Causes
Unfortunately, scientists still cannot say with certainty what exactly affects healthy cells so that they begin to degenerate into cancerous ones. But they identified a number of phenomena, the influence of which negatively affects the condition of tissues and can contribute to their pathological changes.
These factors include:
- Light skin color.
- Elderly age.
- Damage to the epidermis.
- Negative effects on the skin of the sun's rays.
- Contact with poisons and chemicals.
- Weakened immunity.
By eliminating these factors from your life, you can prevent the development of cancer.
Reasons for the development of pathology
Squamous cell skin cancer often occurs against the background of precancerous diseases, which increase the risk of malignancy of damaged cells:
- Keratosis.
- Actinic cheilitis.
- Leukoplakia.
- Xeroderma pigmentosum.
- Bowen's disease.
- Paget's disease.
- Cutaneous horn.
- Contact dermatitis.
- Papillomatosis.
The risk of developing cancer is higher if, in addition to precancerous conditions, there are external and internal factors that can accelerate the process of malignancy.
Main factors of the disease
It is customary to identify the main negative factors that increase the risk of developing skin cancer:
- prolonged exposure to sunlight;
- frequent visits to the solarium;
- exposure to ionizing radiation;
- thermal and chemical burns, frostbite;
- regular injury to the skin;
- occupational factors (contacts with carcinogenic substances);
- long-term use of immunosuppressants;
- immunodeficiency diseases.
Sometimes squamous cell skin cancer develops in healthy areas of the body that have no external damage. In this case, doctors are inclined to believe that the development of an oncological tumor is a consequence of a hereditary predisposition causing genetic mutations.
Symptoms
Squamous cell carcinoma of the facial skin manifests itself poorly at an early stage, so people do not pay attention. This interferes with timely diagnosis and treatment of the disease. The first symptom of squamous cell skin cancer is the appearance of a lump with a yellow tint.
The growth is dense to the touch and may protrude slightly above the surface of the cover. Over time, an obvious tumor forms, which tends to grow rapidly and causes pain when touched.
Morphological features of the tumor
Squamous cell carcinoma of the uterus is heterogeneous. There are several histological types of tumor, the identification of which significantly affects the prospects for complete recovery. In addition to the generally accepted stages from the first to the fourth, the following morphological variants of the disease are distinguished:
- intraepithelial;
- invasive;
- keratinized;
- highly differentiated;
- with a tendency to keratinization;
- moderately differentiated;
- non-keratinizing;
- low differentiated.
Intraepithelial squamous cell carcinoma of the cervix is the most favorable histological type of the disease. It means that the malignant neoplasm is localized exclusively by epithelial cells, without growing into other layers of the mucous membrane. Typically, such a tumor corresponds to the very initial manifestations of the disease and can be completely cured. A type of intraepithelial cancer is the “in situ” process. This is the earliest stage of the disease, which does not even require radical mutilation. Unfortunately, the detection rate of such cancer is negligible and amounts to less than 5% of cases.
Squamous cell carcinoma of the cervix
Squamous cell non-keratinizing cervical cancer is the most common. This process is prone to infiltrative growth, so the likelihood of deep damage to the uterine tissue at the time of diagnosis is very high. Squamous cell keratinizing cancer of the cervix is prone to the formation of dense foci and limited growth. The process of keratinization itself is favorable, since the tumor creates a kind of dense capsule around itself, beyond which it spreads in the most advanced stages. However, radical operations in the case of cancer with a tendency to keratinize, even at stage 3, are very effective in approximately 50% of cases.
Malignant neoplasms are also differentiated depending on the degree of differentiation. The higher it is, the more favorable the prognosis, since the tumor grows slowly. The worst option is low-grade squamous cell carcinoma of the cervix. This type of neoplasm means uncontrolled cell division and a tendency to rapid metastasis. The five-year survival rate for this type of tumor, even at stage 2, is less than 30%.
Kinds
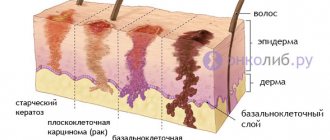
There are several forms of squamous cell keratinizing skin cancer:
- Nodular. This type is diagnosed in most cases. Characterized by the formation of one or several small nodules of 3 mm. They tend to grow together with each other. The color of the growths may be grayish, yellowish, or in rare cases red. The tumor is growing rapidly. Over time, it becomes like a plaque with a smooth or rough surface. The tumor protrudes slightly above the skin and has clear boundaries. In the middle there is a depression with a crust.
- Ulcerative. At an early stage, a papule appears on the skin, which over time turns into a dense nodule. After another period, an ulcer appears at the site of the growth. It has an irregular shape, a rough surface, and grows quickly. When touched, bleeding and an unpleasant odor occur. The tumor has a destructive effect on blood vessels and tissues.
- Papillary. Rarely seen. It appears as a nodule prone to rapid growth. The surface of the seal is lumpy and has a red or brown depression in the middle. At a later stage, the tumor may develop into an ulcer.
- Plaque. When it occurs, a reddish compaction appears on the skin, on the surface of which plaques form. The tumor grows rapidly, causing pain and bruising.
