| Atrioventricular block | |
| ICD-10 | 44.044.0-44.344.3 |
| ICD-9 | 426.0426.0-426.1426.1 |
| eMedicine | med/189 |
| MeSH | D006327 |
Atrioventricular block (AVB)
is a type of heart block that indicates a violation of the conduction of electrical impulses from the atria to the ventricles (atrioventricular conduction), often leading to disturbances in heart rhythm and hemodynamics. There are 3 degrees of atrioventricular block.
Atrioventricular block
The basis of atrioventricular block is the slowing down or complete cessation of the passage of the impulse from the atria to the ventricles due to damage to the AV node itself, the His bundle or the branches of the His bundle. Moreover, the lower the level of damage, the more severe the manifestations of the blockade and the more unsatisfactory the prognosis. The prevalence of atrioventricular block is higher among patients suffering from concomitant cardiac pathology. Among people with heart disease, I degree AV block occurs in 5% of cases, II degree - in 2% of cases, III degree AV block usually develops in patients over 70 years of age. Sudden cardiac death, according to statistics, occurs in 17% of patients with complete AV block.
The atrioventricular node (AV node) is part of the conduction system of the heart, providing sequential contraction of the atria and ventricles. The movement of electrical impulses coming from the sinus node is slowed down in the AV node, allowing the atria to contract and pump blood into the ventricles. After a short delay, the impulses spread along the His bundle and its legs to the right and left ventricles, promoting their excitation and contraction. This mechanism ensures alternate contraction of the atria and ventricles myocardium and maintains stable hemodynamics.
Diagnostics
Atrioventricular block on the electrocardiogram
Establishing the correct diagnosis is carried out by a cardiologist, who must study the results of laboratory and instrumental examinations and independently carry out a number of manipulations.
Thus, the primary diagnosis for AV block includes:
- studying the medical history - to search for diseases that could precede the onset of pathology;
- collection and analysis of life history - to establish the fact of inadequate use of medications;
- listening to the patient using a phonendoscope to determine heart rate;
- a detailed survey - to identify the first time of onset and intensity of symptoms, which will indicate the form and nature of the disease.
Among the most informative instrumental procedures it is worth highlighting:
- ECG and EchoCG;
- Ultrasound of the heart;
- daily ECG monitoring;
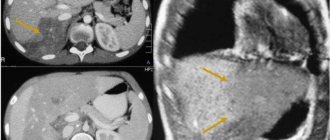
- CT or MRI of the heart;
- MSCT and EPI.
Laboratory tests are of an auxiliary nature and are limited to general clinical and biochemical blood tests.
Classification of AV blocks
Depending on the level at which the disturbance of electrical impulse conduction develops, proximal, distal and combined atrioventricular blockades are distinguished. With proximal AV blockade, impulse conduction may be disrupted at the level of the atria, AV node, and His bundle branch; at distal – at the level of the branches of the His bundle; with combined ones, multi-level conduction disturbances are observed.
Taking into account the duration of development of atrioventricular block, it is divided into acute (with myocardial infarction, drug overdose, etc.), intermittent (intermittent - with ischemic heart disease, accompanied by transient coronary insufficiency) and chronic forms. According to electrocardiographic criteria (slowness, periodicity, or complete absence of impulse conduction to the ventricles), three degrees of atrioventricular block are distinguished:
- I degree
- atrioventricular conduction through the AV node is slowed down, but all impulses from the atria reach the ventricles. Clinically not recognized; on the ECG the PQ interval is prolonged > 0.20 seconds. - II degree
– incomplete atrioventricular block; not all atrial impulses reach the ventricles. The ECG shows periodic loss of ventricular complexes. There are three types of second-degree AV block according to Mobitz:
- Mobitz type I - the delay of each subsequent impulse in the AV node leads to a complete delay of one of them and loss of the ventricular complex (Samoilov-Wenckebach period).
