Distinctive features of veins
The walls of the veins have a thinner layer of smooth muscle, and at the same time they are less elastic. This can be explained by the fact that in the veins the blood pressure is several times lower than in the arteries. Veins contain valves that move blood flow in the right direction. In turn, there are no valves in the arteries, because the blood flows there under very high pressure. Now that it has become clear how the veins differ from the arteries of the lower extremities, it is worth describing the diseases associated with this important part of our body. Today, a large number of such diseases are known, the most common of which are presented in this article.
Problems with blood circulation can occur in various parts of the human body, and they are associated with disorders in the arteries and veins of the lower extremities. If the walls of blood vessels have changed under the influence of certain pathologies, then blood circulation will be impaired. Ischemia can occur in the intestines or kidneys, or in the spinal cord. It is worth noting that a spinal stroke rarely leads to a heart attack or cerebral hemorrhage, but can cause disability and permanent loss of movement in a person’s lower limbs.
Perforating veins
Perforating vessels are designed to connect the veins of two systems to each other. Their number can vary between 53-11. But only 5-10 vessels, which are most often located in the lower leg area, are of primary importance for the venous system of the lower extremities. The most significant perforators for humans are:
- Coquette. The vessels are located in the tendon zone of the lower leg;
- Boyd. Located in the upper part of the lower leg in the medial region;
- Dodda. In the lower part of the tibia on the medial surface;
- Gunther. Localized on the surface of the thigh in the medial zone.
In a normal state, each such vessel is equipped with valves, but during thrombotic processes they are destroyed, which entails trophic disorders of the skin in the lower extremities.
Venous vessels of this type have been studied quite well. And, despite the sufficient number, you can find their localization zones in any medical reference book. By location they can be divided into the following groups:
- medial zone;
- lateral zone;
- back zone.
The medial and lateral groups are called straight because they connect the superficial veins with the posterior tibial and peroneal veins. As for the posterior group, they do not merge with large venous flows, but close only on the muscular veins. Therefore, they are called indirect venous vessels.
Causes of vascular diseases
Pathologies of the arteries and veins of the lower extremities can arise for a variety of reasons. The main ones include the following:
- The person is not eating properly.
- Insufficient amount of movement and physical activity.
- Presence of chronic diseases.
- Genetic predisposition.
- Various injuries.
- Long period of immobilization.
Most often, problems with the arteries and veins of the lower extremities occur in older people. This is not explained by the fact that in old age a person begins to move less. The main factor is a change in the vascular wall; the elasticity of veins and arteries also decreases several times.
Anatomy of the veins of the lower extremities (lecture at Diagnostic) – Diagnostic
The venous network of the legs organizes the return of blood to the right heart in defiance of gravity.
A duplicate of the superficial and muscular fascia divides the deep and superficial veins.
The superficial and muscular fascia originate from the ecto- and mesoderm layers, respectively.
The superficial vein system is born along the nerves: femoral, sciatic, cutaneous nerves.
Deep veins are formed from lacunae near the arteries, their development runs parallel to the arteries.
Veins above the muscular fascia collect blood from the skin and subcutaneous fat; pump 10% of the blood.
The veins under the muscular fascia along the arteries take blood from the muscles and bones; pumps 90% of the blood.
The superficial and deep veins are connected by perforators directly or circumferentially by muscle veins.
Perforators maintain the balance of superficial and deep veins; a greater number in the lower sections.
The lower leg muscles are like a pump - at rest, the deep veins are filled, contraction pushes the blood.
The intimal layer is composed of extended endothelial cells on a substrate; organizes vein valves.
Bicuspid unidirectional valves keep blood flowing toward the heart.
The valves in the perforators are configured to stop the flow from the deep to the superficial venous network.
Deep veins of the legs
The inferior vena cava system originates from the veins of the fingers, the venous arch of the sole and the dorsum of the foot.
From the venous arch of the dorsum of the foot, blood flows into the deep anterior tibial veins (DATIVs).
From the venous arch of the sole, the posterior tibial veins (PTV) and peroneal veins (MPV) are born.
The deep veins of the leg follow with the artery two, rarely four or more; merge before PKV.
PBBV lie in the anterior muscle bed of the leg; through the interosseous membrane they merge into the BBBV.
The internal and external marginal veins of the sole in the calcaneal canal will form two trunks of the BBBV.
ZBBV on n/3 of the leg immediately behind the muscular fascia, then between the flexors and the triceps muscle.
The MBV arises from the posterolateral calcaneus, superiorly between the MBV and the flexor pollicis longus.
On the third third of the leg, the deep veins merge, thus giving rise to the short trunk of the popliteal vein (PCV).
Drainage of the soleus and gastrocnemius muscles into the soleus and gastrocnemius (sural) veins.
Close to the joint space of the knee joint, the soleus and gastrocnemius veins merge into the PCV.
The SVC lies posterior to the RCA, from its junction with the thigh, called the superficial femoral vein (SFE).
The SMV from its confluence with the deep femoral vein (DFE) is called the common femoral vein (CFV).
The EIVs collect blood from the lower extremities and continue into the external iliac veins (ELVs).
At L5, the iliac vein and internal iliac vein (Iiliac vein) join to form the common iliac vein (CIV).
At L4, the IVCs drain into the inferior vena cava (IVC); The IVC runs to the right of the aorta and has no valves.
Superficial veins of the legs
From the cutaneous venous arch of the dorsum of the foot, the saphenous great and small veins (GSV and SVC) arise.
With a network-like form of the structure, the trunk of the GSV and SSV are distinguished, the tributaries form a network of saphenous veins.
Basin of the great saphenous vein
The GSV ascends anterior to the medial malleolus, along the edge of the BB, posterior to the medial condyle onto the femur.
The GSV lies on the adductors of the thigh, pierces the ethmoidal fascia at the inguinal ligament, and merges into the GSV.
The saphenofemoral anastomosis (SFS) of every person is located strictly in a certain place.
In 90% of cases, the GSV has ostial and preostial valves 0-1.5 and 1.5-8.5 cm below the SPS.
Constant subcutaneous tributaries drain into the GSV close to the SPS; counterclockwise order:
PDPPV, PDPPV, external pudendal, inferior epigastric and circumflex iliac veins.
The superficial fascia splits into two layers and forms the fascial sheath (FF) for the GSV.
The GSV segment from the third thigh to the knee is absent in aplasia; in hypoplasia it narrows to less than 3 mm.
