Causes of the disease
The exact causes of primary arteritis have not yet been identified. Scientists were able to find out that certain groups of bacteria and viruses . a hereditary factor cannot be ruled out , since several cases of morbidity are often detected in one family.
Other causes of inflammation of the arteries include taking certain medications, as well as the immune reactivity of the human body.
The process of disease development begins with immune inflammation of the arterial wall. The inflammatory process occurs due to the formation of autoantibodies and immune complexes in the blood, deposited on the walls of blood vessels. Affected cells release inflammatory mediators, which leads to the formation of inflammatory foci.
Causes
The causes of arteritis have not yet been studied, which forces scientists to make assumptions about why this disease develops:
- Viruses and bacteria that infect organs and cause other diseases;
- Hereditary predisposition, which is noted in the fact that close relatives get the same diseases;
- Long-term use of medications;
- Weak immunity.
One of the causes of arteritis can be called age and lifestyle. Over the years, the walls of blood vessels become less elastic, which can lead to various disorders. A sedentary lifestyle or provoking the development of blood clots in them can become an additional factor that causes inflammation.
The main cause of the development of temporal angiitis is considered to be an autoimmune reaction, in which specific complexes are produced that destroy healthy cells. Antibodies to immunoglobulins M and A are found in the blood of most patients. Immune complexes are deposited in the elastic layer of the arterial wall, causing persistent inflammatory processes. Other causes of the disease include:
- viral infections (hepatitis, herpes, influenza);
- genetic predisposition;
- chronic autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis);
- taking certain medications (vascular damage can be promoted by treatment with antibiotics, chemotherapy drugs, immunostimulants);
- age-related changes in the body;
- penetration of toxic chemicals into the blood;
- exposure to ionizing radiation.
The causes of temporal arteritis in young people are different. Like other angitis, it occurs both as an independent pathological process (primary arteritis), the causes of which have not been thoroughly determined by science (versions of its occurrence from an infectious factor to a hereditary predisposition), and in the form of a concomitant disease (most often accompanies a disease such as rheumatic fever). polymyalgia), as well as as a consequence of other pathological conditions - the so-called secondary arteritis.
In addition, the cause of secondary temporal arteritis is advanced age, viral infections and nervous overload, causing a decline in immunity. Also, many experts consider taking large doses of antibiotics to be a provoking agent.
The disease is quite common, affecting on average 19 people out of one hundred thousand.
When Horton's syndrome occurs, the walls of the arteries become inflamed, become swollen, and the space between them narrows. As a result, blood transportation becomes difficult and the delivery of oxygen and nutrients slows down. If the disease is not diagnosed in time and treatment is not started immediately, then a thrombus may form - a blood clot that will completely block the vessel. Another danger is an aneurysm (protrusion of the wall of a vessel), which after some time can rupture.
The causes of temporal arteritis are still poorly understood. It has been proven that the process of aging of blood vessels and destruction of their walls plays a significant role in the occurrence of the disease. This is why arteritis is typical for older people (60-80 years old). More often, the disease occurs in women, as well as in people of the white race and identical twins. Researchers say arteritis may be genetically transmitted.
It is possible that environmental factors contribute to the occurrence of temporal arteritis. Many cases have been identified in which arteritis accompanies polymyalgia rheumatica. This disease is characterized by pain symptoms that manifest themselves in various muscle groups and are rheumatic in nature.
One of the signs of arteritis is constant headache
There are primary and secondary forms of arteritis.
- The primary form – vasculitis – occurs as an independent disease in older people.
- Secondary arteritis is a consequence of another infectious disease. Infections caused by Staphylococcus aureus and hepatitis virus are considered particularly dangerous.
Inside view: arteritis affected and healthy artery
Despite numerous studies that have been conducted since the first description of the manifestations of temporal arteritis by American rheumatologists Horton, Magath and Brown in 1932, they have not been reliably established. It is generally accepted that some time before the first signs of the disease appeared, the patient could come into contact with various viruses, bacteria, including Mycobacterium tuberculosis.
The possible influence of heredity is also not denied - in those areas of the globe where the population has entered into consanguineous marriages for a long time, the number of cases is significantly higher than in the population as a whole (the largest number of cases were identified in the Scandinavian countries of Europe and the northern states of the USA).
Its main foci are concentrated in the vascular wall of medium- and small-caliber arteries. As a result of these processes, normal blood flow is hampered, and the phenomena of degeneration and ischemia develop in the tissues that are located behind the site of vessel damage.
Most often, the inflammatory process in the vascular wall with giant cell arteritis affects the arteries of the head, but in exceptional cases, with rapid progression of inflammation, damage to the coronary arteries, kidney vessels, and intestines is possible - parietal blood clots can form in them, causing a progressive narrowing of the lumen of the blood vessel.
Types and symptoms
The most common type of arteritis is the so-called temporal or giant cell arteritis , in which the inflammatory process mainly affects the vessels in the eyes, temples and spine. Lack of timely medical care can lead to the development of a chronic form of the disease and complete loss of vision.