Squamous cell carcinoma with keratinization: clinical picture and treatment
Despite the fact that scientists have not yet found a remedy that can defeat cancer, the research conducted has made it possible to study the problem as much as possible and identify the main forms, types and stages of pathology.
It becomes possible to provide much better and more effective therapeutic treatment and give many patients a chance at a future life.
About the disease
Squamous cell carcinoma with keratinization is an aggressive in nature, malignant neoplasm, formed from cells of the epithelial skin layers and mucous tissues.
The anomaly is characterized by the slow development of the situation - the time intervals from one stage of the disease to the next can be quite long.
Originating in the superficial epithelial layers, cancer gradually affects neighboring lymph node connections and then metastasizes to other organs and vital systems of the human body.
Very often, this clinical picture leads to the early onset of multiple organ failure and death.
In three of four situations when diagnosing the disease, it affects the area of the face and skull. Moreover, this type of tumor is more often detected in people with light skin types, those who do not tolerate exposure to ultraviolet radiation.
The complexity of the disease lies in its ability to grow quite deeply into the internal layers of tissue, right down to the skeletal muscles. If the disease occurs against the background of cancroid, formations may develop that, almost from the moment of inception, sprout deep internal shoots.
In this situation, the malignant anomaly is constantly injured, which is accompanied by internal hemorrhages and hematomas.
There are two types of cancer with keratinization:
In the first case, the compaction is a raised area above the surface of the skin, and is also characterized by dense structural filling and a massive base. In the second, the nodular formation quickly undergoes expression.
As the anomaly progresses, irreversible processes occur in the body that destroy vascular sections, soft and hard bone tissue.
Initially, the compaction resembles a plaque, the consistency of which is denser than that of the skin. The shade of pigment at the site of the lesion becomes pink or reddish, and the lesion becomes covered with scaly, keratinized layers - hence the name of the disease.
A little later, the plaque is replaced by an ulcer, characterized by an uneven shape and blurred, ragged outlines.
In addition to the skin, the disease affects:
- respiratory system - in 40% of detected cancer cases, it penetrates into the root zone of the lung over time and is extremely difficult to diagnose;
- genitourinary sections - the cervix - the organ most affected by a tumor of this form. Initially, the pathology resembles the papilloma virus or condyloma. With timely diagnosis, the prognosis for cure is quite optimistic;
- The cervical region is poorly identified and just as difficult to treat. The clinical picture and primary symptoms are extremely vague.
Causes
The main provoking factors that can cause the development of a squamous cell tumor with keratinization are:
- incorrect exposure to the sun - direct radiation flows are extremely aggressive and can deeply affect tissues, destroying their structure at the cellular level. At the same time, the qualitative content of the cells undergoes a change, causing their degeneration;
- thermal or chemical burns - such phenomena completely break the structural molecular lattice, resulting in the appearance of abnormal, chaotically multiplying cells of a malignant nature, which, in fact, is cancer;
- direct contact with dangerous chemical components - during the production process a person may be forced to receive a certain toxic dose, which, accumulating in the body, gives rise to pathological formations;
- skin diagnoses - Paget virus, Bowen virus, xeroderma pigmentosum - the chronic course of these diseases can cause microtraumas to the surface and qualitatively change the content of tissues. The usual processes of cell division in the lesion are disrupted and the process becomes uncontrolled. After a little time, this zone becomes malignant and a precancerous anomaly forms;
- smoking - carcinogens, penetrating into the blood, create favorable conditions for the development of cancer processes in the most vulnerable places of the human body.
Stages
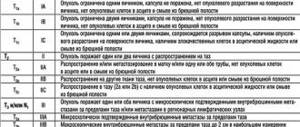
In order to better select a treatment plan for the disease, the disease is classified into the following stages:
- 1 – initial . The lesions are minimal, their size does not exceed 1-2 cm. Despite the fact that the base of the formation is not motionless, it is located within the affected area and does not injure neighboring tissues. There are no symptoms, metastasis is not detected;
- 2 – this stage is characterized by the rapid growth of the anomaly . The disease progresses, the area of distribution of mutating cells increases. However, such a course cannot yet be considered active, since the tumor can be controlled. In some cases, distant single metastasis and damage to lymph node connections located in the immediate vicinity may be observed;
- 3 – cancer spreads to most of the lymphatic system , affects surrounding formations, tissues and actively grows into neighboring organs and systems. Treatment at this stage is difficult, but there is still a chance for an optimistic prognosis. Symptoms are severe and often painful;
- 4 – the final stage of the disease, stage . Not only soft tissues, but also bone tissues and cartilage joints were subjected to irreversible processes. Even with a relatively small tumor, it is capable of producing multiple metastases. Almost all joints become immobilized. The patient endures stage 4 extremely difficult. Treatment is no longer effective. The only thing doctors can do is to alleviate the symptoms and somewhat prolong the patient’s life.