With aplasia of the GSV, a segment of a vein with a three-layer wall, but without a lumen, is found under a microscope.
In hypo- and aplasia, the upper and lower segments of the GSV are connected by a large suprafascial tributary.
Continuing tributaries parallel to the GSV are called accessory great saphenous veins:
- anterior accessory great saphenous vein (AASV),
- superficial accessory great saphenous vein (SASV),
- posterior accessory great saphenous vein (PAGS).
At the top, accessory veins in the FF; The PDBPV merges into the GSV at the SPS, the VDBPV and the ZDPPV - 5-10 cm lower.
The PDBP begins on the outside of the lower leg and behind the knee rises to the anterior surface of the thigh.
The superficial accessory great saphenous vein flows suprafascially strictly over the GSV.
The PVD begins at the back of the knee and rises along the inner thigh, to the middle outside the FF.
On the thigh, the continued tributaries perpendicular to the GSV are called the surrounding thigh veins:
- posterior circumflex femoral vein (PVV),
- anterior circumflex vein (AFV).
A certain number of suprafascial anterior and posterior tributaries merge into the GSV at n/3 of the thigh.
Frequent tributaries of the GSV on the lower leg are the popliteal, posterior arch (PAV) and anterior arch (AV) veins.
The popliteal vein drains the skin and subcutaneous tissue of the area in front of the knee joint.
The VAV originates behind the inner malleolus, rises straight on the shin, and close to the third ventricle merges into the GSV.
The surfactant originates on the outer ankle, rises to the lower leg, and at the border of c/3 and b/3 merges into the GSV.
Each person has many accessory, surrounding hip and arched subcutaneous tributaries.
Basin of the small saphenous vein
The SPV enters the lower leg behind the outer malleolus, and in c/3 it follows between the bellies of the gastrocnemius muscle.
The connection between the SVC and the deep venous system through the saphenoplasteal junction (SPJ) is very diverse.
In 25% of cases, the SVC merges into the PCV at the level of the joint space of the knee, but more often it flows wherever it wants.
In the s/3 tibia, double, triplicate, and quintuple of the MPV in the FF are encountered; twin veins are linked by ligaments.
With hypoplasia of the SVC segment in the third leg of the leg, a large portion of blood drains into any sural vein.
With aplasia of the SSV segment on the third third of the leg, all the blood through the intersaphen peritoneum is directed to the GSV.
The cranial segment of the SVC extends to the top of the popliteal fossa and fuses in a very multivariate manner:
- into the deep veins through the postero-external perforator (Hach);
- in the PVD using the knee-femoral vein (Giacomini);
- in the GSV directly and indirectly through intersaphen pericurrents;
- sometimes cums freely in the subcutaneous fat behind the thigh;
- rarely drains into the sciatic vein under the gluteal fold.
Only the expanded tributaries of the MPV can be discerned; the diverse network is difficult to categorize.
Important duties are performed by the intersaphen veins - transverse periflows connect the SSV and GSV.
Periflow from the SVC into the PAV below the medial malleolus and over the Achilles tendon is common.
The permanent vein on the s/3rd leg from the SSV is directed to drain into the GSV, directly or indirectly through the RAV.
With reflux along the SVC, dilated and varicosely tortuous intersaphen periflows become visible.
Veins perforating the legs
Straight veins perforators move in the intermuscular septa together with the artery and nerve.
The anterior tibial group of perforators in the anterior muscle bed connects the SAV to the PBBV.
The posterior tibial group lies along Linton's line (Cockett's area) and connects the PAV with the PTA.
The paratibial perforator on the verge of the c/3 and c/3 tibia (Sherman) bridges the gap from the PAV to the PCA.
The paratibial vein perforator immediately below the knee (Boyd's) regulates flow from the GSV and SVV.
Direct veins perforate the adductor (Dodd) and adductor canals (Hunter) in the n/3 and s/3 thighs.
The GSV drains into the SPV through the SPS; in rare cases, you can find a perforator 5 cm below the SPS.
The anterior femoral perforators pierce through the quadriceps muscle and merge into the SMV and GBV.
The sciatic vein perforators are located longitudinally along the midline of the posterior thigh.
Four permanent connections of the SVC with the deep veins:
- paraachilles perforators (Bassi) behind the lateral malleolus;
- a perforator vein at a height of 12 cm from the ground connects the SVC with the MBV;
- the peroneal veins that perforate outside the leg are drained into the MBV;
- indirect perforator of the soleus muscle (May) in the s/3 tibia.
Subcutaneous nerves of the legs
During surgery and thermal endovenous procedures, accidental injury to the saphenous nerves is dangerous.
Above the popliteal fossa, the sciatic nerve divides into the common peroneal and tibial nerves.
The OMBN is directed along the biceps femoris muscle and slides distally immediately behind the head of the MBF.
At high SPS, the OMBN is close to the MPV; In case of injury, the extensor muscles - “horse foot” - are paralyzed.
In the popliteal fossa, the BBN, PkA and PkV lie side by side, below the popliteal fossa behind the gastrocnemius muscle.
The medial cutaneous nerve is a branch of the SBN along the SVC; forms the sural nerve with the peroneal branch.
The MCI is responsible for sensation in the back of the distal leg and the outside of the foot.
Take care of yourself, Your Diagnosticer !
Source: https://diagnoster.ru/uzi/lektsii/anatomiya-ven-nk/
Diseases of the arteries of the lower extremities
Arterial diseases include:
- Atherosclerosis. A small amount of cholesterol begins to deposit in the inner lining of the vessel. Gradually, its amount increases and begins to protrude the vessel inward. Blood cells adhere to the formation, which leads to the development of a fairly large blood clot. Provided that the vessel has a smooth surface, the thrombus does not affect the blood flow, but if there is a loose surface, pieces of the thrombus can enter the bloodstream, which has negative consequences. The blockage causes a stroke.
- Endarteritis. The lumen in the vessels is almost completely closed, making blood movement impossible.
- Stenosis. The blood vessels narrowed greatly.
- An aneurysm is an excessive dilation of the arteries.
- Occlusion - the lumen in the vessels is completely closed.
Structure of the venous system
The anatomy of the vascular system has its own characteristic features that distinguish it from other parts of the body.
The femoral artery is the main highway through which blood enters the area of the lower extremities and is a continuation of the iliac artery. Initially, it runs along the anterior surface of the femoral groove. Next, the artery moves to the femoral-popliteal shaft, where it penetrates the area of the popliteal fossa. The largest branch of the femoral artery is the deep artery, through which blood is supplied to the muscle tissue of the thigh and skin.
