Congenital cataract is a disease that causes clouding of the eye lens. In most cases, congenital childhood cataracts occur in newborns.
However, there are cases that this kind of pathology does not manifest itself immediately. Therefore, confirmation of the diagnosis occurs after a certain period of time after a detailed examination of the eyeballs. This disease can be either bilateral or unilateral, that is, it can affect 1 or 2 eyes at once.
[toc]
Congenital cataract (photo)
Basically, congenital ophthalmological pathology is detected in infancy, that is, during the first years of the baby’s life. However, sometimes this disease may not manifest itself for a long period of time, so in medical practice the phenomenon of congenital cataracts in adults is often observed.
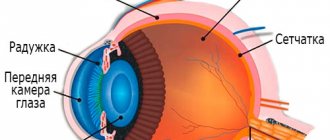
In a healthy baby, the lens looks like a transparent biconvex lens. There is no blood supply, and nutrients enter it through the watery structure of the eyeball.
In the event that a violation of the structure of the protein fibers of the lens occurs as a result of the influence of certain factors. This organ begins to lose its transparency, resulting in clouding.
Causes and symptoms
Diagnosing congenital cataracts remains difficult due to the fact that usually the disease, in the first stages of development, is detected only by patient complaints. And yet, there are several symptoms that help determine the presence of congenital cataracts in a child.
These symptoms include:
partial (very rarely - complete) clouding of the pupil, the presence of lighter dots or discs on it; strabismus or pathological rhythmic trembling of the eyeball; upon reaching the age of two months, the baby does not fixate his gaze on the faces of his parents or on toys; when examining various objects, the child turns to them with only one eye (the symptom will be absent in the case of bilateral congenital cataracts).
There are few reasons for the development of congenital cataracts, these include:
infectious diseases of the mother in the first trimester of pregnancy, in particular toxoplasmosis, rubella, herpes; maternal diabetes; metabolic disorders in the child’s body; pathological metabolic disorders in the mother’s body during pregnancy.
Symptoms
Normally, all newborns have very poor vision. They see only blurry outlines of surrounding objects and, moreover, are painfully tolerant of bright light. In addition, young children have physiological farsightedness, which can reach +6 diopters. This means that they have difficulty distinguishing objects located close to them. All this greatly interferes with the diagnosis of cataracts.
As a rule, the first symptoms of the disease in a child are detected at the age of 2-6 months. With massive clouding of the lens, the baby cannot fix his gaze on the faces of loved ones, bright toys or other objects. His eyes may wander aimlessly and not “catch on” to anything.
Other symptoms that may indicate congenital cataracts include:
- nystagmus - chaotic involuntary movements of the eyeballs in the left-right or up-down direction;
- the appearance of white spots in the pupil area, which can be noticed upon careful examination;
- strabismus is a pathological deviation of one or both eyeballs from its normal axis;
- decreased visual acuity, which can be detected at an older age using special tests.
With unilateral cataracts, the child fixes his gaze on objects with only one eye. The second one at this time may move chaotically or deviate in the other direction. Naturally, such a phenomenon should alert parents and force them to see a doctor.
Types of congenital cataracts
Congenital cataracts come in different types, each of which has individual disorders in the lens tissue, causes and associated diseases.
There are the following main types of congenital cataracts:
capsular; polar; layered; nuclear; full; complicated.
Capsular congenital cataract is an isolated lesion of the anterior or posterior capsule of the lens. Depending on the area and intensity of the clouding, vision may be slightly blurred or completely absent. The reasons for the development of this type of cataract may be metabolic disorders in the maternal body or intrauterine inflammatory processes (of bacterial or viral origin).
Polar congenital cataract is a lesion of not only the anterior or posterior capsule, but also the adjacent surface of the lens. In most cases, this disease develops bilaterally. The quality of vision directly depends on the strength and area of the clouding.
Layered congenital cataract is a clouding in the central part of the lens. This type of cataract is the most common. The danger is that in the vast majority of cases the disease develops bilaterally and almost completely deprives vision.
Nuclear congenital cataracts always develop simultaneously in both eyes, and the cause is heredity. Metabolic processes in the nuclei of lens cells change greatly, as a result of which transparency is lost almost completely. This type of cataract can deteriorate vision to 0.1 or even completely deprive a person of vision.
Complete congenital cataract - this disease develops in both eyes at the same time, and the degree of opacification is so great that in most cases children are born blind, they have only light perception. A distinctive feature of this type of cataract is that it is accompanied by other ophthalmological diseases, such as strabismus, microphthalmos, choroidal colombus, nystagmoma, macular hypoplasia, etc.
Complicated congenital cataracts can develop as a result of infection of the mother and fetus with viral and bacterial diseases in the first trimester of pregnancy. This disease always develops bilaterally and is almost always accompanied by other diseases. A distinctive feature is that concomitant diseases are not always of an ophthalmological nature - these can be not only damage to the eyes, but also to the hearing aid, speech apparatus, nervous system and various heart defects.
Congenital cataracts (Part 2) | Guide to Pediatric Ophthalmology
Description
There are a large number of other forms of congenital cataracts with partial, limited opacities, which usually do not affect visual acuity (or do not significantly reduce it); they are usually detected during routine examinations.
These cataracts include coronary (coronary), characterized by numerous limited opacities, greenish-bluish in color, which are located in the middle and deep layers along the periphery of the lens like a wreath.
With anterior axial embryonic cataract, there is opacification of the lens near its anteroposterior axis in the region of the anterior upsilon-shaped suture of the embryonic nucleus. Suture star cataract is characterized by opacification in the area of the anterior or posterior sutures of the lens.
