercise program that's right for you. Nutritional Supplements A comprehensive nutritional program will usually stop the progression of the disease and may even partially reverse it. Typically, such a wellness program aims to increase antioxidant processes, reduce inflammation, and stimulate the immune system to protect against infections. Below is a list of nutrients that work in these three areas: • Antioxidants - important protection for the lungs • CoQ-10 - coenzyme Q10 • Glutathione - one of the most powerful antioxidants (walnuts, tomatoes) • Green tea • Resveratrol • Vitamin A • Vitamin C • Vitamin E (mixture of tocopherols) • Anti-inflammatories - reducing inflammation in the lungs and bronchi, are absolutely essential for the fight against COPD • Borage oil • bromline • Curcumin • NAC (N-acetyl-L-cysteine) • Omega-3 fatty acids acids • Quercetin • Vitamin D-3 • Immune system stimulants – to reduce the risk of infection. They are especially important for people with chronic COPD, as infection can lead to pneumonia, which is a leading cause of death. • AHCC (see below) • Maitake (D-fraction of the product) • Beta-carotene - 300 mg per day AHCC, developed in Japan in 1984 from components extracted from several species of mushrooms, has been successfully used to treat a wide range of diseases - from minor ones like colds and flu, to serious ones like cancer, hepatitis, diabetes and cardiovascular disease. It is currently the most studied dietary supplement in the world to support the immune system (over 80 studies). AHCC is a very effective immunomodulator, used in more than 700 clinics as a standard preventive agent for all incoming patients, in order to reduce the risk of nosocomial infections. Coherent (coenzyme) Q-10, better known as COQ-10, is an excellent antioxidant and anti-inflammatory agent, increases energy at the cellular level, and also helps to fight infection. This additive is especially important if you take any drugs of statins class, since they destroy COQ-10, reducing its level in the body. Dosage: 50 mg twice a day. Kurkumin, the component of turmeric, which gives it the yellow color, as shown in several studies, reduces the inflammation of the respiratory tract and protects against the progression of lung cancer. Since many patients with COPD were avid smokers, this additive can benefit them in two directions - a decrease in respiratory tract inflammation and suppression of infection in mucus. Helping to reduce inflammation, curcumin facilitates the respiratory process, and helping to reduce the infection, reduces the threat of pneumonia, which is one of the main causes of death in patients with COPD. In this regard, turmeric is strongly recommended to include it in a healing program, especially if you often pick up infections. Enzymes. Enzyme failure leads to many health disorders, including acute and chronic bronchitis, asthma, inflammation and food allergies, that is, to such painful conditions that are part of the general disease of COPD. Enzymes regulate all chemical reactions in the body, and if they are not enough, then these reactions necessary for the body weaken and the risk of COPD increases. Correction of the deficiency of enzymes helps digestion and assimilation of nutrients, bringing the functioning of the body into dynamic balance. Flaxseed oil - 1.5 tablespoons per day to improve the surface properties of all cells. Flue oil is a good source of omega-3 fatty acids. Glutathione. It was established that healthy people have a high concentration of glutathione, but people with COPD do not have enough. How to eliminate this shortage? Jonathan V. Wright, Doctor of Medical Sciences, uses Glutation in his practice as an inhalation remedy for the treatment of COPD. Glutation is the most effective remedy against free radicals in the respiratory tract, which is confirmed by dozens of studies. It significantly improves breathing. Dr. Wright recommends 120-200 mg twice a day, but other doctors use 300 mg twice a day. This inhalation agent should be prepared by a pharmacist by compounding components according to a doctor's prescription. Iodine can greatly help with COPD. He penetrates the mucus well, facilitating its conclusion and helping to fight infections. Before use, consult a doctor. Lecithin - 1.5 tablespoons along with vitamin E and linseed oil, to improve the surface properties of all cells. L-carnitine-as shown, provides significant assistance to patients with COPD. 2000 mg twice a day. Lycopine - 15 mg twice a day. Magnesium - helps to relax and expand the smooth shell bronchiol (small bronchi). Dr. Wright recommends taking 300-400 mg of magnesium citrate daily. You can try to increase the reception to 400-500 mg twice a day. Magnesium can cause diarrhea, so you will have to make appropriate adjustments. Metake D-fraction is a powerful immune amplifier obtained from the mushroom of Matake. This is one of the most recommended immunity amplifiers. NAC (n-acetyl-l-cysteine). Jonathan Wright recommends taking this supplement 500 mg three times a day to liquefy dense bronchial secretions. He also recommends taking 30 mg of zinc picolinate and 2 mg of sebacath copper if you take NAC for more than a few months, and zinc, copper and NAC should be taken separately, since they are associated with each other and are excreted from the body. It should be emphasized that the NAC antioxidant reduces inflammation in the respiratory tract, is the precursor of glutation and is used against chronic bronchitis for almost 40 years. Quercetin is a flavonoid, has a wonderful property of restraining the reproduction of rhinoviruses that cause inflammation in the respiratory tract, a very important factor of