- Mobitz type II - critical impulse delay develops suddenly, without a previous prolongation of the delay period. In this case, the absence of conduction of every second (2:1) or third (3:1) impulse is noted.
- III degree
– (complete atrioventricular block) – complete cessation of the passage of impulses from the atria to the ventricles. The atria contract under the influence of the sinus node, the ventricles contract at their own rhythm, less than 40 times per minute, which is not enough to ensure adequate blood circulation.
Atrioventricular blocks of the 1st and 2nd degrees are partial (incomplete), blockades of the 3rd degree are complete.
Atrioventricular block and bundle branch block are the same thing
With the development of conduction block in all three main branches of the His bundle, atrioventricular block occurs. If the blockade of one or two branches is incomplete, then the atrioventricular block will also be incomplete. Then the ECG will record signs of a two-bundle blockade in the His system (those two branches whose blockade is more complete) and signs of incomplete A-V blockade of the corresponding degree. This type (level) of atrioventricular block is called distal, because conduction disturbances occur in the distal part of the atrioventricular system (distal localization of A - V blockade).
The figure shows an ECG with an incomplete three-bundle block in the His system, determined by the presence of slowing of atrioventricular conduction (1st degree block, P - Q = 0.31 sec.) and complete blockade of the right and left anterior branches of the His bundle. There are no signs of incomplete blockade of the third branch (left posterior in this case), through which the impulse passes into the ventricles (with a slowdown leading to widening of P - Q), on the ECG.
Of course, in the presented case, it is impossible to completely exclude a combination of a proximal type of atrioventricular block (block at the level of the A-V node) and a two-bundle block in the His system. However, such an assumption is less likely, because for this there must be myocardial damage at two levels: meanwhile, this combination is less common. In such cases, it is sometimes possible to finally resolve the issue of the level of A-V blockade based on the dynamics of ECG changes.
Complete blockade of all three main branches of the His bundle is one of the causes of complete atrioventricular block. A characteristic feature of complete three-fascicular block, which determines the severity of the prognosis for patients suffering from it, should be considered idioventricular rhythm. The latter is characterized by low frequency and often arrhythmic contractions of the ventricles due to migration of the source of automaticity in the ventricles. Low reliability of the idioventricular rhythm often manifests itself in the form of periods of asystole of varying duration and the appearance of ventricular fibrillation, clinically manifested by Morgagni-Adams-Stokes syndrome.
On the ECG, complete three-fascicular block is characterized by a picture of complete atrioventricular block at the distal level (complete lack of connection between usually rare ventricular complexes and more frequent atrial waves - the P-Q intervals are different) and deformation of the ventricular complex like a two-fascicular block. However, such a deformation of the ventricular complex does not reflect the blockade of the His bundle, but the idioventricular rhythm emanating from the third branch, which has no signs of blockade on the ECG.
The impulse arising in this branch excites first of all the corresponding ventricle or half of it, and then belatedly spreads to other parts of the ventricles, supplied by the remaining two branches of His. Thus, if during complete A-V blockade the ventricular complex is deformed according to the type of blockade of the two left branches, then this means that the idioventricular rhythm originates from the right branch of the His bundle. If there is a pattern of blockade of the right and left anterior branches, then the idioventricular rhythm comes from the left posterior branch. When the idioventricular pacemaker changes, the QRS shape (similar to another blockade of two branches) and the rhythm frequency change simultaneously. Often, an incomplete three-bundle block becomes complete and vice versa. For illustration, we present an ECG - observations of three-bundle blockades.
— Return to the table of contents of the section “
Cardiology."
Atrioventricular block is a partial or complete cessation of impulse transmission from the atria to the ventricles. The most common cause is idiopathic fibrosis and sclerosis of the conduction system. Pathology is diagnosed using ECG data. Symptoms and treatment depend on the degree of blockage, but therapy, if necessary, usually involves the use of a pacemaker.
