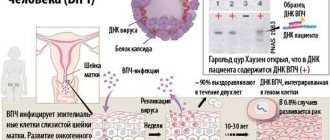
Human papillomavirus (HPV) is the most common genital tract infection caused by a virus. In total, there are about forty different types of this virus in the world that can infect the genital area of both men and women, including the vulva (female external genitalia), the skin on the surface of the penis, as well as the rectum and cervix . The human papillomavirus vaccine is now very popular.
About the virus
Certain types of HPV do not harm the human body, but others can cause a variety of malignant tumors that arise from epithelial cells and primarily in the genital area:
- A malignant tumor that develops on the mucous membrane of the cervix (cervical cancer) in women.
- Precancerous and pathological modifications of the cervix (so-called modifications of cervical cells that carry the risk of development and transformation into a malignant tumor).
- Malignant tumor of the female external genitalia (cancer of the vulva and vagina).
- Condylomas (warts) in the genital area in female and male populations.
Papilloma virus - what is it?
The term HPV refers not to one virus, but to a whole group, a separate family of papillomaviruses, of which today there are about 200 species.
In order to distinguish them, each new type is assigned a numerical name - HPV-16, 22 or 36. Not all of them are dangerous for people; some are parasitic on animals or plants. People become infected with HPV in different ways - for example, during childbirth, an infected mother can pass the virus to her baby, although the likelihood of this is low. Most often, viruses are exchanged at the beginning of sexual activity, and even condoms are not 100% protection against them. And the infection is so common that by the age of about 30, about 80% of men and women are infected with it. Usually an asymptomatic carrier of the virus develops, without any special manifestations, but some viruses provoke skin problems - papillomas (or, more simply, warts), as well as condylomas in the genital area (male and female). These formations do not look aesthetically pleasing in appearance, but are relatively safe. Of course, if it is a profuse rash in the perineal area, it is also unpleasant because it brings discomfort. We wrote about other diseases that are sexually transmitted in the article at the link. Some viruses (but not all) are oncogenic; when they remain in the body for a long time and influence cells, they sometimes provoke the development of cervical dysplasia with its possible transition to cancer. In addition, they may be involved in the development of cancer of the pharynx and larynx in men and women. There is evidence that HPV can cause penile cancer. Important! The most dangerous viruses with regard to oncology are types 16 and 18; other HPVs are less oncogenic. No specific drugs have been developed against the virus: usually, within two years from the moment it enters the body, the virus is neutralized on its own. But it is possible to become infected with new types that manifest themselves on the skin or in the genital area.
Oncology
Cervical cancer is a very serious disease that can be life-threatening for a woman. Almost all recorded cases (99%) of the development of a malignant tumor on the mucous membrane of the cervix are directly related to infection of the female genitals by certain types of congenital heart disease. These types of human papillomavirus are capable of changing the cells of the surface layer of the epithelium of the cervix, transforming them from normal healthy ones to precancerous ones. Such changes, in the absence of timely treatment, may well develop into the form of malignant tumors. This type of cancer ranks 2nd in the list of all known types of cancer that occur in the female body.
The human papillomavirus vaccine will help prevent it.
Possible complications and consequences after vaccination
Vaccination against papillomavirus in most cases does not provoke negative reactions, since it is well tolerated and completely absorbed in the body. But each patient tolerates vaccination differently, so they should be aware of possible adverse reactions.
There may be redness and swelling in the injection area. The patient reports pain when touched, as well as mild itching, which intensifies upon contact with chemicals. After a few days, the symptoms disappear. Only in some patients such manifestations persist for more than 4-6 days.
In addition to local manifestations, headache and dizziness may develop. Sometimes patients talk about weakness and loss of appetite, stomach and intestinal disorders. Such complications are easily eliminated with the help of special means and do not persist for more than 3 days in a row.
Fever is a common complication. Even in the absence of complications from other organs and systems, hyperthermia often occurs. In exceptional cases, after vaccination, loss of consciousness, muscle cramps and other reactions are possible. In this case, the patient is immediately treated and left in the hospital for observation.
Many years of experience in using the vaccine confirms its safety. It does not provoke negative consequences. Most of the negative reviews you can find are unfounded. Some women are sure that the serum leads to infertility. This opinion is erroneous and has been refuted many times during research.
Vaccination promotes the development of active immunity to human papillomavirus types 6, 11, 16 and 18. The first two cause the development of genital warts. They are found in 9 out of 10 cases of growths. HPV 6 and 11 are strains with low oncogenic risk.
HPV 16 and 18 are viruses with a high oncogenic risk; they develop in the zone of dysplasia of the cervical epithelium.