Multiple very small opacities of a grayish-blue color, diffusely scattered in the region of the embryonic nucleus, are observed with punctate cataracts. Nuclear powder cataract is characterized by diffuse opacification of the embryonic nucleus, consisting of dust-like elements.
Congenital cataracts are relatively rarely an isolated lesion of the lens; they are often combined with other pathological changes in the organ of vision, as well as other organs and systems of the child’s body. Various defects of the organ of vision are observed in 36.8 - 77.3% of children with congenital cataracts: strabismus, nystagmus, microphthalmos, microcorneal pathology of the cornea, vitreous body, retina and optic nerve.
Strabismus is observed in a large number of children (up to 83%) with congenital cataracts. In some cases, it can be a complication of cataracts, a consequence of a sharp decrease in vision and profound disturbances in the sensory-motor connections of the visual analyzer. In others, strabismus is a congenital pathology accompanying cataracts. Strabismus with congenital cataracts is often converging, alternating, and predominantly permanent. The angle of deviation of the eye varies from 5 to 60%, more often it is 15 - 20°.
Nystagmus observed in children with congenital cataracts can be congenital or acquired, associated with a sharp decrease in vision. Pendulum-like and mixed type nystagmus is more common, jerk-like is less common, it is predominantly horizontal, small-caliber. Most often, nystagmus is observed with complete, membranous cataracts, combined with other defects of the visual organ, such as microphthalmos, microcornea, etc. Microphthalmos, characterized by a decrease in the size of the eyeball and functional inferiority of the visual organ, is observed in children with congenital cataracts.
The causes of congenital microphthalmia can be hereditary genetic factors, as well as intrauterine inflammatory and degenerative processes that retard the growth of the eyeball. The degree of reduction of the eye varies. With microphthalmia, other malformations of the eye may be observed: colobomas of the vascular tract and optic nerve, macular aplasia, etc.
Microcornea or small cornea, in most cases is noted with microphthalmia, but can also occur independently. With congenital cataracts, other corneal anomalies may be observed: opacities, dermoid cysts, megalocornea.
Congenital cataracts are often combined with various changes in the vitreous body, in particular with its opacities of varying severity - from small to severe fibrous. A common finding is the remains of an incompletely reduced vitreous artery.
Anomalies of the choroid in congenital cataracts are colobomas of the iris and choroid, polycoria, and pupil displacement. Hypoplasia and aplasia of the dilator, hypoplasia of the iris are often observed. Less common are irises and corneas, the manifestations of which are posterior embryotoxon, hyaline films and thickenings on the posterior surface of the cornea, and peripheral anterior adhesions.
Fundus changes detected after removal of congenital cataracts include partial atrophy of the optic nerve, myelin fibers, chorioretinal lesions, macular hypoplasia, retinal dystrophy, pigment redistribution, etc.
Obscuration amblyopia, or more precisely, underdevelopment of the visual analyzer as a result of the absence of a light stimulus to the retina, is a severe complication of congenital lens opacities, which is the most common cause of low visual acuity after cataract removal and the discrepancy between the functional results and the optical effect of the operation.
The most severe obscurational amblyopia develops with complete (diffuse) lens opacities. In order to prevent damage to the visual analyzer, a method has been proposed that consists of permanent dilation of the pupils with the help of mydriatics and subsequent irritation of the eyes with light stimuli. These manipulations should be performed in the first 6 months of life, if surgery (cataract extraction) has not been performed by this time.
Treatment
. Treatment of congenital cataracts is surgical. Most authors recommend removing congenital cataracts when visual acuity is below 0.3. After cataract extraction, correction of aphakia, pleoptic and, if indicated, ortopic treatment are carried out, measures aimed at eliminating strabismus, and treating nystagmus.
The question of the timing of removal of congenital cataracts is decided individually based on the clinical form of the cataract, residual visual acuity, etiology of the cataract, and the general condition of the child. Due to the danger of obscuration (deprivation) amblyopia with long-term existence of congenital cataracts, as well as the need to increase visual acuity, in order for the child to develop, it is advisable to perform the operation in the early stages.
According to most authors who have studied changes in the visual analyzer under conditions of deprivation, the sensitive period of vision development occurs in the period from the 2nd to the 6th month of a child’s life. In this regard, this age is optimal for the removal of congenital cataracts in children if there are indications for early surgery.
Early surgery is indicated for:
- complete, half-resolved, membranous cataracts;
- zonular, central, atypical cataracts with an opacity diameter of more than 3 mm, when retinoscopy cannot be performed under conditions of mydriasis;
- the presence of a rigid pupil in all forms of congenital cataracts due to the fact that in these cases it is impossible to achieve mydriasis necessary for preoperative measures to prevent amblyopia and retinal underdevelopment;
- the appearance of nystagmus in any form of cataract, which indicates a violation of the development of the oculomotor reflex.
Early surgery is not indicated for zonular cataracts with a disk of opacification less than 3 mm, in which retinoscopy can be performed due to the presence in these cases, as a rule, of relatively high residual visual acuity and the absence of the risk of developing severe amblyopia.
In such patients, surgery can be performed at a later period. It should be borne in mind that with congenital cataracts, the development of which is associated with intrauterine infection (rubella, etc.), complications (iridocyclitis) may occur after early surgery.
Unilateral congenital cataracts should be removed at almost the same time as bilateral ones. For any form of cataract, surgery should be postponed in cases where there are general contraindications to surgery and anesthesia (acute infections, chronic diseases in the acute stage and decompensation, the presence of foci of focal infection, allergic status, enlarged thymus gland, etc.).
The operation in these cases is carried out after treatment with the permission of the relevant specialists. For cataracts, the origin of which is associated with hereditary metabolic disorders (galactosemia, homocystinuria, etc.), corrective treatment must be carried out before surgery.
