According to statistics from various authors, the incidence of the disease varies within very wide limits - from 3 to 70%.
This variability is due to the lack of uniform pathomorphological criteria for diagnosis and significant differences in the material sent for research. Women of reproductive age are most often affected - this category accounts for about 97% of all patients.
The disease is always a consequence of acute inflammation, which is not completely cured. The result of this is prolonged chronic endometritis. The main threat posed by a chronic inflammatory process is infertility, so the problem is not only medical, but also social in nature. In addition to problems with conception, the pathology sharply reduces the likelihood of successful in vitro fertilization and provokes various complications during pregnancy, including premature birth.
Classification
Endometritis is classified according to stages:
- acute – occurs with severe general (intoxication) and local symptoms;
- subacute – occurs in the absence of treatment of endometritis in the acute phase against the background of weakened immune defense;
- chronic - characterized by an unexpressed clinical picture, involvement of the basal (deep) uterine layer, proliferation of the mucosa, disruption of its structure. Most often, it is chronic endometritis that leads to a woman’s infertility and miscarriage. Depending on changes in the endometrium, this stage can be hypertrophic (excessive growth of the membrane), atrophic (underdevelopment and insufficiency of glandular cells, proliferation of connective tissue). And cystic - the formation of intraendometrioid cysts.
Among patients experiencing problems with natural conception, from 12 to 68% suffer from chronic endometritis.
Among women with unsuccessful attempts to use assisted reproductive technologies, the disease occurs in approximately 60%. 70% of patients with recurrent miscarriage have a diagnosis of chronic endometritis.
Causes of chronic endometritis of the uterus
The main causes of chronic endometritis are pathogenic and opportunistic bacteria. In most cases, they enter the uterine cavity in an ascending way - from the vagina. Factors that contribute to infection of the uterine mucosa include:
- childbirth;
- surgical interventions (caesarean section and others);
- abortion (especially criminal abortion);
- period;
- intimacy during menstruation;
- any diagnostic and therapeutic procedures in the uterine cavity;
- the presence of an infectious process in the body;
- immunodeficiency states.
As a rule, when exposed to unfavorable factors, an acute pathological process develops in the inner lining of the uterus. The disease is characterized by a fairly typical clinical picture and does not present any particular difficulties in terms of diagnosis and treatment, but in some cases the process enters the chronic phase. A certain role here is played by secondary causes of chronic endometritis, or factors contributing to the transition of an acute process to a chronic one.
The main ones include:
- insensitivity of microorganisms to antibacterial agents;
- incorrectly drawn up treatment regimen;
- too late therapy;
- premature discontinuation of medications;
- independent discontinuation of medications, changes to the therapeutic plan without the consent of the attending physician;
- individual characteristics of the female body.
Against the background of all these situations, chronic endometritis may occur, the symptoms and treatment of which directly depend on the severity of the problem and the general condition of the patient.
Regulation of endometrial thickness and its changes during the menstrual cycle
The endometrium is a hormonally dependent tissue. Its condition is influenced by hormones produced by the ovaries, which prepare the mucous membrane for pregnancy. The changes that occur in the lining of the uterus constitute the uterine cycle. Its duration is the same as the ovarian cycle, but there are more phases:
- desquamation - rejection of the mucous membrane;
- regeneration – reproduction of epithelial cells and formation of the integumentary layer;
- proliferation – formation of a functional layer of the endometrium;
- secretion – the structure of the mucous membrane changes, preparing it for implantation.
Desquamation corresponds to the period of menstruation, and together with regeneration and proliferation they fit into the first phase of the ovarian cycle - follicular. During this period, under the influence of follicle-stimulating hormone, follicles mature in the ovaries, and gradually one of them becomes dominant. They secrete estradiol, the concentration of which increases at the time of ovulation.
The size of the endometrial layer depends on the phase of the uterine cycle. At the very beginning it consists only of the basal layer. It has minimal thickness, but it retains the bottoms of the glands that were removed during menstruation. Thanks to the remnants of the glands, their restoration occurs. The higher the level of estradiol becomes, the more active the division of epithelial cells occurs, and the functional layer is formed.