The main symptom of temporal arteritis is severe throbbing pain in the right or left temple. Also, the clinical picture may include signs of general malaise, loss of appetite, drooping eyelids on the affected side, increased body temperature, double vision and blurred vision, soreness of individual vessels in the affected area, hyperemia of the skin over them. It is worth noting that the risk group for developing temporal arteritis mainly includes older people.
People who lead a sedentary lifestyle, as well as smokers, often experience arteritis of the lower extremities , manifested mainly by pain in the legs, which intensifies after walking. Due to a local drop in temperature, the patient may constantly feel chilly in the legs, even with warm socks and shoes. In addition, there is slow growth of nails on the affected limb and hair loss.
Takayasu arteritis is a rare form of the disease that mainly affects the branches of the aorta in the arms, as well as the large arteries leading to the brain. Less commonly, the inflammatory process affects the vessels leading to the intestines, heart, and kidneys. The clinical picture of the pathology includes symptoms such as weakness in the arms, lack of pulsation in the affected area, headaches, and dizziness. This form of the disease rarely occurs in older people, but mainly affects people under 30 years of age.
Temporal arteritis
Temporal arteritis is a rheumatic vascular disease. Victims suffer mainly from unilateral, severe headaches in the temporal region.
The disease is diagnosed using ultrasound and analysis of a tissue sample. Because the disease can have serious consequences, such as blindness, it must be treated quickly.
Here on the page you can read all the important information about temporal arteritis.
ICD code for this disease : B08
What is temporal arteritis?
Temporal arteritis , also called Horton's disease, giant cell arteritis , or cranial arteritis, is a rheumatic vascular disease. Large and medium-sized vessels are mainly affected.
Most often, the disease occurs on the branches of the carotid artery. These vessels supply blood to the temporal region, the back of the head and the eyes. In approximately every fifth patient, temporal arteritis affects the aorta.
In less than one percent of cases, the disease affects blood vessels, arteries of the brain, or other arteries of internal organs.
Temporal arteritis is one of the autoimmune diseases. Because in the affected vessels certain cells of the immune system (granulocytes and lymphocytes) accumulate and form chronic inflammation.
Particularly large cells called giant cells . The disease, commonly called giant cell arteritis today, causes cells in the vessel wall to multiply and eventually narrow the affected vessel .
As a result, especially during physical activity, the blood supply is no longer sufficient. Depending on the organ affected, corresponding symptoms occur.
Temporal arteritis is also called Horton's disease or Horton's temporal arteritis, according to its discoverer. This is one of the most common rheumatic vascular diseases. The disease mainly affects adults and elderly people aged 50-70 years. Giant cell arteritis affects women about three times more often than men.
Symptoms and signs
Almost all patients with temporal arteritis have particularly severe headaches. However, most of them have common symptoms of the disease that affect the eyes, heart, circulation or nervous system long before the first headache.
Headache due to temporal arteritis
About 70 percent of people with temporal arteritis have severe headaches. The pain is mostly boring and usually occurs on one side of the temple. The pain increases when a person chews, coughs or turns his head . This occurs due to damage to the artery that supplies the chewing muscles with oxygen and nutrients.
When chewing hard foods, the masticatory muscle becomes more tense and needs more nutrients. If, when an artery is damaged, blood circulation cannot be restored, pain occurs in the temple area, scalp or masticatory muscles. Some patients have to take breaks while eating.
Visual impairment in temporal arteritis
If temporal arteritis affects the vessels in the eye, both the optic nerve and eye muscles may have limited function. Like muscles, the optic nerve must be constantly supplied with blood.
With pathological changes in the blood supply arteries, visual impairment may occur. These include short-term vision loss, in which patients suddenly lose vision in one eye and cannot see anything.
If only part of the image is missing, it is called a scotoma .
Under certain circumstances, visual impressions are perceived as flickering images. If the eye muscles are supplied with too little blood, double vision , pain when looking left and right or up and down may occur. In the worst case scenario, patients with temporal arteritis may remain blind.
Other symptoms of temporal arteritis
For some time before a typical headache occurs, patients often suffer from nonspecific symptoms of the disease .
The patient feels tired and the body temperature rises . If giant cell arteritis affects only the main artery, fever may be the only symptom of the disease.
In addition, lack of appetite and weight loss are associated symptoms of temporal arteritis.
These signs may be similar to signs of tumor diseases and therefore doctors sometimes make incorrect diagnoses.
Less than two percent of the disease affects not only the arteries outside the head, but also the internal vessels. As a result, areas of the brain may not be adequately supplied with oxygen and nutrients - this can lead to strokes with symptoms such as paralysis, speech difficulties or dizziness.
In principle, Horton's disease can affect every nerve in the body if the blood supply is limited. As a result, the sensitivity of the skin or even individual muscle movements may deteriorate. Rarely, the functioning of the heart, kidneys or lungs may be disrupted.
If the main artery is affected, the blood pressure between the two arms may differ. Additionally, in some patients, the tactile pulse at the wrist disappears.
Others suffer from arm pain, especially when they are under stress.