Contraindications to the removal of congenital cataracts may be extensive inoperable retinal detachment, severe vitreous fibrosis in combination with retinal damage, etc. However, indications and contraindications for surgery in these cases are established individually based on the results of a clinical and functional study of the organ of vision.
Due to age-related characteristics (strength of the ligamentous apparatus of the lens), the extracapsular method is used to remove cataracts in children. Intracapsular extraction in childhood is not used due to the high traumatic nature of the operation and the possibility of developing severe complications due to the strength of the fibers of the ciliary girdle and the hyaloid-capsular ligament, the close connection between the posterior capsule of the lens and the anterior limiting membrane of the vitreous body. The use of zonulolytic agents to dissolve ciliary girdle fibers in children is not recommended.
One of the oldest methods of treating congenital cataracts is discision. The principle of the operation is to dissect the anterior capsule of the lens with a discision needle, as a result of which the lens substance comes out into the anterior chamber, swells and resolves.
The disadvantages of the method are the frequent complications associated with leaving the lens substance in the eye: the formation of secondary cataracts , secondary glaucoma, phacogenic iridocyclitis, as well as the slow resorption of cataracts, and therefore the visual effect of the operation appears after several months, during which conditions for increasing obscuration Amblyonia.
Due to these disadvantages, discision is not currently used for soft cataracts. A two-stage operation, in which discision is first performed, and after 2-3 weeks, when swelling of the lens substance occurs, it is removed or aspirated, is also not without these disadvantages, and therefore cannot be recommended.
For zonular cataracts with a small (no more than 5.0-5.5 mm) disk of opacification and a significant increase in visual acuity when dilating the pupil using mydriatic means, an optical iridectomy is performed, the advantage of which is the preservation of accommodation.
However, the method has a number of significant drawbacks: vision is not fully restored due to the persistence of an optical obstacle in the form of central clouding of the lens, the shape of the pupil changes, so it is not advisable to use it.
For congenital cataracts, various modifications of extracapsular (linear) extraction are used. The principle of the operation is the extracapsular removal of cataracts through a small (2.5-3.0 mm) corneal incision.
In the surgical treatment of congenital cataracts, the aspiration method is widely used. The principle of the operation is to suction the lens substance. The advantage of aspiration is the ability to remove congenital cataracts through a small incision (1.5-2.0 mm), which ensures the safety of the method.
With a cystotome inserted into the anterior chamber through an incision in the cornea, limbus, or in the limbus under the conjunctival flap, the anterior capsule of the lens is opened, the substance of which is sucked out through a cannula connected to a syringe.
It is advisable to use aspiration-irrigation technique, which ensures greater efficiency and less trauma of the operation. Thanks to the irrigation of liquid carried out simultaneously with aspiration (most often isotonic sodium chloride solution), a constant depth of the anterior chamber is maintained, and therefore the possibility of injury to the endothelium of the cornea and iris by instruments is eliminated.
The operation is performed using two separate or double cannulas, one of which is intended for aspiration, the other for irrigation. The domestic industry produces a special device intended for these purposes. Aspiration of zonular cataracts can be facilitated by first injecting a 15-30% sodium sulfacyl solution into the lens, as a result of which the substance liquefies and becomes cloudy within a few minutes.
An effective, low-traumatic method is phacoemulsification, the principle of which is to emulsify the cataract using ultrasound, followed by aspiration of the lens substance.
The method proposed for the extraction of age-related cataracts is successfully used for congenital soft cataracts. The operation is performed using a special device - a phacoemulsifier, which provides ultrasound and aspiration - irrigation with precise (thanks to a computer system) balancing of fluid inflow and outflow, which makes it possible to maintain constant the depth of the anterior chamber and intraocular pressure throughout the surgical procedure.
The advantages of the method are that it allows you to completely remove the cataract through a 3 mm incision and preserve the posterior capsule of the lens, as well as a minimally traumatic operation and rapid rehabilitation of the patient.
For the removal of congenital cataracts, the domestic ultrasonic ophthalmic fragmentator UZH-F-04-0, the ultrasonic phacofragmentation system “Sparta”, vitreotome, “Ocutom” (France) are widely used. It has been established that it is possible to eliminate cataracts using laser phacopuncture and subsequent resorption therapy.
Congenital cataracts are removed under an operating microscope using micro-instruments. Operations are performed under conditions of reduced intraocular pressure, which is achieved by taking Diacarb orally the evening before the operation and in the morning on the day of the operation. To dilate the pupil, 0.1% solution of adrenaline hydrochloride (0.2 ml) is injected under the conjunctiva 30-40 minutes before the start of the operation.
Cataracts are removed through corneal incisions of minimal length (1.5-3.0 mm), which are made at a distance of 0.5-1.0 mm from the limbus, in the limbus or in the limbus under the conjunctival flap. An incision is also used in the area of the flat part of the ciliary body.
At the end of the operation, the incision is sealed by suturing using microneedles and special suture material with a thickness of 20-50 microns (threads made of supramid, nylon, etc.).
Surgical intervention is attempted with the anterior chamber preserved, which is ensured by the use of aspiration and irrigation techniques. In cases where the posterior capsule is transparent, it is preserved by clearing it of subcapsular elements with special instruments to prevent the development of opacities.
After the operation is completed, the pupil is constricted with miotic agents (pilocarpine, acetylcholine) and the anterior chamber is restored by introducing a 0.85% sodium hydrochloride solution or sterile air. An antibiotic solution is injected under the conjunctiva and a binocular bandage is applied.
In the postoperative period, 3-4-fold installations of solutions of antibiotics, sulfonamides, corticosteroids, mydriatics and other drugs according to indications are performed. Sutures are usually removed by the end of the 2nd week after surgery.
