Arteriovenous malformation is a disease that represents the formation of lesions with a pathological connection between the arterial and venous vascular networks.
Normally, the cardiovascular system functions as follows.
From the aorta, which is the largest artery in the human body, a whole network of arterial vessels departs, which alternately divide, acquiring smaller and smaller diameter. Arteries become arterioles, which subsequently become capillaries. These are small vessels, the wall of which consists of only one layer of cells. In these capillaries, gas exchange occurs between the cardiovascular system, which contains oxygen-enriched blood, and the tissues and organs of the human body.
Subsequently, the processed blood, which has given up oxygen and is enriched with carbon dioxide, through the same capillaries, the blood enters a vein of larger diameter, and it flows into larger and larger veins and eventually enters the superior and inferior vena cava and back into the chambers of the heart.
In the presence of a focus of arteriovenous malformation at a level above the capillary artery and vein are connected incorrectly, often confused, and dilated. Therefore, in this place, arterial blood does not enter the capillaries, and therefore cannot enrich nearby tissues and organs with oxygen. Blood from the artery immediately enters the venous bed, bypassing the capillaries, and returns back to the heart.
In fact, arteriovenous malformation is an arteriovenous fistula or arteriovenous shunt. The difference between these pathological conditions is that arteriovenous malformation is a congenital disease inherent in the child from the moment of birth.
What is the essence of the disease?
This deviation is more common in the brain, in the posterior regions of the hemispheres; the thoracic or cervical spine is often affected. An anomaly also occurs in the spinal cord, but it is rare. Arteriovenous malformation varies from one centimeter to a very large size in the cranial cavity.
The resulting defect usually looks like a tangle of thin, thinned and tortuous vessels, in which arteries and veins meet directly, which occurs without the participation of capillaries. Thus, arterial blood does not enrich tissues and organs in any way.
This disease is chronic in nature and occurs mainly in young men. In one family, such a pathology sometimes manifests itself in several members at once, but it is not considered hereditary. The pathology first appears between the ages of ten and thirty, and its peak occurs at the age of twenty. Violation of vascular formation occurs in the second month of fetal development, and the exact causes of this anomaly have not been established. The incidence of the disease in the world is one person per hundred thousand people.
Symptoms
Arterial-venous malformation has two course options:
Hemorrhagic
Occurs in 60% of all malformations. This type of flow predominates with small shunts where there are draining veins. Also found in the occipital regions of the brain. The dominant syndrome is arterial hypertension with a tendency to hemorrhagic stroke. With a latent course, the disease is asymptomatic.
An exacerbation of the hemorrhagic course is characterized by a rapid increase in headache, disturbance of consciousness and disorientation. Suddenly a part of the body goes numb, most often one side of the face, a leg or an arm. Speech becomes disordered according to the type of aphasia, and the grammatical component of sentences is disrupted. Sometimes the understanding of oral and written speech is impaired. The consequences of hemorrhagic course are stroke and long-term recovery of neurological functions.
Fields of vision are lost, and its accuracy decreases. Sometimes diplopia occurs - double vision. Less commonly, vision is completely lost in one or both eyes at the same time. Coordination is impaired: gait becomes unsteady, movements lose precision.
Torpidny
Torpid is the second flow option.
Venous malformation of this type has a characteristic feature – cluster cephalgia. Characterized by acute, difficult to tolerate and severe headaches. Sometimes the pain syndrome reaches such a height that sufferers commit suicide. Cephalgia appears as periodic episodes (cluster) of pain in the head and is practically unresponsive to non-steroidal anti-inflammatory drugs.
Due to strong pain irritation, the following symptom complex is formed - petit epileptic seizures. They occur in 20-25% of patients. The attack is characterized by contraction of the eye muscles and spasms of skeletal muscles. Some develop a grand mal seizure with the manifestation of typical clinical pictures (aura, warning signs, tonic convulsions, clonic convulsions and exit from the state).
Arteriovenous malformation can mimic a brain tumor. In this case, focal neurological deficit symptoms are observed. For example, if the malformation is located in the frontal gyri, a motor disorder such as paresis or paralysis is recorded. If in the parietal region, sensitivity in the limbs is impaired.
