What is retinopathy
Retinopathy is a disease that affects the retinal vessels, which leads to retinal blood circulation, dystrophy and atrophy of the optic nerve.
The disease is not accompanied by pain. This is accompanied by the following symptoms:
- The appearance of floating spots before the eyes;
- Decreased vision;
- The appearance of a veil before the eyes;
- Narrowing of the field of view;
- Edema of blood vessels;
- Deterioration of central vision.
In order to diagnose the disease, it is necessary to consult a neurologist, endocrinologist and cardiologist.
Causes of retinopathy depending on the type
The causes of hypertensive retinopathy are:
- Arterial hypertension;
- Kidney failure;
- Toxicosis of pregnant women.
Diabetic retinopathy caused by type 1 or type 2 diabetes.
Arterial hypertension, obesity, nephropathy, and hyperglycemia can accelerate the appearance of symptoms of the disease. The disease develops in almost all patients with long-term diabetes mellitus.
Retinopathy can occur with the following blood pathologies:
- Leukemia;
- Polycythemia;
- Anemia;
- Waldenström's macroglobulinemia.
At the same time, the ophthalmological picture of the disease differs depending on the causes of the disease.
Atherosclerotic retinopathy develops in patients with systemic atherosclerosis. In this case, the same changes occur in the retina as with hypertensive retinopathy.
Traumatic retinopathy appears as a result of sudden compression of the chest, which causes spasm of arterioles and retinal hypoxia and the release of transudate.
The cause of the disease in premature infants is underdevelopment of the retina. Children born at a gestational age of less than 31 weeks are most susceptible to this disease.
Causes
The causes of retinopathy can be very different and depend on the form of the disease:
- Hypertensive. Develops due to increased blood pressure. With hypertension, the retinal vessels begin to spasm, as a result of which the inner membrane is split, and hyalinosis begins. The extent of damage depends on the severity of hypertension. Severe toxicosis during pregnancy or renal failure can also provoke the occurrence of pathology. What to take for such an illness? Drug therapy is primarily aimed at reducing pressure and normalizing blood circulation in the retina.
- Diabetic. It occurs as a complication of diabetes mellitus type 1 or 2 and provokes rapid deterioration of vision. Provoking factors include: prolonged course of pathology, significant increase in blood glucose levels, obesity, blood anemia, with nephropathy, increased blood pressure. Proliferative diabetic retinopathy causes retinal detachment and vision loss. The risk of developing complications increases with age.
- Traumatic. The main reason for the development of this type of disease is mechanical damage to the organs of vision, as a result of which there is pronounced vascular spasm and oxygen starvation of the retina, leading to the effusion of intraocular fluid and intraocular hemorrhages. Purtscher's retinopathy may result from chest compression.
- Atherosclerotic. The pathology develops against the background of systemic vascular atherosclerosis. With this disease, multiple pinpoint hemorrhages and blanching of the optic nerve head appear, provoking retinal detachment.
- Hemorrhagic. Occurs as a result of various blood pathologies. Most often it is a consequence of leukemia, anemia or myeloma. Features of manifestation and treatment depend on the underlying disease.
Sometimes the tamoxifen form of pathology occurs. In ophthalmology, retinopathy of prematurity is often diagnosed. The main reason for the development of this form of the disease is underdevelopment of the retinal vessels. The following factors can provoke the appearance of such a pathological condition:
- unformed body due to early birth,
- long-term use of oxygen therapy,
- too low birth weight
- the presence of concomitant pathologies,
- birth bleeding,
- inflammatory chronic diseases in the mother.
Retinopathy of prematurity is predominantly diagnosed in children who were born before 30 weeks of gestation and weigh less than 1400 grams.
Classification of the disease
Primary retinopathy is damage to the pigment epithelium in the macular zone of the retina. The disease is not inflammatory in nature.
The reasons for it have not yet been clarified. Most often, the disease manifests itself in males, aged from 20 to 40 years, who have experienced severe emotional stress. Manifests itself in the form of the following symptoms:
- Narrowing of the field of view;
- Veil before the eyes;
- Floating spots (comas) that impair vision;
- Impaired central vision.