Functional results of surgical pleoptic treatment of congenital cataracts and prognosis. In connection with the use of microsurgery, the optical results of operations to remove congenital cataracts have significantly improved (Fig. 109). Visual acuity after extraction of congenital cataracts does not always correspond to the optical effect of the operations, which in most cases is due to obstructive amblyopia and concomitant visual defects. Visual acuity of 0.3 and higher after treatment is observed in 26.7-29.4% of patients, 0.05 -0.2 in 46.8-48.5%, below 0.05 in 23.8-24. 8%.
The highest functional results of surgical pleoptic treatment are observed for zonular and central cataracts with small discs of opacification, relatively high residual visual acuity, without concomitant pathology of the visual organ.
In 83.6 - 89.9% of children, visual acuity after treatment increases to 0.2 or higher, and in a significant number of patients binocular vision is restored. The prognosis for microphthalmos, nystagmus, etc. is less favorable. The functional results of treatment for unilateral cataracts are much worse than for bilateral ones. In 80.6% of children, visual acuity is below 0.05.
The prognosis for the restoration of visual acuity in congenital cataracts is determined by the achieved optical results of the operation, the clinical form of the cataract, the level of visual acuity before surgery, the presence or absence of concomitant visual defects, as well as how timely surgical treatment was performed.
Treatment of congenital cataracts
Early diagnosis of the disease allows you to either stop the development of cataracts without surgery, or perform eye surgery, thereby allowing the child’s visual system to fully develop. Therefore, all parents are strongly recommended to give their children maximum attention.
If, upon detection, the disease is not large in size and is localized in areas that do not interfere with the full development of the visual system, then surgery is not necessary. In this case, ophthalmologists prescribe a course of drug treatment that can slow down the development of the disease and even slightly improve the condition of the eye.
In case of active cataract growth, surgery is the only treatment option. Thanks to the development of modern medicine and technology, cataract surgery can be performed at any age. To effectively eliminate the disease, special ultrasound devices are used, the probes of which, through a small slot, are inserted into the affected eye of the child. The probe emits ultrasonic waves that liquefy the lens or capsule affected by the cataract. After their complete liquefaction, through a ready-made cut in the cornea, the affected part is removed from the eye, and an artificial elastic self-fixing lens made of silicone or acrylic is installed to replace it. The incision in the cornea through which all manipulations are carried out is so minimal that stitches are not required: it seals itself, some time after the operation. This surgical intervention will not require hospitalization of the child and numerous tests, and the cataract removal procedure itself lasts no more than an hour, and usually only 15-20 minutes.
If the operation is performed simultaneously on both eyes, then the artificial lens is not implanted immediately. In the early stages of life, the child develops without lenses in the eyes; after one and a half to two years, contact correction procedures begin, and only at the age of 4-5 years, the child is implanted with artificial lenses.
The sooner congenital cataracts are diagnosed and eliminated, the better, because, once affected by the disease, the eye will begin to develop incorrectly, and in the future, if the cataract is removed late, it will be impossible to restore full vision.
Among congenital pathologies of the visual organs, congenital cataracts occur in more than fifty percent of cases. The disease manifests itself in clouding of the lens of the eye. The etiology of the pathology is both hereditary and acquired in utero.
Treatment method
Congenital cataracts can only be treated through surgery, which involves removing them. However, surgery is performed if the child has reached the age of 2-3 months.
This is due to the fact that at an earlier age, the use of general anesthesia during surgery can cause serious harm to the baby’s health. Cataract surgery for two or three month old children is performed using the aspiration-irrigation method.
There are several other surgical methods to remove an eye defect:
- Cryextraction . This operation is performed using a special medical device called a cryoextractor. Using this method involves removing the eye lens by attaching it to the tip of the device, which has a low temperature. After this, a special lens is installed in place of the lens.
- Phacoemulsification . This operation is characterized by the impact of ultrasound radiation on the affected lens through holes made in advance. After this, it transforms into an emulsion, which is removed through these holes.
Cataract surgery usually takes 2 hours.
Surgeries involving the implantation of appropriate lenses into the eyeballs are carried out only for children over 4 years old!
What is congenital cataract of the eye?
Cataract is a pathological modification of the eye lens. The change is expressed in its cloudiness, deformation in shape and size. May be unilateral or bilateral.
Often, in parallel with this disease, some other anomaly of the visual organs appears.
Congenital cataracts can be recognized by clouding of the eye in the pupil area. The form of turbidity can be different:
Diffuse blurry. In the form of a point. In the form of a disk.
Treatment of congenital cataracts, depending on the type of disease, can be medicinal or surgical.
The most common types of congenital cataracts are:
Layered cataracts usually have bilateral manifestations. The affected area is located in the center of the eye. In the middle of it there is a cloudy, translucent core. With this type of pathology, in one hundred percent of cases, vision is significantly reduced.
Nuclear congenital cataracts have genetic causes. The disease is clearly hereditary. The cloudiness affects the central parts of the lens and has a dusty form. Nuclear bilateral clouding of the lens occurs, in which vision is greatly impaired. There are also cases when the clouding is localized in the form of an embryonic nucleus - in this case, a slight decrease in vision is observed. In polar congenital cataracts, the disease affects the lens capsule and its substance at the posterior and anterior poles. The lesion in the polar form of this disease can have different sizes and shapes. In proportion to their size, vision decreases. The caspulular form is an isolated opacification of the posterior or anterior capsule of the lens. The cause of this pathology is intrauterine inflammatory processes or viral infections suffered by a pregnant woman. Opacities of the lens capsule vary in shape and size. The size of the clouding determines how much a person’s vision is reduced. Complete congenital lens opacity is bilateral. The lens is completely cloudy - the child is born blind. He only has the sensation of light. With this type of pathology, blindness occurs even at the stage of intrauterine development, or can finally form in the first months after the birth of the baby.