Read on our website
Human hip - anatomy Each organ, tissue, joint, bone plays its own, very important role in the anatomy of the human body. Violation…
After passing through the femoropopliteal canal, the femoral artery transforms into the popliteal blood vessel, where its branches extend to the knee joint.
In the ankle-popliteal canal, a division occurs into two tibial arteries. The anterior artery of this type passes through the interosseous membrane to the anterior muscles of the leg. Then, going down, it enters the dorsal artery of the foot, which can be felt from the dorsal surface of the ankle. The functions of the anterior tibial artery are to supply blood supply to the anterior group of muscle ligaments of the lower extremities and to the dorsum of the foot, and is also involved in the formation of the plantar arch.
The posterior tibial canal, descending along the popliteal vessel, reaches the medial malleolus and the foot divides into two plantar arteries. The functions of the posterior artery include supplying blood to the posterior and lateral muscle group of the lower leg, the skin and muscle ligaments of the plantar zone.
Next, the blood flow, passing along the back of the foot, begins to rise upward.
The anatomy of the vascular system of the human lower extremities is conventionally divided into superficial and deep subsystems. The greatest load falls on the deep system, which passes through itself up to 90% of the total blood volume. As for the surface, it accounts for no more than 10% of the outgoing flow.
Blood circulation occurs contrary to gravity - from bottom to top. This feature is caused by the ability of the heart to attract flow, and the presence of venous valves does not allow it to go down.
The venous system consists of:
- superficial venous vessels;
- deep venous vessels;
- perforating veins.
Let us consider in more detail the structure and functions of each of the subsystems.
Depending on the structural features and functions performed, all vessels can be divided into arteries, veins and capillaries.
Arteries are hollow tubular formations that carry blood from the heart to peripheral tissues.
Morphologically they consist of three layers:
- external – loose tissue with feeding vessels and nerves;
- medium, made of muscle cells, as well as elastin and collagen fibers;
- internal (intima), which is represented by endothelium, consisting of squamous epithelial cells, and subendothelium (loose connective tissue).
Transport of oxygenated blood
Depending on the structure of the middle layer, medical instructions distinguish three types of arteries.
| Name | Description | Vessels in the body |
| Elastic | The middle layer of such vessels is represented mainly by elastic fibers. They are able to withstand large pressure differences. | |
| Mixed | The number of elastic and muscle fibers in such vessels is approximately the same. |
|
| Muscular | The middle layer is represented mainly by muscle fibers located along the diameter. |
|
Veins are hollow tubes that carry blood from organs and tissues to the heart. They are divided into:
- Muscular - have a myocyte layer. Depending on the degree of its development, there are underdeveloped, moderately developed, and highly developed. The latter are located in the legs.
- Non-muscular - consist of endothelium and loose connective tissue. Found in the musculoskeletal system, somatic organs, and brain.
Vein structure
Arterial and venous vessels have a number of significant differences, presented in the table below.
| Sign | Arteries | Vienna |
| Diameter | Less | More |
| Number of elastic vessels | More | Less |
| Walls | Thicker | Thinner |
| Middle layer | Developed | Not developed |
| Outer layer | Weakly expressed | Strongly expressed |
| Valves | None | Made of venous wall and endothelium. Regulate the movement of blood “from bottom to top” |
The photo shows a schematic representation of the arteriovenous network in the human body.
Arteries of the legs
Blood supply to the legs occurs through the femoral artery. A. femoralis continues the iliac a., which in turn extends from the abdominal aorta. The largest arterial vessel of the lower limb lies in the anterior groove of the thigh, then descends into the popliteal fossa.
Blood supply to the thigh
Femoral a. gives several branches represented by:
- superficial epigastric, rising to the anterior wall of the abdomen almost to the navel;
- 2-3 external genitalia, supplying the scrotum and penis in men or the vulva in women; give off 3-4 thin branches called inguinal;
- superficial circumflex, directed to the upper anterior surface of the ilium;
- deep femoral - the largest branch, starting 3-4 cm below the inguinal ligament.
With atherosclerosis, blood circulation is often impaired at level a. femoralis
The popliteal artery starts from the adductor canal. It has several branches:
- the superior lateral and middle medial branches pass under the knee joint;
- lower lateral – directly in the knee joint;
- middle genicular branch;
- posterior branch of the tibial region.
In the area of the lower leg, popliteal a. continues into two large arterial vessels called tibial (posterior, anterior). Distal from them are the arteries that supply the dorsum and plantar surfaces of the foot.
Blood supply to the leg and foot
Veins of the legs
Veins provide blood flow from the periphery to the heart muscle. They are divided into deep and superficial (subcutaneous).
The deep veins, located in the foot and leg, are double and run next to the arteries. Together they form a single trunk of V. poplitea, located slightly posterior to the popliteal fossa.
The outflow of blood from the NK is carried out through numerous veins
Leriche syndrome
Leriche syndrome is characterized by a chronic ischemic lesion that occurs due to atherosclerosis of the lower extremities of a person. These pathologies have almost the same symptoms. The main difference is that with atherosclerosis, intermittent claudication occurs exclusively in a low position and does not rise above the calf muscle. Leriche syndrome affects almost all limbs, up to the hip.
The main method of diagnosing the disease is considered to be ultrasound of the veins and arteries of the lower extremities, but additional examinations must be performed to make a final diagnosis.
If Leriche syndrome is severe, then surgical intervention is necessary. The indication for surgery is the presence of ischemia of 2B, 3, 4 degrees. In this case, bypass surgery is performed using prostheses in the femoral-popliteal-tabial segment of the lower limb or the greater saphenous femoral vein is directly bypassed. In case of discomfort, it is advisable to do an ultrasound of the veins and arteries of the lower extremities. The conservative method of treating Leriche syndrome does not differ from that used in the presence of atherosclerosis of the legs.
Deep veins
They lie far from the surface of the body, among the bones and muscles. Formed from blood supply elements:
- veins of the foot from the back and sole;
- shins;
- sural;
- knee joints;
- femoral part.
The components of the vascular subcutaneous system undergo duplication of branches and are mutual companions, passing close to the arteries, bending around them.
The deep venous dorsal arch creates the anterior tibial veins, and the plantar arch forms:
- tibial posterior veins;
- receiving peroneal vein.