In turn, primary retinopathy includes the following conditions :
- External exudative retinopathy;
- Central serous retinopathy;
- Acute posterior multifocal retinopathy.
In secondary cases, retinal destruction occurs as a result of various diseases, such as diabetes mellitus, atherosclerosis, and hypertension.
Secondary retinopathy includes : diabetic, atherosclerotic, traumatic, hypertensive, as well as retinopathy that occurs against the background of blood diseases.
Retinopathy of premature babies is included in a separate group.
Diabetic eye retinopathy
It occurs against the background of long-term diabetes mellitus types 1 (insulin-dependent) and type 2 (non-insulin-dependent). Typically, the development of retinopathy is preceded by nephropathy (diabetic kidney damage), arterial hypertension and obesity.
The initial stages of diabetic retinopathy are manifested by the following symptoms: decreased vision, especially at dusk, the appearance of a feeling of veils before the eyes and dark floating spots.
At the same time, it becomes difficult to perform work associated with the tension of the visual analyzer.
As the disease progresses, it becomes irreversible. Complications develop: deformation of the vitreous body, tractional retinal detachment, hemorrhage into the vitreous cavity, optic nerve atrophy.
These conditions in most cases develop 7-10 years after the onset of diabetes mellitus.
To diagnose retinopathy in diabetes mellitus, the following studies are used:
- Determine visual acuity and width of visual fields;
- Fundus ophthalmoscopy is performed with a detailed examination of the retinal vessels and optic nerve head.
- Ultrasonography. It is used to evaluate compactions, hemorrhages and scar changes on the retina.
- Electroretinography. It allows you to determine the electrical potential of the retina and evaluate its functional abilities.
- Measuring intraocular pressure (tonometry).
In complex cases, the treatment of diabetic retinopathy may require retinal angiography and laser scanning tomography.
Treatment is aimed at stabilizing diabetes mellitus and reducing blood glucose levels.
Treatment
Treatment of retinopathy begins with eliminating the factor that caused its development. For example, patients with hypertension are advised to correct blood pressure, and patients with diabetes are advised to control blood glucose levels. In addition, patients are prescribed drugs that improve blood circulation, strengthen blood vessels and normalize metabolism in the tissues of the eye.
For severe retinopathy, which can be complicated by retinal detachment, patients are advised to undergo laser coagulation. In the event of pathological neovascularization or retinal edema, patients are administered anti-VEGF factors. If retinal detachment does occur, the patient is indicated for surgical treatment (vitrectomy).
External exudative retinopathy
External exudative retinopathy most often occurs in young and middle-aged men. With it, pinpoint hemorrhages (hemorrhages) occur in the retina and cholesterol crystals are deposited. The disease usually affects one eye.
The disease progresses slowly and is accompanied by decreased visual acuity . May be complicated by retinal detachment or the formation of glaucoma. It is treated with laser coagulation of the retina.
With external exudative retinopathy, changes appear in the peripheral part of the fundus; the macular zone is affected in rare cases. Symptoms of the disease are:
- Arteriovenous shunts (direct connections of veins and arteries);
- Microaneurysms (small local expansion of the capillaries of the retina).
Central serous retinopathy
The cause of this retinopathy still remains unknown . A certain pattern was identified in the combination of the disease with migraine-type headaches.
It manifests itself as a narrowing of the visual field, a decrease in visual acuity, as well as the appearance of scotomas (dark spots in the field of vision) and micropsia - a decrease in the objects in question.
Laser coagulation of the retina is used for treatment. Medications are also prescribed to strengthen the vascular wall, reduce swelling in the retina, as well as vitamin therapy.
Acute posterior multifocal retinopathy
Can affect both eyes at the same time. Accompanied by severe swelling of the optic disc and dilation of the retinal blood vessels. In some patients, the transparency of the vitreous body decreases and iridocyclitis develops - inflammation of the iris and ciliary muscle.
