It is a large paired blood vessel that participates in the pulmonary circulation and enters the pulmonary circulation. This artery carries deoxygenated blood from the heart to the lungs. The largest part of the pulmonary artery is the main pulmonary artery, i.e. its part located near the heart is the pulmonary trunk, and its smallest parts are those located at the pulmonary alveoli. The pulmonary artery is divided into left and right. The pulmonary artery is a large paired blood vessel that participates in the pulmonary circulation and is included in the pulmonary circulation. This artery carries deoxygenated blood from the heart to the lungs. The largest part of the pulmonary artery is the main pulmonary artery, i.e. its part located near the heart is the pulmonary trunk, and its smallest parts are those located at the pulmonary alveoli. The pulmonary artery is divided into left and right.
Structure of the pulmonary artery
Following the order of blood flow, the pulmonary arteries originate in the pulmonary trunk, which is the main pulmonary artery. This part of the artery begins at the base of the right ventricle. The length at this point is about 5 cm, and the diameter is about 3 cm.
The left main pulmonary artery is shorter and smaller than the right, it passes horizontally in front of the descending aorta and left bronchus into the root of the left lung. Above, the left main pulmonary artery is connected to the aorta by the argios ligamentum. The left pulmonary artery usually divides into superior and inferior branches, similar to the right pulmonary artery. The left pulmonary artery is divided into branches supplying the upper lobe, the lower lobe of the lung, and also has basal and lingular branches. Includes the following branches: apical, anterior descending, posterior, anterior ascending, superior and inferior lingular, superior branch of the inferior lobe, medial basal, anterior basal, lateral basal, posterior basal.
The right pulmonary artery departs at an angle from the pulmonary trunk, located on one side between the superior vena cava and the ascending aorta, and on the other side in front of the main right bronchus. Before entering the hilum of the lung, the right pulmonary artery divides into inferior and superior branches. Next, the upper branch is divided into two or three branches, which go to the first, second and third segments of the upper lobe of the lung. The branches of the right pulmonary artery go to the upper lobe of the lung, the middle lobe of the lung and the lower lobe of the lung. Accordingly, it has the following branches: apical, posterior descending, anterior descending, posterior ascending, lateral, medial, superior, medial basal, anterior basal, lateral basal, posterior basal.
The left and right pulmonary arteries enter both lungs.
Pathologies and diseases
Pulmonary arteries are vital organs. Diseases of these vessels can lead to death.
Pulmonary embolism
Thromboembolism of the pulmonary artery is a blockage of the pulmonary artery or blockage of its branches by blood clots, most often formed in the large veins of the lower extremities or pelvis. Clots that block such arteries are called emboli. The causes of the disease are the formation of blood clots, and blood clots, in turn, are provoked by several factors, among which the following can be noted:
- Stagnation of blood in the veins. The slower blood flows through the veins, the greater the likelihood of blood clots.
- Inflammation of the venous walls. Inflammation causes blood clots to form.
- Increased blood clotting.
Women are more susceptible to thromboembolism than men.
Pulmonary stenosis
Pulmonary stenosis is a narrowing of the outlet of the right ventricle at the pulmonary valve. The problem in this case is the difference in pressure in the right ventricle and in the pulmonary artery. Pulmonary artery stenosis causes the development of an atrial septal defect and increased pressure in the right atrium, followed by right ventricular hypertrophy and right ventricular failure. The problem is corrected surgically.
Pulmonary valve insufficiency
Pulmonary valve insufficiency is caused by its damage. Symptoms of the disease include shortness of breath, weakness, drowsiness, palpitations, cyanosis, heart pain, arrhythmia, persistent tachycardia, ascites, cardiac cirrhosis, hydrothorax.
This disease can provoke pulmonary embolism and pulmonary aneurysm.
Pulmonary hypertension
This disease includes a whole group of pathologies that are characterized by an increase in pulmonary vascular resistance, causing right ventricular failure. This disease is quite severe, reduces physical endurance, and provokes heart failure.
The relevance of pulmonary embolism cannot be overestimated, because this disease ranks third in the structure of population mortality after coronary heart disease and stroke.
How are they classified?