AV block occurs as a consequence of idiopathic fibrosis and sclerosis of the conduction system in approximately 50% of patients, and in 40% as a result of coronary artery disease. The remaining cases are due to medications (for example, beta-blockers, calcium channel blockers, digoxin, amiodarone), increased vagal tone, valvulopathy, congenital pathology, genetic and other anomalies.
[1], [2], [3], [4], [5], [6], [7], [8], [9]
All normal waves are accompanied by RR complexes, but PR intervals are longer than normal (> 0.2 s). First-degree AV block may be physiological in young patients with excessive vagal influence and in well-trained athletes. First degree atrioventricular block is always asymptomatic and does not require treatment, however, if it is combined with another heart pathology, further examination of the patient is indicated, as it may be associated with the use of medications.
[10], [11], [12], [13], [14], [15]
Some normal waves are accompanied by ventricular complexes, but some are not. There are three types of this pathology.
With Mobitz type I second degree atrioventricular block, there is a progressive lengthening of the PR interval after each contraction until the conduction of the atrial impulse ceases altogether and the complex drops out (Wenckebach phenomenon). Conduction through the AV node is restored to the next contraction, and the situation repeats. Mobitz type I second degree atrioventricular block can be physiological in young patients and many athletes. The block appears in the AV junction in 75% of representatives with narrow QRS complexes and in lower located areas (bundle of His, bundle branches, Purkinje fibers) in the rest. If the block becomes complete, a junctional escape rhythm usually appears. There is no need for treatment as long as the blockade does not lead to bradycardia with clinical symptoms. It is also necessary to exclude temporary or avoidable causes. Treatment consists of pacemaker implantation, which can also be successful in asymptomatic patients with Mobitz type I second-degree atrioventricular block at the subnodal level identified during an electrophysiological study performed for another reason.
With Mobitz type II second degree atrioventricular block, the PR interval is the same. The impulses are not carried out immediately, and the QRS complex falls out, usually with repeating wave cycles - every third cycle (1:3 block) or fourth (1:4 block). Mobitz type II second degree atrioventricular block is always pathological. In 20% of patients it occurs at the level of the His bundle, in the branches of this bundle - in the rest. Patients may have no clinical manifestations or experience mild dizziness, presyncope and syncope, depending on the ratio of conducted and unconducted impulses. Patients are at risk of developing high-grade clinical block or complete block, in which the escape rhythm is likely to be ventricular and therefore infrequent and unable to supply systemic blood supply. Therefore, IVR is indicated.
High grade II degree block is characterized by loss of every second or more often ventricular complex. It can be difficult to distinguish between a Mobitz I and a Mobitz II block because the two waves never appear on the contour line. The risk of developing complete atrioventricular block is difficult to predict, so IVR is prescribed.
Patients with any type of second degree atrioventricular block who have structural heart disease should be considered candidates for permanent pacing, except for transient and reversible causes.
[16], [17], [18]
Atrioventricular block is complete: there is no electrical connection between the atria and ventricles and, accordingly, there is no connection between the teeth and QRS complexes (AV dissociation). Cardiac activity is maintained by slipping pacemaker impulses from the AV node or ventricle. The rhythm generated above the His bundle bifurcation produces narrow ventricular beats of relatively high frequency (>40/min), a relatively high heart rate, and little symptomatology (eg, weakness, postural dizziness, exercise intolerance). The rhythm formed below the bifurcation gives wide QRS complexes, low heart rate and more severe clinical manifestations (presyncope and syncope, heart failure). Symptoms include signs of AV dissociation such as cannonball a waves, blood pressure variability, and changes in the sonority of the first tone. The risk of syncope due to asystole, as well as sudden death, is higher if there is insufficient generation of impulses by the pacemaker.
Most patients require IVR. If the block occurs due to antiarrhythmic drugs, drug withdrawal may be an effective treatment, although temporary pacing is sometimes necessary. If block develops in acute inferior MI, signs of AV node dysfunction usually appear, which are sensitive to atropine or may resolve spontaneously after a few days. The block that develops with anterior MI usually indicates extensive areas of necrosis involving the His-Purkinje system and requires immediate transvenous pacemaker implantation with temporary external pacing if necessary. Spontaneous resolution is possible, but investigation of the AV node and underlying structures is necessary (eg, electrophysiological study, stress test, 24-hour ECG monitoring).