The main clinical manifestation is the appearance of scotomas in the visual field and a decrease in the acuity of visual functions.
Treatment of this disease is carried out conservatively and includes the following groups of drugs:
- Vitamins (mainly retinol and ascorbic acid, read more about products with vitamins here);
- Angioprotectors - agents that protect blood vessels (for example, Solcoseryl);
- Drugs with vasodilating properties;
- Corticosteroids.
Diagnostics
The earlier retinopathy of prematurity or any other form of pathology is diagnosed, the greater the chance of successful treatment and preservation of visual function. The standard diagnostic plan includes the following methods:
- ophthalmoscopy. Used to diagnose the disease in both adult patients and premature babies;
- tonometry;
- perimetry;
- Ultrasound of the eye;
- measurement of retinal electrical potential;
- laser scanning of the retina;
- angiography.
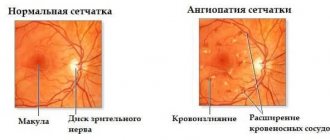
Hypertensive angiopathy
It is formed against the background of hypertension and late gestosis in pregnant women. The course of the disease is divided into four successive stages:
- Hypertensive angiosclerosis . Associated with hardening of the walls of blood vessels. It may not be clinically apparent.
- Actually hypertensive retinopathy . At this stage, organic damage to the retina occurs, associated with the deposition of lipids, hemorrhages (point hemorrhages), as well as the formation of ischemic zones in which there is no blood flow. There is a progressive decrease in visual acuity and scotomas appear. Hypertensive retinopathy develops as a result of improper treatment of hypertension. It occurs especially often when the patient does not follow all medical recommendations or self-medicates; you can read more here.
- Hypertensive neuroretinopathy . It is characterized by damage to the optic nerve head and the development of retinal detachment. These changes are irreversible.
- Optic nerve atrophy and blindness.
Diagnosis of hypertensive retinopathy is not complete without consultations with related specialists - a therapist, an endocrinologist and a cardiologist. An important role in determining the stage of retinopathy is played by ophthalmoscopy with a thorough examination of the fundus.
Treatment of retinopathy is focused primarily on stabilizing blood pressure
Treatment of retinopathy should be focused, first of all, on stabilizing blood pressure and preventing hypertensive crises, during which retinal detachment can occur.
Medications include antiplatelet agents (prevent blood clotting), angioprotectors, agents that improve microcirculation, vitamins, and lipid-lowering agents (reduce cholesterol levels in the blood plasma). As for the treatment of retinopathy itself, it is carried out by laser coagulation of the retina.
Retinopathy of the eye, signs, treatment
The retina is the thin layer of the eye's inner lining that attaches to the back of the eyeball. It is a complex multilayer structure. An image from the cornea and lens is projected onto it, after which it is converted into nerve impulses and transmitted to the visual parts of the brain. Against the background of various general and systemic diseases, pathologies often arise that lead to damage to the retina and its thinning. As a result, the optic nerve atrophies and patients lose the ability to fully see and even completely lose vision.
Retinopathy is a lesion of the retina of the eyeball that has a different etiology. The pathology develops as a consequence of impaired blood circulation due to problems with the retinal vessels. This leads to irreversible vision loss. The causes of the primary form of the disease are not fully understood and are considered idiopathic.
Secondary forms are often a complication of hypertension, diabetes, renal failure, and excess weight. However, there are other reasons for the development of disorders.
The risk group includes people who have:
- moderate and high degree of myopia;
- toxicosis in the later stages of pregnancy (preeclampsia);
- injuries to the brain and the eyeball itself;
- diseases of the cardiovascular system (atherosclerosis);
- arterial hypertension;
- diabetes mellitus, especially in old age;
- severe infectious diseases.
The disease also affects premature babies who are nursed in oxygen incubators. The pathology usually proceeds unnoticed: it is characterized by symptoms such as the appearance of spots and veils before the eyes, and a progressive decrease in visual acuity. Timely vision diagnostics using modern equipment will help identify the disease at an early stage.