We suggest you familiarize yourself with: Red root for prostatitis, Kopeechnik root for the treatment of prostatitis
The use of vaccinations allows you to avoid infection and the development of consequences that cause enormous damage to physical, psychological, and financial well-being.
Condylomas
Genital condylomas (warts) appear when the genitals are infected with certain types of HPV. Condylomas, as a rule, appear in the form of flesh-colored growths and irregular outlines. They are found inside or outside the genital surfaces of both the male and female population. Genital warts typically cause itching, pain, discomfort and sometimes even bleeding. There have been cases when, after they were removed, they reappeared after some time. This is why the human papillomavirus is dangerous.
The human papillomavirus can be infected through household or airborne transmission from person to person, but infection primarily occurs through sexual contact. Both men and women of any race and age who engage in various types of sexual behavior that involve genital contact are at risk of infection. Most people who become infected with human papillomavirus do not develop any symptoms or signs of infection and can therefore unintentionally spread the virus to others. Everyone should know how the human papillomavirus is transmitted.
People aged 16 to 20 years are most at risk for HPV infection. This infection can sometimes heal spontaneously, but in the chronic course of the disease it can contribute to the development of a precancerous condition, and subsequently (after 20-30 years) turn into cancer.
So far, doctors and scientists have not found 100% effective and practically proven methods for treating the virus caused by the infection in question.
But there is a vaccine against the human papillomavirus. Let's take a closer look at it.
The body's reaction to vaccination
Due to the fact that the reactogenicity indicators of this category of drugs are at a low level, the vaccinated patient often does not experience any complications, and side effects occur extremely rarely. The body reacts only by:
- in a slight painful condition;
- in swelling at the insertion sites;
- in redness;
- the lesions may be itchy.
The presence of individual sensitivity leads to mild attacks:
- may hurt and feel dizzy;
- there is general malaise and weakness;
- temperature increase.
The presence of mild symptoms leading to specific reactions to vaccinations, which are manifested by redness and inflammation, does not require specific treatment. Often, such complications disappear after a few days.
When the temperature rises, it is fixed at a maximum of thirty-eight degrees, and such an increase is easily eliminated by taking antipyretic drugs such as Ibuprofen.
A vaccinated person may also experience certain complications that are caused by decreased immune functions of the body. Thus, a number of patients experienced Quincke's edema, anaphylactic shock, and urticaria. Similar complications occur in those people for whom the use of the vaccine was contraindicated.
Ibuprofen will relieve fever after vaccination
Vaccination options
There are currently two types of vaccines licensed in the world for the prevention of pathologies caused by HPV infection. These are Cervarix and the Gardasil vaccine.
They contain capsid proteins that self-assemble into virus-like particles. Such particles do not contain any genetic viral materials and therefore are not capable of causing infection.
Both vaccines protect against HPV types sixteen and eighteen, which are the cause of about 70% of cases of cervical cancer recorded worldwide. In addition, the Gardasil vaccine protects against HPV types six and eleven, which can cause mild cervical pathologies and most anogenital warts.
Benefits of HPV vaccination
The benefits of the HPV vaccine are:
- Reducing the risk of developing cervical cancer . Every year, approximately 500,000 new cases of cervical cancer are reported worldwide, half of which are fatal. Vaccination against papillomavirus provides a high percentage of guarantee that oncology will not develop.
- Reducing the risk of developing cancer of other organs . HPV is also the cause of cancer of the vagina, penis, larynx and rectum. Timely vaccination significantly reduces the likelihood of these pathologies occurring.
- Vaccination helps prevent infection with warts and genital warts in the external genital area.
- Safety . Contrary to popular belief, the HPV vaccine does not cause infertility or miscarriage. In addition, the risk of stillbirth or the birth of a child with developmental defects has not been proven at all. Also, you should not be afraid of getting infected with papillomavirus through vaccination, since modern drugs do not contain live pathogens.
- Vaccination is also effective for men , since it significantly reduces the likelihood of contracting genital warts and prevents the development of cancerous tumors of the penis and rectum.
- Formation of immunity . There are currently a number of cases where vaccination has helped develop permanent immunity against the papilloma virus.
Experience with the use of vaccines to protect against HPV
Today, the experience of using vaccines to protect against infectious diseases caused by HPV is practiced in most developed countries. And in some foreign countries, these vaccinations are even included in national immunization programs. So, for example, in the USA such vaccination is carried out among absolutely all girls aged 11-13 years, in Germany - at the age of 13-16 years, in France - at the age of 15, and in Austria - from 10 to 18 years.
The experience of using these vaccinations around the world for many years has proven their high effectiveness for prevention and complete safety.