There are several types of classifications, for example, according to Sommerville, where pulmonary atresia is distinguished into 4 types:
- I – Valve atresia. There are formed and passable trunk and both pulmonary arteries.
- II – Atresia of the valve and trunk of the artery. Both pulmonary arteries operate and can have a common or separate origin.
- III – Atresia of the valve, trunk and one of the pulmonary arteries. The second pulmonary artery is normal and carries blood.
- IV – Atresia of the aortic valve, trunk, both pulmonary arteries. Blood flow in the lungs is carried out through auxiliary vessels.
A more modern version of the classification is also used:
- Type A – there are true pulmonary arteries, no accessory arteries, pulmonary blood flow is through the PDA.
- Type B – the presence of true pulmonary and accessory arteries.
- Type B – true pulmonary arteries are absent, pulmonary blood flow is carried out through collaterals.
Sometimes during diagnostics mixed forms are revealed.
Pathogenesis and etiology of pulmonary embolism
Currently, there is an increase in the incidence of pulmonary embolism due to a number of reasons:
- insufficient provision of hospitals at the district level with the necessary equipment for timely diagnosis;
- high prevalence of cardiac and bronchopulmonary pathology among the population, which often masks the signs of pulmonary embolism.
Numerous clinical studies have established that PE is never diagnosed in 60% of patients during their lifetime.
The main function of the lungs is gas exchange: all the venous blood of the human body is delivered through the vena cava system to the right half of the heart, and then to the lungs for enrichment with oxygen.
The superior vena cava drains blood from the upper half of the body (head, neck and upper extremities), while the inferior vena cava collects blood from the lower half of the body. Next, the vena cava carries venous blood to the right parts of the heart: the atrium and ventricle.
Through the pulmonary trunk, which immediately divides into the pulmonary arteries (right and left), blood from the right ventricle flows into the lungs. From the lungs, arterial blood flows through the pulmonary veins into the left atrium, ventricle, and then spreads through the aorta throughout the human body.
The pulmonary circulation is formed by the pulmonary arteries and veins, and the aorta, superior and inferior vena cava form the major circle.
A number of diseases are accompanied by thrombus formation in various veins. Growing blood clots can break off and travel through the vena cava system into the pulmonary artery, leading to thrombosis (see diagram).
The result of thrombosis and cessation/obstruction of blood flow is an increase in resistance in the pulmonary vessels, which spreads to the right ventricle and then the atrium, which leads to an increase in pressure in the right sections (right ventricular failure).
The leader in supplying blood clots to the lungs is the inferior vena cava system, and the most common etiology of pulmonary embolism is considered to be deep vein thrombosis, in particular the femoral and pelvic veins.
Risk factors for pulmonary embolism
Pregnancy and the postoperative period represent a serious cause for concern in terms of pulmonary thrombosis: during pregnancy the risk of thrombosis increases 5 times, after surgery - 4 times.
Pulmonary embolism clinic
The manifestations of pulmonary embolus are largely determined by the caliber of the embolus, the underlying disease that caused the thrombosis, and the massiveness of the arterial lesions. A blood clot in the lungs can be asymptomatic or lead to sudden death.
Clinicians define the following syndromes:
- Cardiac: collapse, chest pain, increased heart rate, shock, pallor of the skin with a combination of blue discoloration of the nasolabial triangle, ears, limbs, drop in pressure;
- Pulmonary-pleural: shortness of breath, hemoptysis, dry cough, chest pain due to the effusion of serous exudate into the pleural cavity.
- Abdominal: feeling of heaviness and pain in the area of the right hypochondrium.
- Brain: severe weakness, headache, fainting;
- Nephrotic: a sharp decrease or complete absence of urine.
Most often, the signs of pulmonary embolism are as follows:
More rare symptoms include:
- cough;
- fainting and headache;
- hemoptysis;
- cyanosis;
- fever.
In many ways, the clinical picture is determined by the massiveness of the damage to the vascular bed:
For the treatment of VARICOSE and cleaning blood vessels from THROMBUS, Elena Malysheva recommends a new method based on Cream of Varicose Veins. It contains 8 useful medicinal plants that are extremely effective in the treatment of VARICOSE. Only natural ingredients are used, no chemicals or hormones!