Symptoms
Despite the fact that there are practically no symptoms at the initial stages of the progression of the anomaly, as it grows, the signs make themselves felt. The following manifestations of squamous cell keratinizing carcinoma are distinguished:
- increased body temperature – characterized by a low growth rate, which accompanies the patient for a long period of time and is difficult to stop;
- fatigue, weakness - even after a full rest a person feels tired. However, this condition is not associated with physical activity. Its reason is the increased load on the body due to a developing disease, the fight against which requires additional strength;
- loss of appetite - the patient begins to eat less food, trying to save energy costs that are spent on the processes of its digestion;
- pain – depending on the location of the anomaly, the degree of pain may vary, but almost always, starting from the second stage of the disease, discomfort accompanies the pathology to one degree or another;
- swelling of the surrounding tissues - this is due to the negative impact of mutating cells on neighboring, still healthy fragments;
- disturbances of sensitivity at the site of the lesion - nerve endings become dull as inflammation spreads, their endings partially atrophy. Hence the decrease in reflex.
Diagnostics
To better determine the disease and obtain a detailed clinical picture, the following diagnostic methods are applicable:
- PET is a fairly accurate type of diagnosis. It is prescribed not only at the examination stage, but also in order to develop an optimal treatment regimen, as well as after therapy, to understand its effectiveness. Detects the presence of metastases in the lymph nodes, monitors possible risks of relapse;
- endoscopy - the method is based on the use of a special device - an endoscope, which allows you to examine the pathology approximately and in more detail and transmit the image to the monitor. In addition, it is used to take a tissue fragment for histological analysis;
- X-ray is one of the oldest diagnostic methods, and in one case it is very effective. Allows you to determine the location of the compaction and understand its approximate dimensions;
- CT scan – if this diagnosis is suspected, the doctor may prescribe a CT scan if, in the process of obtaining data, certain doubts arose about the nature of the pathology and the degree of its malignancy. The study objectively determines the type, structure, shape and size of the lesion, as well as the epithelial state of focal keratinizing cells;
- MRI gives an in-depth assessment of the condition of the tumor - allows you to understand its structure, size, shape and boundaries. Reveals the degree of damage to the organ in which the compaction is concentrated;
- biopsy is a mandatory analysis for cancer diagnosis. A fragment of material taken from the site of the lesion is sent for further microscopic examination. There, the nature and degree of aggressiveness of the cells is revealed, thus confirming or refuting the presence of a keratinizing cancer tumor;
- tumor markers - this analysis is highly likely to detect a tumor. By the body's reaction to a certain marker characteristic of a particular form of tumor, the doctor understands whether there is such a type of cancer cells in the body.
Treatment
To eliminate the disease, the following methods of influencing the tumor are used:
- removal - refers to radical ways to eliminate the problem. Depending on the location, the anomaly itself and the surrounding tissues surrounding it are removed. If the situation requires, an entire organ or section that has been irreversibly damaged by cancer can be amputated;
- Radiation therapy is used infrequently for this diagnosis, since its high effectiveness has not been proven. Can be prescribed comprehensively, before or after surgery to improve the clinic and consolidate the positive dynamics from the surgical intervention;
- Chemotherapy consists of prescribing drugs that have a detrimental effect on cancer cells without disturbing the integrity and condition of healthy tissues. The course is carried out - their duration and dosage are individual;
- cryodestruction – this procedure involves exposing the tumor to extremely low temperatures. The effectiveness of this treatment has not yet been 100% confirmed, although positive results are recorded. Due to the high cost and lack of equipment, its use is limited;
- photodynamic therapy - its principle is the selectivity of damage to tumor tissue fragments. It is done using sensitizers that precisely deliver radiation flows, and the oxygen dissolved during such therapy enters into a chemical interaction with the affected epithelial cells, provoking their death. It is used comprehensively.
Learn more about the photodynamic therapy method in this video:
Forecast
Squamous cell carcinoma with keratinization has a difficult prognosis, even if detected in a timely manner. Only treatment carried out in the early stages can improve the situation.
Thus, the five-year survival threshold against the background of intensive therapy and depending on the stage of development of the anomaly is overcome:
- 1 – more than 92%;
- 2 – about 60%;
- 3 – about 35%;
- 4 – no more than 12%.
the process of restoring the skin area after tumor removal
Regardless of the not so optimistic statistics, it is necessary to understand that persistent ignoring of the problem makes these figures even more pessimistic - in an untreated state, the disease quickly progresses and claims a person’s life 2 to 3 years after the onset of the disease.
, please select a piece of text and press Ctrl+Enter.
Source: https://stoprak.info/vidy/golovy-i-shei/chto-takoe-ploskokletochnyj-s-orogoveniem.html
Stages of pathology
Doctors distinguish several stages of squamous cell skin cancer:
- First. At an early stage of development, a small lump appears on the skin. It does not yet cause discomfort in the patient, but visually attracts attention. At the first stage there are no metastatic changes. This degree is rarely diagnosed and most often by chance, because people do not attach importance to the appearance of nodules on the cover.
- Second. At this stage, the first metastases may already occur. Usually they still develop only in the lymph nodes. The affected cells actively disperse throughout the body along with the blood. The neoplasm increases in size, has a pronounced shade and density. There is no pain when pressing on the growth.