Development mechanism
Normally, oxygenated blood flows from the heart to various tissues and organs. At first it passes through the arteries. Then the artery turns into an arteriole, through which blood flows into the capillaries. Here is the capillary bed in which cellular exchange occurs. The cells take oxygen from the arteries, releasing waste products with carbon dioxide. The blood then flows further through the veins, from there rising again to the heart.
In the presence of arteriovenous malformation, blood from the arteries enters the veins through a tube called a fistula, and hypoxia develops directly in the tissues. Increased pressure occurs in the veins through which blood passes.
Over time, fistulas can gradually expand and enlarge, and the arterial walls thicken. If the malformation is very developed, then the blood flow in it turns out to be strong, and at the same time cardiac output increases. In such cases, the arteries and veins look like giant pulsating vessels. They are not able to withstand such pressure because they are not designed for this, so they stretch and often break. A similar condition of blood vessels can be observed in any part of the body. If the malformation affects only the veins, then they speak of the presence of venous angioma.
General information about pathology
The term “malformation” is usually understood as a congenital pathology of lymphatic vessels, veins and arteries.
The exact causes of the anomaly are currently unknown. Some experts believe that malformation (arteriovenous) occurs due to intrauterine injuries to the fetus. At the same time, professionals are inclined to believe that there is no direct connection between the presence of an anomaly and the gender, as well as the age of the patient.
Some popular hypotheses claim the opposite.
Risk factors include:
- Male gender.
- Genetic predisposition.
This defect in vascular development is classified into 5 main groups:
- Hemangioma and other vascular angiomas. This group includes benign neoplasms that develop directly from the vascular wall. This tumor can occur in various human tissues and organs. As a rule, it is accompanied by cosmetic defects, as well as dysfunction of organs.
- Arteriovenous fistulas. An acquired or congenital anomaly, characterized by the formation of an anastomosis between an artery and a vein, through which arterial blood begins to flow directly into the venous system, bypassing the capillary bed.
- Arteriovenous pathological connections. This disease occurs due to pathology of blood vessels. The formation of arteriovenous malformations can occur where veins and arteries are located. The most dangerous to human health are those that form in parts of the brain or spinal cord.
- Venous. This type of anomaly is considered the most common vascular pathology. Pathology can cause damage not only to the internal organs of a person, but also to muscles, bones, and skin.
- Lymphatic. These are congenital pathologies, the structure of which consists of thin-walled cysts of various shapes and sizes. This disease is much less common than other vascular pathologies.
Malformation: main symptoms
Very often, arteriovenous malformation does not manifest itself in any way. The pathology is discovered accidentally when performing a CT or MRI for stroke, spinal cord injury, etc.
The disease manifests itself when the formation increases in volume and puts pressure on the brain.
When intracranial pressure increases, cerebral symptoms occur.
Among them:
- bursting headache, often accompanied by vomiting;
- decreased ability to work and lethargy.
If the arteriovenous malformation is localized in the frontal lobe, the patient suffers from:
- decreased intelligence,
- manifestations of foolishness,
- speech disorders,
- unsteadiness of gait,
- seizures
With pathology in the cerebellar area, the following symptoms appear:
- sweeping and unclear movements,
- deviation to the side when walking,
- pendulum-like eye movements,
- decreased muscle tone.
If the pathology is localized in the temporal lobe of the brain, the patient may experience problems such as:
- speech disorders, misunderstanding of the interlocutor’s phrases;
- loss of visual fields;
- convulsive attacks that are observed both in the limbs and throughout the body.
With pathology of the base of the brain (bottom), symptoms may include:
- impaired movement of the eyeballs,
- strabismus,
- visual impairment,
- paralysis.
In cases of spinal cord pathology, the following disorders are noted:
- all types of sensitivity in the hands or feet,
- motor activity.
Connections often fail. In this case, the blood supply to the spinal cord and brain is reduced.
If blood enters the space between the brain and the membranes, the patient experiences a sudden headache and may lose consciousness. Photophobia, vomiting and nausea also develop.
If blood enters the brain matter, a hematoma is formed. Possible manifestations include:
- visual impairment, speech impairment;
- convulsions;
- paralysis of limbs.
In some cases, the patient loses consciousness.
If a rupture occurs in the spinal cord, paralysis of the limbs develops.
