Mechanism of cyst development
The synovial capsule of the knee joint is lined from the inside with cells that produce internal lubricant (intra-articular fluid). The inner shell of the capsule, the synovium, is formed from them. It communicates with the external synovial bursae located outside the joint capsule.
Structure of the knee joint
External bags (bursae) perform shock-absorbing and protective functions, protecting the most unprotected places of the knee from damage. If necessary, excess intra-articular fluid drains and dissolves in them.
Bursa of the knee joint. Click on photo to enlarge
- Injuries.
- Autoimmune inflammation of the inner lining of the joint capsule.
- Changes in the density, structure and functions of tissues - their destruction and damage (degenerative processes).
Synovial cells begin to produce much more fluid than is necessary for normal knee function. The pressure of the fluid inside the joint increases, and it is “squeezed” outward - into the popliteal bursa, located in the area of attachment of the tendons of the semimembranosus and gastrocnemius muscles.
This is how a Baker's cyst appears - a pathological cavity with contents, limited by its own walls.
If the pathological process that caused its appearance continues, the cyst of the knee joint:
- increases in size;
- compresses adjacent tissues, causing discomfort and unpleasant, painful sensations - tingling, numbness of the foot due to impaired innervation, difficulty bending the knee, pain when pressing.
Treatment of Baker's cyst without surgery
In our manual therapy clinic, Baker's cyst is treated exclusively with conservative methods, without surgery or the use of dangerous pharmacological drugs. First, an experienced doctor conducts a detailed diagnosis and identifies the potential cause of the tumor. Then he develops an individual course of therapy. It may include the following methods of influence:
- laser therapy can reduce the size of the cyst and accelerate the process of its reverse development;
- massage increases blood flow and microcirculation of lymphatic fluid, improves the condition of all soft tissues of the knee joint;
- reflexology launches natural processes of tissue restoration by using the internal hidden reserves of the human body;
- pharmacopuncture allows you to administer microscopic doses of drugs with fibrinolytic properties, which promotes the resorption of scar tissue;
- kinesitherapy and therapeutic exercises are aimed at improving the performance of the lower limb, restoring normal blood flow and preventing the development of contracture;
- osteopathy restores the normal position of bone heads, increases the elasticity of tendon and ligament tissue.
The course of treatment for Baker's cyst is developed individually and all the patient's characteristics are taken into account. If there are problems with excess weight, then work will be carried out in this direction. If osteoarthritis, bursitis, tendovaginitis or flat feet are detected, these diseases will also be corrected and treated.
Book a free appointment with a podiatrist at our chiropractic clinic. Start treatment early and you can restore the health of your musculoskeletal system without surgery.
Causes of pathology
It is not possible to find out why a Baker's cyst forms.
- osteoarthritis of the knee: degenerative changes in tissue (loss of elasticity, disruption of structure, thinning, fragility) due to metabolic deficiencies and malnutrition;
- inflammatory processes in the joint (arthritis, synovitis);
- injuries, sprains and damage to the anatomical elements of the joint (cartilage, menisci);
- excessive physical stress on the knee;
- autoimmune processes (rheumatoid arthritis, lupus erythematosus);
- musculotendinous atrophy (weakness of the muscles, tendons and the entire knee joint);
- metabolic disorders (increased uric acid levels, gout).
If the suspected cause of a Baker's cyst cannot be determined, then it is called idiopathic.
- Age – after 40 years, the risk of pathology increases by 2 times.
- Gender – it develops less frequently in men; the ratio of sick men to sick women is 3:7.
How to treat Baker's cyst under the knee?
It is important to understand that a Baker's cyst under the knee does not just happen. There are a number of reasons that contribute to this disease. Most often this is a pathology of the knee joint and the surrounding soft tissues. Therefore, often even surgical removal of the tumor leads to a relapse in the patient over the next 12 to 18 months. This is due to the fact that the potential cause of cystic tissue changes has not been eliminated.
Before treating a Baker's cyst under the knee, you need to contact an experienced orthopedic specialist and find out what caused the appearance of such a neoplasm. An experienced orthopedist will be able to assess the condition of the cyst and give advice on effective treatment. It is likely that at this stage it will be possible to do without surgical intervention.
In manual therapy, there are a number of techniques for treating Baker's cyst conservatively. Laser therapy is used to reduce the size of the internal cavity, reflexology, osteopathy and massage.