- Third. The lesion is growing larger and larger. The presence of metastatic changes is observed not only in the lymph nodes, but also in the nearest internal organs. When the tumor is felt, pain occurs. The surface of the formation may become covered with ulcers and secrete fluid. A ridge forms along the edges of the growth, rising slightly above the epidermis.
- Fourth. At the last stage of development, metastases reach bones and cartilage. The person constantly feels severe pain. Ulcers are present at the site of the tumors.
The sooner treatment is started, the better the prognosis. It is better if therapy is carried out before the metastasis process starts.
Causes of oncology
Medicine cannot name the exact causes of squamous cell skin cancer. Why does abnormal cell activity occur, and as a result, the occurrence of malignant formation. Medicine knows the factors that contribute to an increased risk of developing squamous cell skin cancer.
- thermal or chemical burns;
- influence of carcinogenic substances (arsenic, tar, resins, soot);
- predisposition at the genetic level;
- some types of medications;
- exposure to radiation and ultraviolet.
Additional reasons are:
- Dermatic diseases of a chronic nature.
- Ulcerative lesions that do not heal, skin injuries.
- Boils.
- Inflammatory processes in the layers of the skin are permanent.
- Diseases: Reticular melanosis, Bowen's disease.
And the influence of papilloma viruses on the development of skin cancer has been confirmed by research.
Ultra-violet rays
Ultraviolet rays are one of the causes of squamous cell skin cancer. Such rays are part of the radiation from the sun and the human eye does not perceive them. When exposed to the sun for a long time, or when creating an artificial tan in ultraviolet baths, such rays affect the skin and contribute to the formation of cell mutations at the genetic level.
The tumor cell develops with less resistance to the cell's antitumor system, since the anti-oncogene that performs the protection undergoes mutation. Squamous cell skin cancer progresses with prolonged exposure to ultraviolet rays, which is why the immune system does not eliminate the negative effects of most malignant cells.
Ionizing radiation
These include x-rays, gamma rays and radiation. When exposed to such radiation, the cellular apparatus is disrupted at the genetic level, resulting in numerous mutations. The primary effect occurs on antitumor immunity, which is why the chances of developing cancer increase tenfold. Nuclear industry workers and doctors who work with ionizing radiation should be especially vigilant, as they are at risk of cancer.
Ecological situation
City dwellers of megacities are at risk of developing skin cancer, since traffic exhaust contains harmful and carcinogenic substances. And people living near industrial enterprises have a high risk of developing cancer.
Working with carcinogens
Constant inhalation of compounds associated with human work and prolonged exposure to chemical elements on the skin lead to the development of squamous cell carcinoma. Moreover, the role is played not by concentration, but by the duration of exposure to the factor.
Age
People over the age of 65 are at high risk of getting sick. The functions of most organs of the immune system are impaired with age. Cellular defense against the tumor is no longer as strong, and the detection and elimination of cancer cells becomes worse, which is the cause of the development of skin cancer.
Infections
Some viruses contribute to the development of squamous cell carcinoma. This has already been scientifically proven. Among these viruses is the papilloma virus, which changes the DNA structure of cells and is a provocateur of the development of papillomas, condylomas and other benign formations on the mucous cavities and skin. This includes HIV, which suppresses the immune system, reducing the body's immune resistance to tumors.
Diet
A correct, and most importantly healthy diet maintains the proper functioning of the human body’s defense systems. The abundance of animal fats in food increases the risk of tumors in the digestive system. A plant-based diet, such as vegetables and fruits containing vitamins, minerals and beneficial substances (folic acid or selenium), prevents the development of cancer.
Bad habits
Smoking and alcohol in excessive doses also do not have a beneficial effect on the human body. And although ethyl alcohol is not the root cause of cancer, it has a connection with their occurrence. Thanks to it, benzopyrene and other compounds penetrate cells more easily. In combination with smoking, squamous cell skin cancer has a greater chance of progression.
Diagnostics
When a patient consults a doctor, a differential examination is carried out. It is aimed at distinguishing squamous cell carcinoma from other types of oncology, as well as dermatological diseases. The first examination by the doctor is carried out using a dermatoscope. This is the name of a special device that allows you to enlarge the skin several times, which helps to assess its condition and examine the tumor in more detail.
Next, cytology is prescribed. To do this, the doctor takes a scraping from the surface of the growth. The resulting cells are then studied in the laboratory. A biopsy is also performed, during which the affected tissues are also collected, which are subsequently sent for histology. Thanks to these methods, it is possible to accurately determine whether the pathology is malignant or benign.
To detect metastasis in the body, the patient needs to undergo a number of instrumental types of examination. These include magnetic resonance imaging, radiography, and ultrasound.
Treatment
Based on the diagnostic results obtained, the doctor selects treatment tactics. There are many treatments for squamous cell skin cancer. These include:
- Surgical intervention. Removal of squamous cell skin cancer can be carried out in the usual way. The surgeon excises the growth using a scalpel. In this case, it necessarily captures another 2 cm of healthy tissue located around the tumor. This operation allows most patients to cope with oncology if it was performed correctly and at an early stage of development.