Price for the drug
Gardasil can be purchased at prices ranging from 5,500 to 8,500 rubles. The cost of Cervarix is 3500-5500 rubles. The difference in price comes down to where exactly the vaccine will be delivered.
In order not to risk your own health, you need to get vaccinated only in trusted medical institutions, where the storage conditions of the drug were 100% observed.
Author of the article:
Lapikova Valentina Vladimirovna |
Gynecologist, reproductive specialist Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova. Our authors
Who are the HPV vaccines for?
Today, HPV vaccinations are used primarily among adolescent girls and young women.
Gardasil is approved for girls and boys aged 9 to 17 years and young women aged 18-26 years. Cervarix is currently restricted to girls and young women aged 10 to 25 years.
The age for vaccination against human papillomavirus should be discussed with your doctor.
Despite the undeniable effectiveness of these vaccines, research continues around the world on their use to protect other age groups from HPV. Over time, this will cause the age range for the use of these vaccines to expand.
Since 2009, vaccination against diseases caused by HPV has been included in the preventive vaccination calendar of Moscow. In addition, vaccination is given absolutely free at the clinic to teenage girls 12-13 years old.
Why is vaccination now recommended for adults?
Initially, the vaccine is indicated for adolescents from 8 years of age and young people up to 26 years of age. But there were no recommendations for vaccinating adults because scientists had not previously assessed its effectiveness in this age category. Today, when global studies of the vaccine among adults have been conducted, the recommendations have changed. Many people are in no hurry to start a family now and remain in a monogamous relationship all their lives, so the risk of infection increases. And most sexually active women and men were not vaccinated in childhood. If a girl donates blood during a preventive examination and does not have HPV, she is recommended to be vaccinated to protect herself from infection. There will be no harm from it, and the benefits of protection against cervical cancer are obvious. In the United States, this vaccine is already widely distributed, so there is already significant experience with its use. The vaccine does not cause any complications or severe side effects.
Schematic diagram of vaccination against diseases caused by HPV
The standard course of vaccinations involves three vaccinations:
- Gardasil is administered for the first time on any day chosen for convenience. The subsequent vaccination is given 2 months after the first time the vaccine is administered. And the final vaccine that protects against HPV is given 6 months after the first vaccination.
- The Cervarix vaccination is done according to the same scheme, but the only difference is that the second one is administered a month after the first time.
The vaccine against diseases caused by human papillomavirus is administered to all age groups as an intramuscular injection in a dose of 0.5 ml.
This is confirmed by the instructions for use of Cervarix.
What happens if you miss a revaccination?
If the patient missed the revaccination date, the second and subsequent vaccinations are given in compliance with the recommendations for maintaining a time interval between them - there is no need to start the cycle of vaccinations against papilloma again.
So, for example, when receiving the first vaccination and the revaccination is overdue, the second vaccination against papillomavirus is given as soon as the conditions for this arise, and the third - after four months when vaccinated with Gardasil and after five months when vaccinated with Cervarix.
If the first vaccination and revaccination have been done, and the last injection is overdue, then it is done immediately when the opportunity arises.
Attention! People who have started vaccination with one of the vaccines cannot continue it with another - all vaccinations given must be made with one drug (vaccines cannot replace each other).
Contraindications to vaccination against HPV
Before getting vaccinated, you must consult with an immunologist and family doctor. You should also be tested to detect human papillomavirus in the body in order to be sure that at the time of planning vaccination the person does not have diseases caused by this infection. Only a doctor can prescribe vaccination!
If suddenly a person is still infected with human papillomavirus at the time of vaccination, but has a mild form of the disease, then he can still be vaccinated. And if the disease is already advanced and long-lasting, then vaccination cannot be done until complete recovery through the use of antiviral and immune system-boosting drugs. Only after complete recovery can vaccination be carried out. Here's what else is said in the instructions for use of Cervarix:
- The vaccine is contraindicated for people who may have allergic reactions to any of the components of the vaccine. If a person is prone to allergic reactions, then he needs to inform the therapist about this before getting the vaccine. If suddenly an allergic reaction occurs after the first administration of the vaccine, then further vaccinations are strictly contraindicated.
- Vaccination cannot be carried out if at the time of vaccination a person has any infectious diseases in an acute stage or organ pathology. But acute respiratory diseases are not contraindications to vaccination.
- If a woman is prone to anaphylactic reactions, then she must notify her doctor about this before administering preventive vaccines.
Vaccination rules
The HPV vaccine is administered exclusively intramuscularly. The need for intramuscular administration in this case is determined by the need to create a small supply of the vaccine, allowing the latter to be absorbed into the blood not immediately, but in small parts, which, in turn, allows the production of the required amount of antibodies.