If PE develops in a relatively healthy person, for example, during surgery (caesarean section, appendectomy, etc.), fracture or injury to large bones, then a phenomenon of discrepancy between the clinical picture and the severity of the disease occurs. This is explained by the fact that the reserve capacity of the vessels, lungs and heart is great and is capable of not responding with a bright clinic to a large embolus in the lungs.
Clinical classification of pulmonary embolism
Recurrent chronic pulmonary embolism, as well as acute non-massive lung damage, present the greatest diagnostic difficulties due to nonspecific and mild symptoms.
In the presence of cardiovascular and bronchopulmonary pathology in a patient, the main difference between PE and exacerbations of the disease is a sharp increase in or unmotivated shortness of breath. And also, thrombosis of the small arteries of the lungs is a very common cause of exacerbations of COPD.
Images
- Bronchial anatomy.jpg
Alveoli with vessels
- Alveolus diagram.svg
Alveolus
- Illu bronchi lungs.jpg
Trachea, bronchi, lungs
- Illu light circuit.jpg
Small circle
- Lungs anatomy.png
Lungs
- Gray490.png
Heart and lungs, front view.
- Gray503.png
Cross section of the chest.
Diagnosis of the disease
The range of diagnostic measures aimed at confirming pulmonary embolism and searching for the source of the embolus is as follows:
MSCT and CT with pulmonary angiography in the diagnosis of pulmonary embolism are methods No. 1.
Differential diagnosis:
- acute myocardial infarction;
- attack of bronchial asthma;
- attack of cardiac asthma;
- accumulation of blood or serous effusion in the heart sac (hemo- and hydropericardium);
- acute pneumonia;
- chronic pulmonary embolism.
Diagnostics
If atresia of the cardiac pulmonary valve is suspected, the following types of diagnostics are performed:
- Outpatient. It includes questioning, examination, and auscultation. The doctor examines the patient, detects cyanosis, severe weakness, shortness of breath, a characteristic cylindrical shape of the chest; upon auscultation, rough systolic murmurs are heard, the first tone is strong, the second tone is weak.
- In the hospital. The patient needs to undergo echocardiography, electrocardiography, chest radiography, phonocardiography, as well as angiocardiography and, if necessary, catheterization of the cardiac cavities.
Also read: What is the Eisenmenger complex
In addition, you will need to undergo other examinations as directed by the doctor and undergo a number of tests.
Treatment and prevention
Therapy for pulmonary embolism is aimed at preventing severe pulmonary hypertension and improving circulation in the lungs. The main treatment direction is antithrombotic. Consider the following therapeutic measures:
During treatment, strict bed rest is observed.
Primary prevention is as follows:
- during long flights, it is important to ensure that the lower extremities are not pinched and take a prophylactic dosage of indirect anticoagulants before the flight;
- take contraceptives under the control of a hemostasiogram;
- after surgery, practice getting up as quickly as possible;
- fight obesity and physical inactivity.
Secondary prevention is carried out by installing venous filters and using elastic bandages (tight bandaging). Filters are relevant in the presence of thrombosis in the deep veins and previous pulmonary embolism, before major surgical interventions.
The consequences of pulmonary embolism are disabling and serious diseases: chronic pulmonary heart disease, chronic pulmonary hypertension, pulmonary infarction, embolism of large vessels. Therefore, it is extremely important to take into account the risk factors of pulmonary thrombosis in predisposed individuals, regular diagnosis of the main parameters of venous insufficiency (coagulogram, condition of the veins by ultrasound).
DO YOU STILL THINK THAT IT IS IMPOSSIBLE TO GET RID OF VARICOSE VARICOSIS!?
Have you ever tried to get rid of VARICOSE? Judging by the fact that you are reading this article, victory was not on your side. And of course you know firsthand what it is:
- feeling of heaviness in the legs, tingling...
- swelling of the legs, worsening in the evening, swollen veins...
- lumps on the veins of the arms and legs...
Now answer the question: are you satisfied with this? Can ALL THESE SYMPTOMS be tolerated? How much effort, money and time have you already wasted on ineffective treatment? After all, sooner or later the SITUATION WILL GET WORSE and the only way out will be surgical intervention!
