Perthes disease is the death of the head of the femur of a non-infectious nature (in the absence of accumulations of pus and pathogenic microorganisms), which is called aseptic necrosis. This disease usually occurs between the ages of four and fourteen years. Of all the types of aseptic necrosis in children, this disease is the most common.
Mentions of Perthes disease can be found in medical records from the century before last as a specific type of childhood arthritis of the hip joint. The incidence in boys is several times higher than in girls. Perthes disease in children is a complex process with a staged structure, at the beginning of which the symptoms are almost invisible.
With timely diagnosis, treatment lasts from one and a half to two years. After the correction, almost all patients return to their normal lifestyle without any restrictions in activity.
Causes
Perthes disease in a child occurs due to a large number of reasons, so the reasons for its occurrence in one case or another can only be assumed. There are general reasons confirmed by the majority of requests:
- presence of myelodysplasia;
- displacement of the head of the femur, which is the result of injuries (bruises, blows, sprains);
- damage by viruses or microbial infections of the joint;
- hormonal changes due to puberty;
- deviations in mineral metabolism;
- genetic predisposition.
The main cause predisposing to the formation of Perthes disease is myelodysplasia. At its core, it is a congenital defect in the development of the spinal cord, with obvious or hidden manifestations and a varied and complex clinical picture, with accompanying deviations in the functioning of various body systems. If this defect is present in the child’s body, there is a decrease in the number of vessels and capillaries supplying articular tissues in the head of the femur, which disrupts the supply of organs and articular tissues with nerves and blood.
Children at risk are those who:
- have weakened immunity;
- suffered from rickets;
- eat little or no variety;
- whose family history includes infectious and allergic diseases.
Osteochondropathy of the tibia
This pathology is a severe degenerative-dystrophic process in bone tissue due to disruption of its blood supply, structure and fatty degeneration of the bone marrow. The disease is classified as polyetiological, but there are a number of main factors that increase the risk of developing necrosis:
- Injuries and dysplasia.
- Toxic effects of drugs.
- Osteopenia.
- Osteoporosis.
- Rheumatoid arthritis.
- Cardiac ischemia.
The pathological condition is manifested by pain in the area of the hip joint and groin, which can radiate to the knee, lower back, and sacrum. As the disease progresses, the discomfort becomes permanent. The patient begins to limp, the affected limb loses its mobility due to muscle atrophy.
Diagnosis of aseptic necrosis of the tibia consists of plain radiography, MRI, CT, and soft tissue scintigraphy. Treatment is conservative: physiotherapy, medication, exercise therapy. Surgery is possible for serious degenerative changes.
Osteochondropathy of the fibula
The fibula is a tubular, thin and long part of the lower leg. It connects to the tibia and consists of a body and two ends. Serves as an external stabilizer of the ankle joint.
Degenerative-dystrophic lesions of the fibula often occur against the background of necrosis of the pelvic bones and are manifested by the following signs: widening of the joint space, decreased height of the epiphyses, and death of bone tissue.
The disease causes pain when moving and palpating the affected area. The pathology is characterized by a cyclical course. Its total duration takes from 2 to 4 years. The treatment is complex: medications, physiotherapy, exercise therapy, mineral complexes.
Osteochondropathy of the tibial tuberosity
Osgood-Schlatter disease is one of the common forms of avascular necrosis in children. Damage to the tibial tuberosity is diagnosed in patients 10-18 years old who are actively involved in sports. The disease can be either unilateral or with symmetrical damage to both limbs.
The main cause of the disorder is frequent injuries and increased physical activity. The degenerative-dystrophic process is manifested by the following symptoms:
- Swelling of the lesion.
- Local pain on palpation and flexion of the limb.
- Upon palpation, a hard bone growth is determined.
In the first stages, discomfort is periodic. As the pain progresses, it becomes persistent and intensifies when walking or squatting. Due to edema, there is a moderate deformity of the anterior proximal part of the leg. This is clearly visible from the side with the knee joint bent. The tuberosity can be an elastic or dense bone structure.
