Structure of the heart.
The heart is a hollow muscular organ divided into four chambers (color table XI).
The widened upper part of the heart is called the base,
and the narrowed lower part is called
the apex.
The mass of the human heart is from 250 to 360 g (the size of a fist).
the coronary groove runs transversely
lying on the border between the atria and ventricles.
The coronary arteries
are located here .
The heart is located behind the sternum, in the lower part of the anterior mediastinum; two-thirds of it is to the left of the midline of the body, and one-third is to the right. The length of the heart is 12-13 cm, diameter 9-10.5 cm, anteroposterior diameter 6-7 cm.
Children's hearts are relatively larger than adults'. The heart grows unevenly. It grows especially intensively in the first year of life and partly in the second, as well as at 14-15 years of age.
The heart is placed in the pericardial sac,
or
pericardium.
The pericardium consists of two layers.
The internal layer - the epicardium
- tightly fuses with the heart muscle, and the parietal leaf, together with the surrounding layer of connective tissue, forms the cardiac sac, or pericardial sac. Between the two layers of the pericardium there is a closed cavity. It contains a small amount of serous fluid that protects the heart from friction during contractions.
Rice. 55.
Bicuspid heart valve:
1 - outer shell of the heart; 2 - muscular wall of the heart; 3 - inner lining of the heart; 4 - bicuspid valve; 6 - papillary muscle; 5 - tendon threads.
The heart lies askew. Its base is directed back, up and to the right, and its top is directed down, forward and to the left. The apex of the heart is adjacent to the anterior chest wall in the region of the fifth left intercostal space; here, at the moment of contraction of the ventricles, a cardiac impulse is felt.
The bulk of the heart wall is made up of a powerful muscle - the myocardium,
formed by 2-3 layers of muscle tissue.
The heart muscle is special. It consists of muscle fibers, the myofibrils in which are located throughout the fiber with some predominance at the periphery and are capable of rapid contractions. Under a microscope, the fibers have transverse striations. Unlike skeletal muscles, the muscle fibers of the cardiac muscle have adhesion lines,
or
anastomoses,
with the help of which they are connected to each other into a single complex network with slit-like loops. The muscle fibers of the heart and the bridges connecting them are rich in sarcoplasm. The thickness of the myocardium varies in different parts of the heart. It is thinnest in the atria (2-3 mm), the left ventricle has the most powerful muscular wall, it is 2.5 times thicker than in the right ventricle.
The atrial myocardium is isolated from the ventricular myocardium, which makes it possible for them to contract separately.
From the inside, the cavity of the heart is lined with an inner membrane - the endocardium,
forming the valve apparatus of the heart.
Work of the heart
One of the distinctive features of the heart muscle is the abundance of mitochondria in its cells, which is associated with the intensive metabolic processes occurring here. As a result of metabolism, the energy necessary for the functioning of the heart is released. The heart spends from 7 to 20% of all energy that is released in the body.
The job of the heart is to pump blood. The heart, which makes up about 0.5% of a person’s body weight (approximately 300 g), pumps about 7,000 liters of blood per day. The daily work of the heart is more than 17,000 kgf•m (1 kgf•m≈9.8 J). Such an effort is necessary to lift a railway freight car to a height of 1 m. Such a high performance of the heart is explained not only by the high level of metabolic processes occurring in it, but also by the rhythmic activity, strict alternation of work and rest of each of its departments. In addition, the heart is intensively supplied with blood.
The heart muscle receives blood through the coronaries,
or
coronary
arteries. The coronary arteries originate from the mouth of the aorta. There are left and right coronary arteries. With each contraction of the heart, approximately 10% of all blood entering the aorta passes into the coronary arteries.
Depending on the work of the heart, its blood supply also changes. The heart of a healthy person in a calm state requires 250-300 cm3 of blood every minute for normal functioning. During heavy physical work, about 2000 cm3 of blood is delivered to the heart through the same coronary vessels.
The heart is the central organ of the circulatory system. Its pumping function is associated with myocardial contractions, alternating contractions of the atria and ventricles and reliable operation of the heart valves.
Why does rhythm disturbance occur?
The cause of extrasystole is a violation of the excitability of the heart. Extrasystole accompanies many diseases, such as myocarditis, ischemic heart disease, cardiosclerosis, rheumatism, heart defects and other diseases. But in half the cases it is not connected with them in any way. Other reasons:
reflex effects from internal organs (for cholecystitis, diseases of the genital organs, stomach); overdose of cardiac glycosides, abuse of diuretics, antiarrhythmic drugs; imbalance of electrolytes sodium, potassium, magnesium; consumption of stimulants - large amounts of coffee, alcohol, energy drinks; high physical activity; neuroses, psychoneuroses, labile cardiovascular system; endocrine diseases – thyrotoxicosis, hypothyroidism; chronic infections.
The causes of supraventricular extrasystole, as one of the supraventricular arrhythmias, are the same as those listed above.
Extrasystole with osteochondrosis has recently become a common occurrence. Its appearance is associated with degenerative-dystrophic changes in the thoracic spine. The nerve roots and plexuses located in this area can be pinched and disrupt the innervation of the heart and other organs.
