Main symptoms:
- Muscle pain
- Joint pain
- Respiratory failure
- Exhaustion
- Heart rhythm disturbance
- Inability to perform physical activities
- Dyspnea
- Chills
- Fever
- Low blood pressure
- Loss of appetite
- Weakness
- Weight loss
- Dry cough
- Fatigue
Doctors talk about interstitial pneumonia when a person’s inflammation in the lungs affects the interstitium, located in the partitions between the blood vessels and alveoli. As a result of the inflammatory process and edema, gas exchange in the affected organ is disrupted, which causes severe symptoms. Idiopathic interstitial pneumonia is not one disease, but a group of pathologies in which diffuse changes develop in the interstitial tissue.
- Classification
- Clinic
- Diagnostics
- Treatment
- Complications
Symptoms
There are several common symptoms that unite all types of interstitial pneumonia:
- cough - usually a paroxysmal cough, dry, unproductive, sometimes it is possible to release a small amount of mucous or mucopurulent sputum;
- shortness of breath - worries all patients, but has different severity;
- symptoms of general weakness and malaise.
Nonspecific
The onset of nonspecific interstitial pneumonia is gradual, with symptoms present for many years and progressing over time. Patients also complain of weight loss, constant physical weakness and poor exercise tolerance.
Diagnosis of the disease takes time, and it is often possible to establish the correct diagnosis only 3-5 years after the onset of the disease. Men and women over 40 years of age are more likely to get sick; smokers and people who already suffer from connective tissue diseases are more predisposed to NIP.
Using radiography, symmetrical lung lesions in the periphery (“ground glass”) are determined.
Acute
This type of pneumonia begins acutely, flu-like - the temperature rises, chills and muscle pain occur. Severe shortness of breath develops very quickly, which leads to respiratory failure and in severe cases requires mechanical ventilation. The course of the disease is similar to adult respiratory distress syndrome; X-rays show bilateral diffuse darkening of the lungs characteristic of this syndrome.
The prognosis is unfavorable, with a high mortality rate.
Cryptogenic organizing pulmonary inflammation
It also has a flu-like onset. The inflammatory process extends not only to the interstitium, but also to the alveolar tissue. On auscultation, you can hear crepitus, characteristic of lobar pneumonia, so the disease is often treated unsuccessfully with antibiotics.
The prognosis is favorable; with adequate treatment, recovery occurs within 3-4 months.
Desquamative
A rather rare type of pneumonia, it occurs more often in male smokers over 40 years of age. The disease progresses gradually, and the bronchioles and alveoli are involved in the inflammatory process.
The appearance of “frosted glass” on an x-ray is characteristic. The prognosis is favorable, complete recovery is possible.
Lymphoid
A gradually developing disease that is rare and more common in older women. In addition to the typical symptoms of cough and shortness of breath, fever, joint pain, and weight loss may occur.
During the examination, alveolar-interstitial infiltrates are revealed. The prognosis is favorable.
Idiopathic pulmonary fibrosis
A disease with a gradual onset and prolonged increase in symptoms. On auscultation, bilateral crepitus is heard, and on x-ray there is a “ground glass” pattern.
Respiratory bronchiolitis
Associated with smokers and characterized by damage to the small airways (bronchioles). Symptoms are nonspecific.
Possible complications of interstitial pneumonia:
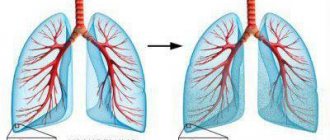
- The development of pulmonary fibrosis is a pathological replacement of normal lung tissue with connective tissue that occurs during a long course of the disease. As a result, elasticity and gas exchange are disrupted.
- The addition of a bacterial infection occurs due to congestion in the lungs and general exhaustion of the body. Abscesses, empyema may occur, and distant purulent metastases may develop.
- Respiratory failure is a consequence of pulmonary fibrosis. It manifests itself as a decrease in tolerance to physical activity, cyanosis, and symptoms of “drumsticks” and “watch glasses”.
- Heart failure - due to respiratory failure, hypertrophy of the right ventricle develops, the so-called “pulmonary heart”.
- Lung cancer: occurs in the later stages of the disease as a consequence of prolonged action of inflammatory factors, especially often observed in patients who smoke.
Kinds
The division of interstitial pneumonia into groups is based on the morphological changes that occur in the lung tissues. According to them, the following types are distinguished:
- nonspecific interstitial pneumonia;
- cryptogenic organizing pneumonia;
- desquamative;
- lymphoid;
- respiratory bronchiolitis;
- acute interstitial pneumonia;
- idiopathic pulmonary fibrosis.