If it is a section of a main artery in the chest, separations (aneurysms) and ruptured blood vessels (dissections) are more likely to occur, which can be life-threatening.
In 30 to 70 percent of cases, temporal arteritis occurs as part of polymyalgia rheumatica. Those affected then additionally suffer pain in the shoulder, pelvis or neck muscles. This pain, unlike a typical headache, is usually symmetrical and does not develop so suddenly. Additionally, morning stiffness may persist and improve throughout the day. Even depressive moods are not uncommon.
Causes and risk factors
Temporal arteritis is a rheumatic disease that affects the functioning of the immune system. Certain immune cells called T cells cause an autoimmune reaction.
Why this happens is not well understood. Perhaps the disease occurs as a result of infections caused by viruses (chicken pox, rubella) or bacteria (Mycoplasma pneumoniae, chlamydia).
Because not all people with such infectious diseases develop temporal arteritis, there is likely a genetic predisposition . People with certain proteins in their white blood cells (HLA-DR4) are more prone to this condition. Additionally, temporal arteritis is more common in people with polymyalgia , another rheumatic pain syndrome.
Examinations and diagnostics
The necessary specialists if temporal arteritis is suspected are doctors of rheumatic diseases (rheumatologists) or nerve diseases (neurologists).
The American Rheumatoid Diseases Task Force (ACR) has put together a set of criteria that your doctor can use to diagnose Horton's disease.
First, the doctor takes a medical history ( anamnesis ), and then, if a disease is suspected, he orders tests, imaging studies, and a biopsy.
A blood test may show increased levels of inflammation. If a person meets at least three of the following five criteria, there is a greater than 90% chance of Horton's disease:
- age over 50 years;
- severe headaches;
- altered temporal arteries (painful, weaker pulse);
- increased erythrocyte sedimentation rate (in blood tests);
- tissue changes of the temporal artery.
Further research
In most cases, a specific ultrasound examination of the temporal arteries is performed. The temporal artery can also be examined using magnetic resonance imaging (MRI).
For this purpose, the patient is first injected into a vein with a certain contrast medium, and then placed on a movable couch in an MRI chamber.
This examination requires certain technical requirements, which can often only be carried out in specialized centers.
The restriction of blood supply caused by temporary arteritis can be further studied using positron emission tomography (PET). The examination procedure is similar to the MRI procedure.
In particular, PET is performed when the aorta or other organ systems are affected, when patients suffer from severe associated symptoms, or when tissue examination (biopsy) does not provide a definitive diagnosis.
Taking a tissue sample for temporal arteritis
If signs and imaging tests indicate temporal arteritis, in many cases a tissue sample ( biopsy ) is taken from the affected temporal area and examined in a laboratory under a microscope.
Because ultrasound does not detect disease in every patient, a tissue sample should be taken even if the ultrasound finding is undetectable.
In some cases, a piece of the artery on the other temporal side is also removed.
Treatment
Once Horton's temporal arteritis has been diagnosed, the person should be immediately treated with the drug cortisone . For the first four weeks, a dosage of one milligram of prednisolone per kilogram of body weight is recommended.
If symptoms have resolved due to therapy and blood levels of inflammation have returned to normal, the dose should be continuously reduced. If symptoms recur, more prednisolone should be taken again. The attending physician will work with the patient on a precise treatment schedule.
If blindness is inevitable, prednisolone therapy should be given in large doses through a vein over three to five days.
Because cortisone therapy can cause many unwanted side effects, it is necessary to take additional medications. Calcium and vitamin D reduce the risk of osteoporosis (brittle bones).
In case of possible vascular occlusions, aminosalicylate (for example, aspirin) should be taken. Proton pump inhibitors protect the gastric mucosa.
In addition, your blood sugar levels should be checked regularly and adjusted if necessary.
Course of the disease and prognosis
Without treatment, about 30 percent of victims go blind. However, with early diagnosis and subsequent treatment, symptoms disappear permanently in almost all patients. Rarely, the disease recurs or develops into chronic temporal arteritis Horton a.
Source: https://tvojajbolit.ru/revmatologiya/visochnyj-arteriit/
Diagnosis of arteritis
Diagnosis of arteritis in our department of vascular surgery includes a whole range of procedures:
· collection of a detailed medical history and complaints of the patient;
· conducting a general examination, during which the doctor determines the pain of the arteries, measures the pulse, listens to the heart and lungs using a phonendoscope;
· blood pressure measurement;
· carrying out general and biochemical blood tests;
· Ultrasound of blood vessels;
· angiography.
In doubtful situations, when making an accurate diagnosis is difficult, a biopsy of the affected artery may be indicated. If temporal arteritis is suspected, consultation with an ophthalmologist is also necessary.
Temporal arteritis: symptoms, diagnosis and treatment
Temporal arteritis is a systemic pathology, an inflammatory disease of the vasculitis group, affecting the temporal and carotid arteries. According to other versions, it is called giant cell arteritis, Horton's disease.
With age, arteries wear out, resulting in possible pathologies in the body. The disease is natural for an elderly person, whose blood vessels are subject to thrombosis and various negative influences.
