Description of the disease
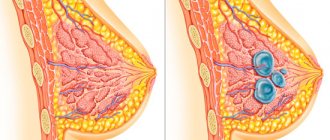
Hygroma is a benign formation that has a dense capsule and is filled with serous fluid inside. Visually, hygroma looks like a lump that is localized in a certain area. In an uncomplicated course, the disease is not dangerous, since it has no tendency to malignant degeneration and metastasis.
It is dangerous if it compresses nearby structures and leads to disruption of their function. In this case, you should definitely consult a doctor to remove the tumor, since prolonged compression of the nerve structures can lead to irreversible consequences.
In addition, the difficulty of treatment lies in the fact that it is not always possible to completely remove the formation and get rid of the disease. Relapse occurs quite often.
Symptoms of hygroma at different locations
It is not difficult to detect a cyst; it is clearly visible and looks like a tubercle, the same color as the skin.
For many, hygroma of the hand is sensitive to touch, aches in bad weather and is painful when injured. A hygroma on the hand can cause swelling of the soft tissues, even if it does not hurt. When the hygroma of the wrist joint of the hand becomes more than 3 cm, it puts pressure on the surrounding blood vessels and nerve endings, which causes numbness or increased sensitivity in certain areas.
Return to contents
On the wrist
In almost 70% of cases, hygroma is located on the right or left hand in the wrist area, but hygroma of the right hand is more common. There are three major nerves located on the dorsum of the wrist: the radial nerve, the posterior interosseous nerve, and the posterior branch of the ulnar nerve. Based on the numbness of the fingers and the location of the bulge, it is determined which nerve was compressed. It is very rare, but when the lump grows to a huge size, all three nerves are compressed, and then neurosurgery helps restore the sensitivity of the organs.
A hygroma near the elbow joint most often grows due to a bruise or an inflammatory process.
Return to contents
Education on the elbow
Most likely, elbow hygroma appears due to a bruise, or after an inflammatory disease (bursitis, tenosynovitis). The reason is regular impact on the elbow joint. Constantly resting your elbow on the same place increases the risk of developing hygroma on the elbow. With a large formation, the median nerve and the terminal segment of the brachial artery are compressed.
Return to contents
Hygroma on the shoulder
The appearance of a lump on the shoulder is accompanied by constant tension in the shoulder joint. This most likely occurs when there is constant impact on the shoulder, such as frequent lifting or moving heavy objects. Sometimes it is accompanied by swelling in the shoulder, forearm, neck area and can be very painful. It is extremely rare.
Return to contents
On fingers
The bump grows anywhere along the entire length of the finger, wherever there is connective tissue, not necessarily near the joint. The tumor is dense and resembles a pea. There can be several of them on one finger at once. They are most often localized on the middle and far interphalangeal joint, less often they grow on the metacarpophalangeal joint.
Hygroma on the hands of children can appear and disappear, and the cause of its appearance can be the same type of physical activity.
Return to contents
Anatomy and mechanism of formation
The formation can appear next to connective tissue of different locations, so hygromas of joints and tendons are distinguished. Anatomically, a hygroma is a cavity that is lined with a connective tissue membrane and filled with heterogeneous fluid.
The main mechanism for the occurrence of hygroma is traumatic damage to an area of connective tissue. Subsequently, improper regeneration occurs, as a result of which the cells degenerate into two types (one forms a capsule, while others line the cavity).
Causes
There is no single cause of hygroma. However, certain risk factors can be identified that contribute to its development:
- Traumatic factor. Post-traumatic formation is the most common. The injury can be either one-time or repeated. For example, hygroma in the clavicle area can develop after stretching the acromial clavicular joint.
- Excessive stress on a joint or tendon. Another reason why hygroma appears is irregular sports activities in the absence of preliminary preparation or warm-up. Hard work can lead to injury to muscle tendons and further degeneration of connective tissue cells. This is especially true for long-term exposure when, despite a past injury, a person continues to load the joint or tendon.
- Hereditary predisposition. The risk of developing hygroma increases if the disease occurs in blood relatives. However, genetic predisposition is realized only under the influence of pathological factors.
Complications and consequences
Hygroma is generally not dangerous, as it is a benign neoplasm. Such tumors never become malignant. Moreover, small hygromas that do not increase in size and do not cause discomfort may not even be treated. A daily massage is enough for the hygroma to decrease in size or disappear completely. True, you should consult a doctor about this, since it is not always possible to independently assess the severity of the pathology.
Complications arise when the tumor ruptures and the wound becomes infected. The infection penetrates the joint, causing it to become inflamed. A severe complication of hygroma is a knee abscess, the treatment of which requires urgent surgery.
Symptoms
Clinical manifestations of this disease depend primarily on the location and size of the tumor. If the size of the formation is small, the disease may manifest itself only in the form of a bulge, hard or soft to the touch. On palpation, the affected area is painless, the skin over the formation is not changed. Other clinical signs may not be of concern.