Intravenous administration of the vaccine leads to immediate entry of the drug into the blood, excessive activation of the immune system, complete destruction of antigens and, accordingly, no need for the production of antibodies - immunity in this case, accordingly, does not appear.
Subcutaneous or intradermal administration of the vaccine leads to an excessively slow release of the drug, complete destruction of antigens and, as in the previous case, no need for the production of antibodies. Moreover, the HPV vaccine injected under the skin can cause a lump to appear in the injection area.
Intravenous, subcutaneous and intradermal administration of the drug makes vaccination untenable, and therefore, the incorrectly administered drug is not taken into account in the vaccination schedule.
As for the intramuscular injection of the vaccine itself, the thigh or shoulder is usually used for this purpose. In this case, administration of the drug to other parts of the body is prohibited.
Vaccination during pregnancy
During pregnancy, vaccination against human papillomavirus is strictly contraindicated due to the lack of specific studies on the effects of vaccination on women during this period. Although studies of HPV vaccination in animals have not shown a negative effect on offspring, pregnant women are still not recommended to undergo vaccination.
As for vaccination of women during lactation, expert opinions differ. From an official point of view, breastfeeding is not considered a contraindication to the HPV vaccine, but there are those doctors who still do not recommend it, because a woman vaccinated during lactation will have to stop breastfeeding for several days.
Vaccination against diseases caused by human papillomavirus can be combined with vaccination against hepatitis B. Research has not yet been conducted on other vaccine combinations.
The price of Gardasil will be presented below.
Where are vaccinations given?
Today, HPV vaccination can be done in:
- in outpatient departments at the place of registration;
- antenatal clinics and gynecological departments of hospitals;
- in specialized vaccination centers.
In addition, the HPV vaccination can be done in non-governmental medical institutions that have a license for this type of activity. In this case, vaccination can be carried out at home, which will allow the manipulation to be carried out in more comfortable and familiar conditions, while avoiding contact with patients in public medical institutions.
Side effects
As a rule, after vaccination with Cervarix or Gardasil, no complications were observed in patients. Like any vaccine, the HPV vaccine can cause anaphylactic and allergic reactions in some cases. No cases of overdose have been recorded.
As with other vaccinations, after vaccination that protects against HPV, the patient may sometimes experience minor adverse reactions. There may be redness and pain at the injection site. There have been cases accompanied by general malaise after vaccination.
Those people who have already been vaccinated may experience severe headaches, dizziness, apathy and a feeling of fatigue.
How safe are vaccines?
As practice shows, vaccination against the human papillomavirus is quite safe and does not cause serious side effects. However, some complications may still occur (more on this below).
Possible complications
Thus, when carrying out vaccination against HPV, there is a possibility of the following complications:
- bleeding – if the vaccination was given to a patient who has problems with blood clotting;
- anaphylactic reactions.
Adverse reactions
After completion of vaccination, the following side effects may occur:
- development of pain at the injection site;
- itching and redness;
- slight swelling;
- headache;
- slight increase in body temperature;
- general weakness.
If Cervarix was administered, the following adverse reactions may additionally occur:
- nausea and vomiting;
- diarrhea;
- rash;
- muscle pain;
- development of infections in the upper respiratory tract.
Contraindications
The main contraindications for HPV vaccination include the following:
- individual intolerance to individual components of the vaccine;
- severe reaction of the body to the first injection;
- high body temperature.
The category of relative contraindications includes a patient's blood clotting disorder. In this case, the main advantages of such vaccination are compared with the risks that it entails.
What is the cost of vaccination and where can it be done?
Due to the relatively high cost, the HPV vaccine is not included in the preventive vaccination schedule. Typically, the course of vaccination lasts six months, and if for some reason the patient misses subsequent injections, then as soon as the opportunity arises, the vaccine is administered immediately. The vaccination course is considered completed if the drug is completely administered within a year. So, what is the price of the drug Gardasil?
In Moscow and its region, the price for a full course of vaccinations against human papillomavirus is 13-15 thousand rubles, depending on the location of the procedure and the vaccine manufacturer. It's quite expensive, but the results are worth it.
It is important to remember that the vaccines against human papillomavirus under consideration are suitable for prevention, but in no case for their treatment. Also, these vaccines cannot protect against diseases not caused by human papillomavirus.
Types of HPV vaccines, composition and principle of action
Today, specialists use therapeutic and preventive types of vaccinations for patients.