When making a diagnosis, radiological signs of pathology are taken into account. There is a change in the structure and contours of the tibial tuberosity - light areas alternate with dark and structureless ones, and a marginal cavity is formed. Differentiation is carried out with recurrent subluxation of the patella, tumors of cartilage tissue, avulsion fracture of the tibial tuberosity, osteomyelitis, and infrapatellar bursitis. Treatment consists of limiting flexion movements in the knee joints of the affected limb. Patients are prescribed painkillers, bone tissue and body strengthening medications. Physiotherapy is aimed at stimulating regenerative processes. Surgical intervention is performed extremely rarely, since there is a risk of damage to the growth zone and the development of synostosis. The disease lasts 1-1.5 years and ends with restoration of the bone structure. In advanced cases, deformation of the lesion may occur.
Symptoms
At first, the child’s symptoms may be minor and manifest only in mild dull pain in the joint when moving and slight disturbances in gait, including a barely noticeable limp. The symptoms of Perthes disease are influenced by the degree of tissue death and the size of the lesion. At the onset of the disease, symptoms are practically unnoticeable, and the child continues to lead his daily lifestyle. If there is no further treatment, the child may experience abnormalities in the bone anatomy, which determine the following symptoms:
- swelling in the joint area;
- inability to turn the leg outward;
- weakness of the buttock muscles;
- increased pain when moving;
- severe lameness;
- difficulty in moving the joint;
- elevated temperature;
- blood test shows increased ESR, lymphocytosis and leukocytosis;
- autonomic disorders such as pale feet, coldness, excessive sweating, numbness of the skin;
- decreased pulse rate in the extremities;
- wrinkled skin on the feet.
Forecast
The outcome of Perthes disease depends on the size and location of the area of necrosis. With a small lesion, full recovery is possible. With extensive destruction, the head breaks up into several separate fragments and after fusion can acquire an irregular shape: flatten, protrude beyond the edge of the articular cavity. Violation of the normal anatomical relationships between the head and the acetabulum in such cases becomes the cause of further aggravation of pathological changes: the formation of contractures, limited support and rapid development of severe coxarthrosis.
Stages of the disease
First, synovitis forms - an inflammatory process in the synovial membrane, accompanied by the transformation of fluid and its accumulation in the joint cavity. If the blood circulation process is disrupted for a long time, then the thigh itself is affected, in which the bone marrow and cartilage may be affected.
Perthes disease in children occurs in five stages, successively replacing each other:
- Necrosis of spongy bone substance and bone marrow occurs.
- The head of the bone is refracted.
- There is a decrease in the size of the femoral neck due to the resorption of dead tissue.
- Thanks to calcium salts and new formed bone tissue, bone reconstruction occurs.
- Stage the structure of the spongy substance is restored.
The above classification helps to clearly outline the changes in the joint during the course of the disease and allows us to roughly estimate the duration and severity of the disease. According to practical data, the formation of each stage takes from five to six months.
Additional facts
Perthes disease is a pathological process characterized by impaired blood supply and subsequent necrosis of the femoral head. It is a fairly common disease and accounts for about 17% of the total number of osteochondropathy. Children aged 3 to 14 years are affected. Boys get sick 5-6 times more often than girls, but girls tend to have a more severe course. Both unilateral and bilateral damage is possible, with the second joint usually suffering less and recovering better.
Diagnostics
Treatment of Peters disease in a child is prescribed by orthopedic doctors, determining the stage of the disease using the following diagnostic procedures:
- ultrasound examination (ultrasound);
- radiography of the knee and hip extremities in several projections;
- radiology diagnostics;
- magnetic resonance imaging (MRI).
It is most difficult to make a diagnosis in the initial stage, when the symptoms are practically invisible and even radiography is not able to accurately determine the presence of an inflammatory process. In 55% of calls, the process is diagnosed at the second or third stage, when deformation is present. To identify the first stage, an ultrasound or, most effectively, an MRI is performed.
The concept of osteochondropathy, its causes
Osteochondropathy is necrosis (death) of a section of bone due to various reasons. The cartilage tissue adjacent to the bone also suffers. The disease is chronic, gradually causing deformation of bones and joints; with age, arthrosis and limited mobility (contracture) develop. Children and adolescents aged 5-14 years are most often affected, but osteochondropathy also occurs in adults. In the structure of orthopedic morbidity, it accounts for 2.5-3% of the total number of visits.