The disease begins with an immune reaction, the production of antibodies and complexes remaining on the walls of blood vessels. The cells release mediators, resulting in inflammation.
Kinds
Types of temporal arteritis:
- by reasons of origin: primary - an independent disease, secondary - arising as a result of ailments affecting small and large arteries;
- by type of inflammation: specific, nonspecific;
- according to the course of the process - purulent, productive, necrotic;
- by localization - local or widespread.
Symptoms
The picture of the disease is expressed with symptoms adjacent to other ailments. Delayed consultation with a doctor complicates diagnosis.
Symptoms of temporal arteritis at the initial stage:
- pain in temples;
- fatigue of the masticatory muscles;
- decreased reflex when talking and eating.
Symptoms of temporal arteritis in subsequent stages:
- cough for no apparent reason;
- a sore throat;
- insufficient blood supply to the optic nerve and blurred vision (sometimes in one eye), double vision;
- fever, temperature instability;
- changes in blood pressure;
- thinning of the scalp in the hair area, which causes pain when touched;
- ocular ischemic syndrome due to deterioration of blood flow;
- sudden weight loss, fatigue.
Symptoms of temporal arteritis may include fainting and unconsciousness. Headaches are present during development and in the advanced stage. Patients typically complain of unilateral headaches.
External symptoms of temporal arteritis appear as:
- swelling of the artery, which is clearly visible externally (without treatment, the disease can lead to death);
- due to poor circulation, vision deteriorates (pain is felt in the eyeball, the perceived image becomes blurred, and without timely treatment, vision loss is threatened).
General signs
Inflammation of the aorta, artery and branches is manifested by the following general symptoms:
- lack of pulse;
- cessation of blood circulation;
- pain in the affected areas;
- loss of consciousness with dizziness;
- atrophied areas of muscles.
Forms of the disease
Inflammatory form of temporal arteritis. Symptoms and treatment: fever, headache, intensive weight loss, for which blood thinning drugs, vasoconstrictors and hormonal agents are prescribed.
Atypical form. There are no symptoms of temporal arteritis; diagnosis is possible based on headache, which can only be detected in the chronic stage. Death is possible if you do not see a doctor in time.
Generalized form. The pathological process develops without taking into account gender and age; the symptoms of temporal arteritis in young people are expressed by stroke due to inflammation of the vestibular zone, heart attack, blindness, and death. Headache is a rare symptom.
Causes
It is impossible to accurately determine the factors causing temporal arteritis. Theoretically, the disease can be triggered by genetic predisposition and natural wear and tear of the arteries with destruction of the walls. Other causes of the disease include a passive lifestyle, prerequisites for the development of blood clots, which becomes an additional factor causing inflammation.
One of the likely reasons is taking antibacterial drugs.
The prerequisites for the development of pathology are: autoimmune processes, weakened immunity, infectious diseases, which are accompanied by well-known symptoms. The cause of temporal arteritis is the production of antibodies by the body, the development of an autoimmune process and damage to large vessels, which is a precursor to the onset of the disease.
Development of the disease
The production of antibodies in the initial stage occurs due to dysfunction of the immune system as a result of the body’s interaction with infection.
Viruses are capable of changing cellular structure, which is perceived by the immune system as activation of foreign bodies. The antibodies that are produced will attach to the walls of blood vessels for destructive purposes.
As a result, inflammation occurs inside the large and medium-sized walls of the vessels, which provokes their thickening.
Granulomas then form in areas of inflammation. Histological examination reveals plasma cells, histiocytes, lymphocytes, eosinophils, plasmatic and multinucleated cells.
The vessels thicken due to inflammation, become uneven, and blood clots appear inside them. In this case, not the entire area of the artery is opened, but individual segments.
The process is asymmetrical and affects the temporal artery to a greater extent. Often other areas of the arteries are also involved. Changes are also found in the coronary, iliac, subclavian, and carotid arteries.
Aneurysms are visible in the inflamed aorta.
Diagnosis
Diagnosis of temporal arteritis involves the following measures.
In order to accurately diagnose the disease and optimal treatment, a general and biochemical blood test is prescribed, which determines the erythrocyte sedimentation rate and malfunctions of the immune system.
To exclude causes unrelated to the disease, for symptoms of temporal arteritis, diagnosis involves a biopsy of the temporal artery. If inflammation affects the organ of vision, the same analysis is carried out on the part of the eye.
If the temporal artery is affected, giant cell arteritis is likely, but in the case of other arteries, the diagnosis is not confirmed. The patient will be redirected to specialists of various profiles without receiving treatment for the pathological process. At the first symptoms, a comprehensive diagnosis is rarely carried out.
Detailed diagnosis of giant cell arteritis:
- inspection and assessment of arterial pulsation;
- detection of shallow arteries, pain and noise in them;
- recommendations from an ophthalmologist taking into account the fundus picture;
- general blood test to determine ESR, moderate normo- or hypochromic anemia;
- determination of C-reactive protein levels to analyze inflammation;
- biopsy, vascular ultrasound, angiography: the tendency of narrowing of the lumen of the arteries allows us to clarify the disease, indirect methods - to establish the diagnosis clinically.