The correct morphological diagnosis can only be established with the help of a lung biopsy, which is done openly or during thoracoscopy. Most often, due to the severe general condition of patients, this diagnostic method is not used.
Right-sided pneumonia in adults and children: causes, symptoms and treatment
Pneumonia is an acute inflammation of the lungs due to damage to the lung tissue by viruses and bacteria. Right-sided pneumonia is the most common and occurs more often than left-sided pneumonia. The lesion is usually located in the lower lobe of the right lung, due to the anatomical feature of the respiratory organs.
The bronchus on the right side is located at an angle and facilitates the penetration and accumulation of bacteria in it. Reproduction of pneumococcus and staphylococcus occurs quickly, so the course of the disease increases; if not treated in a timely manner, complications may arise and death may occur.
Pneumonia is contagious and is transmitted through contact with a sick person through airborne droplets. The etiology of the disease can be different:
- development of a viral infection;
- bacterial damage: staphylococcus, pneumococcus;
- chlamydia infection;
- progressive candidiasis;
- mixed pathogen.
Depending on the type of pathogen, treatment of the disease is prescribed.
Types of pneumonia
Healthy lungs
Right-sided pneumonia is divided into several types depending on the clinical picture:
- lobar;
- focal;
- interstitial;
- purulent.
The most dangerous type of pneumonia is purulent; it is difficult to treat and is more often fatal. In addition, pneumonia is classified according to the localization of the inflammation process:
- focal - if the inflammation process is located in one focus or several;
- segmental - indicates damage to one segment of the lung or several;
- lobar – inflammation of one lobe of the lung, several lobes may be affected;
- confluent - advanced focal pneumonia, in which several lesions turn into one large lesion;
- total or polysegmental pneumonia is a form of inflammation in which the entire lung becomes inflamed;
- hilar - the most difficult form of pneumonia to diagnose, mainly of the right lung.
Right-sided pneumonia is divided into:
- upper lobe;
- middle lobe;
- lower lobe.
Lower lobe pneumonia is accompanied by high fever, chills, severe cough with viscous sputum and chest pain on the right side. It may occur with mild symptoms, which makes diagnosis difficult. The cause is usually a bacterial infection and Haemophilus influenzae.
Right-sided middle lobe pneumonia develops in the middle lobe of the right lung and affects the pleura. It always begins acutely, with all the symptoms.
Upper lobe pneumonia affects 1-3 segments of the lung, the course of the disease is milder than with other types, the main symptoms appear after 2-3 days.
Right-sided polysegmental pneumonia
This form of pneumonia is the most dangerous. It develops quickly, affects the entire lung, contributes to the development of oxygen starvation and can be fatal. Inflammation of the epithelium of the lung can develop into pleurisy, causing breathing problems.
The reasons for the development of polysegmental pneumonia are different:
- bacterial infection in the form of staphylococcus, pneumococcus, chlamydia;
- a viral infection that can enter the lungs during other diseases;
- fungi and parasites.
With right-sided polysegmental pneumonia in children, pulmonary edema very quickly develops, the immune system cannot cope with bacteria, a malfunction occurs, and the immune system begins to destroy its own proteins.
The symptoms are always vivid, the course of the disease is acute:
- high temperature up to 400C, does not subside for several days;
- chills, fever, the patient may be delirious;
- headache and dizziness;
- severe intoxication of the body;
- shortness of breath, wheezing;
- general weakness;
- joint pain;
- severe lingering cough with copious sputum production.
If chest pain appears on the right, this indicates inflammation of the pleura. The pain is always severe and occurs not only when breathing and coughing, but also during sudden movements.
Folk remedies
Of course, traditional medicine recipes are not capable of ridding a patient of his illness. But still, doctors recommend using them as additional therapy. Some recipes help remove mucus and restore respiratory function. Let's take a closer look:
- Licorice root must be placed in water and brought to a boil. The resulting liquid is cooled to room temperature. It is recommended to drink 1/3 cup of the decoction three times a day.
- Peppermint and thyme are finely chopped with a knife and poured with vegetable oil. Leave in a dark place for about a week. Rub the oil on your back and chest every night.
- St. John's wort leaves are steamed with boiling water. Leave for at least 3 hours. The decoction is taken in a glass throughout the day.
- If the patient is bothered by a dry cough with a sore throat, warm milk with liquid honey (at the rate of 1 tablespoon per glass of liquid) helps.
It is important! You can take traditional medicine only at normal body temperature. Specialist consultation is also required.
Clinic
Taking into account the type of pathology, its various clinical manifestations are distinguished. The main symptoms inherent in pathology of any type are:
- dyspnea;
- general weakness;
- cough.