Four types
| Type | Form |
| 1 | Elongated, shaped like a bird's beak |
| 2 | Cross-shaped |
| 3 | A small oblong crescent or slit |
| 4 | Resembles a bunch of grapes (characteristic of the chronic form of the disease) |
The division into types is important for a surgeon operating on a patient diagnosed with a popliteal Baker cyst.
Characteristic symptoms
Until a large amount of fluid accumulates in the cavity, the pathology is asymptomatic and does not cause any inconvenience or discomfort.
The first sign of a Baker's cyst is a slight swelling, a rounded bulge in the popliteal fossa, if you straighten the knee and straighten the leg.
Anterior view of the knee with the patient lying on his side. Baker's cyst is indicated by a white arrow
Sometimes after exercise the formation increases or decreases in size.
The compaction may increase in size, in which case it begins to put pressure on the tissue adjacent to it. A person experiences discomfort when bending and extending the leg at the joint, the limb below the knee goes numb, and tingling sensations occur in the lower leg and foot. Sometimes the gait changes (lameness due to impaired innervation and blood supply to tissues).
General symptoms of pathology:
- dense, round, elastic compaction in the area of the popliteal fossa;
- discomfort, pain at rest, during movement, with pressure;
- tingling, numbness in the lower leg, foot;
- impaired range of motion in the knee (the cyst prevents bending and straightening the leg).
Sometimes the gait may change, lameness may occur due to disruption of the innervation and blood supply to the tissues.
- thrombophlebitis – inflammation of the veins, accompanied by the formation of blood clots;
- thromboembolism - detachment of a blood clot and blockage of the pulmonary artery;
- soft tissue necrosis - massive cell death caused by impaired blood supply;
- osteomyelitis – inflammation of the periosteum, bone;
- purulent inflammation;
A Baker's cyst may also rupture. The membrane ruptures, the fluid that filled it escapes into the periarticular tissues, causing swelling of the lower leg, acute pain, and an increase in local temperature.
The bag can rupture, greatly increasing in size - under pressure, after a blow, or bruise.
Clinical symptoms of Baker's cyst
You can recognize the symptoms of a Baker's cyst without X-ray and ultrasound examinations. Externally, it is a rounded neoplasm, soft and dense to the touch. It is mobile, not fused with surrounding tissues. When moving under the skin it does not cause pain. Dimensions may vary. During heavy physical activity, the outflow of synovial fluid increases, and the cyst grows rapidly. After a long rest, the size may decrease.
Signs of a Baker's cyst may include the following:
- pain in the knee area;
- redness of the skin and swelling of the soft tissues around the neoplasm (indicates that there is an outflow of fluid from the internal cavity into the intercellular space of the subcutaneous fat layer);
- the mobility of the limb in the projection of the location of the cyst is limited;
- It is difficult to bend your leg when walking;
- there is a feeling of numbness due to the pressure of the tumor on the nearby nerve tissue.
If the symptoms of a Baker's cyst are controversial or indicate other pathologies, then for the purpose of differential diagnosis, ultrasound examination, x-ray, puncture with cytological examination of the obtained material, MRI and CT are prescribed.
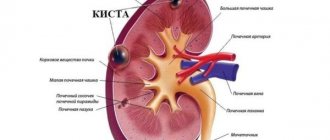
Diagnostics
The diagnosis is made based on examination and complaints of the patient. A characteristic sign is a popliteal compaction of a round shape, with slight pain when pressed.
- Oncological tumors.
- Hygroma is a benign tumor.
- Vascular aneurysms are pathological protrusions of vascular walls.
- Varicose veins are dilation of veins.
- Hematoma is post-traumatic hemorrhage into soft tissue.
A Baker's cyst of the knee joint may have symptoms similar to the pathologies listed in the list above.
The diagnosis is confirmed by instrumental studies:
- Ultrasound and MRI - help to identify the most minor changes in the soft tissues of the knee, determine the exact location and shape of the formation;
- diagnostic puncture of the contents of the cyst - extraction of fluid from the formation for analysis.
Ultrasound examination
In especially difficult cases, if ultrasound and MRI methods are not informative, arthroscopy is used. The study is carried out using an optical device, which is inserted into the cavity of the formation.