The deep veins of the leg are divided into 3 paired types of elements - the anterior tibial vein and the posterior one, the SPV and the MSV. Subsequently, they merge together and form the popliteal canal. The peroneal vein and paired knee vessels also flow there, after which the flow of a large element called the “deep femoral vein” begins. If there is occlusion, drainage into the external iliac vein is possible.
Buerger's disease
Buerger's disease is also called obliterating endarteritis. The disease is based on the development of a serious inflammatory process, which occurs with a severe form of ischemia and almost always affects the venous nodes due to the formation of a large number of blood clots.
The exact reasons have not been established, but there are several factors that most provoke the development of such a serious pathology: smoking, frequent hypothermia.
Pathology can occur at a fairly young age. Very often, Buerger's disease occurs in men from 18 to 35 years old. The disease exclusively affects the legs. In this case, the process occurs equally in both limbs. In almost all cases, the patient feels severe pain in the area of the foot and toes. But besides this, there are three more variants of the clinical picture that are more common than usual.
- In the first case, the pain is acute, has a high level of malignancy and occurs mainly at an early age.
- In the second case, the pain is less pronounced and is characterized by a wave-like course. There are remissions, which may have different durations and periods of exacerbation.
- The third case is chronic, and the pain can persist for many years. At the same time, rather slow progress is observed, and remissions differ in their duration.
Common diseases
Vascular diseases of the legs most often develop as a result of the following factors:
- Age. People over thirty-five years of age are prone to diseases.
- Excess weight.
- Smoking.
- Diabetes.
- Stressful situations.
- Increased blood cholesterol.
- Hereditary factor.
Vascular pathologies are as follows:
- varicose veins;
- thrombosis;
- atherosclerosis;
- thrombophlebitis;
- obstruction and blockage of blood vessels;
- endarteritis;
- arteritis;
- diabetic angiopathy.
Atherosclerosis
This disease of the blood vessels of the legs occurs due to the fact that cholesterol is deposited on the walls of the arteries. As blood flow slows down, there is a shortage of oxygen and other nutrients. Soon the lumen is clogged with an atherosclerotic plaque.
Development of atherosclerosis
Symptoms of the disease:
- acute pain in the affected area of the artery;
- bluish tint or pallor of the skin of the lower extremities;
- fatigue;
- reduced performance.
The most vulnerable in this pathology are the popliteal and femoral arteries.
Vascular obstruction
The disease affects the arteries of the lower extremities. Causes may include: increased blood clotting, trauma, embolism and thrombosis.
Also, a pathological condition of obstruction occurs if the vessels in the legs become inflamed.
Symptoms of blocked blood vessels:
- severe pain in the blockage area;
- cramps in the legs;
- reduction and loss of sensitivity;
- limitation of mobility.
Obliterating arteritis
It usually affects the blood vessels of the legs, located in the area of the lower leg and foot. This disease is common in men. Symptoms:
- pain when moving;
- swelling and numbness of the lower extremities;
- changes in the color of the skin of the legs and its dryness.
Endarteritis
This disease has other names: Buerger's disease or smoker's lameness. This is explained by the fact that due to the effects of nicotine, the vascular lumens narrow, and as a result, tissue blood supply decreases. Therefore, mainly smokers are susceptible to pathology.
Symptoms:
- pain when running or walking;
- tired legs;
- lameness;
- pale skin color;
- the appearance of trophic ulcers;
- numbness of the lower extremities;
- tingling in the legs;
- swelling.
Angiopathy
Vessels in the legs can be affected as a result of diabetes. With angiopathy, the tissue integrity of veins and arteries is disrupted. In addition to the fact that the tissue does not receive enough oxygen and nutrients, the disease is complicated by atrophy of the leg muscles.
Symptoms and diagnosis of pathology
The main symptom of Buerger's pathology is considered to be ulcers that appear in the toe area. They are not treated and may become infected over time. This suggests that the arteries located in the area of the foot and lower leg are affected. The pathology begins to spread directly to the femoral artery and popliteal artery.
The main diagnostic methods include the following:
- Blood pressure is measured in the fingers and ankles.
- Then the spectrum in the arteries is determined and the pressure in the arteries at different levels is compared.
- Oxygen tension is determined on the foot and lower leg in different positions using the transcutaneous method.
- Doppler ultrasound is considered mandatory, followed by an additional duplex scan.
- If reconstructive surgery is planned in the future, a procedure such as Seldinger angiography is required.
It is almost impossible to cure Buerger's disease. With the help of surgery and medications, it is only possible to increase the duration of remission and eliminate unpleasant symptoms. To determine the disease, a scan of the veins and arteries of the lower extremities is performed.
Diagnosis and treatment
Needless to say, the importance of timely diagnosis and drug or other intervention for DVT. To make an accurate diagnosis, it is necessary to do an ultrasound or Doppler examination of the femoral vein. Such diagnostics will help determine the exact location of the blood clot and the degree of its fixation to the vessel wall. In other words, to understand whether it can come off and clog a vessel, as well as cause pulmonary embolism or not. Also, when detecting DVT, the method of venography is used - x-ray with a contrast agent. However, the most accurate method today is angiography. On the eve of the procedure, you must observe strict bed rest. Sometimes a puncture of the femoral vein is performed.
Treatment of DVT depends on the cause of the disease and the individual characteristics of the patient. If the vessel is not completely blocked and thrombus rupture is unlikely, then conservative therapy is indicated. It is necessary to restore the patency of the veins, prevent disruption of the integrity of the blood clot and avoid vascular embolism. To achieve the above goals, special medications, ointments, and compression therapy are used, for example, it is recommended to wear special compression stockings.
If the patient is in satisfactory condition, but drug treatment is contraindicated for him, then surgical methods of treating deep thrombosis are used. The operation is carried out using the latest equipment and is high-tech. Thrombectomy is prescribed when the risk of blood clot rupture and blockage of the main vessels cannot be excluded. This plug is removed through a small incision by inserting a special catheter. During the operation, the “clogged” vessel is completely cleared, but relapse cannot be ruled out.
To avoid thrombosis, you need to follow some rules and completely reconsider your lifestyle. It is recommended to give up bad habits, eat right, lead a physically active lifestyle, try to avoid injuries to the lower extremities, etc. We looked at the femoral arteries and veins. Now you know how they differ and what they are.