All these symptoms have a certain severity and character, depending on the stage of the disease. For example, the most common disease, nonspecific interstitial pneumonia, can last several years and be asymptomatic. Initially, patients complain only of constant fatigue, loss of appetite, and with it comes weight loss, as well as the inability to perform even minor physical activity. It is possible to diagnose the disease only several years after its onset, and smokers are predisposed to it, so they should be periodically checked for this pathology by X-ray examination.
The acute form of this pneumonia begins with fever and chills. And due to the fact that shortness of breath appears in the shortest possible time and respiratory failure develops, the prognosis for this form of the disease is extremely unfavorable. Patients often require mechanical ventilation, and the mortality rate is more than 50%.
Cryptogenic pneumonia also begins acutely, with flu-like symptoms. The person complains of weakness and fatigue, there is an increase in temperature, and muscle pain appears. In addition, the patient develops a dry cough. In a word, the symptoms are very similar to ordinary pneumonia, and due to an erroneous diagnosis, a person with this pathology may be prescribed antibiotics that do not affect his well-being in any way.
Lymphoid and desquamative forms of this disease are quite rare. The lymphoid type most often affects women over the age of 40, while the desquamative type affects men of the same age who smoke. In this case, lymphoid symptoms develop over the years - shortness of breath, dry cough, joint pain, anemia. And with desquamative symptoms, symptoms develop over several months. Patients complain of a dry cough and shortness of breath.
Idiopathic pulmonary syndrome is quite common. The patient has been complaining of weakness and myalgia for many years, he has shortness of breath and a mild dry cough, and also has arrhythmias. If this disease is neglected, complications may develop, including complete depletion of the body.
Respiratory bronchiolitis is a disease that affects long-term smokers. In the case of this pathology, not only the interstitium is affected, but also the bronchioles, however, the symptoms are erased, and it can be difficult to establish a diagnosis.
If we talk about the symptoms of the chronic form of this disease, they are identical to those described above, but do not manifest themselves clearly, and the disease develops over the years, leading to the development of changes in the structure of the lung tissue.
Separately, it should be said about the development of this pathology in childhood. Interstitial pneumonia in children has an acute and severe course, like the acute form of pneumonia in adults, and its symptoms are extremely pronounced. The onset of the disease is often not associated with catarrhal manifestations - shortness of breath is observed, which rapidly increases, leading to respiratory failure. Children also develop symptoms such as high fever that does not subside for more than a week, a drop in blood pressure and the development of arrhythmia. The cough in children is not pronounced; a small amount of sputum, which has a grayish-greenish color, may be released.
Unfortunately, this pathology in children often leads to the development of complications such as pulmonary edema and emphysema, which worsens the prognosis.
Features of interstitial inflammation in different age categories
Interstitial pneumonia in children is characterized by the presence of prolonged febrile fever, rapid development of shortness of breath and respiratory failure, as well as the addition of complications in the form of myocarditis, emphysema and pulmonary edema, which are accompanied by a drop in blood pressure and arrhythmia. The cough is mild, there are no respiratory symptoms.
There are no special features in elderly patients, since this inflammation of the interstitium is typical specifically for people over 40 years of age.
Treatment
Treatment is difficult. Periodic therapeutic bronchoscopy followed by the use of several groups of drugs is indicated.
Among them:
- Antibiotics. The main method of combating interstitial pneumonia. The use of antibiotics with the broadest spectrum of action is required. However, their prescription is practiced based on the results of bacteriological culture of sputum on nutrient media.
- Anti-inflammatory non-steroidal origin. Help relieve generalized pneumonia.
- Bronchodilators. Normalize breathing, relieve bronchospasm.
Otherwise, drugs are prescribed at the discretion of the specialist.
Treatment of pneumonia
Making a diagnosis in the early development of pneumonia plays a big role in achieving a positive result in the treatment of pulmonary pathology. Therapy for pneumonia is based on stopping the inflammatory process.
The following types of medications are used:
- cytostatic agents;
- hormonal medications;
- antibacterial drugs;
- antifibrotic agents;
- antioxidants;
- vitamins;
- cardiac glycosides.
Oxygen therapy is actively used. Treatment with medications is carried out for a long time, from 3 months to several years, with mandatory monitoring of effectiveness after a certain time.
Idiopathic interstitial pneumonia: treatment, x-ray signs and symptoms
Interstitial pneumonia is an inflammation of the lung tissues, affecting mainly the alveolar walls, endothelium, capillaries and fibrous tissues of the lung parenchyma.
This term refers to a whole group of inflammatory processes in the interstitial tissue of the lungs of unknown origin. It is diagnosed in patients of different ages and genders: both adults and children can get sick. Often the outcome of the disease is pneumofibrosis.