Treatment Options
At the initial stages of the disease, non-steroidal anti-inflammatory ointments (Dilac, Diclofenac, Ortofen) are applied to the sore spot to relieve inflammation; The articular joint is fixed with an elastic bandage (the bandage is not applied tightly).
As the process develops, complex conservative treatment is indicated, including drug therapy, exercise therapy, physiotherapy, and traditional medicine.
Drug therapy is aimed at:
- elimination of the root cause that provoked the formation of the cyst - treatment of the underlying disease;
- relieving inflammation, eliminating pain - non-steroidal anti-inflammatory drugs;
- disinfection - antibiotics - Macropen, Azithromycin.
- decreased activity of antigen-antibody complexes in autoimmune diseases - hormonal agents;
Complex therapy includes eliminating symptoms and improving quality of life
For a cyst formed due to osteoarthritis, intra-articular injection of corticosteroids is prescribed. This procedure effectively eliminates the inflammatory process, swelling, and improves motor activity of the limb. A method of injecting hormonal drugs into the affected joint is also used. First, the synovial secretion is sucked out using a puncture needle, and then the medication is injected.
Treatment methods: conservative, surgical, folk
The pathology is highly treatable, especially in the early stages, if the cause of its occurrence can be identified and eliminated. Provided you contact specialists in a timely manner, you can count on a full recovery.
- ranging in size from 2 mm to 3 cm;
- is asymptomatic and without complications.
- Eliminates severe symptoms of the disease (discomfort when flexing and extending the joint).
- Restore knee function (range of motion).
- Treat the disease that contributed to the appearance of the cyst.
The first stage is the extraction of fluid from the formation (puncture). A long needle of a large-volume disposable syringe is inserted into the cyst and, by pulling the piston, the contents are pumped out.
Puncture of the contents of the cyst
After successful puncture (disappearance of the protrusion), an injection of the glucocorticosteroid Hydrocortisone (hormonal anti-inflammatory drug) is given into the cavity.
At the same time prescribed:
- non-hormonal anti-inflammatory drugs (Diclofenac, Indomethacin) for local or systemic use;
- a course of physiotherapy on the popliteal area (electrophoresis with drugs: caripazim, potassium iodide, nimulide. The effectiveness was 82% among patients who completed the course of treatment.
Non-hormonal anti-inflammatory drugs
Usually, after the first puncture, the fluid is collected again, and the procedure must be repeated 2-3 times.
After the procedure, a tight, elastic bandage is applied to the knee joint. It must be worn for 2 weeks until complete restoration of function. Physical activity is limited during this period (you can walk at a walking pace).
Bandaging the knee joint with an elastic bandage
- spare the leg (do not overload the knee);
- walk in a medical compression stocking.
The general recovery period after puncture takes up to 30 days.
When and how is Baker's cyst of the knee treated surgically? Surgical removal is necessary for:
- an increase in the size of the formation to 5 cm or more;
- lack of effectiveness of conservative therapy for more than 6 months;
- carrying out three or more procedures of aspiration of the contents of the cyst (drawing out fluid);
- the appearance of symptoms of compression of adjacent tissues, disturbances of innervation and blood circulation: arise as a result of increased pressure of the cyst contents on soft tissues, nerve endings and blood vessels;
- the appearance of discomfort and pain (at rest, during movement);
- dysfunction of the knee (difficulty with flexion and extension), the appearance of lameness;
- long-term course of the pathology for more than 6 months;
- ineffectiveness of conservative therapy.
- The popliteal area is anesthetized by injecting a local anesthetic (lidocaine, novocaine).
- An incision is made above the protrusion corresponding to the size of the formation.
- The membrane is separated from the adjacent tissues (husked).
- The area connecting the formation to the capsule of the knee joint is bandaged and sutured.
- The cyst is cut off and removed.
- The dissected tissues are sutured, leaving a drainage (a tube for draining fluid, exudate (liquid that is released into the tissue from small blood vessels during inflammation) from the operated area, it is removed 3–5 days after the operation).
Surgical removal of Baker's cyst. Click on the photo to see it
Arthroscopy is most often used to remove a Baker's cyst. This is a minimally invasive intervention under the control of an optical device that is inserted into the cavity of the formation.