Extrasystole during pregnancy occurs in half of expectant mothers 2–3 months before birth. During this period, the woman’s body experiences the highest stress. Treatment of cardiac extrasystole in pregnant women is impossible without finding out the cause, and they can be different. And the treatment should not have a negative effect on the fetus. Therefore, immediately see a cardiologist.
How to restore heart rhythm
How to treat extrasystole, and by what means? You need to start by going to the doctor. First you need to get examined. Identify and, if possible, eliminate the factors causing arrhythmia.
Antiarrhythmic drugs for extrasystole are the main stage of treatment. They are selected individually. The same remedy may help one patient, but simply will not work for another. Single rare extrasystoles not associated with heart disease do not need to be treated. Patients with early polytopic extrasystoles are hospitalized.
For ventricular extrasystoles, novocainamide, lidocaine, diphenine, and ethmozine are indicated. Supraventricular extrasystole is treated using verapamil, quinidine, propranolone and its analogues - obsidan, anaprilin, inderal. Cardarone and disopyramide are active in both types of arrhythmia.
If the rhythm is disturbed due to bradycardia, treatment of extrasystole is carried out with belladonna preparations, atropine and alupent are used. Beta blockers are contraindicated in this case. In case of overdose or poisoning with cardiac glycosides, potassium preparations are used.
Rhythm disturbances caused by psycho-emotional stress can be controlled with sedatives. This extrasystole is treated with folk remedies - infusions and decoctions of herbs. But they must be used correctly; self-medication is also unacceptable. Blood-red hawthorn, motherwort, valerian officinalis, calendula, and blue cyanosis have a good effect.
If the cause of the arrhythmia is discovered, effective drugs are selected for the treatment of cardiac arrhythmias, the extrasystole will certainly recede. You may have to sacrifice something, for example, change your usual lifestyle.
Video about exercises for osteochondrosis and extrasystole:
Extrasystole is a common form of heart rhythm pathology, caused by the appearance of single or multiple extraordinary contractions of the entire heart or its individual chambers.
According to the results of Holter ECG monitoring, extrasystoles are recorded in approximately 90% of examined patients over 50–55 years of age, both in those suffering from heart disease and in relatively healthy ones. In the latter, “extra” heartbeats are not dangerous to health, but in people with severe heart pathologies they can lead to serious consequences in the form of deterioration of the condition, relapse of the disease, and the development of complications.
Heart sounds
The heart makes characteristic sounds similar to a knock. Each beat consists of two main tones. The first is the result of contraction of the ventricles, or, more precisely, the slamming of valves, which, when the myocardium is tense, close the atrioventricular openings so that blood cannot return to the atria. A characteristic sound is produced when their free edges close. In addition to the valves, the myocardium, the walls of the pulmonary trunk and aorta, and tendon threads take part in creating the shock.
The second sound is formed during ventricular diastole. This is the result of the semilunar valves, which prevent blood from flowing back, blocking its path. A knock is heard when they connect in the lumen of the vessels with their edges.
In addition to the main tones, there are two more - the third and fourth. The first two can be heard using a phonendoscope, while the other two can only be recorded by a special device.
Cardiac cycle
The human heart works like a pump. Due to the properties of the myocardium (excitability, ability to contract, conductivity, automaticity), it is able to pump blood into the arteries, which enters it from the veins. It moves without stopping due to the fact that a pressure difference is formed at the ends of the vascular system (arterial and venous) (0 mmHg in the main veins and 140 mmHg in the aorta).
The work of the heart consists of cardiac cycles - continuously alternating periods of contraction and relaxation, which are called systole and diastole, respectively.
Heart functions
Human blood supplies the entire body with oxygen and useful elements. The biological fluid also has a cleansing function, helping to eliminate metabolic waste. The function of the heart is to pump blood through blood vessels in humans.
On a note! The organ pumps 7-10 thousand liters of blood per day. This is approximately 3 million liters per year. It turns out up to 200 million liters during the period of life!
The amount of blood pumped in 60 seconds. depends on the current load on the body physically and emotionally. The higher it is, the more blood the human body needs. So the organ can pump 5-30 liters through itself in 60 seconds. The blood flow system consists of approximately 65,000 vessels, their total length is about 10,000 km. Yes, the number is amazing.
Forecast for advanced forms of extrasystole
The prognosis for heart damage in the form of extrasystole depends on the type and severity of the disease.
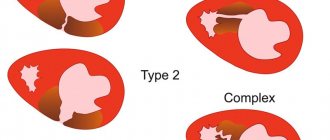
All extrasystoles are formed either in the ventricles or in the atria. But there is also a mixture of them; such extrasystoles are usually called atrioventricular extrasystoles.
Extrasystoles formed in the atria or atrial septum are called supraventricular extrasystoles.
The prognosis for this form of the disease is favorable; early identification and elimination of the cause allows the body to recover in a short time.