Most patients with congenital third degree atrioventricular block have a junctional escape rhythm that maintains a fairly adequate rhythm, but they require implantation of a permanent pacemaker until middle age. Less commonly, patients with congenital third degree atrioventricular block have a rare escape rhythm, which creates the need for pacemaker implantation in childhood, perhaps even in early childhood.
[19], [20], [21], [22], [23]
One of the fairly common pathologies is heart block. Their cause lies in a violation of the conduction of impulses from the atrium to the ventricle of the heart. It may not be transmitted at all or may be partially transmitted. One of the varieties is atrioventricular blockade. The essence of the disease is that the electrical impulse does not completely or partially pass to the atria from the ventricles. The main reason for the block is that there is damage to the atrioventricular node of His or the bundle branches.
The lower the location of the lesion, the more complex the form of the pathology. According to statistics, the diagnosis of atrioventricular block develops in people after 70 years of age.
The AV node is one of the components of the parts of the heart through which impulses are conducted. It is this impulse coming from the sinus node that causes the heart to contract. When an impulse enters the atrioventricular node, its speed slows down. This is necessary for blood to enter the ventricles and the atria to contract. Upon completion of this process, the impulse goes to the His bundle and along its legs. As a result, the left and right ventricles contract. The frequency of contraction of the ventricles and atria of the heart, as well as the stability of hemodynamics, depend on the condition and ability of the atrioventricular node to perform its functions.
In modern medicine, to classify AV block, factors such as the localization of the place where impulse conduction is disrupted, its duration, as well as electrocardiographic criteria for pathology are used.
Blockades are classified according to location:
- Proximal. The disorder is located near the atrioventricular node, atria, or PG trunk.
- Distal. The site of the disorder is localized near the branches of the His bundle.
- Combined. The location of the impulse conduction disturbance can be located as in the first and second cases.
If we talk about the duration of the blockade, there are the following types:
- Spicy. Atrioventricular block of this type is possible in case of a previous myocardial infarction or in case of violation of the dosage of medications.
- Intermittent. The cause of its occurrence may be coronary heart disease, which is accompanied by the presence of coronary heart failure.
- Chronic. This type of blockage is the result of chronic heart disease.
As for electrocardiographic indicators of the course of the pathology, experts classify AV blockade into the following types:
- 1st degree. This is the initial stage of the pathology. The deceleration of impulse conduction in this case slows down for a short period of time. First degree blockade can be diagnosed using an electrocardiogram, which will clearly show an increase or decrease in the height of the teeth. In most cases, the blockade at this stage of development occurs without any symptoms. Treatment consists of identifying the cause that caused the disturbance in the conduction of impulses and eliminating them. Otherwise, the disease can be neglected and its development will continue with complications.
- Atrioventricular block, 2nd degree. The peculiarity of the course of the disease at this stage is that the passage of only part of the impulses to the ventricles is blocked. This is due to the loss of some ventricular contractions. When deciphering the results of the electrocardiogram, you can see that normal contractions are replaced by slow ones. When deceleration occurs, the patient experiences darkness before the eyes, the heart contracts irregularly, weakness occurs, and possibly fainting. Such attacks can be repeated several times throughout the day. When diagnosing 2nd degree AV block, in parallel with an electrocardiogram, electrocardiography is also prescribed, as well as a general analysis of blood and urine for the presence of electrolytes and cardiac-specific enzymes.