Changes in endometrial thickness during the menstrual cycle
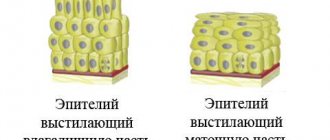
An increase in the thickness of the endometrium also occurs due to an increase in the height of the cells, and later the number of their rows: the epithelium changes from single-row to multi-row. The following changes are also observed:
- swelling of the stroma of the mucous membrane;
- increased tortuosity of blood vessels;
- the appearance of ciliated epithelial cells.
After the peak rise in estradiol, luteinizing hormone is released in the hypothalamus, and ovulation occurs in the ovaries after 12-24 hours. At the site of the burst follicle, a corpus luteum is formed, which produces progesterone. The function of this hormone is to prepare the endometrium. The mucous membrane of the uterus enters the secretory phase. Its thickness no longer increases, proliferation stops. But changes are observed in the structure of the glands:
- by day 16 of the cycle, vacuoles containing glycogen appear;
- on day 17 of the cycle, vacuoles push the nucleus towards the center of the cells;
- on the 18th day, vesicles with glycogen are located at the top of the cell, the secretion begins to be released into the lumen of the glands, and through them into the uterine cavity.
Glycogen is a versatile nutrient made up of chains of glucose. It will be used by the embryo in the first days of its existence in the uterine cavity. The endometrium also secretes trace element ions in a certain concentration, which are necessary to maintain the existence of the embryo. Therefore, the most favorable day for implantation is 6-7 days after ovulation, which corresponds to days 20-21 of the cycle.
If conception does not occur, from day 22, decidual cells appear in the mucous membrane, which gradually form couplings on the spiral arteries. Eosinophils migrate to them from the bloodstream, increasing tissue swelling. And from day 25, neutrophils appear in the endometrium, which contributes to tissue necrosis and its rejection along with menstrual blood. The main reason for rejection of the mucous layer is considered to be a sharp decrease in progesterone and estradiol due to involution of the corpus luteum.
Menstrual bleeding stops after a spasm of the vessels supplying the basal layer occurs. Small blood clots form in them, but complete fibrin deposition does not occur. After the bleeding stops, the mechanisms of cell division in the basal layer are launched, gradually blocking the vessels and promoting the growth of new ones.
Signs and symptoms of chronic uterine endometritis
Endometritis is manifested by the following symptoms:
- increased body temperature;
- vaginal discharge that is brown or bloody;
- pain above the pubis, in the lower abdomen, lower back.
Upon objective examination, the uterus is enlarged, palpation is accompanied by pain. Most often, chronic endometritis is a consequence of the acute form of the disease. The main reason for the chronicity of the process is incorrectly selected, untimely or prematurely stopped treatment. The external manifestations of the disease decrease, but the inflammatory process is not eliminated completely, which causes a number of changes in the structure and functioning of the endometrium.
Most often, the symptoms of chronic endometritis manifest themselves in waves - periods of exacerbation alternate with periods of clinical symptoms. But in some cases, even during remission, patients report moderate aching pain in the lower abdomen, irregular menstruation, and mucous discharge from the vagina. Very often, menstruation becomes excessively heavy, and miscarriages may occur in the early stages. During the period of exacerbation, intoxication symptoms of chronic endometritis occur - increased body temperature, general weakness, chills, decreased appetite, temporary loss of performance, sweating, drowsiness.
Types of endometritis
There are three types of disease according to the intensity of symptoms:
- acute type;
- subacute endometritis;
- chronic or sluggish endometritis.
The course of acute endometritis always manifests itself with severe symptoms:
- a sharp increase in body temperature to 38-40 degrees Celsius;
- signs of intoxication – headache, pain, dizziness, weakness, drowsiness;
- sharp or nagging pain in the lower abdomen and back;
- vaginal bleeding, unusual purulent or sanguineous vaginal discharge.
The gynecologist, based on the data from the patient’s survey and examination, will quickly make a diagnosis in the acute stage. On palpation, the uterus will be spherical in shape, noticeably enlarged, soft and painful when pressed.
The acute course of the disease usually causes intervention in the pelvic area: abortion, complicated childbirth, cesarean section, diagnostic procedures (hysteroscopy, curettage, probing), installation or removal of an intrauterine device. The reason in these cases will be non-compliance with the rules of septic and antiseptics during the operation, severe damage to the walls of the uterus, accumulation of blood and its clots, remains of the fertilized egg, placenta or suture material inside the organ.