Complications
If left untreated, other arteries may be affected, in some cases the kidneys are damaged, and ophthalmological problems arise (about 15% of complications in patients).
If the pathological process affects the functions of the central nervous system. Ischemic disorders of this type can lead to a stroke.
The presence of a pathological process in the superior mesenteric artery provokes a malfunction of the gastrointestinal tract, and the development of underlying diseases is possible.
Therapeutic measures
There is no universal scheme that allows you to effectively treat pathology, but there are a number of basic measures:
- identifying and eliminating the source of infection;
- maintaining the functions of the vascular system and affected organs;
- strengthening the immune system and central nervous system;
- removal of toxins;
- diet, fractional meals, salt restriction, replenishment of potassium and calcium.
Recommended Products:
- boiled vegetables;
- milk porridges and soups;
- lean meats and fish;
- steam omelettes;
- vegetable jelly, juices;
- rosehip decoction;
- green tea;
- fruits and berries.
ethnoscience
Experts warn against uncontrolled treatment with folk remedies during a progressive disease. But the plant components in the tinctures can improve the patient’s immunity and relieve negative symptoms. In combination with therapeutic treatment, massages, acupuncture, etc. are indicated.
For symptoms of temporal arteritis, treatment with folk remedies is as follows: the use of plants with anti-inflammatory properties that enhance immunity and reduce pain.
For temporal vasculitis it is recommended:
- chamomile tea;
- infusion of calendula (flowers);
- infusion, decoction of licorice (roots);
- tea with echinacea.
A drink with echinacea is considered preventative. Better results can be achieved in combination with the main therapy, but it is necessary to consult a specialist. Self-treatment without diagnosis is unacceptable.
Prevention
It is impossible to cure the disease at home; health can be improved with preventive methods: light physical exercise, warming procedures, breathing exercises, diet.
A diet that includes fiber and vitamins is recommended. Measures are needed to strengthen the immune system, given its relationship with the disease.
Treatment methods
Treatment of arteritis in our department is carried out by experienced, highly qualified specialists in the field of phlebology, who use various therapeutic and surgical methods in their practice.
Drug treatment of arterial inflammation involves hormonal therapy using high doses of glucocorticosteroids. As a rule, such treatment continues for a long time, up to one year. If a patient is intolerant to glucocorticosteroids, he is given other drugs that are less effective.
Patients with temporal arteritis with the threat of vision loss are prescribed special treatment, including pulse therapy with prednisone, as well as the use of vasodilators and vasodilators.
Surgical treatment of arteritis is indicated for complicated development of the disease. An operation may be prescribed if the patient has blood clots or vascular aneurysms. Surgical intervention is also required for cancer that causes the development of arteritis.
Timely diagnosed arteritis allows doctors to carry out effective therapy and completely rid the patient of the disease. If the diagnosis was made at an advanced stage with complications, the prognosis may be less favorable.
Treatment
The pathology is based on a powerful inflammatory process, which only corticosteroids can cope with. They suppress inflammation within the arteries, while at the same time being a reliable prophylactic agent. Patients are prescribed high doses of corticosteroids for oral or parenteral administration - “Decortin”, “Prednisolone”, “Medopred”, “Prednisol”. Tablets are taken 3 times a day, mainly after meals.
The duration of treatment with Prednisolone ranges from 12-24 months. Prednisolone is by far the most effective remedy in the treatment of arteritis. In almost all patients, it gives a clear therapeutic effect: body temperature normalizes, symptoms of intoxication and asthenia disappear, and ESR decreases. Glucocorticoid drugs have a number of side effects, including hyperhidrosis, the appearance of hematomas, swelling of the face, weight gain, osteoporosis in the elderly, and psycho-emotional breakdowns.
Persons who do not tolerate glucocorticoids well are treated with Methotrexate, Azathioprine and other drugs of this group.
To improve the rheological properties of blood and its state of aggregation, Aspirin, Dipyridamole, Curantil and other angioprotectors are prescribed. They restore blood microcirculation in the affected artery, reduce the risk of hypercoagulation, and eliminate vasoconstriction.
To prevent blood clots and optimize blood flow, heparin therapy is performed. Treatment with Heparin lasts five to six days, after which they proceed to the use of indirect anticoagulants, for example, Warfirin.
If infectious factors are important in the development of arteritis, patients are prescribed antibacterial or antiviral drugs - Ceftriaxone, Ofloxacin, Clindomycin, Interferon, Ingavirin.
With the development of such complications of arteritis as thrombosis of a vessel, oncopathology, or the formation of an aneurysm, surgical intervention is required. In such cases, angioprosthesis or bypass surgery is performed. During the operation, the affected areas of the vascular bed are removed, restoring vascular patency.
ethnoscience
It should be remembered that traditional medicine only relieves pain for a short time and reduces the intensity of other signs of inflammation. They don't deal with the source of the problem. This is just an “ambulance” to alleviate the condition and relieve discomfort. If the symptoms listed above appear, you should consult a doctor and undergo a full examination.