In each case, a preliminary examination is carried out, which helps to identify the presence of the virus in the body, the specific strain and the degree of neglect of the condition. Work on vaccination drugs began in the 1980s. American scientists in several states began to conduct experiments in order to obtain a remedy that could prevent the appearance of malignant neoplasms of the reproductive system.
For almost 30 years, various studies and experiments have been conducted that helped make the drug safe and effective. Already in 2007, vaccination of the population was allowed in 80 countries. Since 2010, this practice began to be used in most countries in order to prevent mass morbidity.
Therapeutic vaccines
Today, therapeutic vaccines are under development. Experts are directing their efforts to produce a product that will act not only on common strains, but also on other varieties of the virus that provoke more serious diseases.
Due to the lack of therapeutic drugs, it is impossible to completely overcome the virus. However, doctors plan to launch test studies in the near future.
Preventive vaccinations have been actively used in different countries for several years to prevent the development of papillomavirus in the body after its penetration. Today, experts have approved 2 drugs for use, which have passed all tests and are considered relatively safe.
These drugs contain special proteins of the human papillomavirus that help fight the pathogen. Additionally, the medication includes water for injection and other substances that ensure its effectiveness.
The mechanism of action of the vaccine is aimed at strengthening the body's immune defense, as well as producing specific antibodies that help prevent the spread of the virus. After entering the body, the proteins bind to the causative agents of papillomatosis, which after some time leads to the formation of antibodies against the virus strains 6, 11, 16 and 18.
Experts say that the drug is highly effective, approaching 100%. When carrying out a full course of vaccination, the likelihood of developing the virus of these strains is almost completely eliminated, which reduces the likelihood of cancer of the genital organs.
What vaccines against papillomas exist?
Today there are two types of vaccines:
- Gardasil is a quadrivalent vaccine that protects against papillomavirus types 6, 11, 16, 18. The vaccine is produced by a Dutch pharmaceutical company.
- Cervarix is a bivalent vaccine that protects against HPV types 16 and 18. Produced by Belgian.
The presented vaccines do not contain viral DNA. The basis of the preparations is the protein of microorganisms contained in the shell. The protein structure of the papillomavirus causes the production of antibodies by the immune system, which will subsequently protect the person from possible infection.
The aluminum hydroxide contained in vaccines triggers this immune response to produce enough antibodies so that the body can fight off the human papillomavirus in the future.
Vaccines are completely sterile. Their contents are poured into specially prepared syringes or vials. The volume of the bottle contains a single dose of use and is 0.5 ml. The vaccine is stored in a cool place at a temperature of 2-8 degrees. Freezing is prohibited, since freezing will cause the vaccine to lose its immunogenic properties.
According to clinical trials, both vaccines have been proven to be very effective in combating oncogenic human papillomaviruses. Many types of HPV are similar to each other. Thanks to this similarity, the HPV vaccine can protect not only against viruses types 16 and 18, but also against types 31, 33, 35, 45, 51, 56, 58, 59.
Analysis of clinical trials: the effectiveness of the HPV vaccine is still unproven
Last year, a systematic review of 10 pre- and post-licensure clinical trials of the HPV vaccine by researchers at the University of British Columbia found that the vaccine's effectiveness was not only overestimated (through the use of selective reporting or "selectiveness" of data) but also unproven. In the summary of the clinical trial review, the authors state quite unequivocally:
“We conducted a systematic review of pre- and post-licensure clinical trials of HPV vaccines to assess the evidence of their effectiveness and safety. We found that the design of HPV vaccine clinical trials and the interpretation of efficacy and safety data were largely unsatisfactory.
In addition, we note evidence of selective reporting of clinical trial results (that is, exclusion from peer-reviewed publications of vaccine efficacy measures associated with study subgroups in which efficacy may be lower or even negative).
Given this, widespread optimism about the long-term benefits of HPV vaccines appears to be based on a number of unproven assumptions (or those that are inconsistent with the evidence) and a significantly misinterpreted interpretation of the available data.
For example, HPV vaccination is said to reduce the incidence of cervical cancer by approximately 70%, even though clinical trial data to date does not show that the vaccine prevented even one case of cervical cancer (let alone about death from cervical cancer). Nor is extrapolation based on overly optimistic surrogate markers justified.
Moreover, the claim of an impressive safety profile for the HPV vaccine is supported only by the grossly flawed design of safety studies and is inconsistent with accumulated data from vaccine safety surveillance registries, as well as case reports that continue to link HPV vaccination with serious adverse outcomes (including number, death and permanent disability).
In summary, we conclude that further reductions in cervical cancer incidence are best achieved by optimizing cervical screening (which does not carry the same risks), targeting other disease factors, and not by relying on vaccines with questionable efficacy and safety profiles " [emphasis mine]