Unfortunately, ventricular extrasystole is the most common. This disease has the most malignant course, in contrast to the supraventricular form, and only single ventricular extrasystoles are not dangerous. They are recorded using an ECG in isolated cases.
All other types of ventricular extrasystoles cause persistent circulatory disorders, leading to flutter and the development of ventricular fibrillation - a fatal condition.
Modern diagnosis of extrasystole
The basis of modern diagnostics is a high-quality medical history (questioning the patient about his complaints) and an electrocardiogram of the heart. Important criteria when questioning the patient:
Emotional state, Relationship between the frequency of extrasystoles and medication intake, and the presence of chronic diseases, especially such as: Hypertension, VSD, Common osteochondrosis.
High-quality listening to heart sounds allows you to determine the type and classify the arrhythmia according to the danger to the patient’s life.
Another significant type of arrhythmia diagnosis is Holter ECG monitoring. The method of taking an electrocardiogram is undoubtedly good, but it also has its drawbacks. In some cases, it does not provide a complete informative picture, but daily monitoring of the electrocardiogram using a small Holter device allows you to view the cardiogram both in wakefulness and physical rest.
Diagnosis of extrasystole
The presence of extrasystoles can be suspected after collecting patient complaints and a physical examination. Here it is necessary to find out whether a person constantly or periodically feels interruptions in the functioning of the heart, the time of their occurrence (during sleep, in the morning, etc.), the circumstances that provoke extrasystoles (anxiety, physical activity or, conversely, a state of rest).
When collecting anamnesis, it is important to note whether the patient has heart and vascular diseases or previous diseases that cause complications on the heart. All this information makes it possible to preliminarily determine the shape of the extrasystoles, the frequency, the time of occurrence of unscheduled “beats,” as well as the sequence of extrasystoles relative to normal heart contractions.
Laboratory research:
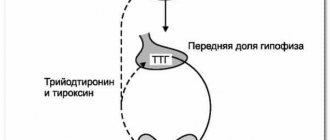
Clinical and biochemical blood tests. Analysis with calculation of thyroid hormone levels.
Based on the results of laboratory diagnostics, it is possible to identify an extracardiac (not related to cardiac pathology) cause of extrasystole.
Instrumental studies:
Electrocardiography (ECG) is a non-invasive method of studying the heart, which consists of graphically reproducing the recorded bioelectric potentials of the organ using several cutaneous electrodes. By studying the electrocardiographic curve, one can understand the nature of extrasystoles, frequency, etc. Due to the fact that extrasystoles can only occur during exercise, an ECG performed at rest will not record them in all cases. Holter monitoring, or 24-hour ECG monitoring , is a heart study that allows, thanks to a portable device, to record an ECG throughout the day. The advantage of this technique is that the electrocardiographic waveform is recorded and stored in the device's memory during the patient's daily physical activity. During the daily examination, the patient makes a list of recorded time periods of physical activity (climbing stairs, walking), as well as the time of taking medications and the appearance of pain or other sensations in the heart area. To detect extrasystoles, full-scale Holter monitoring is more often used, carried out continuously for 1–3 days, but generally no more than 24 hours. Another type - fragmentary - is prescribed for recording irregular and rare extrasystoles. The study is carried out either continuously or intermittently for a longer period of time than full-scale monitoring. Bicycle ergometry is a diagnostic method that consists of recording ECG and blood pressure indicators against the background of constantly increasing physical activity (the subject pedals the bicycle ergometer at different speeds) and after its completion. Treadmill test is a functional load test, consisting of recording blood pressure and ECG while walking on a treadmill.
The last two studies help to identify extrasystole that occurs only during active physical activity, which may not be detected with a regular ECG and Holter monitoring.
To diagnose concomitant cardiac pathology, standard echocardiography (Echo CG) and transesophageal, as well as MRI or stress Echo CG are performed.
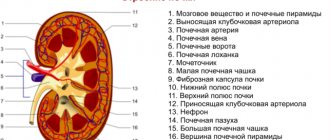
Biophysical view of the structure of the heart
Scheme of the spatiotemporal organization of normal functioning of the human heart. Green inscriptions and arrows indicate the time of arrival of the excitation wave in a given area of the heart. The blue insets show the shape of the profile of the traveling wave (the so-called “action potential”) in different regions of the heart, due to the difference in the properties of the elements of the excitable medium that the heart tissue forms. Beige inset - normal propagation of a traveling excitation wave from the pacemaker zone in the center (sinus node) towards the edges (along the working myocardium) in the simplest simulation mathematical model.
From the point of view of cardiac physics, the heart is a multicomponent polymer heterogeneous active medium of natural origin. The fine organization of the structure of this environment ensures its basic biological functions.
The heterogeneous structure of the heart, which underlies its fine organization, has been repeatedly confirmed, first using electrophysiological methods and then using computational biology methods (see figure).
The autowave properties of cardiac tissue have been actively studied by both Russian and world science for more than half a century.
A new scientific look at this biological object allows us to take a new approach to solving the problem of creating an artificial heart: the task comes down to establishing the production of an artificial polymer active medium with a similar autowave function based on modern nanotechnology.