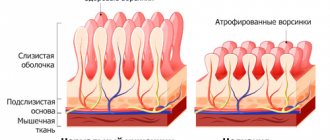
Impaired blood flow through the arteries leading to the epiphysis of the bone leads to the development of aseptic necrosis of the femur and osteochondropathy
The cause of osteochondropathy is a violation of blood circulation in the area of the bone near the joint (epiphysis), leading to its necrosis and associated complications - deformation, fractures. The following factors can lead to circulatory disorders:
- Injuries: bruises, hematomas, damage to soft tissue, bone, cartilage.
- Hormonal and metabolic disorders, mainly during puberty (adolescence), lack of phosphorus and calcium salts.
- Lack of protein in the diet (for example, vegetarians).
- Increased bone growth when it outstrips vascular development.
- Excessive functional load on joints, especially in childhood and adolescence.
- A sedentary lifestyle (hypodynamia), leading to blood stagnation.
- Congenital anomalies of the development of the osteoarticular system.
- Excess weight, which increases stress on bones and joints.
- Hereditary predisposition (feature of bone structure).
Treatment
Age and stage directly affect the treatment of Perthes disease. Immediately after the diagnosis is made, bed rest is prescribed with adhesive traction of the affected leg, which completely eliminates stress, but preserves rotational and flexion movements, which are elements of therapeutic exercises. In addition, the orthopedic doctor prescribes other measures for the treatment of Perthes disease in a child:
- with the help of orthopedic products (functional splints or plaster casts) the centralization of the femoral head is ensured (its complete “immersion” in the acetabulum);
- massage, therapeutic exercises, physiotherapeutic procedures;
- treatment with osteoprotectors and chondroprotectors, as well as non-steroidal anti-inflammatory drugs;
- vitamin therapy.
Treatment of the disease with non-surgical methods takes quite a long time and can last from two to four years.
Surgical treatment is used in extremely rare cases. In advanced stages, restoration of the correct position of the bones in the hip joint occurs surgically. Just as with non-operative treatment, the femoral head is “immersed” in the acetabulum, then this position is fixed with bolts and plates, which are removed after the joint is restored. Massages and therapeutic exercises are prescribed after removing the fixing bandage.
It is important to notice in time the onset of a dangerous disease process in a child. Therefore, it is necessary to be vigilant about your child’s well-being, and if signs of illness occur, consult a doctor immediately.
This disease is eliminated relatively quickly in the initial stages, but as the disease progresses, a much longer period is needed to cope with it. If treatment is not started in a timely manner, the disease can lead to deforming arthrosis of the joint. Watch out for the first symptoms of Perthes disease.
Perthes disease in children: treatment, symptoms, causes
Perthes disease is diagnosed 5 times more often in boys aged 3-14 years than in girls. Usually only the right hip joint is damaged, but cases of bilateral damage are not uncommon.
Clinically, the pathology is manifested by pain, aggravated by walking, limited mobility, and subsequently atrophy of the gluteal muscles.
Treatment of Perthes disease is predominantly conservative, using means to improve blood circulation, orthopedic devices, exercise therapy, massage, and physiotherapy.
What is Legg Calve Perthes disease?
It is important to know! Doctors are shocked: “An effective and affordable remedy for joint pain exists...” Read more…
Perthes disease is a degenerative pathology affecting the femur and hip joint (HJ), belonging to the group of osteochondropathy. The trigger for the development of the disease is a circulatory disorder in the hip joint, often against the background of deteriorating innervation.
The joint tissues are constantly experiencing a deficiency of nutrients and oxygen. Because of this, some of the tissue begins to gradually die, which leads to the formation of an area of aseptic necrosis. This process is not accompanied by inflammation, including infectious origin.
Features of the disease in children
Perthes disease develops in childhood or adolescence. Its danger lies in its asymptomatic course in the initial stages, therefore, when visiting a doctor, significant damage to the cartilaginous and bone structures of the hip joint is often diagnosed.
Children with myelodysplasia are especially susceptible to the disease. This is the name for congenital underdevelopment of the spinal cord in the lumbar spine.
This is a fairly common pathology, which does not manifest itself in any way in some children, while in others it leads to various orthopedic disorders.