The most characteristic manifestations of the pathology are progressive shortness of breath and deterioration of respiratory function.
Causes of the disease
Researchers have not precisely established the mechanisms of origin of this disease, so it is called idiopathic interstitial pneumonia. There is an opinion that the disease can begin due to a disorder of immunological self-regulation, and the impetus for its development is the appearance of an antigen, to which the immune system reacts by actively producing antibodies.
Provoking factors for the development of this severe pathology can be:
- pathogens - cytomegaloviruses, herpesviruses, viruses that cause respiratory infections, some types of bacteria (mycoplasma, chlamydia, legionella, parasitic microorganisms: rickettsia, pneumocystis);
- inhalation of certain types of dust particles;
- long-term smoking (the disease can also develop in those who have given up this bad habit); Cytomegaloviruses
- immunodeficiency conditions, for example, HIV and AIDS, especially in early childhood;
- the presence of certain autoimmune pathologies, for example, Sjögren’s disease (connective tissues are affected, involving the exocrine glands in the pathological process);
- some rheumatic diseases that occur with damage to connective tissue;
- drug treatment with certain drugs (antiarrhythmic and antirheumatic).
Symptoms
All forms of the disease are accompanied by a number of common symptoms. Among them:
Dry cough
- cough (dry, unproductive);
- shortness of breath (at the initial stages of development of the pathology, it occurs during physical activity, and as it progresses, it manifests itself even in a calm state);
- difficulty breathing, inability to breathe fully, feeling of lack of air;
- pain in the affected area, sometimes very intense, tending to intensify when trying to breathe deeply;
- manifestations of bronchial obstruction (most often accompany the desquamative form of the disease);
- febrile phenomena (characteristic of cryptogenic, nonspecific and lymphoid forms);
- sleep disorders;
- high fatigue with minor loads;
- loss of appetite, weight loss.
The acute form is characterized by a sudden onset and rapid development, symptoms of respiratory failure rapidly increase, and more than 50% of patients die. Idiopathic pulmonary fibrosis, on the contrary, begins unnoticed, and symptoms increase rather slowly. When the pathological process begins to progress, the patient experiences respiratory dysfunction and pulmonary hypertension.
Prognosis and prevention
The prognosis for this pathology depends on the form in which it occurs, as well as on how pronounced the fibrous changes in the lung tissue are.
On average, people live with this disease for about five years, but if it occurs in the form of idiopathic pulmonary fibrosis, complicated by sclerosis of lung tissue and insufficient function of the respiratory and cardiovascular systems, then the prospects worsen significantly, survival does not exceed three years.
Acute interstitial pneumonia is a serious and dangerous disease, which, even with early detection and adequate treatment, leads to death in more than half of the diagnosed cases.
With nonspecific interstitial pneumonia, it is possible to achieve improvement in clinical parameters and stabilization of the patient’s condition in 70-75% of cases. In a third of cases, the life prognosis is estimated at 10 years.
Desquamative interstitial pneumonia can be stabilized in 65% of patients, more than 90% live up to 10 years, 60% - five years. Sometimes, with the help of therapy, it is possible to achieve stable remission.
With lymphoid and cryptogenic forms, the prognosis is usually favorable.
Prevention of interstitial lung diseases consists of quitting smoking, regular vaccinations against influenza and pneumococcal infections, preventing bacterial infections, and eliminating the influence of harmful and dangerous factors.
Which method of diagnosing nonspecific interstitial pneumonitis to choose: MRI, CT, X-ray
Selection Methods
- CT.
Is a chest x-ray used for nonspecific interstitial pneumonitis?
- With interstitial pneumonitis, a wide range of changes is detected;
- most often nodular changes in the pulmonary parenchyma are detected.
What will MSCT images of the lungs show in nonspecific interstitial pneumonitis?
- Wide range of changes: diffuse or nodular ground-glass opacities
- Irregular grid or linear shadows
- Micronodules
- Bronchiectasis and bronchiolectasis
- Minimally pronounced “honeycomb” type changes
- Symmetrical changes with predominant localization in the peripheral, basal and subpleural parts of the lungs
- No difference in the severity of changes in the basal and apical segments (absence of an apicobasal gradient).
Distinctive signs of interstitial lung infection
- In interstitial pneumonitis there are no
- The primary diagnosis is correct only in 10% of cases
- The disease is most often mistaken for desquamative interstitial pneumonia
- A biopsy should always be performed to confirm the diagnosis and radiological changes.
Causes of interstitial pneumonia
A large number of regulatory processes in the body are involved in the formation of the disease. It was not possible to establish the exact reasons. The specificity of the disease is such that most often it develops against the background of existing immunological problems.