That's right - it's time to start ending this problem! Do you agree? That is why we decided to publish an exclusive interview with the head of the Institute of Phlebology of the Ministry of Health of the Russian Federation - V. M. Semenov, in which he revealed the secret of a cheap method of treating varicose veins and complete restoration of blood vessels. Read the interview...
According to another classification, pathology is divided into the following forms:
Treatment
Treatment of patients with pulmonary embolism should be carried out in intensive care units.
Correction of hemodynamics and hypoxia
In case of cardiac arrest, cardiopulmonary resuscitation is performed. If hypoxia occurs in a patient with pulmonary embolism, oxygen therapy is administered (masks, nasal catheters); Artificial ventilation is less often required. To eliminate hypotension, saline solutions or vasopressors (adrenaline, dobutamine, dopamine) are administered intravenously [7].
Anticoagulant therapy
Timely anticoagulant therapy reduces the risk of death and recurrent thromboembolism, so it is recommended to start it not only with a confirmed diagnosis, but also during the diagnosis process if there is a high probability of pulmonary embolism. For this purpose, unfractionated heparin (intravenously), low molecular weight heparin is used: enoxaparin, dalteparin (subcutaneous) or fondaparinux (subcutaneous).
The dosage of unfractionated heparin is adjusted based on the patient's weight and activated partial thromboplastin time (aPTT)[19]. To do this, prepare a solution of sodium heparin - 20,000/kg per 500 ml of saline solution. First, 80 IU/kg is administered intravenously, and then an infusion is carried out at a rate of 18 IU/kg/h. 6 hours after the bolus injection, the APTT is checked and the rate of heparin administration is adjusted as indicated in the table. APTT is determined 3 hours after each speed change; when the desired level is reached (46-70 s, 1.5-2.5 times higher than control), this indicator is monitored daily.
| APTT, s | Changing dosage |
| <35 | Increase by 4 IU/kg/h |
| 35—45 | Increase by 2 IU/kg/h |
| 46—70 | Do not change |
| 71—90 | Decrease by 2 IU/kg/h |
| >90 | Stop administration for 1 hour, then reduce by 3 IU/kg/hour |
In most cases, low molecular weight heparins are used, as they are more effective, safer and more convenient to use than unfractionated heparins[20]. However, they should be prescribed with caution in cases of renal dysfunction (decreased creatinine clearance <30 ml/min) and with a high risk of hemorrhagic complications (the duration of action of unfractionated heparin is shorter and therefore can be discontinued more quickly in the event of bleeding). Of the low molecular weight heparins, the following are recommended: enoxaparin (1 mg/kg every 12 hours or 1.5 mg/kg once a day), tinzaparin (English) Russian. (175 IU/kg once a day). Dalteparin can be used in patients with cancer. (200 IU/kg once a day) [7].
For anticoagulation, fondaparinux, a selective factor Xa inhibitor, can be used. It is prescribed subcutaneously once a day at 5 mg for body weight <50 kg, 7.5 mg for 50-100 kg and 10 mg for >100 kg. It is highly effective for pulmonary embolism and does not cause thrombocytopenia, unlike heparin. However, fondaparinux is contraindicated in severe renal failure (creatinine clearance <20 ml/min)[7].
It is also advisable to prescribe warfarin on the first day of introducing direct-acting anticoagulants (heparins or fondaparinux). When an international normalized ratio (INR) level of 2-3 is reached and maintained at this level for at least 2 days, direct anticoagulants are discontinued (but not earlier than 5 days from the start of their use). The initial dose of warfarin is 5 or 7.5 mg once a day. For patients under 60 years of age and without serious concomitant pathology, an initial dose of 10 mg is acceptable. Warfarin is continued for at least 3 months[21].
Reperfusion therapy
The goal of reperfusion therapy is to remove the clot and restore normal pulmonary blood flow. Most often, thrombolytic therapy is used for this. It is recommended for high-risk patients. Some authors allow the use of thrombolysis at moderate risk, but the benefit of such therapy in this group of patients is currently unclear[22]. The following drugs are used:
- Streptokinase - loading dose of 250,000 IU over 30 minutes, then 100,000 IU per hour for 12-24 hours or accelerated regimen 1.5 million IU over 2 hours
- Urokinase - loading dose of 4400 IU/kg body weight for 10 minutes, then 4400 IU/kg body weight per hour for 12-24 hours or an accelerated regimen of 3 million IU for 2 hours
- Alteplase - 100 mg over 2 hours or accelerated regimen 0.6 mg/kg body weight over 15 minutes (maximum dose 50 mg)
Bleeding is the main problem of thrombolytic therapy. Massive bleeding develops in 13% of cases, and intracerebral hemorrhage occurs in 1.8% of cases.