With a larger size or significant growth of the formation, it can compress the surrounding tissues. In some cases, this leads to the appearance of specific symptoms. If pain or other symptoms suddenly appear, you should consult a doctor.
Most often, symptoms appear when the tumor compresses the nerve endings. In this case, a pressing or bursting pain appears, which intensifies with exercise and goes away with rest. During a physical examination, the doctor may detect tenderness to palpation, sometimes a positive symptom of fluctuation.
Treatment of hygroma
Treatment of hygroma in the initial period of development does not involve radical intervention. A good therapeutic effect is achieved by procedures from:
- paraffin applications and heating;
- ultraviolet sessions and electrophoresis procedures with iodine.
The practice is to puncture the cystic sac and extract the contents from its cavity, followed by the introduction of hormonal, anti-inflammatory drugs, or antibiotics (for inflammatory processes) into the cavity with mandatory fixation of the joint.
Or the cavity is opened and its contents are removed. But since the cystic sac remains unchanged, such treatment methods do not guarantee a cure. Neoplasms can reappear at any time.
A radical method of solving the problem is surgical intervention. The indicator is:
- unaesthetic appearance;
- continuous pain;
- intensive tumor growth;
Bursectomy is one of the methods for removing articular tumors, based on the removal of the cystic bursa. This operation is performed using laser burning or a radio wave scalpel, which significantly reduces the operation time, prevents bleeding and the formation of rough keloid scars.
If, after reading this article, you think that you have symptoms characteristic of this disease, then you should
In modern medicine, it is accepted to treat hygroma only surgically. Radical measures help prevent relapses and avoid inflammatory processes in the joints. Previously, it was also believed that hygroma could be cured with some folk remedies and physiotherapy techniques.
Drug treatment
This type of treatment is appropriate for inflammatory processes in the tissues near the hygroma, but only if the inflammation is not purulent (without throbbing pain, temperature above 38 C, a sharp deterioration in joint mobility, severe changes in the skin over the tumor).
For purulent inflammation, the mandatory treatment method is surgery, and only after that the doctor prescribes certain medications to completely destroy the infection.
If the inflammation is not purulent (body temperature is up to 37.5 C, there are no skin changes, movements are not constrained, the pain is not severe, but constant, covering the hygroma itself and a small area of tissue near it), then drug treatment of the hygroma is acceptable (it will relieve inflammation, but the tumor itself will not disappear!).
All calculations of drug dosage should be carried out by a doctor, taking into account concomitant diseases and the patient’s age (for children, calculations are carried out based on body weight).
- Tablets: 1 tablet of Clemastine in the morning and evening (course – 7-10 days).
- Powders: 1 sachet of Nimesil in the morning and evening (course duration is a week-10 days).
- Ointments: applied in a thin layer 2-3 times a day for no more than 7 days (Diclofenac, Gistan, Diprosalik).
Physiotherapy for hygroma will also help relieve inflammation and protect the joint from complications (UHF, ultrasound, magnetic therapy, salt and soda baths).
Surgical methods of treatment
Excision of the tumor is the most effective method, since relapses after surgery occur in 20 cases out of 100. Since hygroma is a benign tumor, it is not necessary to remove it. The only exceptions are those cases when there is compression of blood vessels or nerves, joint mobility is severely limited, and there is concomitant purulent inflammation.
In most cases, the operation is performed under local anesthesia and takes about half an hour. Exceptions include multiple hygromas and purulent inflammations. They use general anesthesia. The surgical opening is small, and with minimally invasive access methods, almost invisible.
After the operation, the wound is treated with antiseptic solutions, drained, covered with a tight bandage and the limb is immobilized (plaster splints). If the wound heals well, the stitches do not come apart, and inflammation does not occur, then by the end of the week the stitches can be removed.
After the surgical suture has healed, it is recommended to perform a set of therapeutic exercises.
Folk remedies (treatment at home)
Treatment of the pathology is determined by the doctor after diagnosis.
Previously, there was a crushing method, as a result of which, under the influence of force, the contents of the tumor were pressed or burst, which caused pain, led to an inflammatory process, and as a result the cyst appeared again.
Today it is not used, since there are many other safer methods.
Conservative treatment
This therapy is used only at the initial stage of educational development and includes a number of the following activities:
- X-ray therapy - it is used mainly to destroy malignant tumors. Therapy of this kind can be dangerous, so it is recommended to carry it out in fairly accessible places; hygroma is included in the list of these places;
- Physiotherapy – electrophoresis with iodine, ultraviolet irradiation;
- Puncture - suctioning out the contents of the hygroma with a syringe, followed by the administration of medications that promote healing. This method is used for large hygroma sizes;
- Glucocorticoid blockade - this treatment method is performed under local anesthesia. The formation is pierced with a syringe, the contents are sucked out in the same way as during puncture, but in this case glucocorticoid drugs are administered;
- Paraffin and mud applications;
- Immobilization with a plaster retainer or orthopedic bandage - to reduce fluid production. It is applied for 7 days, but no more.