Subacute endometritis is most often caused by viruses, fungi and bacteria that enter the uterine cavity, despite all natural barriers.
Endometritis does not develop in a healthy body. Damage to the body's defense mechanisms - the acidic environment of the vagina and cervical barrier - leads to the entry of pathogenic flora into the reproductive organs.
Symptoms of subacute endometritis are similar to the acute form of the disease, but are usually less pronounced.
Chronic endometritis is the result of an untreated acute and subacute disease and its transition to the chronic stage. Sometimes the chronic form develops almost unnoticed. This occurs if the symptoms of the acute form were erased due to the prophylactic use of antibacterial drugs after surgery.
The symptoms of chronic endometritis are very different from acute:
- body temperature is within normal limits or slightly above normal (36.6-37.5 degrees);
- minor periodic pain in the area of the sacrum and lower abdomen, which does not interfere with leading a normal lifestyle;
- light purulent, pink, brown or serous vaginal discharge, possibly with an unpleasant odor;
- painful menstruation;
- disruptions of the menstrual cycle (delays, complete cessation of menstruation, excessively heavy and prolonged menstruation);
- bleeding or spotting at the wrong time.
During a vaginal examination, the gynecologist will note a slight enlargement of the uterus and pain on palpation.
Diagnosing chronic endometritis is quite a difficult task for a doctor. The symptoms are similar to a huge number of other female diseases, so before making a diagnosis you will have to undergo a number of additional examinations.
Diagnosis of chronic endometritis of the uterus
Diagnosis of chronic endometritis is difficult due to the mild severity of clinical symptoms. However, using modern medicine, it is quite possible to make a diagnosis of “chronic endometritis”.
The first thing you need to do for a successful diagnosis is to undergo an examination by a gynecologist. Before examining a woman in a gynecological chair, the doctor will ask in detail about the present complaints, their nature, time of appearance, and possible provoking factors. Of great importance for the doctor is information about previous curettages, abortions, the use of intrauterine contraceptives, and hysteroscopy. During an objective examination, an enlarged uterus and discharge from the external os of the cervical canal indicate a possible pathological process. Sometimes the patient notes pain on palpation. In most cases, the appendages are unchanged, but adnexitis, an inflammation of the fallopian tubes and ovaries, is often possible.
Additional diagnosis of chronic endometritis involves conducting a number of laboratory and instrumental tests, in particular:
- general blood test;
- general urinalysis;
- biochemical blood test;
- ultrasound examination - shows the structural features of the inner lining of the uterus;
- diagnostic curettage followed by bacteriological and pathomorphological examination of the material;
- examination of vaginal discharge to identify a possible pathogen and determine its sensitivity to antibacterial agents.
If necessary, hysteroscopy, computed tomography and magnetic resonance imaging are performed, and related specialists are consulted. Thus, the gynecologist can obtain maximum information about the patient’s condition and select the most appropriate treatment.
How to treat chronic endometritis?
If endometritis has already become chronic, complex treatment cannot be avoided. This is antimicrobial, immunomodulatory and restorative therapy in combination with physiotherapeutic procedures.
Treatment of endometritis involves the need for complex therapy aimed at overcoming painful symptoms and, of course, eliminating the causes of the disease.
According to the National Cancer Institute in the USA, chronic endometritis in advanced stages leads to endometrial cancer. This occurs in obese and overweight women 2 to 4 times more often than women of normal weight. The risk of endometrial cancer increases with weight gain in adulthood, especially among women who have never used hormonal treatment.
Treatment of chronic endometritis of the uterus
Treatment of chronic endometritis is carried out in several stages. First, you need to eliminate the cause of the disease, then restore the function of the endometrium. In conclusion, every effort should be made to restore the woman’s reproductive function. First of all, treatment of chronic endometritis of any form involves the use of broad-spectrum antibiotics. Antibiotics play a particularly important role during exacerbation of the disease. It is best to select medications after receiving the results of a bacteriological study, but since it takes time, the gynecologist prescribes medications empirically, adjusting the treatment regimen after receiving sensitivity test data.
In parallel, anti-inflammatory and symptomatic therapy is used. After eliminating the main symptoms, the woman is prescribed a course of physiotherapeutic procedures and sanatorium-resort treatment for chronic endometritis.