- Radiation therapy. At the first and second stages, radiation is used as an independent type of therapy, and at subsequent stages of the disease - as an addition to other methods. A stream of rays is directed at the tumor, which prevents its growth and reduces it in size. Irradiation affects only the affected tissue, without having a negative effect on healthy skin cells.
- Cryodestruction. The technique is used for small squamous cell carcinomas. During this process, the affected cells are frozen with liquid nitrogen and die.
- Electrocoagulation. It is also used for small lesions. The destruction of cancer cells occurs under the influence of electric current.
- Laser treatment. Also used for small malignant growths. A laser beam is directed at them, which vaporizes the affected cells, killing them.
- Chemotherapy. Chemical treatment for squamous cell carcinoma of the skin is usually prescribed to prepare for surgery or in case of inoperability of the tumor. The disadvantage of this method is the negative impact on the body.
To maintain the functioning of the patient's immune system, medications are prescribed that stimulate its activity. Patients are also required to take vitamin complexes.
Squamous cell skin cancer
Squamous cell skin cancer is the most malignant epithelial tumor with pronounced squamous differentiation and the ability to produce keratin. Its share in the overall morbidity structure of malignant skin tumors is about 20%. In almost every case, it occurs against the background of precancerous dermatoses (solar keratosis, etc.), intraepidermal cancers (Bowen's disease, Queyre's erythroplasia, extramammary form of Paget's disease), foci of cicatricial atrophy in tuberculous lupus, lupus erythematosus, chronic ulcerative pyoderma, trophic ulcers and etc.; scars after burns, trauma, osteomyelitis fistulas; chronic dermatoses, such as psoriasis, verrucous lichen planus, etc., much less often - de novo.
According to our data, the average age of patients with squamous cell skin cancer is 70 years.
In the development of squamous cell skin cancer, an important role is played by a combination of various environmental factors: ultraviolet radiation, ionizing radiation, chemical carcinogens, HPV. The risk of developing squamous cell skin cancer in old age increases in the presence of immune and genetic disorders.
Chronic exposure to sunlight plays a significant role in the development of this tumor, which is why the tumor is extremely often located on open areas of the skin (face, lower lip, neck, back of the hands, scalp).
Clinically, tumoral and ulcerative types of squamous cell skin cancer are distinguished, which are often solitary and less often multiple.
The tumor type is characterized by a nodule or plaque of a red-pink color or the color of unchanged skin, covered with crusts, horny masses or warty growths (warty, hyperkeratotic variety). Over several months, the tumor grows into the deep parts of the skin and subcutaneous fatty tissue, forming a dome-shaped node with a diameter of 2-3 cm or more, dense (cartilaginous) consistency, inactive, bleeding easily with mild trauma, necrotizing and ulcerating. The papillomatous variety is characterized by even more rapid growth and is characterized by individual brown-red mushroom-shaped elements on a broad base, sometimes they have the shape of a cauliflower or tomato.
The ulcerative type is divided into superficial and deep. The superficial variety does not grow in depth, but along the periphery, and is characterized by a superficial ulcer of irregular shape with clear edges, covered with a brown crust. The deep variety spreads both along the periphery and into the underlying tissues. It is distinguished by an ulcer with steep, undermined edges. The bottom of the ulcer is greasy, lumpy, yellowish-red in color with a yellow-white coating. Regional metastases in the ulcerative type are observed earlier, usually at 3-4 months of the disease. At the same time, the lymph nodes enlarge, become dense (sometimes acquiring a cartilaginous consistency), and their mobility is limited (up to complete fixation).
Histologically, squamous cell skin cancer is characterized by branching cords of cells such as cells of the spinous layer of the epidermis, infiltrating the dermis. Tumor masses contain normal and atypical elements (pleomorphic and anaplastic). Cellular atypia is manifested by different sizes and shapes of cells, enlargement and hyperchromatosis of their nuclei. There are many pathological mitoses. Tissue atypia consists of a violation of stratification and vertical anisomorphy of the multilayered flat epidermis, loss of intercellular bridges. There are dyskeratotic and parakeratotic cells, often spirally arranged, forming layered structures and surrounding extracellular accumulations of horny masses.
In histological examination, it is customary to distinguish three degrees of differentiation of squamous cell carcinoma.
Highly differentiated tumors in the skin are more common and are characterized by a regular layer-by-layer arrangement of cells in the tumor layers, preservation of intercellular bridges and pronounced keratinization with the presence of both individual keratinized cells and a large number of structures called horny pearls. Horny pearls consist of concentric layers of spinous cells, the keratinization of which gradually increases towards the center; in the center there is usually incomplete or, rarely, complete keratinization.
In poorly differentiated tumors, stratification in the layers is completely absent; the strands are formed by sharply polymorphic cells that lose the ability to keratinize. Keratin and/or intercellular bridges are preserved only in certain small areas of the tumor; the bulk of the cells are undifferentiated. Cells have different shapes and sizes, cell boundaries are poorly distinguishable. The nuclei are small, hyperchromatic, there are pale shadow nuclei and nuclei in a state of decay. A large number of pathological mitoses are detected.