Stages of pathology
In orthopedics, the classification of Perthes disease is used depending on the pathological processes occurring in the hip joint. The stage of the disease is established using the results of an X-ray examination. Each of them is characterized by specific clinical manifestations. There are 5 stages of Perthes disease in total:
- the first is a deterioration or complete cessation of blood supply to tissues with substances necessary for their functioning, leading to the formation of a necrotic aseptic focus;
- second - in the area of damaged structures of the hip joint, a secondary fracture of the femoral head occurs;
- third - necrotic tissue gradually begins to dissolve, which causes shortening of the femoral neck;
- fourth - at the sites of necrotic changes, connective tissues devoid of functional activity grow;
- fifth - connective tissues are replaced by bone, the fracture heals.
The stage of Perthes disease always becomes the determining criterion when an orthopedist chooses treatment tactics. Most damage can be repaired conservatively, but significant damage requires surgical treatment.
Reasons for development
The causes of Perthes disease have not yet been established, but there are several theories to explain its origin. The most reliable version is that pathology occurs due to a combination of certain factors - initial predisposition, metabolic disorders and environmental influences. The development of Perthes disease is provoked by:
- previous minor injuries - bruises, damage to the ligamentous-tendon apparatus;
- inflammatory pathologies of the hip joint (transient synovitis), caused by the penetration of pathogenic bacteria and viruses into the joint cavity;
- hormonal changes in the body;
- disturbances in the metabolism of minerals involved in the formation of bone tissue - calcium, phosphorus, copper and others.
In some cases, a hereditary predisposition can be traced. Perthes disease most often affects children whose parents were previously diagnosed with structural features of the hip joint or myelodysplasia.
Symptoms and signs
At the initial stage of development of Perthes disease, only mild discomfort occurs when walking. An interesting feature is that pain may first appear in the knee joint on the affected side. Only after some time they are felt specifically in the hip joint.
Due to pain, as well as the gradual destruction of bone tissue, the child’s gait changes. He limps, falling on the sore limb.
Often the symptoms are so mild that parents mistake the occasional soreness for muscle strain after sports training or prolonged standing.
As the head of the femur is destroyed and its impression fracture occurs, the pain increases significantly, and pronounced lameness appears. Swelling of the skin over the hip joint is observed, and difficulties arise with rotation, flexion, and extension in the hip joint.
Autonomic disorders are also observed - the foot becomes cold, pale, and wet. In weakened children, body temperature may rise to subfebrile levels (37.1-38.0 °C).
Healing of the fracture results in relief of pain, but lameness and stiffness often persist.
Treatment options
“Doctors are hiding the truth!”
Even “advanced” joint problems can be cured at home! Just remember to apply this once a day...
>
Therapy for Perthes disease always begins with hospitalization of the child in the orthopedic department with further outpatient treatment. The exception is children under 6 years of age, for whom doctors adhere to observation tactics.
A long-term (up to 4 years), step-by-step, comprehensive approach to treatment is practiced.
It is necessary to maintain a gentle motor regimen, wear orthopedic devices to reduce the load on the hip joint, and in severe cases, apply a plaster cast.
Children with Perthes disease experience a significant decrease in physical activity, which often leads to excess weight gain. A dietary diet is recommended, excluding foods containing high amounts of fat and simple carbohydrates. Nutritionists help create a diet with sufficient intake of proteins, calcium, fat- and water-soluble vitamins into the child’s body.
Massage, physiotherapy, exercise therapy
In the treatment of Perthes disease, various types of massage are used - classical, vacuum, acupuncture. After 15-20 sessions, there is an increase in the range of motion in the hip joint and a decrease in pain.
Massage is always combined in the treatment of pathology with physiotherapeutic procedures: magnetotherapy, UHF therapy, applications with ozokerite and paraffin.
Hyperbaric oxygen therapy, sanatorium-resort treatment with mud, mineral waters, electrophoresis with solutions of calcium and phosphorus salts, and chondroprotectors are indicated.
After severe pain has been relieved, daily physical therapy and gymnastics classes are carried out. Regular training helps strengthen the hip muscles, improve gait and posture.
Surgical intervention
To eliminate biomechanical disorders in the joint in the late stages of Perthes disease, surgical treatment methods are used. Indications for surgery in children over 6 years of age include severe hip joint deformity and hip subluxation. Rotational transposition of the acetabulum or corrective medializing osteotomy of the femur is performed.