To relieve headaches, decoctions and infusions of medicinal herbs are used:
- The crushed St. John's wort herb is poured with boiling water, boiled for 15 minutes, filtered and the resulting decoction is taken for 24 hours.
- A spoonful of dried mint is poured with hot water, the container is wrapped, heated in a water bath for 15 minutes and left for an hour. The infusion is cooled and taken orally three times a day before meals.
- No less effective remedies for arteritis are: decoction and infusion of coltsfoot, wormwood, oregano, clover, valerian root, dill.
- Aloe leaf will help relieve headaches. It is cut into two halves and applied with a cut to the scalp in the temple or forehead area.
- Garlic juice is applied to a cotton swab, which is also applied to the sore head.
- Raw potatoes are applied to the head and secured with a gauze bandage on the forehead.
- Chamomile or lemon balm tea has a good therapeutic effect.
- A warm bath with sea salt will help you relax and ease your headache a little.
- Compresses with mustard, horseradish or radish are placed on the calf muscles and interscapular area.
- Black currants, lingonberries, viburnum and strawberries reduce the intensity of pain. It is recommended to eat them raw, several pieces a day, and also take berry infusion or fruit juice.
With timely consultation with a specialist and adequate therapy, the prognosis of the disease is quite favorable. Minimal pathological changes occur in the body, allowing patients to live a full and normal life.
Patients who ignore constant headaches risk becoming disabled. Advanced forms of arteritis lead to unfavorable and quite serious complications that are difficult to treat and continue to progress.
How does arteritis develop?
Temporal arteritis was described in the first half of the last century, but the exact reasons for its development have not yet been clarified. It is known that inflammation of the arterial wall is caused not by direct damage or exposure to microorganisms, but by autoimmune cell damage.
The primary production of antibodies can be triggered by a disruption of the immune system after contact with viruses and some bacteria. Viruses can change the antigenic composition of cells in the human body, which will be perceived by the immune system as the appearance of foreign harmful agents. The produced protective complexes (antibodies) will attach to the walls of blood vessels and destroy them. As a result, foci of inflammation appear in the walls of large and medium-sized arteries.
First, the vascular walls infiltrate and thicken, then granulomas—clumps of cells—form in areas of inflammation. Moreover, histological examination reveals plasma cells, lymphocytes, eosinophils, histiocytes and giant multinucleated cells. It is because of them that the disease got its name, although not all patients with the classic clinical picture have giant cells.
Due to inflammation, the vessels become thickened, with an uneven surface, and blood clots can be found inside them. In this case, not the entire area of the artery is affected, but only individual segments. This process is asymmetrical and most often involves the temporal artery. The vertebral, posterior ciliary, ophthalmic arteries, and central retinal artery are also often involved. Changes can also be detected in the carotid, subclavian, mesenteric and iliac arteries, and occasionally in the coronary arteries. And when the wall of the aorta becomes inflamed, aneurysms form in it.
Forms of the disease
Inflammatory form of temporal arteritis. Symptoms and treatment: fever, headache, intensive weight loss, for which blood thinning drugs, vasoconstrictors and hormonal agents are prescribed.
Atypical form. There are no symptoms of temporal arteritis; diagnosis is possible based on headache, which can only be detected in the chronic stage. Death is possible if you do not see a doctor in time.
Generalized form. The pathological process develops without taking into account gender and age; the symptoms of temporal arteritis in young people are expressed by stroke due to inflammation of the vestibular zone, heart attack, blindness, and death. Headache is a rare symptom.
In order to take into account all possible pathogenetic factors, it is customary to distinguish two forms of the disease:
- primary - more related to the patient’s age, is an independent disease;
- secondary - there is another pathology against which temporal arteritis develops, the connection with a previous acute infection is more pronounced.
There are two forms of temporal arteritis:
- Primary, occurs as an independent disease. Here, experts are inclined to believe that the vessels are affected precisely because of aging and loss of elasticity of the walls.
- Secondary, when the inflammatory process develops against the background of another disease, usually viral or infectious. The most dangerous viruses are staphylococcus and hepatitis.
Diagnostics
In most cases, a diagnosis of arteritis is made in patients aged 50 years or older. Its symptoms can lead to sudden blindness or stroke. Diagnosis of arteritis consists of a whole complex of sequential operations:
- Preparation of a complete detailed medical history and a set of patient complaints.
- Carrying out a comprehensive examination, during which the doctor identifies painful arteries, measures pulse pressure, using a special device - a phonendoscope, listens to the lungs and heart.
- Systolic and diastolic pressure measurements.
- Carrying out biochemical and general blood tests.
- Ultrasound examination of blood vessels.
- Radiology.
In some situations, when difficulties arise in establishing an accurate diagnosis, a biopsy of the affected artery is prescribed. It is performed under local anesthesia and requires an incision in the skull through an artery. This part contains many blood vessels, and after removing the damaged area, it becomes especially thin and delicate.
Signs of the disease
Inflammation of the aorta, artery and branches is manifested by the following general symptoms:
- lack of pulse;
- cessation of blood circulation;
- pain in the affected areas;
- loss of consciousness with dizziness;
- atrophied areas of muscles.