Retinopathy is pathological changes in the retina of various origins.
Depending on the causes of the disease, it is customary to distinguish the following types:
- Diabetic. It develops in patients who have been suffering from type 1 or type 2 diabetes mellitus for several years, especially with high blood sugar levels, non-compliance with the recommended diet, and violation of medication and injection treatment. Risk factors are high blood pressure, lack of iron in the body, and obesity. This is the most dangerous complication of diabetes. The retinal vessels are affected, and less oxygen reaches the tissues. First, visual acuity decreases, floating spots appear and suddenly disappear. Patients find it difficult to work with small objects and read. At a later stage, in the absence of treatment and progression of the disease, complete retinal detachment occurs and visual function is lost. As part of the treatment, a full examination is carried out by an ophthalmologist and endocrinologist.
- Atherosclerotic. It occurs against the background of general atherosclerosis, since the formation of plaques impedes blood flow. Diagnosis involves performing an ophthalmoscopy (examination of the fundus of the eye) to assess the condition of the retina and the blood vessels that supply it. The specialist can also see changes in the vitreous body. With this form, pallor of the optic nerve head, lipid deposits, and small but numerous capillary hemorrhages are observed. No surgical intervention is required to correct the pathology. Patients are prescribed etiotropic therapy: anti-sclerotic agents, drugs to dilate the vessels of the retina of the eyeball, improve microcirculation in them.
- Hypertensive. This form of the disease develops as a consequence of persistently high blood pressure, renal failure and toxicosis in late pregnancy. Patients experience spasm of the capillaries of the fundus, damage to the vascular walls, and the blood supply to the retina deteriorates, which leads to changes in its structure.
- Traumatic. The disease manifests itself after mechanical damage to the eye due to a sharp spasm of blood vessels, oxygen starvation of the retina, the outpouring of intraocular fluid into it or capillary hemorrhages from the vessels. Topical vitamin drops are used as therapy.
Retinopathy OU
| Name | Form | Signs |
| Diabetic | Proliferative diabetic retinopathy OU | Complication of type I diabetes mellitus. Characteristic is the formation of new vessels that grow from the retina into the vitreous body and cause hemorrhages in it. Often leads to retinal detachment and loss of vision. |
| Diabetic maculopathy | Occurs in type II diabetes mellitus and affects the central zone of the retina, therefore central vision is reduced. | |
| Background retinopathy | Pathological changes occur only in the retina of the eyeball. | |
| Hypertensive | Hypertensive angiosclerosis | Retinal vessels change, their walls thicken |
| Neuroretinopathy | This stage is characterized by focal retinal detachments and persistent and irreversible changes in the retina. Often leads to optic nerve atrophy and complete loss of vision. Timely therapy is important. | |
| Hypertensive angiopathy | Reversible changes affecting exclusively the vessels of the retina. | |
| Retinopathy of prematurity | Retrolental fibroplasia | Occurs in children born prematurely (at 26–28 weeks). Changes occur in the retina and vitreous body due to the high concentration of oxygen in the boxes. |
Retinal vessels
Primary forms of pathology are also distinguished:
| Name | Signs and nature of development |
| Central serous | The epithelial layer of the macular region, which contains pigments, is affected. Vision deteriorates significantly, objects are distorted in size (look smaller), and the field of view decreases. Surgical methods are used for correction. |
| Sharp posterior multifocal | It often affects both eyes. Damaged vessels of the retina of the eye look swollen, the veins are enlarged. The field of vision narrows, visual acuity decreases, and inflammation of the eyeball is observed. This form of retinopathy responds well to treatment with drops to dilate and strengthen blood vessels, and anti-inflammatory drugs. |
| Coats disease | It most often occurs in men under 45 years of age, progresses slowly, and is localized at the edges of the retina. Fundus examination reveals the presence of numerous effusions of blood and intraocular fluid into the area under the retina. Complications include retinal detachment, inflammation of the iris, increased intraocular pressure, and glaucoma. Surgical correction of the disorder is required. |
Signs
With a disease such as retinopathy, symptoms do not appear immediately. They depend on the type of pathology and are usually expressed in visual impairment.