- AV heart block 3rd degree. It represents the most complex and dangerous stage of the disease. The danger lies in complete AV block of the heart for the passage of impulses, severe disruption of the rhythm of heart contraction. The atria contract under the influence of impulses coming from the sinus node. This leads to a slower rhythm of atrial contraction. As a result, the patient develops complex bradycardia, low blood pressure, severe shortness of breath, fainting or dizziness. To diagnose 3rd degree AV block, specialists use various research methods. When the patient develops a complete blockade, he almost completely loses his ability to work. To eliminate the attack, the patient needs resuscitation. The use of drug treatment can eliminate the symptoms of the pathology and its attacks for a very short time. A person needs to use artificial electrical stimulation. If you do not provide timely assistance with the development of incomplete 3rd degree block, there is every chance of it developing into a complete AV block.
Determining the progression of the disease and prescribing an effective course of treatment can save the patient’s life.
The choice of treatment course directly depends on the cause that provoked the pathology. For example, if AV blockade caused a dosage violation while taking medications, you can relieve the attack and eliminate the cause by using the following methods:
- stop taking the medication;
- give the patient Activated carbon tablets;
- Antidigoxin can be administered;
- in the presence of bradycardia, an injection of lidocaine or phenytoin is recommended.
If the cause of the blockade is an increase in the tone of the vagus nerve, good results can be achieved in this way:
- give the patient an injection of Atropine or Zelenin drops;
- The Izadrina injection helps a lot.
The transient type of pathology development significantly complicates the process of its treatment. In this case, hospitalization and surgical intervention cannot be avoided.
When the cause of the pathology lies in coronary heart disease, a whole complex of medications is prescribed, the action of which is aimed at dilating blood vessels, as well as eliminating the source of metabolic disorders within cells. The following drugs are used for treatment:
- beta blockers;
- drugs from the group of coronary lytics;
- Atropine injection.
It is difficult to relieve an attack if it is accompanied by severe swelling and shortness of breath. In this case, the treatment consists of specialists surgically inserting a pacemaker into the patient, which forces the parts of the heart to contract at a certain frequency.
Predicting the effectiveness of treatment and the patient’s return to normal life fully depends on the type of development of the blockade. Prognosis is difficult for patients with a transient type of blockade. It is quite difficult to treat.
Treatment of AV block is also complicated by the need to be careful and constantly keep the patient under electrocardiographic monitoring. The patient is required to fully comply with the requirements of specialists, not resort to the use of traditional methods of treatment and undergo examination on schedule. Be healthy!
Reasons for the development of AV blockades
According to etiology, functional and organic atrioventricular blockades are distinguished. Functional AV blockades are caused by an increase in the tone of the parasympathetic nervous system. Atrioventricular block of the first and second degrees is observed in isolated cases in young physically healthy individuals, trained athletes, and pilots. It usually develops during sleep and disappears during physical activity, which is explained by increased activity of the vagus nerve and is considered a normal variant.
AV blockades of organic (cardiac) origin develop as a result of idiopathic fibrosis and sclerosis of the conduction system of the heart in various diseases. The causes of cardiac AV blockade can be rheumatic processes in the myocardium, cardiosclerosis, syphilitic heart disease, interventricular septal infarction, heart defects, cardiomyopathies, myxedema, diffuse connective tissue diseases, myocarditis of various origins (autoimmune, diphtheria, thyrotoxic), amyloidosis, sarcoidosis, hemochromatosis , heart tumors, etc. With cardiac AV blockade, a partial blockade may initially be observed, however, as cardiac pathology progresses, a third-degree blockade develops.
Various surgical procedures can lead to the development of atrioventricular blockade: aortic valve replacement, plastic surgery of congenital heart defects, atrioventricular RFA of the heart, catheterization of the right side of the heart, etc.
A congenital form of atrioventricular block is quite rare in cardiology (1:20,000 newborns). In the case of congenital AV block, there is an absence of sections of the conduction system (between the atria and the AV node, between the AV node and the ventricles, or both branches of the His bundle) with the development of the corresponding level of block. In a quarter of newborns, atrioventricular block is combined with other congenital cardiac anomalies.