Complete clouding of the lens is accompanied by additional pathologies of the development of the visual organs:
Cross-eyed. Nystagmus. Coloboma of the choroid. Microphthalmos. Macular hypoplasia and others.
In rare cases, complete congenital cataracts may resolve over time. Then a filmy pathology forms in its place, since after resorption a film remains.
A complicated type of eye disease occurs, as a rule, against the background of such congenital pathologies as: Congenital abnormalities of the hearing organs, up to complete deafness. Severe congenital cardiac pathologies, in particular heart disease.
Factors that provoke the development of this form of congenital cataract can be:
Viral rubella. Diabetes. Galactosemia. Other serious illnesses.
In children, congenital cataracts occur without obvious signs of lens opacification. To exclude this pathology in a child, it is necessary to show him to an eye doctor.
Types of lens opacities
A large number of different factors that provoke the development of the disease determine the polymorphism of the pathology. The classification of forms is presented in the table:
| View | Clinical picture |
| Front | Opacities localized on the anterior capsule |
| Rear | Only the posterior capsule is affected |
| Zonular | Gray-white inclusions at the posterior pole of the nucleus |
| Fusiform | Thin spindle from anterior to posterior pole |
| Central | spherical, 2 mm in diameter in the center |
| Membranous | The lens is light gray, with the passage of the mass it liquefies and wrinkles |
| A small dark core may be floating in the center | |
| Star-shaped | Pathological spraying in the area of embryonic sutures |
A congenital disease is transmitted genetically, regardless of the course of pregnancy.
There is a classification according to the degree of vision loss (I-III degree). There are congenital and intrauterine types. In the first case, the disease is inherited from parents, and in the second it is caused by the action of damaging factors. Lens opacities can occur in one eye or affect both sides. Some forms are only bilateral, for example, membranous cataract in children, formed against the background of congenital syphilis.
The treatment tactics and prognosis for the patient depend on the type, location and extent of the disease.
Causes of congenital cataracts in children and adults
All the causes of this pathology of the visual organs can be divided into:
Hereditary. Acquired in utero.
About one third of all cases of congenital eye disease in children and adults are classified as hereditary.
Also, quite often, it occurs against the background of such genetically determined pathologies as:
Down syndrome. Rothmund syndrome. Werner's syndrome.
This clouding of the lens does not develop immediately, but is delayed as the symptoms of these diseases appear.
Thus, with Werner syndrome, the disease can develop between the twentieth and fortieth year of a person’s life.
With Rothmund syndrome, it manifests itself in the third decade of a person’s life.
During intrauterine development, a child may suffer, and, as a result, develop pathology after a pregnant woman suffers from the following diseases:
Rubella. Cytomegalovirus infection. Chicken pox. Toxoplasmosis. Herpes. Syphilis.
The child may also develop in utero in cases where the woman is sick:
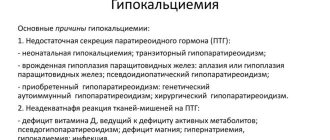
Diabetes mellitus. Myotonic dystrophy. Hypocalcemia. Galactosemia. Wilson-Konovalov disease.
In utero, the considered pathology in children also occurs if the fetus itself has suffered from eye inflammatory infections: for example, from iritis - inflammation of the iris.
Symptoms
Congenital cataracts in children are difficult to diagnose. The main subjective symptom is a decrease or absence of visual functions. Its presence is reliably determined from 2-3 months, when the baby begins to follow bright objects. In rare cases (with the central, membranous type), the child’s naked eye notices a milky-white darkening against the background of the iris. Strabismus and nystagmus (rhythmic movements of the eyeball in a vertical or horizontal direction) may indicate a one-sided lack of vision. With underdevelopment of the lens apparatus and concomitant subluxation, phacodenesis (its trembling) is noted.
The doctor examines the baby immediately after birth to rule out eye problems.
In order not to miss eye symptoms in newborns, neonatologists, while still in the maternity hospital, check the presence of the pupillary reflex and the range of movement of the eyeballs. For babies without concomitant pathologies, a scheduled consultation with an ophthalmologist is scheduled at 3 months. When a premature baby is born, an ophthalmologist is consulted monthly.
How are congenital cataracts treated today - when is surgery needed?
The main symptoms of congenital cataracts of the eye include, in addition to clouding in the pupil area, the following:
Nystagmus. Strabismus. The child shows no signs of following toys with his eyes. The child examines objects with one eye. At the same time, the baby strives to turn one side to the object being studied. The child’s lack of fixation on toys and people’s faces.
To establish an accurate diagnosis, prognosis is extremely important. Depending on the form, the treatment method is prescribed.
It should be understood that this pathology cannot be cured with medication!
However, surgical intervention is not always used immediately. Once a diagnosis is made, treatment is developed individually .
In cases where the localization of clouding of the lens of the eye does not interfere with the normal development of the child’s vision, conservative supportive therapy is prescribed and monitored over time.
Cataracts that prevent the baby’s vision from developing correctly should be removed as soon as possible.
It is important to prevent such a serious complication of congenital cataracts as amblyopia - severe vision loss that cannot be restored.
Once a diagnosis has been established, treatment through surgical intervention is carried out for children starting from two to three months of age . Babies are not scheduled for surgery until they are 6 weeks old due to the risk of complications after general anesthesia.
At the age of three months, to remove the pathological lens in children, it is enough to make a very small incision, since the still soft substance is easily removed using the aspiration-irrigation method.
Today, several types of operations are performed to remove congenital cataracts of the eye.