respiratory normalization. In addition, it is a powerful antioxidant. With these two properties, querecetin should be part of your health program. Vitamin A is recommended 50,000 IU per day to maintain the health of bronchial tubes cells. It is very important to take vitamin A during periods of exacerbations of COPD due to the fact that it catalyzes the removal of the most active forms of oxygen radicals. Vitamin S. Researchers from the University of Nottingham in the UK found that those who consume large amounts of vitamin C or consume food rich in vitamin C and magnesium were much better than lung functions. You can start with 1 g per day and gradually increase until you notice intestinal discomfort. The optimal level of consumption can reach 10 g per day. Vitamin D3. Dr. Wright recommends 5000-10000 IU daily. People with COPD are often a deficiency of vitamin D. In 2011, at the International Conference of the American Breast Society, a presentation was held regarding the use of high doses of vitamin D to help people with hobble. It was about the results of the study, in which one group of participants gave increased doses of vitamin D3 within three months. It was found that the ability to physical activity and the strength of the respiratory muscles showed a significant increase when vitamin D3 was added to the pulmonary rehabilitation program. Vitamin E in the amount of 400-600 IU (mixed tocopherols) was used to improve the surface properties of all cells. The study of the University of Cornell showed that high consumption of vitamin E reduces the risk of COPD in women (there were no men in this study). Other means of treatment with COPD Galotherapy, also known as saline therapy or speleotherapy, uses dry microaerosol salt fog that inhales the patient. This therapy was first developed in the mid -18th century in Poland, when doctors noticed that workers in salt mines do not have lung diseases. As a result, salt hospitals began to quickly arise throughout Eastern Europe. Galotherapy has turned into a successful treatment for asthma, chronic bronchitis and all diseases of the upper and lower respiratory tract. This is an important way to treat respiratory diseases in pregnant women, since it has no side effects and it can be used without harm to the unborn child. Clinical studies have shown that salt therapy is bactericidal and anti -inflammatory properties, as a result of which the mucous membrane of the respiratory passage disappears and they expand, restoring normal mucus transportation and pure bronchi. To use the speleotherapy, you need to come to one of the salt caves of Europe, which are adapted for this type of treatment. Since it is inconvenient and expensive, it is better to use salt chambers that are in almost every city. Treatment of hydrogen peroxide and ozone therapy are two forms of oxygen therapy that are not recognized by most doctors, but work well in many cases. Ozonotherapy, for example, was developed in Germany more than 100 years ago and is successfully used to treat many diseases. Intravenous use of hydrogen peroxide (H2O2) for the treatment of asthma and other forms of COPD has many times described in the literature on natural medicine. In particular, two doctors - Doctor of Medical Sciences William Campbell Douglas and Dr. Richard Shulce, described the use of hydrogen peroxide for the treatment of asthma, bronchitis and lung emphysemes with remarkable results. Potisial insulin therapy, known by reduction of IPT, is a very interesting and powerful type of treatment with COPD. If almost any drug is administered into the body along with insulin, the effect of the drug increases significantly. This type of treatment was developed back in the early 1920s, Dr. Donato Perez Garcia. It was used to treat many diseases, but primarily as an auxiliary tool for chemotherapy. In addition, this method was successfully treated with diseases associated with COPD - asthma, allergic bronchitis, pulmonary emphysema and many others. Magnetic molecular activator (MME) is another type of therapy that was used with great success in patients with COPD. This is a safe, painless and non -invasive method of treatment. Its essence is reduced to the acceleration of normal chemical reactions in the body, which provide, inter alia, oxygen throughput, the absorption of nutrients, removal of metabolism waste, reduce the number of free radicals, tissue regeneration and healing. This technology, acting on biochemical and electromagnetic processes in the body, enhances its ability to self -healing. Experience has shown that for significant improvements to the condition of patients, about 100 procedures are required. Unfortunately, in the USA there are only a few clinics that offer this type of treatment at present. Information about these clinics can be obtained on the website www.amri-intl.com/clinics.html. Oxygen therapy. Most people with COPD do not need additional oxygen, but if testing shows that your oxygen level is too low, oxygen therapy can prevent excessive heart load. Traditional oxygen therapy uses a cylinder with oxygen and plastic tubes that are inserted into the nose. This method works well, but greatly limits your mobility. You can track your level of oxygen by buying a device for its measurement (Finger Meter), which determines not only the oxygen content in the blood, but also the heart rate. Note: Remember that a significant improvement in the state of your health will take a lot of time - from several weeks to several months. Therefore, be patient and persistently use your chosen remedies of COPD and a healing program, then success will come. Source in English: https://www.health911.com/copd on the main page ...