Anatomy of the venous system
of the lower extremities is highly variable. Knowledge of the individual structural features of the human venous system plays a major role in assessing instrumental examination data in choosing the correct treatment method.
In the venous system of the lower extremities, a deep and superficial network is distinguished.
Deep venous network
represented by paired veins accompanying the arteries of the fingers, foot and leg. The anterior and posterior tibial veins merge in the femoropopliteal canal and form the azygos popliteal vein, which passes into the powerful trunk of the femoral vein (v. femoralis). 5-8 perforating veins and the deep vein of the thigh (v. femoralis profunda), which carries blood from the muscles of the back of the thigh, flow into the femoral vein, even before passing into the external iliac vein (v. iliaca externa). The latter, in addition, has direct anastomoses with the external iliac vein (v. iliaca externa), through intermediary veins. In case of occlusion of the femoral vein, part of the femoral vein may flow through the deep vein system into the external iliac vein (v. iliaca externa).
Superficial venous network
located in the subcutaneous tissue above the superficial fascia. It is represented by two saphenous veins - the great saphenous vein (v. saphena magna) and the small saphenous vein (v. saphena parva).
Great saphenous vein (v. saphena magna)
starts from the internal marginal vein of the foot and along its entire length receives many subcutaneous branches of the superficial network of the thigh and lower leg. In front of the inner ankle, it rises to the lower leg and, going around the back of the inner condyle of the femur, rises to the oval opening in the groin area. At this level it flows into the femoral vein. The great saphenous vein is considered the longest vein in the body, has 5-10 pairs of valves, and its diameter along its entire length ranges from 3 to 5 mm. In some cases, the great saphenous vein of the thigh and leg can be represented by two or even three trunks. 1-8 tributaries flow into the uppermost section of the great saphenous vein, in the groin area; these are often three branches that do not have much practical significance: the external genital (v. pudenda externa super ficialis), superficial epigastric (v. epigastica superficialis) and the superficial vein surrounding the ilium (v. cirkumflexia ilei superficialis).
Small saphenous vein (v. saphena parva)
begins from the external marginal vein of the foot, collecting blood mainly from the sole. Rounding the outer ankle from behind, it rises along the middle of the back surface of the lower leg to the popliteal fossa. Starting from the middle of the leg, the small saphenous vein is located between the layers of the fascia of the leg (N.I. Pirogov’s canal) accompanied by the medial cutaneous nerve of the calf. And therefore, varicose veins of the small saphenous vein are much less common than the large saphenous vein. In 25% of cases, the vein in the popliteal fossa passes through the fascia deep and flows into the popliteal vein. In other cases, the small saphenous vein can rise above the popliteal fossa and flow into the femoral, large saphenous vein, or into the deep vein of the thigh. Therefore, before the operation, the surgeon must know exactly where the small saphenous vein flows into the deep one in order to make a targeted incision directly above the anastomosis. Both saphenous veins widely anastomose with each other by direct and indirect anastomoses and are connected through numerous perforating veins with the deep veins of the leg and thigh. (Fig.1).
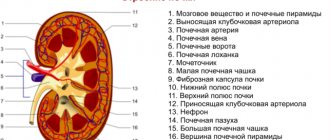
Fig.1. Anatomy of the venous system of the lower extremities
Perforating (communicating) veins (vv. perforantes)
connect deep veins to superficial ones (Fig. 2). Most perforating veins have valves located suprafascially, which allow blood to move from the superficial to the deep veins. There are direct and indirect perforating veins. Direct ones directly connect the main trunks of the superficial and deep veins, indirect ones connect the saphenous veins indirectly, that is, they first flow into the muscular vein, which then flows into the deep vein. Normally they are thin-walled and have a diameter of about 2 mm. If the valves are insufficient, their walls thicken and their diameter increases 2-3 times. Indirect perforating veins predominate. The number of perforating veins on one limb ranges from 20 to 45. In the lower third of the leg, where there are no muscles, direct perforating veins predominate, located along the medial edge of the tibia (Cockett's area). About 50% of the communicating veins of the foot do not have valves, so blood from the foot can flow from deep veins to superficial ones, and vice versa, depending on the functional load and physiological conditions of outflow. In most cases, perforating veins arise from tributaries rather than from the trunk of the great saphenous vein. In 90% of cases, there is incompetence of the perforating veins of the medial surface of the lower third of the leg.
Fig.2. Options for connecting the superficial and deep veins of the lower extremities according to S. Kubik.
1 - skin; 2 - subcutaneous tissue; 3 - superficial fascial leaf; 4 - fibrous bridges; 5 - connective tissue sheath of the saphenous veins; 6 - own fascia of the leg; 7 - saphenous vein; 8 - communicating vein; 9 - direct perforating vein; 10 - indirect perforating vein; 11 - connective tissue sheath of deep vessels; 12 - muscle veins; 13 - deep veins; 14 - deep artery.
The vein is an important component of the human cardiovascular system, performing the function of blood circulation between organs, tissues and the heart.
Veins are divided into superficial (subcutaneous) and deep. The localization of superficial ones is determined directly under the skin, in fatty tissue.
Symptoms of arterial obstruction
Even if one leg is completely healthy, acute obstruction of the arteries can be accompanied by severe spasm in both limbs at once. Symptoms may resemble those that occur during acute ischemia:
- Sharp severe pain.
- The limbs become unnaturally cold.
- The veins begin to collapse.
- Motor activity is impaired, sensitivity almost completely disappears.
- There is a sudden disappearance of the pulse.
If these symptoms appear, it is necessary to do an ultrasound scan of the arteries of the lower extremities. Treatment will be selected depending on the patient's condition. First of all, injections and various kinds of drugs are prescribed. If this is not enough, then surgery is performed.
Arteries
The arteries of the lower extremities are blood vessels through which the blood pumped by the heart is distributed to all organs and parts of the human body, including the lower extremities. Arterial vessels are also represented by arterioles. They have three-layer walls consisting of intima, media and adventitia. They have their own classification characteristics. These vessels have three varieties, which differ from each other in the structure of the middle layer. They are:
- Elastic. The middle layer of these arterial vessels contains elastic fibers that withstand the high blood pressure generated in them when the blood flow is released. They are represented by the aorta and pulmonary trunk.
- Mixed. Here, in the middle layer, different numbers of elastic and myocyte fibers are combined. They are represented by the carotid, subclavian and popliteal arteries.
- Muscular. The middle layer of these arteries consists of individual, circularly located myocyte fibers.