Moderately differentiated squamous cell carcinoma, in terms of a set of histological and cytological features, occupies an intermediate position between well and poorly differentiated tumors.
The course of squamous cell skin cancer is characterized by steady progression with infiltration into the underlying tissues, the occurrence of pain and dysfunction of the corresponding organ. Over time, the patient may develop anemia, general weakness, metastases to internal organs lead to the death of the patient.
The degree of its malignancy is assessed by its invasiveness and ability to metastasize. The most aggressive form is the spindle cell form, as well as the acantholytic and mucin-producing variants of this tumor. In particular, the frequency of metastasis of the acantholytic variety of squamous cell skin cancer varies from 2% to 14%, and a tumor diameter of more than 1.5 cm correlates with the risk of death. Verrucous cancer metastasizes extremely rarely; such cases have been described in cases of true squamous cell carcinoma of the oral mucosa, anogenital area or sole that developed against its background, and metastasis occurred in regional lymph nodes.
Typically, the risk of metastasis increases with the thickness, diameter of the tumor, level of invasion, and decrease in the degree of cell differentiation. It also depends on the location of the tumor and whether it develops from a precancerous lesion or normal epidermis. Thus, for squamous cell skin cancer that developed against the background of solar keratosis, the frequency of metastasis is estimated at 0.5-3%, and for squamous cell skin cancer that developed against the background of solar cheilitis - at 11%. With the development of de novo squamous cell skin cancer, metastases are diagnosed in 2.7-17.3% of cases. The incidence of metastasis of squamous cell carcinoma of the skin, which developed against the background of Bowen's disease and Queyre's erythroplasia, is estimated at 2% and 20%, respectively. In 85% of cases, metastasis of squamous cell skin cancer occurs in regional lymph nodes, in 15% - in visceral organs.
The diagnosis of squamous cell skin cancer is established on the basis of clinical and laboratory data, among which histology is of decisive importance. Histological diagnosis is most difficult in the earliest stages of the disease and in undifferentiated forms. In some cases, the pathologist cannot decide whether the process is precancerous or cancerous. In such cases, it is necessary to examine the tumor using serial sections. When diagnosing verrucous cancer, a deep biopsy is necessary. Detection of squamous cell skin cancer is especially successful when there is close contact between the pathologist and the clinician. In order to develop the most rational treatment tactics for patients with squamous cell skin cancer, they should be carefully examined to detect metastases.
Differential diagnosis includes solar keratosis, basal cell carcinoma, keratoacanthoma, pseudocarcinomatous epidermal hyperplasia, Bowen's disease, Queyre's erythroplasia, Paget's disease, cutaneous horn, and sweat gland cancer.
All treatment methods for squamous cell skin cancer are aimed at radical removal of the tumor focus and obtaining a lasting clinical cure. The choice of treatment method depends on the stage, localization, extent of the process, the presence of metastases, age and general condition of the patient. The oldest, but which has not lost its importance to this day, is a surgical method of treatment, which for small tumors is based on excision of the tumor within healthy skin, 1-2 cm from the edge of the tumor, followed by plastic surgery or without it. This gives not only a good cosmetic result, but also the opportunity to obtain adequate material for pathomorphological examination. Extremely important in the surgical treatment of squamous cell skin cancer using the Moh method is microscopic control of the marginal zone of the removed tumor at the time of surgery, which makes it possible to achieve a high cure rate - up to 99% - and preserve a maximum of normal skin around the lesion. Small tumors can be successfully treated with X-rays and are the treatment of choice.
X-ray therapy is used in the treatment of elderly patients. The use of laser radiation is carried out by two methods: by fogothermic destruction of the tumor (coagulation, excision) and in the form of photodynamic therapy. Alternative treatments for PPH include systemic chemotherapy with cisplatin, bleomycin, and methotrexate. It is more often used for large, inoperable tumors. In some cases, polychemotherapy is indicated. Interferon preparations are also used to treat squamous cell skin cancer. In particular, L. Edwards et al. report a pronounced effect of intralesional injections with interferon-alpha-2-beta (1.5 million IU 3 times a week for 3 weeks). Sometimes this treatment method is combined with oral aromatic retinoids.
Prevention of squamous cell skin cancer consists, first of all, in timely detection and active treatment of precancerous dermatoses, which requires oncological vigilance among dermatologists.
There are special forms of squamous cell carcinoma of external localizations.
Squamous cell carcinoma of the lip occurs in the red border of the lips and mainly affects people aged 40 to 60 years. In the vast majority of cases, it affects the red border of the lower lip, which is more exposed to sunlight. It develops significantly more often in men than in women (40:1). Usually occurs against the background of precancerous lesions, including smokers' leukoplakia, verrucous leukoplakia, precancerous actinic cheilitis, abrasive precancrosis cheilitis, cutaneous horn, foci of discoid lupus erythematosus. Its occurrence may also be associated with immunosuppression and smoking (the incidence of this tumor in smokers is 6.5 times higher than in non-smokers).