Lifespan
Today, COPD has a poor prognosis, since no treatment methods can cure it completely. The disease is constantly progressing, but adequate correction significantly slows down its development, including helping to achieve stable remission for several years. Life expectancy directly depends on the stage of the disease:
- At the first stage, the disease slightly worsens the health of the bronchopulmonary system. Therefore, timely diagnosis of the disease, a complete change in habits and adequate therapy allows you to maintain a normal life expectancy.
- In the second stage of the disease, lung function decreases, but sometimes the disease progresses quite favorably. Life expectancy is quite difficult to predict; on average, it exceeds 10 years.
- The third stage of COPD does not have such a favorable prognosis. The average lifespan of patients with this diagnosis is eight years or less. If the disease often worsens or is accompanied by complications, the risk of death increases.
- At the fourth stage of the disease, the prognosis is quite unfavorable. In approximately half of patients with this diagnosis, life expectancy does not exceed six months.
Prevention of influenza and pneumococcal pneumonia
Because pulmonary infection is common in patients with COPD and can lead to deterioration of lung function and respiratory failure, annual influenza vaccination is recommended for patients who are not allergic to egg whites. Its effectiveness reaches 60-80%. Unvaccinated patients at high risk of influenza A and at an early stage are prescribed amantadine. For patients over 50 years of age, a single immunization with the pneumococcal vaccine is also recommended. Revaccination is now carried out after five or more years, if at the time of vaccination the patient’s age did not exceed 65 years.
Complications
Doctors include the development of possible complications of COPD:
- Pulmonary heart.
- Recurrent pneumonia (against the background of obstructive pulmonary disease, inflammation is especially severe and difficult to treat).
- Depression.
- Pneumothorax.
- Respiratory failure.
- Anemia.
- Polycythemia.
The progressive development of COPD clearly changes the daily activities of patients and reduces their quality of life. The addition of complications makes the prognosis for the patient less favorable.
Modern medicines
Drug therapy is prescribed individually for each patient, depending on the individual characteristics of the body and the stage of development of the disease. For the treatment of chronic obstruction, the following groups of medications are prescribed:
- bronchodilators – help increase the bronchial lumen;
- glucocorticosteroids – fight inflammation;
- mucolytics – help thin sputum;
- methylxanthines – relieve spasms and have an anti-inflammatory effect;
- antibiotics;
- combined means.
The selection of drugs for the treatment of COPD can only be carried out by the attending physician.
Prevention
Specific prevention of COPD consists in eliminating the negative influence of those factors that can cause the development of this disease. To avoid illness, you must:
- Stop smoking.
- Avoid breathing polluted air both at work and at home. To do this, you can use special filters (including for individual use) or completely change your place of work or residence.
Doctors and scientists are confident that COPD is most often preventable. The development of this formidable and irreversible disease in most cases is only a consequence of many years of bad habits.
Types of antibiotics for COPD
Groups of antibiotics and drugs used for inflammation are shown in Table 1.
Table 1. Pharmacological groups of antibiotics and corresponding drugs used for exacerbations of COPD.
| Pharmacological group | Drugs |
| Penicillins | Amoxicillin, Amoxiclav (amoxicillin/clavulanate), |
| Cephalosporins | Cefixime, Cefuroxime |
| Macrolides | Azithromycin, Clarithromycin |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin, Moxifloxacin |
How and how much to take antibiotics
The dosage and duration of use depend on the drug used and the dynamics of the inflammatory process. Average data for adults are presented in Table 3.
Table 3. Regimen for taking oral antibiotics (in tablets) for exacerbation of COPD.
| A drug | Dosage per day | Time of receipt |
| Amoxicillin | up to 1 g x 3 | not related to food intake |
| Amoxiclav | 625 mg x 3 | at breakfast, lunch and dinner |
| Clarithromycin | 500 mg x 2 | not related to food intake |
| Levofloxacin | 500 mg at a time | in the morning, not related to food intake |
| Moxifloxacin | 400 mg at a time |