The method of intracapsular cataract extraction involves removing the lens along with the capsule. During extracapsular cataract extraction surgery, the lens capsule remains in place. Only the core and substance are removed.
The cryoextraction operation involves removing the lens by freezing it to a cooled cryoextractor instrument.
The most common type of surgery is phacoemulsification . During this operation, several very small incisions of 2-3 mm are made. Through them, the mass of the lens is exposed to ultrasound, transforming the lens substance into an emulsion. The softened lens material is then removed. A special flexible lens is placed in place of the affected lens. It straightens and fixes inside the eye.
For children, operations with implantation of intraocular lenses are prescribed at the age of four to five years!
At an earlier age, children undergo operations using the irrigation-aspiration method.
Home Eye diseases Cataract
Congenital cataract is a clouding of the lens that occurs in a newborn child. However, quite often this pathology is not detected immediately, but after a time after a detailed examination.
If any signs appear that indicate cataracts in a child, you should seek help from an ophthalmologist.
The lens of a healthy child is a transparent biconvex lens, which is a refractive medium. There is no innervation or blood supply, and nutrition is provided due to the watery structure of the organ of vision.
There are factors that lead to disruption of the protein composition of the lens fibers, as a result of which it loses its transparency.
According to statistics, this disease is diagnosed in one newborn child out of two thousand. Moreover, the defeat is usually one-sided.
Treatment
In the presence of small opacities, treatment of congenital cataracts is carried out conservatively. The sick child is prescribed cytoprotectors and vitamins. Unfortunately, with massive cataracts, drug therapy does not have the desired effect.
Surgical treatment is indicated for children with central clouding of the lens, which greatly reduces visual acuity. Experts recommend removing such cataracts at the age of 6 weeks to 3 months. The operation is most often performed using the irrigation-aspiration method. The issue of timing of intraocular lens implantation is still controversial in medical circles.
Some doctors believe that placing an IOL interferes with the normal growth and development of the eyeball. Therefore, it is better to implant an artificial lens in a child later, at the age of three or more years.
On the other hand, an intraocular lens provides the highest quality and physiological vision correction. Its placement helps to avoid the development of amblyopia and other undesirable consequences of the absence of a lens.
Classification
This pathology has quite a few varieties, each of which has certain characteristics:
Capsular cataract is an isolated lesion of the posterior or anterior lens capsule. In such a situation, vision may be slightly blurred or completely absent - it all depends on the area of the lesion. The development of this pathology is caused by metabolic disorders in the mother’s body or inflammation during intrauterine development.
Polar cataract affects not only the capsule, but also the surface of the lens. As a rule, this form of pathology is characterized by bilateral damage. The quality of vision is affected by the intensity and area of the lesion.
Layered cataract is a lesion of the central region of the lens. This form of the disease is the most common; its danger is that the child almost completely loses his vision. The main reason for the development of pathology lies in hereditary predisposition.
Complete cataract - this pathology develops in both eyes at once, and it is characterized by such a strong degree of clouding that, as a rule, children are born blind. In addition, complete cataracts are accompanied by other eye diseases - strabismus, macular hypoplasia.
Complicated cataract - this disease is a consequence of viral or bacterial infections in the early stages of pregnancy. In this case, two eyes are affected at once, and other diseases are almost always present. Moreover, concomitant pathologies do not necessarily affect the eyes specifically - disorders can affect the hearing organs, speech apparatus, heart or nervous system.
Prevention
To avoid further progression of eye diseases, the child must be shown to an ophthalmologist. The doctor will prescribe special eye drops that must be used strictly according to the instructions. Lotions with celandine, which should be applied to the eyes throughout the night, are famous for their great effectiveness. They will not only help relieve discomfort, but will also have a beneficial effect on vision. Don’t forget about maintaining a proper diet. You should eat fruits and vegetables, dairy products, nuts, seafood, greens, berries, especially blueberries. It is advisable to exclude all fatty and fried foods, pickles, smoked foods, and spicy foods. After returning home from the street, you need to wash your face with a special gel to remove all dust from it.
In the summer, doctors recommend using sunglasses that will protect your eyes from exposure to ultraviolet rays. You should limit your time watching TV or playing computer games to one hour a day. In this case, you need to take short breaks for eye exercises. It is advisable to read only during the day in good lighting, but if this is not possible, then you should buy a high-quality and bright table lamp, under which the child will not strain his eyesight.
Reasons for the development of the disease
There is a whole group of risk factors that increase the risk of developing congenital cataracts:
Genetic predisposition - this disease can be inherited in an autosomal dominant manner.
Metabolic disorders - hypocalcemia, myotonic dystrophy, diabetes mellitus.
Genetically determined pathologies in a child - this may be Down, Lowe or Marfan syndrome.
Intrauterine infectious diseases - the development of congenital cataracts is often provoked by syphilis, rubella, toxoplasmosis, herpes, and chickenpox.
Intrauterine inflammatory processes of the organs of vision - for example, iritis.
Forecast and preventive measures
If a small patient does not undergo surgery in the first 6 months of life, the prognosis for preserving vision is unfavorable. This is due to the fact that the nerve connections between the visual analyzer and the brain are formed immediately after birth, by “training” the cells of the retina with light. If this does not happen, the nervous tissue dies and cannot be restored.
Prevention is standard screening of pregnant women (HIV, RW). Persons compromised by infectious pathology should be examined for TORCH infections. Genetic counseling is necessary for expectant mothers who have a family history of congenital cataracts. Timely ultrasound diagnosis of the fetal condition is important. If infectious or metabolic diseases are suspected, multiple malformations are possible. This is an indication for termination of pregnancy.