Request a call back Get a free consultation
Varieties
Based on their structure, the following varieties are distinguished:
- A malformation in which there are no veins in the tangle of vessels, there are only arteries.
- In the dura mater, a fistulous type of arteriovenous malformation may occur.
- Racemotic branched malformation occurs in seventy-five percent of cases.
- Cavernous malformation occurs in eleven percent of cases. There are only small capillaries in it, and arteries and veins are completely absent here, the pressure is not disturbed. The subspecies in this case is telangiectasia.
By size they are distinguished:
- Micromalformation is considered the smallest in size.
- Minor malformations, which are less than one centimeter.
- Small malformations, whose size is from one to two centimeters.
- Up to four centimeters are medium malformations. Their risk of rupture is quite high.
- Up to six centimeters are large malformations that are very dangerous.
- More than six centimeters are already gigantic, and they rupture less often, but they are difficult to cure.
Arteriovenous malformation is divided according to the nature of drainage and its location. It can be located in the cerebral cortex, that is, directly on its surface. In this regard, they are also called cortical. Other forms are internal malformations, which are often located in the brainstem or hypothalamus. An arteriovenous fistula may be located inside the dura mater.
Causes of AVM
Acquired nosology occurs against the background of traumatic damage to cerebral vessels. Congenital forms are caused by genetic defects and diseases of a pregnant woman during pregnancy. The exact causes of the pathology have not been established, but provoking factors have been identified:
- Hereditary predisposition;
- Male gender.
Little knowledge of the problem leads to the emergence of new hypotheses, but the evidence base is weak, which makes etiological treatment impossible.
Arnold-Chiari malformation - what is it?
The congenital anomaly is combined with an abnormal location of the cerebellar tonsils. There are several variants of pathology. Arnold-Chiari malformation is characterized by impaired circulation of cerebrospinal fluid, which is accompanied by pathology of the tonsils. Metabolic processes in Arnold-Chiari malformation type 1 lead to hydrocephalus and hydromyelia in children and adolescents.
Experts consider the main cause of the nosology to be an increase in pressure in the cerebellum with subsequent displacement of the tonsils.
Main symptoms of nosology:
- Constant headaches that are not relieved by medications;
- Loss of sensation in the legs;
- Swallowing disorders;
- Vomiting reflex;
- Unsteadiness of gait.
The pain syndrome is localized mainly in the occipital region. Intensifies during coughing and physical activity.
Magnetic resonance imaging (MRI) allows for a correct diagnosis. The three-dimensional modeling mode allows you to visualize the spatial picture of the brain.
Features of Dandy-Walker malformation
A congenital anomaly of the fourth ventricle of the brain is combined with pathological anastomosis between arteries and veins. Dandy-Walker AVM occurs in the presence of cerebellar hypoplasia, and hydrocele may be present. The danger of the nosology is superior herniation.
Clinical symptoms:
- Slowdown of the functionality of the intelligent system;
- Pathology of movement coordination;
- Epileptic convulsions;
- Spasmodic muscle contractions.
Epilepsy occurs in fifteen percent of patients.
Pathological malformations can be traced not only from the brain, but also from the spinal cord. Symptoms depend on the predominant location of the hemorrhage.
Symptomatic manifestation of brain malformation
Arteriovenous malformation of the cerebral vessels, also called cerebral, is accompanied by the following main symptoms:
- The appearance of cephalgia of varying intensity, without any characteristics of regularity and duration. In this case, the pain does not coincide with the localization of the malformation, and its intensity is different.
- Presence of seizures. In this case, general or partial convulsions are observed in various parts of the body. There is no loss of consciousness.
- The appearance of dizziness and fainting.
- Development of muscle weakness along with paresis of the limbs.
- If the cerebellum is affected, gait is impaired. In this case, staggering and loss of coordination are observed.
- There may be loss of vision in the frontal lobes.
- The appearance of dysarthria.
Symptoms of arteriovenous malformation of the right parietal lobe may not appear for a very long time and are sometimes accidentally discovered during examinations.
Main symptoms of the disease
Arteriovenous malformations manifest themselves in two types: hemorrhagic (the most common) and torpid. Their symptoms are somewhat different from each other. In the first case, high blood pressure occurs, in the second, neurological disorders come to the fore: motor and sensory disorders, dizziness, convulsions, fainting.