It is previously known that pathogens that cause conflict in the immune system can be:
- viruses (herpes, influenza, ARVI);
- infections (mycoplasma, ureaplasma, chlamydia);
- some types of dust;
- fungi (aspergillus, candida);
- parasites.
Factors predisposing to the development of pathology and relapses:
- Chronic inflammatory reactions. May contain many bacteria that cause pneumonia. It is transported through the processes of homeostasis through the blood and lymph flow.
- Penetration, inhalation of chemical, toxic substances. They have a detrimental effect on metabolic processes in the lungs and disrupt gas exchange.
- Smoking tobacco in any form. There is a version that passive smoking brings no less problems to human health. Toxic substances, carbon monoxide, which are part of the smoking mixture, irritate all receptors of the respiratory system. It inhibits the vital functions of the lungs, leading to cancer and the formation of chronic bronchiolitis.
- Use of certain medications. In particular those containing gold, antibiotics.
- Carrying out chemotherapy, cancer tumors, taking cytostatics.
- HIV infection, AIDS, other immune disorders.
- Disturbances in the functioning and metabolic process of the liver.
- Surgical procedures of various types.
Often, examination fails to determine the infectious nature of the disease. Characteristic of idiopathic pneumonia. Pulmonitis is characterized by inflammation of the alveolar walls, and the interstitial septum suffers.
An X-ray in the initial stages shows only a faint pattern on the lungs.
Causes and risk factors
Interstitial lung diseases (ILD) combine diseases with identical radiological changes in the respiratory organ in combination with bilateral damage. Pneumonia of an idiopathic nature occupies a special place in this group, however, its etiology remains unclear.
The causes of this type of pneumonia are:
- infectious agents - mycoplasmas, rickettsia, pneumocystis, herpes virus, staphylococci, respiratory viruses, streptococci, legionella;
- a phenomenon of immunodeficiency in which antibodies are produced to a specific antigen.
In addition, there are a number of factors that contribute to a decrease in immunity and increase the risk of a serious pathological process.
These include:
- the presence of foci of chronic inflammation (caries, sore throat, arthritis of the joints);
- frequent respiratory viral infections;
- HIV infection (also applies to carriers);
- long-term use of certain medications;
- smoking;
- frequent drinking of alcohol;
- heavy physical activity associated with professional activities or sports;
- hormonal disbalance;
- bearing a child and lactation period;
- improper working conditions (work in hazardous industries).
Any of these factors or their combination can give impetus and provoke the beginning of the process.
Diagnostics
Various methods are used in the diagnosis of interstitial pneumonia; making a diagnosis is a rather difficult task. First, the doctor examines the patient, studies his complaints and anamnestic data.
During auscultation, soft creaks are heard (at the initial stages of the development of the disease - mainly at the roots of the lungs, at the advanced stage - in all segments and lobes, including the apexes), harsh breathing, and wheezing of various types. The percussion sound in the affected area is shorter than normal.
To make a diagnosis, the following types of examination are prescribed:
Radiography
- radiography;
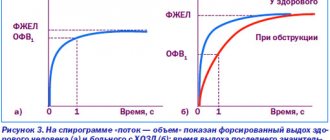
- studies of external respiration function (plethysmography, spirography);
- high resolution computed tomography.
In cases where the data from these studies are insufficient, fibrobronchoscopy and lung biopsy can be performed.
X-ray and HRCT images show one or more foci of tissue compaction, thickening of interlobular and intralobular interstitial tissues, decreased transparency of the lung parenchyma (ground glass type, mainly observed in the lower lobes of the lungs). Also on X-ray and HRCT images you can see the presence of segmental dilations of the lumen of the bronchi, called bronchiectasis.
High-resolution computed tomography is the most informative research method for this disease. With its help, you can establish the prevalence of the pathological process, determine the stage and intensity of fibrosis progression.
Pathology is differentiated from bacterial pneumonia, tuberculosis lesions, and other interstitial lung diseases.
Additional treatment measures
Doctors must prescribe, in addition to antibiotic therapy, agents to maintain intestinal microflora. To prevent this phenomenon, doctors always prescribe drugs such as Linex.
In order to replenish metabolic processes, it is necessary to consume a lot of fluid. This helps remove everything unnecessary and toxic from the body. Vitamins are required. If you have a fever, you need to take antipyretic drugs. If the fever is very pronounced, the doctor in this case recommends taking non-steroidal drugs.
For inflammation, which is accompanied by a wet cough, mucolytic drugs, alkaline inhalations with mineral waters or solutions with soda are recommended. Physiotherapeutic procedures play a huge role.