Among the causes of the development of atrioventricular blockades, intoxication with drugs is often found: cardiac glycosides (digitalis), β-blockers, calcium channel blockers (verapamil, diltiazem, less commonly Corinfar), antiarrhythmics (quinidine), lithium salts, some other drugs and their combinations.
Treatment
If there is 1st degree atrioventricular block and there are no diseases of the cardiovascular system, treatment is not necessary at all.
For mild manifestations, a healthy lifestyle, giving up bad habits, proper nutrition and moderate exercise can help. For neurocirculatory dystonia, water procedures can be used.
For grades 2 and 3, more careful treatment of atrioventricular block is required. It includes diagnosis and treatment of the cause of the blockade and therapy aimed at improving conductivity (M-anticholinergic blockers, glucagon, euphelin and other drugs).
Usually, after treatment, the blockade goes away, but if this does not happen, you need to think about installing a pacemaker.
Symptoms of AV block
The nature of the clinical manifestations of atrioventricular block depends on the level of conduction disturbance, the degree of blockade, etiology and severity of concomitant heart disease. Blockades that have developed at the level of the atrioventricular node and do not cause bradycardia do not manifest themselves clinically. The clinical picture of AV block with this topography of disorders develops in cases of severe bradycardia. Due to low heart rate and a drop in cardiac output during physical activity, such patients experience weakness, shortness of breath, and sometimes angina attacks. Due to decreased cerebral blood flow, dizziness, transient sensations of confusion, and fainting may occur.
With second degree atrioventricular block, patients feel a loss of the pulse wave as interruptions in the heart area. With type III AV block, Morgagni-Adams-Stokes attacks occur: a decrease in heart rate to 40 or less beats per minute, dizziness, weakness, darkening of the eyes, short-term loss of consciousness, pain in the heart, cyanosis of the face, and possibly convulsions. Congenital AV block in patients of childhood and adolescence can be asymptomatic.
Prevention
Prevention of atrioventricular (AV) heart block involves treating the underlying disease. Additionally, the patient is prescribed a cardiological diet, moderate physical and emotional stress, and cessation of smoking and alcohol consumption. It is important to follow the doctor's prescriptions and recommendations for successful therapy.
To prevent the development of the disease, it is necessary to undergo a timely examination by a cardiologist. At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, specialists will select an examination program for you and prescribe adequate treatment.
Take care of yourself and your heart!
Complications of AV block
Complications from atrioventricular blockade are mainly caused by a pronounced slowdown in rhythm that develops against the background of organic heart damage. Most often, the course of AV block is accompanied by the appearance or worsening of chronic heart failure and the development of ectopic arrhythmias, including ventricular tachycardia.
The course of complete atrioventricular block may be complicated by the development of Morgagni-Adams-Stokes attacks associated with cerebral hypoxia as a result of bradycardia. The onset of an attack may be preceded by a feeling of heat in the head, attacks of weakness and dizziness; During an attack, the patient turns pale, then cyanosis and loss of consciousness develop. At this point, the patient may require chest compressions and mechanical ventilation, since prolonged asystole or the addition of ventricular arrhythmias increases the likelihood of sudden cardiac death.
Repeated episodes of loss of consciousness in elderly patients can lead to the development or worsening of intellectual-mnestic disorders. Less commonly, with AV blockade, the development of arrhythmogenic cardiogenic shock is possible, more often in patients with myocardial infarction.
In conditions of insufficient blood supply during AV blockade, phenomena of cardiovascular failure (collapse, fainting), exacerbation of coronary heart disease, and kidney diseases are sometimes observed.
Epidemiology
Most often, this pathology is diagnosed in those who suffer from concomitant diseases of the heart and blood vessels. For example, together with myocardial infarction it is observed in 13% of cases. Mild atrioventricular block in children is recorded in 2% of all patients. Severe heart block occurs after the age of seventy. Sometimes pathology of moderate severity is diagnosed in people who do not have heart disease, this is especially true for athletes. And in 3% of cases, the disease develops due to taking certain medications. Complete atrioventricular block with subsequent death is diagnosed in 17% of cases.