Conservative treatment can be effective if the affected joint is kept at rest. If treatment of hygroma without surgery does not help, it is necessary to resort to surgical intervention.
Surgical method
Today this method is considered the most effective.
Indications for the operation are:
- not aesthetic;
- fast growth;
- discomfort;
- pain when moving.
There are several ways to remove the formation:
- Bursectomy – removal of the synovial bursa.
- Laser therapy – laser removal of hygroma involves heating the hygroma, resulting in its complete destruction.
- Surgical excision - removal of the hygroma and all tissue affected by it.
If, after reading the article, you suspect that you have symptoms characteristic of this disease, then you should seek advice from an orthopedist.
Hygroma is a small cyst that forms in the tissues of the body. It is considered an occupational disease.
The reasons for the formation of hygroma are not fully understood. However, experts make assumptions about the hereditary nature and connection with repeated traumatization.
Conservative therapy in this case is characterized by low effectiveness; surgical intervention is required.
Therapy for cystic formation using the recipes of our grandmothers is quite popular, and in some cases even effective.
- Mix bee honey, rye flour and the fleshy part of aloe in equal proportions until a paste-like consistency is obtained. This cake should be applied to the affected area overnight, covered with cling film.
- Dissolve 2-3 tablespoons of salt in one glass of water. Add red clay to the resulting mixture in such a volume that a creamy mass is obtained. The tumor should be lubricated with a thick layer of mass and wrapped with a bandage each time. This compress must be worn throughout the day, periodically moisturizing with water.
- Squeeze out the juice from 200 g of crushed celandine, blot gauze with it and apply to the affected area. Afterwards, cover it with cling film and leave overnight. It is recommended to repeat this procedure every three days.
In the initial stages, conservative treatment can be reduced to the use of mud, ozokerite applications, and paraffin therapy, heating, physiotherapeutic procedures (for example, ultraviolet irradiation or electrophoresis).
Among external agents, anti-inflammatory and absorbable ointments are used: balsamic liniment according to Vishnevsky, Diprospan, Dimexide, Flexen gel, Heparin ointment.
Quite often, hygroma puncture is practiced with suction of the contents, administration of glucocorticoids or sclerosants, followed by tight bandaging. Such treatment will be effective only if the patient can for a long time refuse activities that cause trauma to the synovial bursa.
If the formation suppurates, a puncture is performed, the pus is sucked out and antibiotic drugs are administered. If necessary, the hygroma is opened, the synovial bursa is scraped out with a sharp spoon, and the wound is drained to ensure the outflow of wound fluid. However, such treatment without surgery is fraught with relapses.
Until recently, crushing the hygroma was a popular method of treatment, but now this method is practically not used due to its high pain, trauma and almost guaranteed relapse of the disease.
If conservative treatment does not produce results or the hygroma constantly recurs, causes distinct pain when moving, has an unaesthetic appearance or grows too quickly, an operation - bursectomy - is indicated.
In this case, the synovial bursa is completely excised. To minimize the risk of relapse, a cast is applied after surgery for 2-3 weeks to limit joint mobility while the scar forms.
Surgical intervention is recommended especially if the cyst is growing rapidly, since excision of a large formation is associated with certain difficulties: the tumor, as a rule, is located in close proximity to ligaments, nerve nodes, and vessels, presses and displaces them, which greatly complicates the operation.
During bursectomy, it is very important to carefully remove all areas of changed tissue, otherwise the hygroma will recur again.
In connection with the development of endoscopic surgical techniques in recent years, this minimally invasive method of removing hygromas has become increasingly practiced, due to which the rehabilitation period after surgery is significantly reduced. In addition to classic removal with a scalpel, laser surgery can also be used.
Along with conservative and surgical methods, folk methods are also used, but their effectiveness is significantly lower than classical treatment. It is not possible to completely get rid of hygroma using folk remedies, but you can try to reduce its size and pain, especially in the initial stages of the disease.
- Alcohol compress: make a gauze tampon, soak it in alcohol, apply it to the tumor and wrap the compress tightly for 2 hours. If you have sensitive skin, it is advisable to lubricate it with hand cream after the procedure. Repeat compresses 1-2 times a day until the hygroma disappears or is sufficiently reduced in size.
- Compress from celandine: squeeze out the juice from 200 grams of crushed stems and leaves of the plant, soak gauze with it and apply to the hygroma. The lotion is wrapped in plastic wrap and left overnight. Repeat the procedure once every 3 days.