Surgical methods
Kava filter.
Surgical removal of the blood clot (thrombectomy) is considered an alternative treatment for high-risk pulmonary embolism when thrombolytic therapy is contraindicated. In patients with a high risk of relapse and with absolute contraindications to anticoagulant therapy, vena cava filters can be installed[23]. They are mesh filters that catch blood clots coming off the wall and prevent them from entering the pulmonary artery. The vena cava filter is inserted percutaneously, usually through the internal jugular or femoral vein, and placed below the renal veins (higher in the presence of blood clots in the renal veins)[21].
Mechanism of development of cor pulmonale
In order to understand how pathology occurs in people, it is necessary to have a general understanding of how the process of gas exchange and blood circulation occurs in the human body.
These two processes are inevitably interconnected, since saturation of the blood with oxygen is possible only through the breathing process, and the breathing process itself depends on the saturation of the lungs with blood.
Naturally, these physiological functions are provided by the anatomical structure of the human body. Therefore, if there are violations in at least one system, the second inevitably suffers.
The blood is saturated with oxygen in the following way: venous blood is transferred to the right side of the heart, from where it is pushed by the heart muscles into the pulmonary artery. It is when the blood enters the lungs that it takes in the oxygen that was absorbed from the outside, and then the arterial blood enters the left side of the heart, subsequently spreading throughout the body.
Venous blood contains quite a lot of carbon monoxide. Its content is normal, because it is a natural element that is formed as a result of the vital activity of all the cells of our body.
The superior and inferior vena cava converge in the sinus, a small cavity located in the vestibule of the right atrium. After the blood remains in the atrium, it is transported to the right ventricle, which pushes the blood into the pulmonary artery.
It delivers blood to the lungs. Through many branched smaller vessels - arterioles and capillaries - the blood reaches the deepest parts of the lung. The main task of the blood is to move to the smallest alveoli, which take carbon monoxide from the blood and release oxygen into them.
In order for the process of direct gas exchange to take place with maximum benefit, the alveoli are intertwined with many capillaries. For proper exchange of oxygen and carbon monoxide, normal pressure is necessary, both from the circulatory system and from the alveoli.
Despite the fact that the vascular network is quite dense and the capillaries are very narrow, normally the human body is able to ensure blood flow under normal pressure even in the smallest vessel.
Some lung pathologies can cause capillary obstruction, as a result of which the pressure in this area will increase, because the blood volume does not decrease. The pulmonary artery will try to push blood into the lungs with high pressure to supply the entire organ. This is how pulmonary hypertension is formed.
Blood entering the left side of the heart transports oxygen throughout the body. The release is carried out into the aorta under significant pressure.
Pathological mechanisms occurring in the respiratory system also provoke changes in the heart. The situation can develop in two ways: in the acute form, the pressure rises rapidly, which means the right ventricle stretches quickly and to a significant volume.
The walls of the organ simply do not compress with enough force to transport blood to the pulmonary artery. In this case, some of the blood does not leave the ventricle. The new volume of blood from the atrium only further stretches the walls of the compartment.
The second option is gradual stretching of the cavity. This occurs during the chronic course of the pathology. The heart simply has time to adapt to such changes, while the muscle of the right ventricle grows due to an increase in the number of myocardiocytes. Thus, the right side of the heart increases not so much due to the expansion of the cavity, but due to the thickening of the walls of the section.
Despite the fact that the pathology manifests itself differently, the symptoms of the disease are similar in both cases.
Pulmonary artery
The pulmonary arteries are among the largest vessels in our body. They are laid in the embryonic period and develop from six arterial arches. The pulmonary artery belongs to the circulation of the same name. The pulmonary artery has branches on two sides, extending from the trunk.