Chronic pneumonia: Diagnosis
The differential diagnosis of chronic pneumonia and lung cancer is of greatest practical importance; It is well known that cancer patients are often observed for months with an erroneous diagnosis of chronic pneumonia, resulting in missed treatment opportunities.
It should be well remembered that lung cancer is very common, and chronic pneumonia is much less common. Therefore, in any cases of prolonged or recurrent inflammatory process in the lung, especially in elderly men and smokers, one should first of all exclude a tumor that stenoses the bronchus and causes the phenomenon of so-called paracancrosis pneumonia. The same must be said regarding large focal shadows in the lung, often discovered during random X-ray examination, which most often turn out to be tumors, but can also represent areas of carnification.
In the absence of a typical clinical and radiological picture of the tumor, the correct diagnosis can be established based on the dynamics of the radiological picture, which in cancer appears negative. It should, however, be emphasized that specially undertaken dynamic monitoring of a patient with suspected cancer poses a high risk and, as a rule, is unacceptable. In most cases, it is possible to clarify the diagnosis in a timely manner using special methods - bronchoscopy with biopsy, transbronchial or transthoracic biopsy of the pathological focus, regional lymph nodes, bronchography, etc. If it is impossible to establish an accurate diagnosis using these methods, thoracotomy is indicated with clarification of the diagnosis on the operating table and subsequent interventions of the appropriate extent.
The differential diagnosis of chronic pneumonia and chronic bronchitis is established on the basis of the absence in patients with bronchitis of a direct connection between the onset of the disease and acute pneumonia, as well as local changes in the type of infiltration of lung tissue during exacerbations. Bronchitis is characterized by diffuse lesions and typical functional changes (obstructive ventilation disorders, pulmonary and pulmonary-heart failure).
Bronchiectasis, in contrast to chronic pneumonia, is characterized by a younger age of patients with impaired patency of the distal branches, as well as typical dilatations of the bronchi detected by bronchography. It should be noted, however, that according to bronchographic data, there are also transitional forms between these two states.
Chronic lung abscess differs from chronic pneumonia in the typical clinical picture of acute pulmonary suppuration at the onset of the disease, as well as the presence of a cavity against the background of pneumosclerosis, detected by X-ray (tomography, bronchography).
Certain difficulties often arise when differentiating chronic pneumonia and some forms of pulmonary tuberculosis. The latter is characterized by the absence of an acute nonspecific process at the onset of the disease, predominantly upper lobe localization of lesions, petrification in the lung tissue and hilar lymph nodes. The diagnosis of tuberculosis is confirmed by repeated examination of sputum, tuberculin skin tests, and serological methods.
Basic approaches to the treatment of interstitial pneumonia
The main task for the doctor is to slow down the process. The goal is clinical recovery of the patient. Most often, patients follow the path of drug therapy; a surgical method is also used - lung transplantation; with such an operation, life extension is possible up to five years.
Main groups of drugs
The most used group of drugs are glucocorticosteroids. They are prescribed in large doses for a long period of time up to 3 months or more. In some patients, this method of treatment gives quite good results. As mentioned earlier, there are seven forms of interstitial pneumonia, so for each specific form, the result of therapy may be different. Cytostatics and antifibrotic drugs are also used.
Physiotherapy
The most effective physiotherapeutic method is long-term oxygen therapy. It helps improve the quality of life in patients, increasing endurance in terms of minor activities (walking, self-care). But, alas, this method does not affect life expectancy.
Traditional methods
As folk methods of treatment, decoctions of herbs and berries are used: viburnum, birch buds, coltsfoot, marshmallow root. With a disease such as interstitial pneumonia, these methods will help little, so glucocorticosteroids still remain in first place.
Mode
The regimen must be followed throughout the entire treatment! In severe forms, hospitalization is required. Bed rest, lack of contact with infectious patients, rational work and rest regime. A diet rich in protein foods.
Preventive measures
To prevent the development of interstitial pneumonia, it is necessary to carry out a number of preventive measures, which include the following:
- eliminate smoking;
- vaccinate annually before seasonal epidemics of influenza and colds;
- increase immunity by taking vitamin complexes and practicing hardening procedures;
- regularly engage in physical exercise including breathing exercises in the set of exercises;
- maintain personal hygiene;
- timely treatment of chronic diseases;
- attend an annual medical examination at the clinic;
- exercise;
- Avoid public places during seasonal epidemics.
By following these simple rules of prevention, you can prevent the occurrence of such a serious disease as interstitial pneumonia.
What is SARS?