The characteristic features are as follows:
- decreased visual acuity;
- decreasing viewing angle;
- the appearance of dots, dark spots, a sudden veil;
- microscopy of objects (reduction in size).
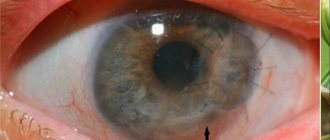
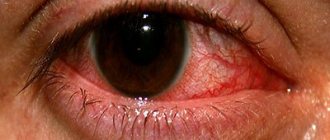
Also, hemorrhage often occurs in the eyeball, blood vessels grow, which leads to redness of the white. In severe forms of the pathology, the color of the pupil changes and its reaction is disrupted. Patients often experience symptoms of general malaise: dizziness, headache, nausea. For a more accurate diagnosis, you will need to conduct a fundus examination.
Diagnosis of the disease
Diagnosis of the disease includes visits to several highly specialized specialists - ophthalmologist, neurologist, cardiologist, endocrinologist. The attending physician writes out a referral for a comprehensive examination, which is carried out using high-precision equipment.
Ophthalmology offers the following methods:
- visual acuity test;
- perimetry - study and analysis of the visual field;
- tonometry - measurement of intraocular pressure;
- electrophysiological study, which helps determine the level of viability of the nerve cells of the retina and optic nerve;
- laser scanning of the retina;
- ultrasound examination of the internal structures of the eye;
- ophthalmoscopy - examination of the fundus of the eye, which helps to accurately assess the condition of the retina and retinal vessels, as well as the vitreous body;
- fluorescein retinal angiography.
Diagnostics is selected for each patient individually based on anamnesis and examinations performed.
Patients suffering from diabetes are examined every six months. Women during pregnancy - once every trimester. For children, an examination by an ophthalmologist is mandatory at the age of one month and then every two weeks until the retina completes its formation.
Changes in the fundus of the eye help determine the shape and type of retinopathy; for this purpose, a special study is performed - ophthalmoscopy. Typically, numerous small hemorrhages, fragile blood vessels, and exudate are observed initially. At the second stage, dilation of the retinal veins is noted. Then blockage of blood vessels occurs due to lack of oxygen and nutrients.
Treatment
With retinopathy, it is necessary to achieve compensation for concurrent diseases and eliminate the causes. Treatment of pathology depends on the type and stage of the process.
In modern medicine, two directions are used:
- Conservative - the use of eye drops, anticoagulants, vasodilators, vitamins and hormonal drugs.
- Surgical. The method of correcting the disorder depends on the extent of the lesion. As a rule, laser surgery, cryosurgical coagulation of the retina (exposure to liquid nitrogen), and vitrectomy (removal of the vitreous body) are prescribed. The operation should be entrusted only to an experienced ophthalmologist surgeon in a medical clinic, since the result is not always satisfactory.
Venous type retinopathy
Venous stasis retinopathy (ischemic) is manifested by a sudden appearance of a veil before the eyes and clouding of both eyes, doubling of objects, short-term loss of the ability to see in one eye, and a persistent decrease in visual acuity. The veins of the retina are dilated, their walls become permeable, the blood flow in them slows down, and microaneurysms are also observed. The patency of the large cervical arteries is impaired, and the presence of small hemorrhages tending to the venous vessels is also characteristic. Sclerotic processes are expressed in the arteries, and plaques form in the lumen of the arterial vessels.
Diagnosis of the disease includes fluorescein angiography. Typically, this form of pathology develops in patients with atherosclerosis, blood diseases and with complicated high myopia. It is recommended to undergo examination by an angiologist and neurosurgeon
Myopic retinopathy
This form of the disease develops against the background of myopia (myopia) of moderate and high degree. Lesions of the retina occur due to impaired blood circulation and vascular disorders. The tissues do not receive sufficient nutrition, which impairs the functioning of the retina of the eyeball.