The diagram of arterial vessels according to the location of the internal ones is divided into three types, presented:
- Main, providing blood flow in the lower and upper extremities.
- Organs that supply blood to the internal organs of a person.
- Intraorgan, having their own network, branched throughout all organs.
Arteriovenous fistulas
This disease is considered congenital and most often affects the lower extremities. In this case, fistulas or malformations can also form in internal organs. Pathological changes occur due to venous hypertension and prolonged hypoxia affecting the distal sections. The disease appears already in the first days of the baby’s life. Peripheral circulation is gradually impaired, which makes the limbs practically non-functional. This is considered a direct indication for surgery, which is carried out in several stages. To detect the disease, an ultrasound scan of the vessels (arteries, veins) of the lower extremities is performed.
Superficial veins
They are located immediately under the skin of the lower extremities and include:
- cutaneous veins of the plantar zone and the back of the ankle;
- great saphenous vein (hereinafter GSV);
- small saphenous vein (hereinafter referred to as SSV);
- various branches.
In the foot area, two types of networks are formed by the saphenous veins. The first is the venous plantar subsystem and the second is the venous subsystem of the dorsum of the foot. The dorsal arch is formed by the fusion of the common dorsal digital veins from the second subsystem. Its ends form a pair of longitudinal marginal trunks: medial and lateral. On the plantar zone there is a plantar arch, which connects with the marginal veins and through the intercapitate veins with the dorsal arch.
Read on our website
Causes of varicose veins Varicose veins are a progressive disease of the subcutaneous and deep veins, which cease to be elastic. Because of this…
The GSV is a continuation of the medial trunk, gradually passing to the tibia and then to the medial region of the tibia. Curving around the surface of the medial condyles behind the knee joint, it ends up on the inner side of the femoral area of the lower extremities.
The GSV is the longest venous vessel in the body, having up to 10 valves.
In normal condition, its diameter is about 3-5 mm. Along the entire path, many branches and up to 8 large venous trunks flow into it. It receives the epigastric, external pudendal, and superficial blood canals from the ilium. As for the epigastric vein, it is the one that should be ligated during surgery.
The origin of the small saphenous vein is the external marginal vessel of the foot. Moving to the top, the SPV through the lateral malleolus is first on the edge of the calcaneal (Achilles) tendon ligament and then on the middle straight dorsum of the leg. Further, the MPV can be seen as one trunk or, in rare cases, two. In the upper zone of the leg it passes through the fascia and reaches the popliteal fossa, after which it flows into the popliteal venous trunk.
Varicose veins
Varicose veins in the lower extremities are divided into two types. Primary occurs due to hereditary failure of the venous valves or due to congenital weakness of connective tissue. Secondary varicose veins become a consequence of diseases that a person previously suffered. It is very easy to notice the presence of varicose veins by external signs. In addition, other symptoms appear: heaviness in the lower extremities, pigmentation appears, and a complication such as thrombophlebitis may occur. The ultrasound method is used as diagnostics. Treatment can be very different. Most often, hirudotherapy, wearing compression hosiery, venotonics are used, a diet and regimen are followed, and special exercises are performed. As a supplement, you can use traditional medicine recipes. In especially severe cases, sclerotherapy or surgery is prescribed.
How many veins are there in a person's leg?
The anatomy of the veins of the lower extremities has general principles of construction and an approximate layout, but its peculiarity is in the presence of variability and variability. Each individual's venous network is unique. It is important to understand its structure in order to avoid the development of diseases in this area, the most common of which is varicose veins.
Supplying blood flow to the venous system of the legs
Along the bed of the femoral artery, which serves as a continuation of the iliac artery, blood enters the legs. When entering the limb zone, the channel runs along the frontal plane of the femoral groove. After which it is directed to the femoral-popliteal shaft, in which it goes into the popliteal fossa.
The deep artery is the largest branch of the femoral artery. Its main function is to supply nutrients to the subcutaneous muscles and epidermis of the thigh.
After the shaft, the main vessel turns into the popliteal and diverges in a network to the area of the corresponding joint.
Two tibial conductive streams are formed in the ankle-popliteal canal:
- The anterior one passes through the interosseous film and goes to the muscles of the lower leg, then falls to the dorsal vessels of the foot. They can be easily felt on the back of the subcutaneous part of the ankle. The function is to nourish the frontal cluster of ligaments and muscles of the leg and dorsum of the foot, to create the shape of the plantar arch.
- The posterior one makes its way along the popliteal vessel to the medial surface of the ankle, in the area of the foot it divides into two processes. Its blood supply affects the posterior and lateral muscles of the lower leg, the skin and ligaments in the area of the sole.
Having circled the foot from the back, the blood flow begins to move upward and flows into the femoral vein, which supplies the entire length of the limbs (thighs and legs).
Functions of veins in the legs
The structure of the venous system of the lower extremities by the network of vessels under the upper integuments is focused on performing the following functionality:
- The removal of blood filled with carbon dioxide molecules and waste products from cellular structures.
- Supply of hormonal regulators and organic compounds from the gastrointestinal tract.
- Monitoring the functioning of all circulatory processes.
The structure of the venous wall
The common femoral vein and other vascular structures in the legs have a specific design, which is explained by the principles of location and function. Under normal conditions, the channel looks like a tube with stretching walls that are deformable within limited limits.
The stem frame, consisting of collagen and reticulin fibers, provides containment. They themselves are capable of stretching, so they not only form the necessary properties, but also retain their shape during pressure surges.
Looking at the wall, three structural layers can be distinguished:
- Adventitia. The outer part develops into a stretchy outer membrane. Dense, formed from longitudinal muscle threads and collagen protein fibers.
- Media. The central element has an inner shell. The smooth muscles that form it are arranged in a spiral pattern.
- Intimacy. The deepest layer is the layer lining the cavity of the vessel.
The smooth muscle layer in the leg veins is denser than in other parts of the human body, which is determined by their location. Lying in the subcutaneous tissue, the vessels constantly overcome pressure, which negatively affects the integrity of the structure.
Structure and purpose of the valve system
It occupies a significant position in the anatomical map of the circulatory system of the lower extremities, as it forms a correctly directed fluid flow.
At the bottom of the limbs there are valves in maximum concentration, which occur at intervals of 8-10 cm.
The formations themselves are bicuspid growths of connective tissue cells. Consist of:
- valve flaps;
- rollers;
- adjacent parts of the venous walls.