Diagnosis of AV blocks
When assessing the patient's medical history in case of suspected atrioventricular block, the fact of past myocardial infarction, myocarditis, other cardiopathologies, and taking medications that interfere with atrioventricular conduction (digitalis, β-blockers, calcium channel blockers, etc.) is ascertained.
When auscultating the heart rhythm, a correct rhythm is heard, interrupted by long pauses, indicating loss of ventricular contractions, bradycardia, and the appearance of Strazhesko's cannon I tone. An increase in pulsation of the neck veins is determined compared to the carotid and radial arteries.
On the ECG, first degree AV block is manifested by a prolongation of the P-Q interval > 0.20 seconds; II degree – sinus rhythm with pauses, as a result of loss of ventricular complexes after the P wave, the appearance of Samoilov-Wenckebach complexes; III degree – a decrease in the number of ventricular complexes by 2-3 times compared to atrial complexes (from 20 to 50 per minute).
Carrying out 24-hour Holter ECG monitoring for AV blockade allows one to compare the patient’s subjective sensations with electrocardiographic changes (for example, fainting with sudden bradycardia), assess the degree of bradycardia and blockade, the relationship with the patient’s activity, medication intake, determine the presence of indications for pacemaker implantation, etc.
Using an electrophysiological study of the heart (EPS), the topography of AV block is clarified and indications for its surgical correction are determined. If there is concomitant cardiac pathology and to identify it during AV block, echocardiography, MSCT or cardiac MRI is performed.
Additional laboratory tests for AV blockade are indicated in the presence of concomitant conditions and diseases (determination of the level of electrolytes in the blood during hyperkalemia, the content of antiarrhythmics in case of overdose, enzyme activity during myocardial infarction).
Therapy methods
Atrioventricular block requires treatment only when it is diagnosed in the second or third degree. In the first degree of pathology, only observation of the patient is required. When the disease develops due to taking medications, the doctor reduces their dosage or completely eliminates it. In case of blockade as a result of organic heart damage, for example, a heart attack or myocarditis, the doctor treats with special medications, and in the future it may be necessary to install a pacemaker.
When an attack of MES develops, it is necessary to provide first aid using drugs such as Isoprenaline or Atropine. In the case of existing heart failure, medications in the form of diuretics or glycosides are suggested for atrioventricular blockade. For chronic forms of blockade, therapy is carried out using Theophylline.
Typically, conservative treatment of the underlying disease allows for complete restoration of conduction through the atrioventricular node. But sometimes a scar that forms in its area leads to a persistent signal conduction disorder. In this case, the patient requires installation of an artificial pacemaker. Also, indications for this operation are the presence of attacks of MES, chronic bradycardia, second-degree heart block of the second type or third degree, accompanied by angina, heart failure or hypertension. This surgical treatment increases the patient's chances of a full recovery and improves quality of life.
Treatment of AV blocks
With first degree atrioventricular block that occurs without clinical manifestations, only dynamic observation is possible. If AV block is caused by taking medications (cardiac glycosides, antiarrhythmic drugs, β-blockers), dose adjustment or complete discontinuation is necessary.
In case of AV blockades of cardiac origin (myocardial infarction, myocarditis, cardiosclerosis, etc.), a course of treatment with β-adrenergic stimulants (isoprenaline, orciprenaline) is carried out, and then implantation of a pacemaker is indicated.
First aid drugs for the relief of Morgagni-Adams-Stokes attacks are isoprenaline (sublingual), atropine (intravenous or subcutaneous). For symptoms of congestive heart failure, diuretics, cardiac glycosides (with caution), and vasodilators are prescribed. As symptomatic therapy for the chronic form of AV blockade, treatment is carried out with theophylline, belladonna extract, and nifedipine.