The development of cancer begins with the appearance of scales, under which a compaction can initially be identified, which later becomes palpable to the patient himself. Sometimes the tumor manifests itself as a small erosion with a dense base or a primary painless ulceration without exophytic growth or a dense node, in place of which necrosis later develops. Initially, the pathological process is accompanied by horizontal and then vertical growth. Cancer that develops against the background of erosive actinic cheilitis can reach several centimeters in diameter and have a more or less nodular tumor part. In this case, the lip is thickened due to the tumor growing deep into it, and the corner of the mouth can be displaced by the tumor mass from metastases to the regional lymph nodes (usually on the affected side). Later, distant metastases appear. Squamous cell carcinoma of the corner of the mouth is rare, but has a more aggressive course and a tendency to metastasize. If clinical involvement of the cervical lymph nodes in the pathological process is noted in 10% of cases, then when the tumor is localized in the corner of the mouth - in 20%.
Differential diagnosis is carried out with keratoacanthoma, verrucous leukoplakia, vulgar wart, chancroid, blooming oral papillomatosis. In the differential diagnostic plan, it should be taken into account that basal cell carcinoma affects the lips only secondarily.
Squamous cell carcinoma of the oral cavity. Although the development of oral squamous cell carcinoma has traditionally been associated with leukoplakia, only 2-4% of leukoplakias are squamous cell carcinoma in situ or invasive squamous cell carcinoma histologically; Only erythroplasia and erythroleukoplasia have clinical similarities with squamous cell carcinoma. In this case, the most common (in 80% of cases) invasive squamous cell carcinoma are erythroplasias, localized in areas of high risk of malignancy: the floor of the mouth, the ventral-lateral surface of the tongue, the soft palate.
Clinically, the malignancy of erythroplasia is manifested by the presence of granularity and dotted hyperkeratosis against the background of a red velvety element, as well as granularity against the background of a smooth red spot with slight hyperkeratosis. Clinically, squamous cell carcinoma in situ can be distinguished from invasive squamous cell carcinoma of the oral cavity only by the presence of coarsening or granularity of the mucous membrane, which indicates invasive squamous cell carcinoma.
In approximately 28% of cases, during the period when oral cancer is relatively easy to treat and is not yet accompanied by metastasis, it is asymptomatic. The ego requires oncological vigilance in relation to all, even asymptomatic, but suspicious elements, which must be re-examined 10-14 days after the cause of their acute or chronic irritation has been eliminated. Elements that persist without external reasons should be examined histologically. Lipids from risk groups in the absence of clinical signs of malignancy are given a test with a 1% aqueous solution of toluidine blue, in which pathologically altered areas of the mucous membrane are more intensely stained compared to intact ones, and thereby facilitates the visual detection of precancerous lesions and squamous cell carcinoma of the oral cavity.
Squamous cell carcinoma of the oral cavity in 28% of cases is accompanied by multiple lesions affecting the lips, pharynx, larynx, esophagus, and tongue.
Squamous cell cancer of the tongue is 10 times more common in men; it occurs against the background of chronic inflammatory diseases (lichen planus, gumma), scars, leukoplakia, and blooming oral papillomatosis. The lateral edges are more often affected than the base and tip of the tongue. The tumor process is initially represented by dense nodes or foci of compaction, later by ulceration spreading to varying depths. The ulcer can be quite painful. In the presence of immunosuppression, squamous cell carcinoma of the tongue is often multiple.
The prognosis is bad. A characteristic feature of tongue cancer, as well as oral cancer in general, is early and almost exclusively lymphogenous metastasis. Moreover, its frequency increases with the spread of the primary tumor. Early lymphogenous metastases are usually dense, painless, slowly increasing in size.
Differential diagnosis is carried out with gumma, as well as with other benign or malignant tumors of the oral cavity.
Penile squamous cell carcinoma (PPCC) most often occurs in the 5th decade of life. Caused by HPV-16 and 18 types. The risk of its development increases under the influence of ultraviolet radiation, PUVA therapy, chemical carcinogens and immunosuppression. Congenital narrowness of the foreskin and acquired phimosis predispose to its development, while in men with excised foreskin, PPR is extremely rare.
Unlike squamous cell carcinoma of other localizations, PRPC often occurs de novo (92.4%) and not against the background of precancerous skin lesions. At the same time, it can develop against the background of giant Buschke-Levenshtein condyloma, cancer in situ, lichen sclerosus, chronic recurrent balanitis, cutaneous horn and some other chronic dermatoses.
The lack of sufficient hygiene skills also plays a certain role in the occurrence of PHR. The preventive effect of circumcision is associated precisely with the prevention of sperm retention, a common cause of secondary infection and phimosis. Although PRPC is generally associated with a high incidence of cervical cancer in wives of patients with this disease, many features of its development have not yet been explained.