The causative agents of SARS are:
- mycoplasma;
- legionella;
- Leptospira;
- Coxiella;
- coronaviruses (cause severe acute respiratory syndrome - SARS).
cough, sputum, shortness of breath Symptoms of SARS are:
- high fever - more than 38 degrees, and for pneumonia caused by Legionella - 40 degrees;
- symptoms of general intoxication predominate, such as painful headaches, muscle pain;
- erased pulmonary symptoms - moderate, non-productive (without sputum) cough, and if sputum appears, its amount is insignificant;
- the presence of extrapulmonary symptoms characteristic of the pathogen (for example, rash);
- mild changes in the blood - no leukocytosis, which is characteristic of pneumococcal pneumonia.
- The radiograph shows an atypical picture - there are no pronounced foci of darkening;
- there is no reaction to sulfonamide drugs.
severe acute respiratory syndromeFeatures of atypical viral pneumonia or SARS are:
- Mostly adults from 25 to 65 years old are affected; isolated cases have been reported among children;
- the incubation period lasts from 2 to 10 days;
- The route of transmission of infection is airborne and fecal-oral;
- pulmonary symptoms appear on day 5, and before that symptoms of viral intoxication appear - chills, muscle pain, nausea, vomiting, and sometimes diarrhea (this course of the disease can imitate an intestinal infection);
- on the blood side, there is a decrease in the number of both lymphocytes and platelets (which often provokes hemorrhagic syndrome);
- a biochemical blood test shows an increase in liver enzymes, which reflects liver damage by the virus.
- Complications such as distress syndrome, toxic shock, and acute respiratory failure quickly develop.
Classification
Interstitial pneumonia is not a homogeneous disease, but a whole group of heterogeneous inflammations of the lungs, united by the name.
Among the types are:
Simple or common interstitial pneumonia (idiopathic interstitial pneumonia).
During the pathological process, rapid fibrous transformation of the alveoli with their scarring, destruction of the interstitium (connective tissue of the lungs), and a decrease in the rate of cellular metabolism at the local level are observed. It tends to be chronic and long-lasting, more than 6-12 months on average.
Cryptogenic pneumonia.
It almost always flows acutely or subacutely. Leads to rapid exudation (filling with fluid) in the alveolar area. This is one of the most dangerous forms of the disease.
Non-specific.
It occurs subacutely or chronically. Causes indolent scarring of interstitial tissue and parenchyma. This is a characteristic feature of nonspecific pneumonia of this kind.
Desquamative interstitial pneumonia.
It always flows sub-sharply. The duration of the disease is months, in some cases it can last for years. Requires urgent medical correction with medications. It is characterized by a dual process in the lungs: scarring and destruction of lung tissue occurs.
Acute form.
It is considered the most dangerous and lethal, since it is characterized by a dual process: both fibrosis and exudation are observed. Mortality, according to medical statistics, is more than 70% of all patients (clinical cases). Requires hospitalization and intensive care.
Lymphoid. Occurs with symptoms of extensive lymphadenitis. Lymphocytic infiltration is observed.
The main category of patients are middle-aged people. Representatives of the stronger sex are most often affected. The ratio of men to women is determined by the proportion 3:1.
Respiratory bronchiolitis
Smokers are again in the spotlight, with men getting sick more often. This form of the disease is characterized by a combination of an inflammatory process in the small bronchi (bronchioles), occurring against the background of any other lesion of the interstitial tissue. This may include idiopathic interstitial pneumonia. There is a great similarity with desquamative interstitial pneumonia, however, with this pathology the process is not as extensive.
The main complaints patients make are cough and shortness of breath, although the severity of symptoms is much less. Moist rales are heard over the lung fields.
X-rays reveal mesh or nodular darkening of various shapes, including ring-shaped, thickened bronchial walls, and hyperplasia of surrounding tissues. During a functional study, signs of two processes are observed - obstruction and restriction of the bronchi.
Treatment of this pathology requires complete cessation of smoking, which significantly improves the prognosis for life. Corticosteroids are indicated.
How are interstitial lung diseases diagnosed?
In most cases, the first suspicion of ILD arises after fluorography or chest x-ray. However, these studies are not sensitive enough to determine the specific type of ILD, which is why there are often cases when such patients are treated for pneumonia for a long time and without results. Sometimes a patient with ILD may have a completely normal chest x-ray. In this regard, the diagnosis of ILD necessarily requires a computed tomography scan of the lungs. This study allows us to describe in detail the nature of changes in lung tissue.
The second necessary component of the diagnosis of ILD is a study of pulmonary function, and in this situation we are not talking about spirometry - a study of the function of external respiration, which is performed today in almost any clinic and hospital, but about a more detailed study of lung function with measurement of lung volumes and diffusion capacity, that is, the ability of the lungs to conduct oxygen from inhaled air into the blood.