Diagnosis at an early stage
Diagnosis of this disease begins with a visit to an ophthalmologist. In order to promptly identify pathology, you need to know what symptoms it is accompanied by:
clouding of the pupil; lack of gaze fixation at the age of two months; strabismus; viewing objects with one eye; nystagmus; Severe amblyopia is blindness associated with lack of treatment.
In addition, the pediatric ophthalmologist must conduct the following types of studies that will help detect the disease:
Ophthalmoscopy. Optical coherence tomography. Slit biomicroscopy. Echoophthalmoscopy - ultrasound of the eyeball.
Therapy
The sooner a cataract is detected, the higher the chances of successfully getting rid of it. When cataracts are removed in a child before six months of age, the likelihood of proper eye development is greatest. At the same time, the bilateral form is cured better and faster than the unilateral one.
Thanks to the development of modern medicine, the prognosis for the disease is favorable, but depends on the following factors: the severity of the disease, the area affected, as well as concomitant diseases.
Traditional methods
There are many traditional methods for treating cataracts. The most popular of them are the following:
- Drops with honey and apple. Take a small apple and cut off the top of it. After this, the entire core is removed. Place 2 teaspoons of honey into the resulting recess. Then the apple is closed at the top with the cut off top. The fruit is left in this form for 2 days. After this time, the juice from the apple is poured into a container. Then the liquid is instilled into the eyes, one or two drops three times a day. The product is stored in the refrigerator.
- Honey. For a honey compress, take 1 tsp. Add this product to 1 cup of hot water and boil for several minutes. After cooling, a piece of gauze is soaked in the mixture and applied to the eyes as a compress. This procedure is carried out every night, keeping the gauze on the eyes for 5 minutes.
- Onion drops. The onion is peeled, grated and the juice is decanted from the pulp, which is then mixed with water 1 to 1. It is better to take purified or distilled water. The resulting infusion is dropped into the eyes every day.
- Infusion of potato sprouts. Potato sprouts are collected and dried. Dry sprouts (1 tbsp) are poured with vodka (0.5 liters). The resulting mixture is infused for a week in a cool, dark place. The infusion is used one teaspoon three times a day.
Drug treatment
Drug treatment has the following goal: increasing blood circulation; improvement of metabolic processes that affect the transparency of the lens; saturating the eyes with vitamins and other missing substances.
Drops for treatment should contain the following substances: nicotinic acid, K, Mg, Ca, C, B2, and PP. The most common drugs for the treatment of cataracts are Taufon and Emoxipine. However, the big disadvantage of these products is that they can only be stored for a week when opened, and then they lose their beneficial properties.
In this regard, imported drugs have an advantage, such as:
- Quinax (Belgium.
- Catalin (Japan).
- Katachrom (Finland).
- Senkatalin (India).
- Vicein and Vitaiodurol (France).
To cure cataracts without surgery, tablets with vitamin complexes can be prescribed. These drugs enhance the effects of drops.
This treatment method has certain disadvantages: long-term use of drops and tablets can adversely affect the overall health of the eyes. Therefore, ophthalmologists advise using the drugs in courses with a break between them. Another disadvantage is the fairly high cost of the drops.
Useful video
Causes, types and stages (degrees) of cataracts:
Operation
If the size of the clouding in the thickness of the lens is large and negatively affects visual acuity, the ophthalmologist may recommend surgical removal of the cataract.
When is it appointed?
Treatment with surgery is prescribed if cataracts impair vision to such an extent that it affects the further development of the child. In the case of congenital cataracts, surgery is recommended to be performed as soon as possible.
Preparation
At the clinic, the patient may be given a light sedative and then prepared for surgery. The skin around the eye is wiped with a bactericidal agent to prevent bacteria from entering. After this, the child is given anesthesia and his face is covered with sterile napkins, leaving only the area of the operated eye exposed.
Features of surgical treatment
There are various approaches to the treatment of congenital cataracts.
If it negatively affects central visual acuity, the cataract should be removed as soon as possible. If the location of the opacity does not affect the clarity of central vision, such a cataract does not require surgical treatment, but requires dynamic monitoring.
Moreover, the operation is also associated with the threat of complications – in particular, increased intraocular pressure. General anesthesia used for surgery is also a risk factor.
Many doctors say that the appropriate age for a child to undergo surgical correction is from 6 weeks to 3 months. Today there are several types of interventions:
extracapsular cataract extraction; cryoextraction; intracapsular cataract extraction; phacoemulsification.
Forms of manifestation of cataracts
There are many manifestations of this disease. If in adults they are most noticeable, so such patients can easily describe their sensations, then a child is a difficult patient in terms of making a diagnosis. The most obvious violations that you need to pay attention to during inspection are:
There are also types of cataracts in a child’s eye, in which the anterior and posterior parts of the eye undergo mutations. At the same time, localizing the turbidity is quite difficult. When these indicators indicate a complicated form of the disease, it is necessary to prescribe much more complex treatment with constant maintenance of the level of vision even after surgery.
If it develops, there are only two options for treating cataracts in a child:
Diagnosis of cataracts in children
Congenital cataracts are often diagnosed during the first examination of a baby after birth. However, the pediatrician does not always detect vision problems in a child. Most often, the disease is detected when you return to the clinic for a routine examination. Also, when parents identify symptoms, they independently make an appointment for their children to see an ophthalmologist.
The ophthalmologist is primarily involved in collecting anamnesis - information that will help in making a diagnosis (information about medical history, previous diseases, etc.). After this, visual acuity is checked, the retina is examined, visual fields are identified, and the pressure inside the eyeball is measured.