Elderly women are more susceptible to temporal arteritis, however, in medical practice there are exceptions in which age patients are men or people of both sexes of middle age.
In the first stages of the disease, symptoms are mild, but they can already be detected. What are the main symptoms of temporal arteritis:
- Muscle pain throughout the body, similar to rheumatic pain. Such pain can be “floating” and vague.
- Due to the pain that arises, the patient notes a general deterioration in his health: weakness, loss of appetite, sudden weight loss. The duration of development of symptoms varies and ranges from a couple of weeks to several months.
- Frequent migraine-like headaches. As a rule, they are based on one side, arise at one point and over time spread over a large area. Most often, such pains torment at night, interfere with sleep, and are either throbbing or aching in nature.
- Poor circulation and subsequent changes in mental activity.
- Body temperature, as a rule, rises slightly and remains at the reached level.
- Over time, eye pain develops. This is associated with the fact that advanced temporal arteritis contributes to the deterioration of vision, as well as the development of diseases associated with the eyes.
The symptoms and treatment of temporal arteritis are directly related. Thus, in the initial stages of the disease, which are indicated by mild symptoms, treatment will be more restrained and simpler.
If the disease has already started and has managed to develop, then the treatment will be complex and will have to be directed to all affected areas of the body.
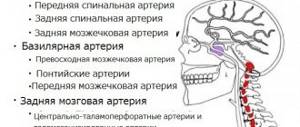
Maxillary artery
Beginning: in the thickness of the parotid gland at the level of the neck of the lower jaw;
Parts: mandibular, pterygoid, pterygopalatine;
End: pterygopalatine fossa
A. Mandibular part of the maxillary artery
Location: medially from the neck of the lower jaw;
- Deep auricular artery - to the external auditory canal;
Anterior tympanic artery – to the tympanic cavity;
Inferior alveolar artery: passes between the medial pterygoid muscle and the ramus of the mandible, then into the mandibular canal. At the level of the 1st premolar it divides into a branch to the incisors and the mental artery, which exits under the skin through the mental foramen. Gives off branches: the mylohyoid branch (to the mylohyoid and digastric muscles) and dental branches (to the teeth, alveoli and gums). The branch to the incisors supplies blood to the incisors, their alveoli and gums, the mental artery supplies the skin of the mental area and the lower lip;
Middle meningeal artery: enters the cranial cavity through the foramen spinosum and branches in the dura mater of the brain. Branches: frontal branch, parietal branch, petrous branch to the trigeminal ganglion, anastomotic branch with the lacrimal artery (participates in the blood supply to the orbit), superior tympanic artery (to the tympanic cavity);
Anastomoses: inferior labial artery, submental artery, lacrimal artery, posterior auricular artery
B. Pterygoid part of the maxillary artery
Location: in the infratemporal fossa between the lateral pterygoid and temporal muscles
- Deep temporal arteries - to the temporal muscle;
Masticatory artery - to the masticatory muscle and the temporomandibular joint;
Posterior superior alveolar artery - through the posterior superior alveolar foramina on the tubercle of the upper jaw passes to the roots of the molars;
Buccal artery - to the buccal muscle and soft tissues of the cheek;
Pterygoid branches – to the pterygoid muscles;
Anastomoses: superficial temporal artery, facial artery
B. Pterygopalatine part of the maxillary artery
Location: in the pterygopalatine fossa
- Infraorbital artery: through the inferior orbital fissure it enters the orbit, passes through the infraorbital groove and canal, through the infraorbital foramen it enters the face in the area of the canine fossa; 2nd order branches: superior anterior alveolar arteries (to the roots of premolars, canines and incisors, alveoli and gums), orbital branches (to the muscles of the eyeball); anastomoses with the ophthalmic, buccal and facial arteries;
Descending palatine artery: passes through the greater palatine canal to the mucous membrane of the palate and gums; anastomoses with the ascending palatine artery;
Sphenopalatine artery: passes through the sphenopalatine foramen into the nasal cavity. It supplies the lateral wall of the nasal cavity, the maxillary sinus and the nasal septum. anastomoses with the ascending pharyngeal artery and branches of the descending palatine artery;
Artery of the pterygoid canal. Supplies blood to the auditory tube, the mucous membrane of the tympanic cavity and the nasal part of the pharynx.