The following procedures have a particularly strong effect:
- magnetic therapy - has an anti-inflammatory effect, reduces swelling, accelerates tissue regeneration, improves microcirculation, activates local immunity;
- UHF therapy helps to expand capillaries and improve blood supply to tissues. Indicated only during periods of exacerbation;
- electrophoresis with medications, most often absorbable, anti-inflammatory, painkillers;
- Ultrasound treatment - improves nutrition and tissue restoration.
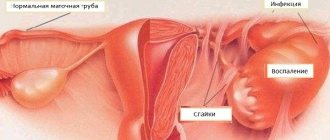
With improper or inadequate treatment, the following complications of chronic endometritis develop:
- adhesive process. Cells synthesizing collagen fibers accumulate at the site of inflammation. These are quite dense structures that are the main component of scars. By connecting with each other, the fibers form peculiar cords that connect organs and tissues. The affected structures are not able to perform their direct function, which is externally manifested by a characteristic clinical picture;
- infertility is the most common complication of chronic endometritis. With a prolonged inflammatory process, the inner lining of the uterus is infiltrated with leukocytes, blood supply deteriorates, and the functional endometrium loses sensitivity to hormones. A fertilized egg cannot successfully implant and develop in pathologically altered tissues. Even if pregnancy occurs, there is a very high risk of spontaneous miscarriage in the early stages. In addition, due to pronounced adhesions, male reproductive cells are not able to reach the egg and fertilize it;
- Irregular menstruation due to decreased sensitivity to hormones. In most cases, there are delays, long and heavy menstruation, and bleeding that occurs between periods.
If chronic endometritis is diagnosed, is it possible to get pregnant? This is what interests many women suffering from the corresponding pathology. It should be noted that there is a small chance of conception. However, due to the inflammatory process, the likelihood of its implantation into the endometrium is significantly reduced.
Endometritis is a pathology that leads to changes in the wall of the uterus. It swells and changes its functional activity. Even if the fertilized egg implants in a separate, less affected area of the endometrium, there remains a very high risk of miscarriage or problems with pregnancy.
The wall of the organ is less well supplied with blood. It contains bacteria and cellular immune factors that try to eliminate the infection. All this has an extremely adverse effect on the embryo. When the uterus becomes inflamed, it loses its contractile function, which also needs to be taken into account when planning to conceive a child. That is why most doctors believe that chronic endometritis needs to be cured, and pregnancy should be planned only after completing a full therapeutic course. This allows you to increase the chances of conception and provide optimal conditions for fetal development.
Prevention of chronic endometritis of the uterus
Prevention of chronic endometritis is, first of all, prevention of an acute inflammatory process. To prevent acute endometritis, you need to adhere to the following rules:
- observe the rules of personal hygiene;
- have a permanent sexual partner;
- avoid sexual intercourse during menstruation, at least four weeks after abortions and curettage, six weeks after childbirth;
- strictly follow the doctor’s recommendations in the postpartum period or after intrauterine interventions;
- At the first manifestations of the disease, seek medical help.
If, despite all preventive measures, it was not possible to avoid the disease, secondary prevention of chronic endometritis, aimed at preventing complications, comes to the fore. It consists of correct and complete treatment and timely preventive examinations. The AltraVita reproductive medicine clinic employs gynecologists with extensive experience. They treat their patients very carefully and carefully maintain medical confidentiality. Our doctors will draw up an individual treatment plan and monitor its effectiveness. Since chronic endometritis is a disease that often leads to infertility, gynecologists will make every effort to ensure natural conception, and, if necessary, select the optimal assisted reproductive technology and provide qualified supervision of the pregnant woman.
Causes of the disease
The entry of various microorganisms and bacteria into the uterine cavity leads to the development of an inflammatory process.
Most often, the main ways infection enters the uterine cavity are:
- failure to comply with basic rules of personal hygiene;
- frequent change of sexual partners;
- decrease in the protective functions of the female body;
- use of an intrauterine device;
- douching.
In addition, the development of uterine endometritis can occur as a result of various surgical interventions:
- abortions;
- uterine probing;
- curettage of diagnostic and therapeutic nature.
Most often, the disease is diagnosed in women who have had an abortion. The development of the inflammatory process in the uterine cavity occurs not due to non-compliance with certain rules of medical intervention, but due to a decrease in the protective barrier mechanism at the entrance to the uterine cavity.