The strength of the elements allows them to withstand loads of up to 300 mmHg, but over the years their concentration in the vascular system decreases.
The valves work like this:
- A wave of moving liquid falls on the formation, and its doors close.
- A neural notification of this is sent to the muscular sphincter, according to which the latter expands to the required dimensions.
- The edges of the element are straightened, and it can provide complete blocking of the blood flow.
Great saphenous and small veins
The medial vein, located on the inner edge of the dorsum of the foot, where the great saphenous vein of the leg (in Latin - v. saphena magna) originates, passes from the medial malleolus to the area of the anterior inner part of the leg, then higher along the thigh leading to the ligament in the groin.
In the upper third of the femoral region, the lateral branch of vessels branches off from the BMW. It is called the “anterior accessory saphenous vein” and plays a role in the recurrence of varicose veins after surgery in the area of the great saphenous vein of the thigh.
The point of confluence of the above two elements is called the saphenofemoral anastomosis. You can feel it on the body a little lower from the inguinal ligament and inward from the palpably pulsating femoral artery.
The beginning of the small saphenous vein of the leg - saphena parva - is located on the outer edge of the dorsum of the foot, which is why this area is called the marginal lateral vein.
It lifts up the shin from the lateral part of the ankle, between the heads of the calf muscles, reaching the pits under the knees. Up to the second third of the leg, the flow of the SVC is superficial and even, then displacement occurs under the fascia.
There, after the fossa, the vessel flows into the popliteal vein, this place is the sapheno-popliteal anastomosis.
Under the influence of varicose veins, a certain area of this subcutaneous vessel, which is located superficially, close to the skin, is deformed.
The exact location of the confluence of the MPV varies significantly in individual variants. There are situations when it doesn’t flow anywhere at all.
It can be connected to the GSV by an indirect suprafascial vein.
Superficial veins
They lie shallow in the body, located almost under the skin itself. This type includes:
- Plantar venous vessels supplying the dermis and inner area of the ankle joint.
- Greater and lesser saphenous veins.
- Superficial femoral vein.
- Many processes and branches of large elements of the system.
Diseases affecting this area of the venous blood supply in the lower extremities are mainly formed due to significant deformation of the components. The lack of strength and elasticity of the structure makes it difficult to resist the negative effects of external effects and high pressure due to the internal pressure of liquids.
The saphenous veins, located in the lower third of the legs, are divided into two types of networks:
- Plantar.
- Dorsal foot subsystem. The common digital veins belonging to it unite in the posterior part and create the dorsal arch. The ends of the formation form the medial and lateral trunks.
On the plantar side lies an arch of the same name, communicating with the marginal veins and the dorsal circle, involving the intercapitate veins.
Deep veins
They lie far from the surface of the body, among the bones and muscles. Formed from blood supply elements:
- veins of the foot from the back and sole;
- shins;
- sural;
- knee joints;
- femoral part.
The components of the vascular subcutaneous system undergo duplication of branches and are mutual companions, passing close to the arteries, bending around them.
The deep venous dorsal arch creates the anterior tibial veins, and the plantar arch forms:
- tibial posterior veins;
- receiving peroneal vein.
The deep veins of the leg are divided into 3 paired types of elements - the anterior tibial vein and the posterior one, the SPV and the MSV. Subsequently, they merge together and form the popliteal canal.
The peroneal vein and paired knee vessels also flow there, after which the flow of a large element called the “deep femoral vein” begins.
If there is occlusion, drainage into the external iliac vein is possible.
Source: https://BoliGolovnie.ru/varikoz/skolko-ven-v-noge-u-cheloveka.html
Thrombosis, phlebitis
The acute form of venous thrombosis occurs due to the fact that:
- A blood clot forms, which is characteristic of hypercoagulation.
- The walls of blood vessels change due to the effects of injury and inflammation.
- There is a disturbance in the outflow of blood due to a decrease in the speed of blood flow.
Thrombosis can affect any vein. As numerous practice shows, most often the pathology occurs after a myocardial infarction or stroke. As a complication, thrombophlebitis and pulmonary embolism may develop. As a rule, thrombosis has virtually no effect on the general condition of the patient. The main symptoms are swelling, pain, and hyperemia in the affected area. If severe thrombosis is present, arterial spasm may occur. In this case, cyanosis can be added to the symptoms.
Prevention of vascular diseases of the lower extremities
In order not to endure constant pain in the legs and not to spend a lot of time and money on treatment, it is worth taking simple preventive measures. With their help, you can avoid many diseases or make their course easier. The main tips include the following:
- Avoid stagnation or thickening of the blood. Very sudden temperature changes are dangerous.
- Avoid wearing clothes that are too tight. This causes blood circulation to begin to deteriorate.
- Follow a special, non-strict diet. Eliminate all foods with cholesterol from your diet. Try to eat as many fruits and vegetables and seafood as possible.
- Pay attention to physical education. Take up some kind of sport that you like, or at least walk more often.
- Get tested to check your hormones. If you find any violations, get rid of the problem. If you are taking hormonal contraceptives, it is better to avoid them.
- Get rid of bad habits. They are the cause of the development of many diseases of the arteries and veins of the lower extremities.
- In order to make the blood more liquid, you can drink cinquefoil tea, eat more citrus fruits, berries, dark chocolate, and sometimes aspirin is prescribed.
- To increase the elasticity of the walls of blood vessels, parsley, honey, apricots, fish, honey will be useful.
With the help of such prevention, the risk of developing pathologies of arteries and veins located in the lower extremities can be minimized. If your body is predisposed to vascular diseases, it is recommended to perform Doppler ultrasound of the veins and arteries of the lower extremities.
Anatomy of the veins of the lower extremities: deep, saphenous and superficial veins
The location of the veins of the lower extremities (abbreviated VNK) in the body is farthest from the heart, which affects their functionality and anatomical structure. They experience the greatest stress and are more likely than others to undergo pathological changes.
If we compare the anatomy of the veins of the lower extremities with the structure of the circulatory network in other parts of the body, it turns out that they are characterized by a greater number of anastomoses and valves, as well as an almost complete absence of muscle tissue in the medial layer.
These features are far from the only reason why especially close attention is paid to the group of vessels of the lower extremities.
Functions of the leg veins
The veins of the legs have a difficult task - without contractility, they must deliver a mass of blood from the most distant parts of the body to the heart. This is what predetermined the structure of the network, divided into superficial and deep vessels, connected by a network of perforating ducts.