The dilation of the pulmonary artery of the heart is about two and a half centimeters. The right artery is four centimeters longer than the left, and the left artery is a continuation of the pulmonary trunk.
Each of these arteries is immersed in the lung, allowing further gas exchange. Both arteries in the lung itself are divided into branches that penetrate the lobes. Normally, the pulmonary arteries provide a constant pressure of fourteen millimeters of mercury.
Functions
The pulmonary artery is the only vessel in the human body that transports venous blood. Therefore, the main function of this vessel is the delivery of venous blood to the lungs. This is why the condition of the artery and its physiological indicators are so important for human health.
| Chronic cor pulmonale |
|
| Thromboembolism |
|
| Stenosis |
|
| Valve insufficiency |
|
Along with other diseases, cor pulmonale often occurs. This is a pathology in which the pressure of blood flow in the pulmonary circulation increases as a result of overload of the right parts of the heart. Speaking in medical terms, hypertrophy (enlargement) of the right atrium and ventricle occurs and...
Cor pulmonale develops against the background of pulmonary hypertension, i.e. increase in pressure in the pulmonary circulation. As a result of hypertension, sooner or later pathological processes begin in the myocardium: thickening and stretching of the right ventricle. For effective treatment, the primary task is to identify and eliminate...
Chronic cor pulmonale, otherwise called kyphoscoliotic or emphysematous heart, is nothing more than hypertrophy of the right ventricle of the heart, which occurs against the background of diseases that cause dysfunction or disruption of the structure of the lungs (in some cases simultaneously). This does not include moments when...
Today, an increasing number of people are exposed to various heart diseases. Various reasons can lead to such pathologies, including existing ailments that cause serious complications. One of the most common pathologies is cor pulmonale. This is the name of a disease in which abnormalities in…
Pulmonary artery: pressure norm, what kind of blood flows, functions and diseases
The lungs are a paired organ of human air respiration. Without it, human life is impossible, so you need to monitor your condition carefully. For normal functioning you need an active lifestyle.
Fresh air and optimal physical activity will help reduce the risk of pulmonary artery diseases.
If you have health problems (for example, high cholesterol), exercise should be moderate so as not to provoke a deterioration in your health.
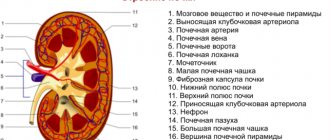
Structure of the pulmonary artery
The pulmonary artery is a vessel with a diameter of about 2.5 cm. Since there are two lungs in the human body, there are also 2 arteries (right vessel and left). They originate from the pulmonary trunk (one of the largest human arteries, which drains blood from the heart to the lungs). These vessels enter the gates of the lungs:
- right artery - to the right lung;
- left - to the left.
The right pulmonary artery of the heart is slightly longer than the left. The anatomy of an artery is complex. The wall of this vessel consists of three layers:
- internal;
- muscular;
- outdoor
The inner layer (endothelium) is adapted for the movement of blood through it. Muscular, located in the space between the endothelium and the outer one, complex in composition. Despite the name, it also includes connective tissue. The outer layer is the serosa.
On a note!
The pulmonary arteries are vessels of the muscular-elastic type. This means that in addition to muscle fibers, their walls have an elastic component.
This structure makes the vessels more elastic and is determined by the function they perform.
Functions of the pulmonary artery
The function of the pulmonary artery is to move venous blood from the heart to the lungs. From the school biology course we know that veins contain venous blood, and arteries contain arterial blood. The peculiarity of the pulmonary artery is that it contains venous blood. This gives her the opportunity to enrich the blood leaving the right side of the heart with oxygen.
In addition to this function, there are others. The lining of the artery walls performs the following functions:
- The outer shell does not allow the walls of the vessel to rupture, with constant pressure on it from the inside.
- The muscular (middle) layer controls the expansion of the vessel when blood is pushed out and controls the process of returning to its original form.
The inner lining (endothelium) contains receptors that are capable of detecting all changes: changes in blood pressure, changes in blood properties, narrowing of the lumens of blood vessels. The endothelium helps control these changes.