This difference in the signs of the disease in two different types is due to their pathological structure: in the hemorrhagic variant, the tangle of vessels is small in size, while in the torpid variant it is larger, localized in the cerebral cortex and supplied with blood from the middle artery of the brain. Both types may be accompanied by headaches.
However, in most cases, the symptoms of arterial-venous malformations do not appear for a long time, and the disease can be discovered either accidentally during a tomography, or after a hemorrhage has occurred.
Small vascular tangles are more dangerous in terms of hemorrhage than large ones. Also, the risk of rupture increases if the pathology is localized in the basal ganglia and posterior cranial fossa. According to population studies, 40–70% of all vascular malformations end in hemorrhage. In this case, death occurs in 10–15% of patients.
Vascular malformation of any type can be localized in any part of the brain, so if symptoms are detected, they are associated with the location of the pathology relative to the structures of the brain (compression of some parts may occur) . For example, its location in the frontal lobe can lead to disruption of the optic nerve and, as a consequence, visual impairment. The focus of pathology in the cerebellum leads to coordination disorders. The deeper the vascular tangle is, the more severe the symptoms.
Occasionally, a malformation can go away on its own - it completely regresses without any treatment, or suddenly increases in size, which can be fatal if it ruptures. In this case, removal of the formation is required.
Neuralgic symptoms
As the malformation grows and pressure begins to put on the brain, neurological symptoms occur. The following manifestations may be present:
- Intracranial pressure increases, there is persistent pain in the head of a pressing or pulsating nature.
- The appearance of apathy, lethargy, decreased performance.
- Impaired coordination of movements.
- Decrease in intelligence level.
- The appearance of speech disorders in the form of motor aphasia.
- Failure of innervation of certain areas of the body.
- Unsteady gait with sudden falls on the back.
- The appearance of cramps and muscle hypotension.
- Paresis of the limbs.
- Vision problems in the form of strabismus or blindness.
Against the background of the gradual development of arteriovenous malformation of cerebral vessels, neurological symptoms can increase sequentially. Upon reaching middle age, the disease becomes stable, and new disorders no longer arise. Women may feel worse and develop new symptoms if they become pregnant. Hemorrhagic stroke in pregnant women is caused by this disease in twenty-three percent of cases.
Lungs
Arteriovenous malformation of the pulmonary vessels can occur as a result of trauma, diseases of the liver, thyroid gland, and repeated diseases of the bronchi. Pulmonary vascular disease is a little known and also a congenital disorder. According to statistics for one year, a maximum of one case can be identified.
At the initial stage of development of arteriovenous malformation of the pulmonary vessels, symptoms do not appear. In case of acute complications, difficulty breathing and vascular insufficiency appear.
You can visually observe swelling of the fingers. Coughing with the release of blood masses is just a symptom and does not pose a great danger.
Coughing up blood is one of the symptoms of pulmonary vascular malforation
Diagnostics
Most people with lung malformation have a sharp, round formation in the lower part of the lungs. With repeated disease, x-rays show an average of up to 110 such formations. You can get a more detailed picture of the feeding artery using a tomogram.
Changes in the pulmonary vessels reveal the following symptoms:
- attacks of headache;
- spasms;
- damage to the functions of blood vessels in the brain;
- hemorrhages in the lungs;
- chronic disorders of the heart;
- anemia;
- inflammation of the inner lining of the heart.
Treatment
With age, the symptoms of pulmonary vascular malforation intensify and have a disappointing prognosis. During this period, treatment occurs at a surgical level to block the artery or compress it. The first way to eliminate bleeding, using special spirals, gives more effective results.
Arteriovenous malformation of the spinal cord
In this case, the symptoms will be as follows:
- Problems with sensation in the limbs, for example, pain or touch may not be felt.
- The occurrence of intense pain.
- The appearance of sudden progressive paralysis of the lower extremities. Arteriovenous malformation is a very serious disease.
- The appearance of tingling in the limbs.
- Failure of sphincteral activity and urodynamics, when it is impossible to control defecation or urination.
Most people recover almost completely from the first attack, but there is a risk of further symptoms. If left untreated, over time the patient may become helpless and will be completely dependent on his loved ones.