- White cabbage compress: a leaf of the plant is smeared with honey, applied to the tumor, and wrapped in a warm cloth for 2-3 hours. Repeat the procedure 1-2 times a day.
- Salt compress: 3-4 tablespoons of salt, preferably sea salt, are dissolved in 500 milliliters of hot water. After cooling, moisten the skin in the tumor area with the solution, cover the affected area with a warm cloth, preferably wool, then with plastic wrap and leave overnight. The duration of treatment is 10 days, then after a few days of break the course can be repeated.
Kinds
The following types of localization of hygroma are distinguished:
- Foot. On the foot, hygroma is most often localized in the ankle area and has an asymptomatic course.
- Palmar surface of fingers. There are many nerves on the palmar side of the fingers, so when hygroma is localized in this area, pain often develops.
- The back surface of the fingers. Formation on the dorsal surface is usually characterized by an asymptomatic course.
- Metatarsophalangeal joint of the hand. The area most often affected is the thumb. The disease is characterized by the presence of protrusion.
- Hygroma of the tendon in the forearm area.
Less commonly, formations are localized on the side of the neck, in the area of the elbow joint, or on the edge of the palm. Depending on the structure of the capsule, soft and dense hygromas are distinguished.
What is it and how does it work
The Almag 01 or Almag 02 device for joints is extremely simple in design and can be used in the treatment of various diseases both in a medical facility and at home. The device is compact and lightweight, making it easy to transport as needed. The device is powered from a 220 Volt network.
The classic device for the treatment of joint pathologies “Almag1” includes the following elements:
- an electronic unit that supplies electrical impulses;
- four inductors, through which the effect is exerted on the affected joints.
When connected to the network, a green light comes on on the inductor. After this, the coils can be applied to the knee joint or any other unhealthy part of the body. The duration of the exposure session is 20 minutes. After this, the device turns off automatically. If necessary, the duration of one procedure can be adjusted manually.
Under the influence of electromagnetic waves, natural metabolic and neurovegetative processes in the patient’s body are stimulated, which reduces swelling and joint pain, improves blood circulation, and increases immunity. The Almag device emits traveling electromagnetic pulses that penetrate tissue to a depth of 8–15 cm. The positive effect is carried out at the cellular level. Pulse waves restore normal electrical balance in cells, thanks to this all metabolic processes are activated, and the body begins to restore itself.
Thanks to the pulsed effect of electromagnetic waves at the cellular level, after the first session the patient feels noticeable relief
For this reason, the Almag device has virtually no contraindications and can be used at any stage of arthritis of the knee joint, for acute inflammation and even for open wounds of the knee and other parts of the body. Here's what happens in the body during a magnetic therapy session:
- The vessels feeding the joints dilate - the tissues receive more oxygen, more nutrients, metabolic processes in the cartilage and ligaments return to normal.
- In parallel with intensive nutrition and oxygenation, cartilage tissue begins to be actively cleansed of metabolic products, and deposits of harmful substances are removed from the joints.
- The production of synovial fluid is stimulated - a substance necessary for lubrication of joint structures, their mobility and full shock absorption.
- The tone of the surrounding muscles and ligaments is normalized, resulting in reduced swelling and pain.
- If the patient takes chondroprotectors and anti-inflammatory non-steroidal drugs, their absorption becomes more complete.
- The production of cytokine substances that provoke the inflammatory process is suppressed.
- Due to the active work of cells, excess fluid is removed from tissues, swelling and hematomas are reduced, and wounds heal faster.
With each session, the cells are nourished, which means their activity improves, the cartilage becomes denser and more elastic, and the joints become more mobile. Positive changes are noted by almost all patients and their attending physicians.
One compact device is suitable for the treatment of almost all joint pathologies, regardless of the location of the lesions
Diagnostics
Preliminary diagnosis is carried out according to the clinical picture (tumor formation, symptoms of compression of nerve endings) and medical history (indicating a single or multiple injury). In most cases, this data is sufficient to make a diagnosis.
For differential diagnosis, in order to establish the difference from other pathologies of the musculoskeletal system, instrumental research methods are carried out:
- Ultrasound examination (ultrasound). It is the most accessible and non-invasive diagnostic method. Allows you to identify the localization of formation, its type, homogeneity of structure. The disadvantage is the low information content and the dependence of the research results on the knowledge of the specialist.
- Radiography. Used for differential diagnosis of injuries and fractures. In addition, an x-ray method is prescribed if bone formation is suspected.
- Magnetic resonance imaging (MRI). The most specific method for tumor imaging. Allows you to identify the boundaries of formation, localization, and degree of blood supply. The disadvantage is the high cost.
Since the disease is benign, histology is usually not necessary. However, if it is not possible to identify the nature of the tumor by other signs, and it is not possible to exclude malignancy, a biopsy is performed.