INTERNAL CAROTID ARTERY
Origin: from the common carotid artery at the level of the upper edge of the thyroid cartilage within the carotid triangle;
End: at the level of the lesser wing of the sphenoid bone, divided into medullary branches
- Cervical part - from the origin to the external opening of the carotid canal;
The stony part is located in the carotid canal;
Cavernous part - passes through the cavernous sinus of the dura mater of the brain;
Brain part - lies at the level of the optic canal
- Ophthalmic artery
- Branches to the eyeball: central retinal artery, anterior and posterior ciliary arteries;
Branches to the auxiliary apparatus of the eye: muscular branches, lacrimal artery, eyelid arteries;
Branches to the ethmoidal labyrinth and nasal cavity: anterior and posterior ethmoidal arteries;
Branches exiting to the face - frontal artery, dorsal nasal artery (exits to the face through the frontal notch of the orbit, anastomoses with the angular artery), supraorbital artery (passes to the face through the supraorbital notch, supplies blood to the skin of the forehead and frontal region, anastomoses with the superficial temporal artery)
: through the optic canal it is directed into the orbit. Groups of branches of the ophthalmic artery:
Anterior cerebral artery
supplies blood to the medial surface of the cerebral hemisphere;
Middle cerebral artery
supplies blood to the superior lateral surface of the cerebral hemisphere;
Posterior communicating artery
anastomoses with the posterior cerebral artery (branch of the basilar artery)
SUBCLAVIC ARTERY
Origin: from the brachiocephalic trunk (right subclavian artery), from the aortic arch (left subclavian artery);
End: at the level of the outer edge of the 1st rib, it passes into the axillary artery;
Course: through the upper aperture of the chest, bending around the dome of the pleura, passes into the interscalene space
Parts: 1st section (from the origin to the inner edge of the anterior scalene muscle); 2nd department (located in the interstitial space); 3rd section (from the exit from the interscalene space to the outer edge of the 1st rib);
Temporal arteritis, also known as Horton's syndrome or giant cell arteritis, is a systemic disease that is characterized by damage to the large and medium-sized arteries located in the carotid artery. Most often, the vessels supplying blood to certain areas of the head, eyes and optic nerves are affected.
Although almost any large or medium-sized artery can be involved in the pathological process. Changes in smaller vessels are not observed.
The disease manifests itself as swelling and pain in the temple area and scalp. It is mostly diagnosed in elderly and senile people (over 60 years old); according to some data, women are more susceptible to this process than men.
One of the most serious complications of temporal arteritis is considered loss of vision. This occurs due to impaired blood flow through the inflamed vessels to the eyeballs and optic nerves. As a result, without appropriate treatment measures, the nervous tissue of the retina and optic nerves dies, which leads to blindness.
Diagnostic issues
Angiography reveals changes in the arterial wall characteristic of arteritis.
If a person develops symptoms of damage to the temporal artery, then the diagnosis of giant cell arteritis is very likely. If damage to other arteries predominates, the disease may remain unconfirmed for a long time. The patient will consult doctors of various profiles and receive symptomatic therapy that does not affect the course of the underlying pathological process. Only a comprehensive assessment of all existing violations in combination with additional examinations will make it possible to clarify the cause of numerous violations. And such a diagnosis, unfortunately, is rarely carried out when the first symptoms appear.
A number of tests are used to identify giant cell arteritis:
- general examination with assessment of pulsation of various arteries;
- identification of changes in shallowly located arteries: uneven thickening of their walls, pain, the appearance of noise in them;
- consultation with an ophthalmologist to determine the fundus picture;
- CBC, which allows to detect a pronounced increase in ESR, moderate normo- or hypochromic anemia;
- determination of the level of CRP (C-reactive protein), an increase in this indicator indicates an active inflammatory process;
- biopsy of the temporal arteries to identify characteristic changes in its wall;
- Vascular ultrasound, angiography: allows you to see segmental changes in the walls of the arteries, leading to a narrowing of the lumen of the arteries.
At the same time, a biopsy allows you to reliably confirm the disease, and other laboratory methods are indirect and allow you to establish a diagnosis in combination with a characteristic clinical picture.
Main symptoms
All clinical signs of temporal arteritis can be divided into several groups:
- general symptoms of inflammation in the form of weakness, fever (infrequently), sweating, fatigue, weight loss;
- local symptoms associated with damage to superficial arteries (temporal, occipital) in the form of headache, local pain when touching the skin over the affected vessel, sometimes bulging and tortuosity of the artery;
- signs of organ failure that receive insufficient oxygen due to narrowing and thrombosis of the affected arteries.
Headache with temporal arteritis can be diffuse or one-sided, in which case it resembles a migraine. The pain intensifies when chewing, touching the temple, and is pulsating in nature.
Giant cell arteritis very often leads to ocular pathology, which is often associated with inflammation of the ophthalmic arteries (emanating from the external carotid arteries), damage to the central retinal artery and smaller ciliary arteries. This can lead to deterioration of vision and even to acute blindness. And if the vertebral arteries are damaged, double vision (diplopia) and drooping of the upper eyelid (ptosis) may occur. This is due to ischemia of the nuclei of the cranial nerves in the medulla oblongata, which are responsible for the functioning of the muscles around the eyeball.
Inflammation and subsequent thrombosis of various arteries can cause angina pectoris, attacks of weakness and pain in the limbs and tongue during exercise, abdominal pain, cerebral ischemia with the development of various neurological and mental disorders. Occasionally, with pronounced narrowing of the arteries, necrosis of the limbs and skin areas occurs.
It happens that temporal arteritis is combined with polymyalgia rheumatica syndrome, manifested by muscle pain and a feeling of stiffness. Therefore, patients with such symptoms should be further examined to exclude giant cell arteritis.