Symptoms of ruptured blood vessels
Vascular rupture due to malformation is possible in every second patient. Increased workload, stress and alcohol consumption play a significant role in this. Hemorrhage occurs suddenly. Often it is subarachnoid in nature. The symptoms are similar to a stroke. The patient complains of a severe headache, from which he may even lose consciousness. Vomiting occurs for no apparent reason, and after cleansing the stomach, no relief appears. Fainting occurs. Irritation appears with pain in the eyes, which is caused by bright light, vision is impaired, complete blindness develops, and speech impairments are noted.
Convulsive seizures along with hearing loss cannot be ruled out. Visual disturbances may occur, and paralysis of the limbs may develop. When hematomas appear, meningeal syndrome is often diagnosed, and the pressure is increased. The next day the temperature rises. With proper treatment, after five days you will feel better. After a hemorrhage in the first year, the risk of recurrence remains. Moreover, if treatment is not carried out, the risk increases threefold.
Carrying out diagnostics
Patients most often seek help after hemorrhage. The doctor conducts a detailed examination of the patient, determines the presence of injuries and diseases, and determines the neurological status. Then a computer and magnetic resonance imaging scan and an angiogram are prescribed.
These methods for diagnosing AVMs allow for a layer-by-layer study of the brain structure, in which the location of the malformation and its size are determined, and the general condition of the brain is assessed. With computed tomography, X-rays can be used to identify an abnormality within the parenchyma. When performing CT angiography, the arteries of the brain are even more detailed. CT scan is the fastest method, but not the most effective, it is more suitable for detecting hemorrhage.
MRI for arteriovenous malformation is more informative. Thanks to it, this disease is easily detected and the severity of the patient’s condition is determined. A cerebral angiogram also assesses the patient’s condition very accurately, but this is a rather expensive examination. As part of the procedure, a catheter is inserted into a peripheral artery and advanced to the vessels of the brain. Afterwards, pictures of the vessels are taken. Although there is a risk of complications after this manipulation, only this method allows one to accurately determine the causes of hemorrhage.
Electroencephalography determines foci of excitation, finding the zone of its localization. When performing Doppler ultrasound, doctors determine the speed of blood flow and examine the spatial position of the vessels in the affected area. Angiography is also performed. But this procedure takes a long time, and it is done under anesthesia. Angiography is indispensable when it is necessary to determine the venous increase in pressure; this is very important in the selection of surgical treatment of arteriovenous malformation (ICD Q28.2.).
Diagnostics
Vascular malformation, concentrated in the right or left region of the brain, requires timely detection and treatment. A neurologist diagnoses the disease. Procedures that can be informative in terms of detecting vascular pathology:
- EEG.
- Echo-EG.
- REG.
If a patient is admitted to the hospital with acute cerebral symptoms, he is urgently given a CT or MRI. The second type of tomographic study is considered more informative. With the help of MRI, it is possible to visualize the location of the breakthrough, determine its extent and distinguish it from other neoplasms, for example, from a cyst, angioma or hematoma.
If a rupture does not occur, and the disease proceeds according to the torpid type, then classical brain tomography will not provide complete information. The vascular bundle can only be detected using CT or MRI of the vessels. The procedure is performed using a contrast agent.
The data obtained must be interpreted by a neurosurgeon. It is he who determines the further tactics of patient management.
Carrying out surgical treatment
This method involves complete removal of the malformation with a volume of up to 100 milliliters. The surgical technique involves opening the skull to identify the malformation. In addition, it is subsequently cauterized with a laser or using other instruments. The cauterized area is completely removed from the tissue. If the operation is successful, the patient recovers completely. But complications are nevertheless possible in the form of strokes.
After the operation, a full rehabilitation course is carried out for one week. After the patient is discharged, he is recommended treatment with nootropics and angioprotectors. As part of prevention, it is necessary to periodically be examined by a vascular surgeon and neurologist, and also undergo magnetic resonance imaging.
Treatment of brain AVM
Treatment consists of surgical removal of pathological vessels. Classical open excision of a malformation is used mainly only in emergency cases, when a vessel ruptures, when it is necessary not only to remove it, but also to aspirate the resulting hematoma.
In case of uncomplicated malformation, one can resort to angioembolization, when an embolic substance is injected into the pathological vessel, its lumen is permanently closed and the vessel functionally disappears.