- the knee is fixed with a tight or plaster cast for 5–7 days;
- stepping on the foot is allowed on the 5th day, full walking - on the 14-15th day (with reasonable restrictions - no heavy lifting, running, sports training);
- the patient should wear compression garments (stockings) for the next 2–3 weeks;
- From the moment of surgery until complete recovery, it usually takes 30 days (or a little more).
Compression monostocking
Possible complications of surgical removal of a Baker's cyst:
- rupture at the time of removal (the torn shell is more difficult to peel off - to separate from the adjacent tissues);
- noticeable postoperative scars;
- bacterial infections (antibiotics are prescribed to prevent infections);
- hemorrhage into surrounding tissues due to damage to large vessels;
- pain syndrome due to innervation disorders.
Surgical treatment of Baker's cyst achieves a positive result in 90% of cases.
Folk remedies
At home, Baker's cyst can be treated until it becomes very large and is asymptomatic (does not cause tissue compression). The effectiveness of this therapy has not been proven, so you should not count on completely getting rid of Baker’s cyst at home. Although there may be an improvement - for example, a clear reduction in the size of the formation.
Folk remedies are recommended to be combined with conservative methods (after consultation with your doctor).
- Golden mustache compress. Take the green part of the Golden Usher plant (Callisia fragrant), chop finely, fill a liter jar (loosely). Fill with vodka, leave to infuse for 3 weeks (in a dark, cool place). Strain, moisten a wide bandage folded in four with the tincture, apply it to the popliteal area overnight, covered with polyethylene and woolen cloth. Continue the course for 10–12 days (can be repeated after 5 days).
- Geranium compress. Grind the leaves of the common geranium into porridge (you can grind it in a meat grinder or blender), put the resulting mass on compress paper, apply it to the popliteal area (at night), secure with a bandage. Wrap the top with woolen cloth. Compresses can be done for 10 - 12 days (5 days break, then the course of treatment for Baker's cyst of the knee joint is repeated).
- Compresses with Dimexide. Dilute the pharmaceutical liquid with water in a ratio of 1:5 or 1:6 (1 part Dimexide, 5-6 water). Moisten the prepared cotton rag or bandage, place it on the popliteal fossa (for 2–4 hours), cover with a piece of polyethylene and secure with a bandage; no need to insulate it. Continue treatment for 7 or 10 days (after 3 days you can repeat the course).
Golden mustache tincture
Compress with Dimexide
Large Baker's cyst: what to do?
If the size of the Baker's cyst is insignificant, then spontaneous reverse development of this neoplasm is possible. several massage sessions in combination with kinesitherapy and reflexology will help start the reverse process of involution of the cystic formation. But, if the size of the Baker’s cyst is large and it is visible to the naked eye and interferes with the usual movements of the lower limb, then it is necessary to approach the treatment process more responsibly.
Let us say right away that treatment of this disease using manual therapy methods is possible only in the early stages, until irreversible processes of fibrinogen deposition begin in the cyst cavity. If the cyst thickens significantly, help can only be provided surgically.
Don't delay seeing a doctor. If you have a Baker's cyst, the first thing to do is seek medical help. In a city clinic you are unlikely to find a specialist who can provide qualified assistance. In the best case scenario, you will be referred to see a surgeon. This doctor will prescribe an ointment with a non-steroidal anti-inflammatory component and a course of physical therapy (for example, electrophoresis with lidase). If the cyst is large, puncture of the internal contents will be suggested to remove fluid. As a result of such treatment, time will be lost. The cyst will harden and this will become a direct indication for surgery.
If you contact a chiropractor at an early stage of this disease, then with the help of special techniques it will be possible to achieve spontaneous removal of the cyst. Impact on the damaged bursa will prevent further accumulation of fluid in the cavity of the knee joint.
Large Baker's cysts lead to various complications:
- varicose veins of the lower limb;
- thrombosis of large blood vessels of the leg;
- lameness caused by impaired mobility in the joint;
- dystrophy of the muscle tissue of the lower leg;
- contracture of the knee joint;
- pinching of the lesser and greater tibial nerves.
Prompt treatment guarantees recovery and restoration of mobility of the injured limb. You can contact our orthopedist for an initial consultation, which is absolutely free. During the appointment, the doctor will conduct an examination and make his opinion on the possibility of treatment using manual therapy methods and its prospects.