So, it's not clear why:
- the frequency of HPV detection in PRPC is lower than in cervical cancer,
- in male sexual partners of women with cervical intraepithelial neoplasia and cervical cancer, the frequency of malignant or precancerous HPV-induced lesions of the penis was only 32.8%;
- there is no increase in the incidence of PRP in men who are sexual partners of women with cervical cancer;
- There is no dependence of the frequency of PPH on the timing of the onset of sexual activity, sexual activity, number and type of sexual partners, as is the case in women.
Differences in the course of HPV infection in men and women gave rise to the hypothesis that there are two types of HPV with different etiology: in young men - associated with a sexually transmitted virus, in older men - caused by an as yet unknown agent not associated with cancer cervix.
Most often, PRP is localized in the area of the glans penis (almost 50% of cases). There are papillomatous (exophytic, tumor); flat (endophytic, ulcerative-infiltrative) and mixed types (with signs of both types) PRPC. The papillomatous type is manifested by warty lesions on the head and/or inner layer of the foreskin, merging into a mushroom-shaped lesion, often ulcerating; flat - infiltrates spreading over the surface of the penis, quickly ulcerating like ulcus rodens. The tumor often grows into the corpora cavernosa, which leads to bleeding. Due to the addition of a secondary infection, the surface of the ulcers is usually covered with foul-smelling purulent discharge.
Although inguinal lymphadenopathy in PRPC is detected in 58% of cases, in 55% it is inflammatory and not specific, but almost 20% of non-palpable lymph nodes contain metastases. Distant metastases as a result of vascular dissemination are rare.
Histologically, depending on the severity of cellular atypia, it is customary to distinguish: well-differentiated squamous cell carcinoma, observed in 80-85% of cases, and poorly differentiated PRPC.
The prognosis for PRPC is poor - early metastases (mainly lymphogenous) occur in almost 50% of cases.
When treating PRP, surgical, radiation, and a combination of both are used. Chemotherapy (methotrexate, vincristine, vinblastine) and laser therapy, mainly carbon dioxide laser, are less commonly used.
Prevention of HPV consists of preventing HPV infection, that is, limiting casual sexual contact and using barrier methods of contraception.
Squamous cell carcinoma of the scrotum is now extremely rare and is described in workers who have occupational contact with coal tar, tar oil derivatives, petroleum, shale oil, paraffin, as well as in patients who used tar preparations in the treatment of psoriasis. Compounds of inorganic arsenic and HPV are also indicated as an etiological agent.
Clinically it is characterized by a rapidly growing nodule, which soon hardens, ulcerates and becomes painful. It is often anaplastic and often metastasizes.
Treatment consists of surgical removal, but recurrences are common.
Squamous cell carcinoma of the vulva. In older women, it is not usually associated with HPV and occurs in association with Bowen's disease, lichen sclerosus, Queyre's erythroplasia, or extramammary Paget's disease. Clinically characterized by hyperkeratotic papules, plaques or nodules, inducible erosions or eroded papules on the inner surface of the labia majora at the junction with the labia minora and the clitoris. There are infiltrating, ulcerative and papillomatous forms of cancer.
The prognosis is unfavorable due to the pronounced tendency to metastasis.
The diagnosis is confirmed histologically.
Treatment is surgical, often with removal of lymph nodes.
Prognosis and prevention
The prognosis for squamous cell skin cancer is made by the attending doctor based on data about the disease: stage of development, type of oncology, extent of the lesion. The outcome is also influenced by the effectiveness of the treatment, the patient’s compliance with all doctor’s recommendations, and the patient’s age.
Prevention of squamous cell carcinoma consists of following the following recommendations:
- Regularly undergo preventive examinations with a dermatologist.
- Promptly treat any dermatological diseases. In this case, under no circumstances should you carry out therapy on your own.
- Do not stay in the sun for a long time.
- To live an active lifestyle.
- Eat properly.
- Refrain from bad habits.
- Spend more time outdoors.
- Avoid stress.
- Follow safety rules when working with poisons and chemicals.
Only if you pay close attention to your health can you prevent the development of dangerous diseases. Therefore, you should not ignore any pathological manifestations that occur in the body.
Prevention measures
As with all skin cancers, early diagnosis and treatment are critical to the possibility of recovery. If during the operation no metastases present in neighboring lymph nodes or other organs are detected, then there is a chance of recovery. If the tumor is smaller than one centimeter, the chance of recovery is almost 100 percent. For spinal cancer in the genital area or mouth, the prognosis is worse: without treatment, carcinoma can lead to death.
Excessive UV radiation to the skin is considered a major risk factor not only for spinal cancer, but also for other types of skin cancer, such as basal cell carcinoma or black skin cancer.
For men with blond hair, hats are highly recommended. Children should not be exposed to direct sunlight. More attention should be paid to sunscreens.
Special precautions:
- avoid midday sun (11:00 to 15:00);
- do not visit the solarium;
- outdoors in good weather, look for shade, use sunscreen and a wide-brimmed hat;
- Get screened for skin cancer every two years.
Women should undergo regular gynecological examinations, as they often have squamous cell carcinoma, a histological type of cervical cancer that affects the squamous epithelium (stratified squamous epithelium that covers the vaginal part of the cervix).