The most modern method is radiosurgery, during which the malformation is irradiated, leading to complete closure of the lumen of the vessel.
Embolization, or Performing Endovascular Surgery
Endovascular surgery involves removing the malformation from the general bloodstream by gluing the vessels. Against this background, complete gluing of blood vessels is feasible in thirty percent of patients; in other patients it turns out to be partial. This technique is very often used and is effective in preventing hemorrhages. The embolization technique in endovascular surgery involves the supply of a special adhesive element through a catheter.
Carrying out radiosurgical treatment
When using this method, obliteration of the malformation is possible when its size is less than three centimeters. Eighty-five percent of patients recover after such surgery for arteriovenous malformation. This method is used when the localization of the malformation is inaccessible for classical surgery. As part of this technique, radiation is focused and directed to the site of the anomaly; this procedure lasts exactly an hour. Next, the vessels sclerose on their own within two years and are replaced by connective tissue. The disadvantage of this technique is that before the development of sclerosis, hemorrhage may occur in this area.
Currently, various types of operations are actively combined. This allows you to expand the possibilities of radical approaches, reducing the percentage of complications.
Treatment of arteriovenous malformation of the spinal cord is carried out using surgery. It is also possible to use an interventional method. The latter method is less invasive. It involves the introduction of a special adhesive element, which immediately hardens, clogging the vessel. When using this method, there is a risk of damage to healthy blood vessels. In this regard, the substance is administered as close as possible to the anomaly.
Sometimes special microspirals are introduced that are adjacent to the abnormal vessels and block blood access to them. In addition, the detachable helices subsequently help the development of collaterals. The blockade of blood vessels is carried out with a substance that resembles sand particles. But such particles can lead to new recanalization. In this regard, for preventive purposes, angiography should be performed annually. If a malformation is discovered, embolization is repeated. It is usually carried out under anesthesia, and the procedure lasts from three to six hours. If the patient experiences slight pain in the incision area after the procedure, analgesics are prescribed.
ARTERIOVENOUS MALFORMATIONS (AVMs) are a congenital anomaly of the development of the vascular system of the brain and are tangles of various shapes and sizes formed as a result of the random interweaving of pathological vessels.
The total incidence of angiomatous malformations is 19 per 100,000 population per year.
Arteriovenous malformations (AVMs) are the cause of non-traumatic subarachnoid hemorrhage in 5% - 10% of cases.
AVM rupture usually occurs between the ages of 20 and 40 years.
In arteriovenous malformations, most often, there is no capillary network, resulting in direct shunting of blood from the arterial basin to the system of superficial and deep veins.
Types of Vascular Malformations:
| A) arterial B) arteriovenous fistulous C) arteriovenous racemose (75%) D) arteriovenous micromalformation E) arteriovenous cavernous (11%) F) Telangiectasia G) Venous |
Clinic of arteriovenous malformations.
1.
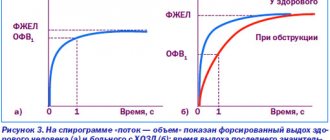
Hemorrhagic type of the disease - in 50 - 70% of cases. This type of course is characterized by the patient having arterial hypertension, a small size of the malformation node, its drainage into the deep veins, as well as an AVM of the posterior cranial fossa. 2. Torpid type of flow , typical for patients with large AVMs, its localization in the cortex, blood supply from the branches of the middle cerebral artery. Hemorrhagic type
In 50% of cases, it is the first symptom of AVM, which causes death in 10-15% (with aneurysms up to 50%) and disability in 20-30% of patients. (N. Martin et al.,1994). The annual risk of hemorrhage from an AVM is 1.5–3%. During the first year after hemorrhage, the risk of recurrence is 6% and increases with age. (R. Braun et al., 1990). During life, repeated hemorrhage occurs in 34% of patients who survived the first, and among those who suffered a second (mortality rate up to 29%) - 36% suffer from a third. (G. Rasmussen 1996). Bleeding from AVM is the cause of 5-12% of all maternal deaths, 23% of all intracranial hemorrhages in pregnant women. (B. Karlsson et al., 1997) The picture of subarachnoid hemorrhage is observed in 52% of patients (Lebedev V.V., Krylov V.V., 2000). In 47% of patients, complicated forms of hemorrhage occur: with the formation of intracerebral (38%), subdural (2%) and mixed (13%) hematomas; ventricular hemotompanade develops in 47%.