Complications and consequences
One of the complications of Perthes disease is shortening of the leg, which leads to lameness, improper distribution of loads on the symmetrical hip joint, knee and ankle joints, and spine. In the future, this can lead to their involvement in the destructive and degenerative process.
Prognosis and disability
With timely detection of pathology with minor destruction of the femoral head, the prognosis is favorable.
If it has already broken up into separate fragments, then after fusion its configuration changes.
As a result of the discrepancy between the femoral head and the acetabulum, pathological changes are aggravated with the formation of contractures and the rapid development of deforming osteoarthritis of the hip joint (coxarthrosis).
Mild (insignificantly expressed) dysfunctions of the hip joint are not grounds for establishing disability. Children with Perthes disease, even stage 4, are not always recognized as disabled. To assign a specific group, the rate of destruction of the femoral head, preserved range of motion, shortening of the leg, and signs of coxarthrosis are assessed.
Preventive actions
Prevention of Perthes disease consists of eliminating traumatic situations and excessive loads on the hip joint. When identifying a predisposition to the development of the disease, pediatric orthopedists recommend regular exercise therapy, taking vitamins and microelements, and conducting an annual medical examination, including x-rays.
- Joint pain limits your movements and full life...
- You are worried about discomfort, crunching and systematic pain...
- You may have tried a bunch of medications, creams and ointments...
- But judging by the fact that you are reading these lines, they did not help you much...
Source: https://sustavlive.ru/drugie-bolezni/bolezn-pertesa-u-detej.html
Osteochondropathy of the femoral head (Legg-Calvé-Peters disease)
In modern literature, an opinion is expressed about the dysplastic nature of the pathology, according to which the cause of vascular disorders of the femoral head is the pathological orientation of the components of the hip joint. In this case, disturbances of arterial and venous circulation are detected in the entire lower limb, and not just in the area of the hip joint.
Clinic.
Osteochondropathy of the femoral head develops slowly, initially asymptomatically, which makes it difficult to diagnose the disease in the early stages of the development of the process. Fatigue appears when walking, mild lameness
Over time, hypotrophy of the muscles of the thigh and gluteal region increases, and movement is limited, especially abduction and internal rotation. Children, as a rule, do not pay attention to these “minor” symptoms of the symptom complex that appears
The first signs of the disease are pain and mild lameness, which force the patient to see a doctor. The pain is localized in the groin and is often paroxysmal in nature, alternating with light intervals. Moreover, in the initial stage, in 75% of children, pain is localized not only in the hip joint, but radiates to the knee joint (so-called “referred” pain). Shortening of the limb occurs, which at first is apparent (due to flexion-adduction contracture in the hip joint). With the progression of the process and flattening of the head of the femur, as well as in connection with its developing subluxation, a true shortening of the femur appears by 2-3 cm. The greater trochanter on the affected side moves above the Roser-Nelaton line. Sometimes a positive Trendelenburg symptom, weakness of the gluteal muscle group, is detected. If treated incorrectly, the pathological process ends with deformation of the head and the development of arthrosis with persistent pain and dysfunction of the hip joint.
X-ray examination
helps in making a diagnosis. For comparative analysis, X-rays of both hip joints are taken. The most complete information about the localization and extent of pathological changes in the femoral head is provided by computed tomography of the hip joints.
Changes in radiographs depend on the stage of the process.
In stage 1, there are no changes or osteoporosis of the femoral head, heterogeneity and spotting of the femoral neck, and some widening of the joint gap are detected.
In stage II (impression fracture), the head of the femur loses its characteristic trabecular structure, and the femoral neck becomes more osteoporotic. The joint space clearly widens compared to a healthy hip joint. The femoral head is deformed, loses its usual spherical shape, becomes denser, and its “false osteosclerosis” is revealed (due to the impression, there is more compacted bone substance per unit area of the head).
In stage III (fragmentation of the epiphysis), the joint space is still widened, the head is flattened and, as it were, divided into separate lumps or irregularly shaped small focal fragments.
In stage IV (reparation), the epiphysis is completely replaced by newly formed bone. The structural restructuring and restoration of the shape of the femoral head and neck is completed. The joint space narrows and approaches normal in size. If the treatment was correct, the shape of the restored head differs slightly from spherical. Otherwise, a mushroom-shaped head with a shortened, widened neck is formed. Signs of coxarthrosis are revealed.