A radical method of treating AV block is the installation of an electrical pacemaker (pacemaker), which restores normal rhythm and heart rate. Indications for implantation of an endocardial pacemaker are a history of Morgagni-Adams-Stokes attacks (even a single one); ventricular rate less than 40 per minute and periods of asystole of 3 or more seconds; AV block II degree (Mobitz type II) or III degree; complete AV block, accompanied by angina pectoris, congestive heart failure, high arterial hypertension, etc. To decide on surgery, consultation with a cardiac surgeon is necessary.
How to treat
The choice of treatment method for AV heart block is determined depending on the degree of the disease. At our center, the Federal Scientific and Clinical Center of Federal Medical and Biological Agency, there are several treatment options. Usually, with 1st degree AV block, only dynamic observation is prescribed. For such cases, a therapeutic department is provided. The patient is under the constant supervision of doctors and undergoes the necessary procedures in a timely manner. For significant 2nd degree AV block and 3rd degree AV block, there is no drug therapy. For such patients, implantation of an electrical pacemaker (pacemaker) is vitally indicated.
Forecast and prevention of AV blocks
The influence of developed atrioventricular block on the patient’s future life and ability to work is determined by a number of factors and, above all, the level and degree of blockade and the underlying disease. The most serious prognosis is for grade III AV block: patients are unable to work, and the development of heart failure is noted.
The prognosis is complicated by the development of distal AV blocks due to the threat of complete blockade and rare ventricular rhythm, as well as their occurrence against the background of acute myocardial infarction. Early implantation of a pacemaker can increase the life expectancy of patients with AV block and improve their quality of life. Complete congenital atrioventricular blocks have a more favorable prognosis than acquired ones.
As a rule, atrioventricular block is caused by an underlying disease or pathological condition, so its prevention is the elimination of etiological factors (treatment of cardiac pathology, avoidance of uncontrolled use of drugs that affect the conduction of impulses, etc.). To prevent worsening of the degree of AV block, implantation of a pacemaker is indicated.
LiveJournal
Complications and consequences
With heart blocks, complications arise in the form of a slowdown in heart rate against the background of damage to an organ of an organic nature. Most often, AV block leads to chronic heart failure, arrhythmias, and tachycardias. The course of the disease is often complicated by attacks of MES, which can result in death as a result of cardiac arrest. Repeated attacks of MES in old age cause the development of the syndrome of intellectual-mnestic disorders. Cardiogenic shock, collapse, and encephalopathy can also rarely be observed.
Clinical picture
With a first-degree blockade, as a rule, the patient does not present any specific complaints. Changed health is associated with the underlying disease. In the second or third degree, circulatory disorders of a compensatory and adaptive nature occur: each contraction of the ventricles becomes larger in volume, which leads to myocardial hypertrophy. Cardiac pathology is usually accompanied by a number of symptoms:
- Bradycardia of 30 beats per minute causes insufficient blood flow to the brain, dizziness occurs, and short-term loss of consciousness is possible.
- Patients feel rare strong impulses (beats) of the heart into the chest. This is caused by the overlap of the rhythm of contractions of the atria and ventricles and the formation of single complete regular systoles.
- When listening to the patient's heart, they have the characteristic of a “cannon shot”. During examination of the neck, a pronounced pulsation of the veins is detected due to the return wave of blood into the jugular vein.
- For diagnosis, an important point is the absence of acceleration of the pulse after physical activity, or any fluctuations when holding the breath while taking a deep breath.
The distances between atrial and ventricular contractions are not changed, but are not connected into a single complex
If the blockade is caused by an inflammatory process or unfinished scarring, then all the signs are inconsistent.
In patients with pathological menopause and vegetative-vascular dystonia, the influence of the vagus nerve is pronounced. This is determined by conducting a test with Atropine. After a small dose is administered subcutaneously, the blockade is removed.
A severe manifestation of complete atrioventricular block is Morgagni-Adams-Stokes syndrome, caused in half of the cases by short-term ventricular asystole with preserved atrial flutter. The other half is represented by the outcome of flutter or ventricular fibrillation (hyperdynamic form).