Sometimes - in the presence of classic changes on a computed tomography of the lungs - these studies are enough to make a final diagnosis, but, unfortunately, such cases are rare. In other situations, the third stage of diagnosis is necessary - surgical biopsy of lung tissue. This procedure is a surgical procedure that is performed in specialized thoracic surgery units.
The resulting biopsies (pieces) of lung tissue are examined under a microscope, and based on the nature of changes in the structure of the lung tissue, a final diagnosis is made, indicating the specific type of ILD. There is another method for obtaining a lung biopsy - with. Of course, this is a more gentle and easier procedure to perform, which does not require hospitalization and is easier to tolerate by the patient himself, however, the amount of information obtained as a result is disproportionately less than with a surgical biopsy. Often it does not allow us to judge the diagnosis, and the doctor and the patient still return to the need for a surgical biopsy.
Thus, the diagnosis of ILD should always be carried out as accurately as possible in the interests of the patient himself. Sometimes the doctor may need additional studies, for example, immunological blood tests to clarify the role of molds or poultry allergens in the development of the disease, to diagnose systemic connective tissue diseases (rheumatoid arthritis, systemic scleroderma, etc.) as a background for the occurrence of ILD, for analysis of blood gas composition in severe cases of the disease, etc.
Computed tomography of the lungs and a complete study of pulmonary function are used not only for the initial diagnosis of interstitial lung diseases, but also subsequently to monitor the course of the disease and evaluate the effectiveness of treatment.
In our medical center you can:
- undergo all necessary examinations within a few days;
- undergo a biopsy of lung tissue;
- obtain a histological report from leading morphologists in the field of lung pathology;
- develop a treatment plan;
- take advantage of annual monitoring programs for patients with interstitial lung diseases.
Treatment methods
There are several procedures available to treat interstitial pneumonia. General therapy includes the use of drug and non-drug methods. Medications include:
- Taking Prednisolone and other glucocorticosteroids. There are several regimens for taking these drugs, which are selected by the doctor depending on the patient’s health condition.
In addition to corticosteroids, drugs belonging to the group of cytostatics that help restore the immune system, such as Cyclosporine and Methotrexate, are used. Most often they are used in cases where therapy with drugs of the first group does not bring results.- Combination treatment involves taking the above medications simultaneously. This approach is considered especially effective in advanced forms of the disease.
- Mucolytics. Many experts advise taking medications from this group as an addition to basic treatment.
The duration of drug therapy is about six months. After this, its effectiveness is assessed. This is evidenced by a decrease in the clinical manifestations of the disease, the disappearance of signs of the disease on x-rays, etc.
If the results of treatment are positive, then to consolidate the results obtained, the patient must adhere to the same treatment regimen for a year. If there is no effect, Interferon and Colchicine are used as additional drugs.
Non-drug treatment methods include:
- complete cessation of smoking, which can significantly improve the prognosis;
physical therapy, namely breathing exercises that improve lung ventilation and prevent the likelihood of respiratory failure;- oxygen therapy and artificial ventilation (ALV). The latter technique is used most often in the last stages of the development of the disease, when the patient has obvious respiratory failure.
The oxygen treatment method is not able to completely stop pathological processes, but is used as an additional therapy, since it allows the following effects to be achieved:
- Facilitating the breathing process.
- Significant reduction in blood pressure.
- Preventing or reducing complications that arise due to low oxygen levels in the blood.
- General improvement in the patient's well-being.
- Return of healthy sleep.
Respiratory rehabilitation is very important for the treatment of interstitial pneumonia, since this technique allows patients to return to a normal lifestyle.
Lung rehabilitation programs include the following:
physical exercises aimed at generally increasing the patient’s endurance;- breathing techniques to improve lung function;
- nutrition adjustments;
- emotional support for the patient.
The most radical method of treating the disease is a lung transplant. It is practiced mainly among young people who have not used other treatment methods in a timely manner. Transplantation is performed in acute forms of the disease.
Prevention of pneumonia
Prevention measures include a healthy lifestyle. To have strong lungs, you need to stop smoking, avoid contact with harmful gases and walk more in the fresh air away from the bustle of the city.
Hiking in mountainous areas and where coniferous forests grow is good for the lungs. Some people benefit from the maritime climate.
It is useful for older people to visit health resorts. It is better for them to live in a village or in a dacha somewhere outside the city. The older a person is, the more sensitive his lungs are to the environment. City dust and exhaust fumes have a negative effect on older people.
Also at this age, people in many cases switch to strong medications. This negatively affects the respiratory and cardiac organs. There is a risk of side effects and complications.
Children need to undergo hardening activities to help strengthen their immune system. There are many different ways and recommendations for this. These can be obtained from your doctor.