Types of diseases
When diseases of the pulmonary arteries occur, blood circulation worsens. The patient's condition gradually begins to deteriorate. There are several types of pathologies and each of them is dangerous in its own way. The causes also differ; some can be cured, while others become chronic. But in any case, if you feel unwell, you need to consult a doctor and get diagnosed.
Pulmonary embolism
Thromboembolism or PE is a life-threatening condition in which blood circulation deteriorates. The blood flow is impaired due to the embolus. This is a particle that, under normal conditions, should not be present in the blood.
Note!
An embolus can occur after various injuries (for example, fractures), after amputations of limbs, if the drug is administered incorrectly intravenously, or with the formation of blood clots (thrombi).
Thromboembolism comes in different groups (depending on the origin of the embolus):
- Thromboembolism by foreign bodies (clogging with shell fragments, pieces of catheter, bullet, etc.).
- Thromboembolism microbial or bacterial (clogging with clusters of microorganisms, fungi, protozoa, etc.).
- Tissue or cellular thromboembolism (impaired blood circulation in the artery due to pieces of tissue, a large number of cells. Such an embolus can form due to injuries, tumors).
- Fat thromboembolism (a fat embolus can form due to injuries with damage to fatty tissue or due to improper administration of an oil preparation).
- Air thromboembolism (blood flow disturbance begins due to the accumulation of bubbles in the artery that enter the blood from the outside. For example, during injuries, operations).
The degree of thromboembolism depends on the damage to the pulmonary vessels:
- Non-massive if less than a quarter of the lung vessels are affected.
- Average, if we come across from a quarter to half of the vessels.
- Massive if more than half of the lung vessels are affected.
Symptoms of this disease: acute respiratory and/or heart failure, drop in blood pressure and slowing of blood supply (collapse), respiratory arrest.
Pulmonary stenosis
Stenosis is a narrowing. It occurs at the valve site of the pulmonary artery. Because of this, a pressure imbalance is formed in the right ventricle of the heart and in the pulmonary artery. It takes more effort to push the blood out.
Gradually, the stenosis leads to an atrial septal defect. The right ventricle enlarges to cope with the increasing load (hypertrophy occurs). Right ventricular failure appears. Pulmonary stenosis can only be eliminated through surgery.
Pulmonary valve insufficiency
It is expressed in the inability of the artery valves to close completely. This problem causes venous blood to back up into the right ventricle. The load on the right ventricle increases. Valve insufficiency can be a congenital pathology, or it can also be acquired.
The patient develops the following symptoms: general weakness, sweating, attacks of shortness of breath, increased heart rate, and others.
Symptoms and diagnosis of pulmonary artery diseases
Symptoms of pulmonary embolism, pulmonary stenosis, and pulmonary valve insufficiency are similar. It is especially difficult to distinguish them at the initial stage of disease development. A person experiences:
- feeling of lack of air, shortness of breath;
- general weakness, lethargy;
- sweating;
- cardiopalmus;
- surges in blood pressure.
If these symptoms appear, you should consult a doctor. The doctor will collect anamnesis and prescribe diagnostics to confirm or refute the diagnosis. It is not recommended to postpone your doctor's appointment, because... processes may be irreversible.
Types of diagnostics:
- Laboratory research. An indicative study (especially for thromboembolism) is a blood test. A possible diagnosis can be judged by an increase in: the total number of leukocytes, the rate at which red blood cells settle, and the level of bilirubin.
- Angiography. It is considered an accurate study that allows you to quickly make a diagnosis. With this diagnostic method, the vessels are visible in volume. But such a study cannot be carried out in all clinics.
- Radiography. An X-ray is less informative than an angiography. But with its help, you can exclude other diseases and continue the diagnosis process.
- Electrocardiogram (ECG). This is an accessible study, the results of which can be deciphered immediately. An ECG transmits electrical impulses from the heart using electrodes. If there is a blood clot and poor circulation, electrical impulses will not be transmitted normally. The result of this research is printed by the device on paper.
- Scintigraphy. This study is carried out with the introduction of a radioactive drug intravenously. It will help you see in which areas of the vessels blood circulation is impaired.
To clarify the diagnosis and determine the severity of the disease, the doctor selects several diagnostic methods simultaneously.