Torpid type Convulsive syndrome (in 26–67% of patients with AVM) Cluster headaches. Progressive neurological deficit, as with brain tumors.
| All arteriovenous malformations (AVMs) have a typical structure: 1,2 - afferent arteries (terminal and transit types) 3 - a tangle of altered vessels (core) 4 - draining vein |
The main mechanisms of the pathological effect of arteriovenous malformation on the brain : - Rupture of pathologically altered vessels of the tangle or aneurysms of the arteries feeding the AVM. — Chronic circulatory failure caused by arteriovenous shunting. — Normal perfusion pressure breakthrough syndrome.
Typical localization of arteriovenous malformations of the brain.
Diagnosis of arteriovenous malformations is the same as for subarachnoial hemorrhage or brain tumor (depending on the type of course).
| MR angiography of a patient with arteriovenous malformation | CT angiography | Angiogram |
Classification of arteriovenous malformations.
There are many classifications of brain AVMs (by size, location, morphological characteristics, etc.), but the following is most often used in the clinic:
Classification of AVM (according to Spetzler-Martin, 1986)
| By size: Less than 3 cm – 1 point 3 – 6 cm – 2 points More than 6 cm – 3 points By localization: Outside the functionally significant zone* – 0 points Within the functionally significant zone – 1 point AVM division according to the nature of drainage: Absence of deep draining veins – 0 points Presence of deep draining veins** – 1 point | According to this classification, most neurosurgeons determine degree of operability of malformation. There are 5 gradations of malformation : with gradation I (1 point), the risk of surgical intervention is insignificant, with gradation V (5 points), great technical difficulties arise, and the risk of severe disability and death is high. |
| * Functionally significant areas - sensorimotor area, Broca's and Wernicke's centers, occipital lobes, thalamus, deep structures of the temporal lobe, brainstem. ** Deep venous collectors are draining veins that flow into the system of the great cerebral vein, the straight sinus. | |
Treatment methods for arteriovenous malformations.
1.
Surgical : open operations, endovascular interventions 2. Conservative 3. Radiosurgery
Principles of providing surgical care to patients with AVM. 1. Complete treatment of patients with AVM requires the possibility of three main treatment options - surgical, embolization, radiosurgery. 2. The decision on treatment tactics and surgical intervention for AVM should be made by a surgeon who has personal experience in this field. 3. When discussing the issue of indications for active methods of treatment of patients with AVM, they proceed from the ratio of the risk of spontaneous course of the disease and the risk of complications of a particular treatment method. 4. The main goal of any type of intervention is complete obliteration of the malformation to prevent intracranial hemorrhage.
Surgery.
• The risk of surgery must be weighed against the risk of the natural history of the disease. • The purpose of the operation is complete excision of the AVM, because even if fragments are left, the risk of hemorrhage remains and even increases.
Classic method of AVM removal.
| Coagulation of afferents. | Isolation of the AVM node. | Ligation of efferent vessels and removal of AVM |
Endovascular operations.
Types of intravascular embolization of AVM 1. Embolization in the flow (uncontrolled). 2. Stationary balloon occlusion of the feeding arteries of the spinal column. 3. A combination of temporary or permanent balloon occlusion with flow embolization. 4. Superselective embolization or thrombosis of AVM. (N-butylcyanoacrylate (Hystoacryl) + fat-soluble contrast agent).
Radiosurgical treatment.
Indications for radiosurgery : 1. Malformations with a diameter of less than 3 cm, inaccessible for direct surgical removal. 2. Remains of an AVM of the same size after direct or endovasal operations.
The degree of radicality of various AVM treatment methods
— Surgical treatment – radical extirpation of AVMs with a volume of up to 100 ml is technically feasible. - Embolization - radical exclusion of AVM from the bloodstream is possible in 10-40% of patients, in other cases - obliteration of AVM occurs in 15-75%. — Radiosurgical treatment – complete obliteration of SM with a diameter of less than 3 cm is possible in 85% of patients (over 2 years).
Currently, combined treatment methods are actively used (embolization + surgery and/or radiosurgery and other combinations). This can significantly reduce the risk of complications and increase the radicality of the intervention.