Possible examinations that a child must undergo for an accurate diagnosis:
- ophthalmoscopy – assessment of the condition of the fundus using a mirror or electric ophthalmoscope;
- optical coherence tomography (OCT) – using a special device, the layers of the retina are scanned, after which the image is transmitted to the monitor;
- biomicroscopy – examination of the cornea, lens, anterior segment of the eye. The diagnosis takes place in complete darkness, the ophthalmologist directs a beam of light onto the patient’s lens and, through a microscope mounted on a special device, determines the transparency of the lens, refractive power, etc.
Older children are prescribed a visual acuity test using the Sivtsev or Orlova table. The lines of the first table contain letters, so this diagnosis is carried out for school-age children. Orlova’s table contains pictures instead of letters, which is why the table is used to test visual acuity for patients who do not yet know the alphabet.
How to treat cataracts in children
Treatment of cataracts with medications is not effective. Eye drops can only slow down the development of the disease, but not restore full vision. The only option for young patients is surgery.
Surgical intervention is carried out taking into account the following factors:
- patient's age;
- degree of cataract development;
- type of disease;
- the presence of accompanying diseases.
Cataract surgery is performed under general anesthesia. The essence of the treatment is that the affected lens is removed and a new one is put in its place, which will act as a natural lens. The artificial lens has greater optical power, which allows the child to regain full vision. The implant is replaced as the child grows.
Removing a cataract surgically takes from 15 minutes to half an hour, depending on the complexity of the case. Infants are placed in a hospital after surgery, while older children can undergo the recovery period at home.
The success of the operation also depends on the rehabilitation process. The eye heals in about two weeks. To avoid complications, you must follow your doctor’s instructions: use special eye drops to prevent infectious diseases, come regularly for examinations, and avoid getting water in your eyes for one month.
To correct vision, an ophthalmologist may also prescribe wearing glasses. This is possible with a bilateral form of the disease. Glasses can be with multifocal and bifocal lenses. The former help focus vision on objects that are close, far and at an average distance from the child. Bifocals allow you to clearly see what is far or close.
Main causes of childhood cataracts
Congenital cataracts in children develop in utero and can occur due to the following factors:
- viral disease during the first trimester of pregnancy;
- abuse of alcohol, drugs or contraceptives during pregnancy;
- chronic illnesses of parents;
- different Rh factor in mother and child;
- lack of vitamins;
- metabolic disorders.
Premature birth can cause congenital cataracts . In premature babies, the visual system is not fully formed, which can lead to the development of cataracts and other eye diseases.
Acquired childhood cataracts occur due to the negative impact of external factors on the fragile body:
- head and eye injuries;
- bad ecology;
- illnesses of the baby (diabetes mellitus, infection, toxocariasis and others);
- taking medications that are inappropriate for children;
- impaired metabolism;
- radiation.
Depending on the cause of cataracts in children and the nature of the disease, appropriate treatment is prescribed. If you seek help from a clinic in the initial stages of pathology development, it is possible to restore the ability of the lens to focus light rays.
Symptoms
It is quite difficult for parents to identify the symptoms of cataracts in young children. You should carefully monitor the child's behavior. Signs of cataracts in newborns:
- gray/white pupils;
- the child’s eyes move quickly and do not focus on one point;
- the child does not observe what is happening around him or examines objects with one eye;
- strabismus.
In one-year-olds and older children, cataracts appear gradually. Visual acuity decreases depending on the degree of damage to the lens.
Symptoms of childhood cataracts:
- blurred vision;
- when viewing a picture or photo, a child cannot clearly answer what exactly is shown there due to blurred lines;
- in ordinary life situations, the child behaves differently, becomes more irritable, withdraws into himself;
- complaints of dots and stripes flashing before the eyes;
- the color of objects is distorted, the shades are confused.
Diagnosis of the disease
Diagnostic procedures include medical history, ophthalmological examination, and instrumental methods.
- History: maternal illness or medication taken during pregnancy. Systemic or ocular diseases in newborns and children. Radiation, trauma. Congenital cataracts run in the family.
- If possible, determine the visual acuity of each eye in particular using tables with sticks, drawings, or evaluate how the child follows small toys or light.
- Ophthalmological examination to determine the role of cataracts in reducing visual acuity. Determine the size and location of cataracts, the possibility of retinal detachment using direct ophthalmoscopy with a normal (non-dilated) pupil. Examination with a portable slit lamp, as well as a retinoscope, is useful (dulling of the retinoscopy reflex indicates that cataracts significantly affect vision). Identification of signs of concomitant glaucoma (increased corneal diameter, corneal edema, ruptures of Descemet’s membrane) and retinal pathology, if any.
Prevention of childhood cataracts
If one of the parents (or both parents) has cataracts, then you need to inform the gynecologist about this before conceiving a child. It is necessary to undergo examinations to identify the hereditary factor of the disease. To prevent the development of cataracts in utero, the mother is prescribed special treatment and vitamins. Also, the expectant mother should:
- stop drinking alcohol and strong drugs;
- promptly treat infectious diseases if they arise during pregnancy;
- protect yourself from injury, radiation;
- spend more time outdoors;
- Healthy food;
- worry and worry less to eliminate the risk of premature birth.
To prevent acquired cataracts in children, you must adhere to the following recommendations:
- provide optimal lighting in the nursery so that the child can play and study comfortably;
- watch how we feed the child. His diet should always contain vegetables, fish, fruits, and dairy products so that the body is saturated with vitamins and minerals;
- walk more in the fresh air. Limit your time watching cartoons, playing games on a computer or tablet;
- do not forget to undergo routine examinations with an ophthalmologist every year;
- Monitor your child's hygiene. Infectious diseases associated with unwashed hands are one of the causes of eye diseases;
- Buy sunglasses for your child. This should only be done in an optician under the guidance of a specialist. Otherwise, there is a risk of buying glasses with poor quality lenses that will not protect the eyeball from ultraviolet radiation and bright light.