Prevention
Certain categories of people need prevention: those with obesity, those with diabetes, those over 40 years old, after a stroke or heart attack. The risk category includes people who previously suffered from pulmonary embolism, stenosis, pulmonary valve insufficiency, and who have varicose veins.
Prevention of pulmonary artery problems:
- Blood pressure control. Self-guided at home. They use a tonometer, which can be purchased at any medical equipment store or pharmacies.
- Avoid being overweight. It strains the heart, increasing the likelihood of high blood cholesterol and blood pressure problems.
- Control the level of cholesterol in the blood, because it affects the condition of blood vessels in the body. As cholesterol levels rise, cholesterol plaques begin to form on the walls of blood vessels. If they are torn off, pulmonary artery stenosis may occur;
- Quitting bad habits (smoking and drinking alcohol).
Note!
You need to watch your diet. Fatty, fried foods, overeating, contribute to excess weight, increased cholesterol levels, and more.
If you have diseases that provoke problems with the pulmonary arteries, follow all doctor’s prescriptions (for example, use compression stockings for varicose veins). Follow the recommendations in the period after surgery.
Treatment methods
Thromboembolism is a condition that requires urgent intervention. A patient with this diagnosis is placed in intensive care and placed on strict bed rest.
Use an oxygen mask or another method of oxygen supply to avoid oxygen starvation. A venous catheter is installed.
The faster these measures are carried out, the less likely the development of negative consequences (impaired blood supply to the lungs, development of chronic pulmonary hypertension and sepsis).
Vessel stenosis, if pronounced, is eliminated surgically. To maintain the general condition of the patient and prevent the development of complications, the doctor prescribes medications.
Valve insufficiency in severe cases is eliminated surgically. In other conditions, drug treatment is used.
Medications
In the case of pulmonary embolism, medications are prescribed: heparin intravenously, antibiotics if necessary, dopamine and more. They supply oxygen.
For stenosis, the following may additionally be prescribed:
- diuretics;
- drugs against acute and chronic heart failure (glycosides);
- calcium channel blockers and others.
Valve insufficiency requires prescription:
- antibiotics;
- nitric acid salts to dilate blood vessels;
- diuretics;
- ACE inhibitors (block the process of vasoconstriction).
Traditional methods
Traditional methods are used only after consultation with the attending physician and diagnosis. Self-prescribing treatment for yourself can lead to a worsening of the condition.
One of the recipes that helps reduce blood cholesterol levels and strengthen the walls of blood vessels includes:
- Dill seeds;
- honey;
- water.
For 2 liters of water, use dill and honey in a ratio of 1 glass to two. The mixture of seeds and honey is poured with boiling water and left for a day in a thermos. Next, the infusion is filtered and stored in the refrigerator.
Take orally twenty minutes before meals, a tablespoon four times a day. After the infusion is over, you need to take a week break.
If an allergic reaction occurs, stop taking it.
Other methods
These are methods that involve surgical intervention. Severe degrees of stenosis can only be eliminated using this method. Used: excision of the affected vessel wall, separation of the vessel walls, excision of the affected area of the myocardium.
Valve insufficiency in severe cases is corrected surgically:
- valve prosthetics (there are mechanical valves and biological valves);
- plastic surgery of your own valve;
- heart and lung transplant (performed in rare cases when the heart is significantly damaged).
It is possible to simultaneously correct several pathologies.
Possible complications
With thromboembolism of the pulmonary artery, its stenosis, or valve insufficiency, serious complications can occur. They mainly develop if treatment is started late and the patient has a malfunction of the immune system
More common:
- Pneumonia (inflammation of the lungs of infectious origin).
- Pleurisy (inflammation of the lining of the lungs).
- Lung abscess (formation of a nonspecific cavity “ulcer” in the lining of the lung).
- Lung infarction (the process of necrosis of its tissues due to deterioration of blood circulation).
- Acute renal failure (deterioration of filtration function).
- Pneumothorax (presence and accumulation of gas in the pleural cavity).
Vascular problems increase the risk of liver cirrhosis.
The consequences of pulmonary artery diseases develop rapidly. If you have these symptoms, it is important to consult a doctor who can make a correct diagnosis.
Source: https://sosud-ok.ru/serdce/legochnaya-arteriya.html