Their walls consist of three layers:
- Intima is the inner layer of endothelium, separated from the middle layer by a thin membrane.
- The medial layer is the middle “layer” of the tube, represented by elastic fibers and a small proportion of muscle fibers. It is this layer that gives them strength and stretchability.
- The outer layer, consisting of connective tissue bordering the membrane that separates the blood tubes from the muscle tissue.
Despite the fact that in the lower extremities the drainage network is represented by tubes of different diameters (from 1.5 to 11 mm), the anatomy of the veins is almost the same. The only difference is the thickness of each layer and the number of valves.
For example, the veins of the lower leg have more valves, but their diameter is 2 times smaller than that of the great saphenous vein.
In addition to blood pressure, superficial vessels experience significant stress due to external influences, so the thickness of their middle layer is much greater than that of deep-lying tubes.
For example, the walls of the great saphenous vein are 1.3 times thicker and stronger than those of the deep vein.
The main functions of the VNK are:
- Ensuring uninterrupted outflow of blood, in which carbon dioxide and waste products of tissues located within their reach are dissolved.
- Delivery to tissues of hormones, organic compounds (enzymes, amino acids, proteins), vitamins and microelements coming from the intestines.
- Regulation of general blood pressure.
It is the variety of tasks assigned to the VNK that has led to close attention to the condition of the blood vessels. Any deviation in their functionality can cause irreparable harm to health.
Superficial veins of the lower extremities
Superficial VNK are responsible for draining blood from the toes and metatarsal part of the foot, therefore the localization of the superficial veins of the lower extremities is limited to the foot and ankle. The list of blood vessels located along the upper (front) part of the leg includes:
- dorsal digital vessels;
- dorsal arch of the foot;
- medial marginal tube;
- lateral marginal tube.
On the one hand, the superficial VNCs border with the venules of the toes and feet, and on the other, they connect with the large and small saphenous ducts.
On the underside of the foot, the superficial network is represented by plantar digital ducts flowing into the plantar arch. The vessels then connect to the medial and lateral plantar tubes, which empty into the posterior tibial tube.
The diameter of this group of blood ducts ranges from 1.5 to 3 mm.
Due to their short length, they have fewer valves, but the walls are quite dense and elastic due to the large number of reticular and collagen fibers, as well as spirally arranged muscle cells.
Superficial VNK are clearly visible under the thin skin of the feet, which is practically devoid of subcutaneous tissue. They look like bluish tracks, and with heavy stress on the legs they can swell and become bulging.
Deep veins of the lower extremities
Localization of the deep veins of the lower extremities (abbreviated as DVNK) is the thickness of the muscles along the entire length of the legs and thighs. The GVNK include:
- femoral;
- anterior tibial;
- posterior tibial;
- fibula;
- popliteal
The deep ducts are located near the arteries of the same name, and are connected to the superficial ones by a network of perforating vessels. Their walls are highly elastic and resilient. There are numerous valves along the entire length. The thickness of the GVNK ranges from 3 to 10 mm.
In the lower part of the bed, metatarsal vessels flow into the GVNK, from where blood flows through the tibial anterior vein into the popliteal vein.
Next, the deep vein of the thigh, which flows into the iliac vessel located in the groin area, is responsible for the drainage of blood. It contains up to 5 valves that support fluid flow in one direction.
Part of the blood is “dumped” through a network of perforating tubes into the superficial channels.
The deep-lying network at the level of the lower leg runs virtually parallel to the arterial network, and in the thigh area they are located at a distance from each other.
Saphenous veins
The network of drainage vessels located directly under the skin is represented by the small and large saphenous veins.
The origin of the small saphenous vein (abbreviated SSV) is the lateral marginal vein located on the foot, as well as the plexus of vessels of the lateral part of the foot and heel.
The localization of this blood tube is limited to the two heads of the gastrocnemius muscle, and in the upper part it passes through the popliteal fossa, where it connects with the popliteal vein.
A special feature of the MPC is the presence of a large number of valves, thanks to which the active movement of blood upwards is maintained. It has many tributaries in the form of superficial veins at the back of the leg. In addition, it is connected to the lower leg by numerous anastomoses. Its diameter does not exceed 4.5 mm.
The origin of the great saphenous vein (abbreviated as GSV) is the medial part of the ankle, along which it runs up along the leg and rises first behind the epicondyle of the femur, and then along the premedial surface of the thigh to the ethmoidal fascia, where it drains into the femoral vein.
Its tributaries are numerous preantemedial veins, entwining the entire surface of the thigh and lower leg, epigastric and superficial vessels surrounding the ilium. In addition, shortly before entering the femoral vein, the venous ducts of the external genitalia join it.
The peculiarity of BOD is its large diameter (up to 11 mm) and the presence of a developed valve system.
Diseases
The most common pathologies of the veins of the lower extremities are considered to be changes in their anatomy, mainly varicose veins. The following may contribute to their appearance:
- excess weight and increased load on the limbs;
- genetically inherited weakness of the vascular walls;
- lack of physical activity;
- prolonged static loads on the legs.
Varicose veins are always based on insufficiency of the valve system of the veins, in which part of the blood remains in the lower parts of the bed, creating additional pressure and leading to stretching of the walls of the tube.
The subcutaneous vessels are most often affected by it, since they are affected not only by internal, but also by external factors.
Sometimes varicose veins are found in deep veins, and their causes are mainly genetic abnormalities and increased stress (lifting and carrying heavy objects, childbirth, etc.).
Another problem that affects the venous plexuses of the lower extremities is thrombosis and thrombophlebitis. These diseases are caused by stagnation and gradual increase in blood density. Thrombosis can be observed in the PVNK and GVNK.
Blood clots in a network of vessels located on the surface are accompanied by chronic symptoms, but are easily identified and do not pose a threat to life.
Deep thrombosis is dangerous because it has a less pronounced course, but it can be complicated by the penetration of a blood clot into vital organs: lungs, heart, brain.
Doctors call adherence to the principles of a healthy lifestyle a measure to prevent varicose veins and thrombophlebitis: proper nutrition, maintaining normal body weight, moderate physical activity. If you experience increased fatigue in your legs, dull or sharp pain in the muscles of the lower extremities, a feeling of numbness, or a change in skin color, you should consult a phlebologist.
Source: https://bloodvessel.ru/krovenosnaya-sistema-cheloveka/veny-nizhnih-konechnostej