The progression of the disease leads to the formation of degenerative processes in its cells, the optic nerve atrophies, and as a result, the patient’s visual acuity significantly decreases. The pathology should not be neglected, otherwise it may lead to loss of visual function.
Spread the love
- Pinguecula of the eye, causes, treatment Pinguecula of the conjunctiva of the eye is an ophthalmological disease in which...
- Iritis of the eye: symptoms and treatment Iritis is an ophthalmological disease in which the iris becomes inflamed...
- Signs and treatment of round-concave back Round-concave back is a postural disorder that is characterized by an increase in all…
Atherosclerotic retinopathy
It occurs against the background of atherosclerosis, a disease characterized by the appearance of cholesterol plaques on the inner wall of blood vessels. Plaques tend to constantly grow and at one point can completely block the blood flow.
Treatment of this condition requires intensive lipid-lowering therapy. Today, the most powerful group of drugs that lower cholesterol levels are statins : rosuvastatin, simvastatin, atorvastatin.
Their regular use can reduce the size of atherosclerotic plaques. In addition, antiplatelet agents, vasodilators, and neuroprotectors (drugs that protect the nerve and improve impulse transmission) are prescribed.
Traumatic retinopathy
Retinal tear Destruction of the vitreous body
It is associated with a sharp and strong compression of the chest, which leads to spasm (narrowing) of blood vessels, including retinal ones. The result is retinal hypoxia (oxygen starvation) and damage to its structure.
If there is a contusion of the eyeball, then retinal clouding develops. It is associated with tissue swelling and hemorrhage. Vitrectomy, the removal of part of the vitreous, can be used for treatment.
To correct this condition, it is necessary to carry out active correction of oxygen starvation and vitamin therapy.
Neonatal retinopathy
The disease, which develops in newborns, especially premature babies, is classified as a special type of retinopathy. The disease is often associated with incomplete formation of the structure, but a typical cause is exposure to oxygen when nursing a premature baby in an incubator. The gas has a destructive effect on tissue, leading to increased growth of retinal vessels. The greatest risk is when a baby is born at less than 31 weeks and weighs less than 1.5 kg. Treatment measures must be taken within 3-4 weeks after birth. In the future, self-limitation of the disease is possible, but in case of complications, laser coagulation or cryoretinopexy is performed. Retinopathy of newborns is dangerous due to complications in the form of subsequent development of myopia, strabismus, glaucoma, and retinal detachment.
Retinopathy of prematurity
If a baby is born at less than 32 weeks, his retina does not have time to fully develop. In particular, in some of its zones there may be no blood vessels.
The earlier the baby is born, the less developed the retina.
To prevent the development of oxygen starvation and other complications, the body begins to launch compensatory reactions aimed at activating the growth of new blood vessels. However, the wall of the newly formed vessels is very thin and fragile, which leads to the appearance of many intraocular hemorrhages.
As a result, the following complications of retinopathy in premature infants may develop:
- Astigmatism;
- Glaucoma;
- Myopia (nearsightedness);
- Strabismus;
- Cataract;
- Retinal detachment;
- Hypermetropia (farsightedness);
- Amblyopia (lazy eye syndrome).
Risk factors for retinopathy in newborns are:
- Low birth weight.
- Delivery at less than 32 weeks.
- Severe respiratory and cardiovascular failure.
- Presence of intrauterine infections.
Treatment of the disease of prematurity is surgical. Depending on the indications, it is possible to perform vitrectomy, scleroplasty, laser coagulation of the retina, or cryotherapy, in which the retina is exposed to low temperatures.
Treatment of 1-3 (active) stages
In addition to stages, retinopathy of prematurity is divided into 2 phases: active and cicatricial, the treatment of which is different. Active phases include stages 1-3 of the disease. The main method used for treatment is laser coagulation of the retina. The timing of this procedure is especially important. Just a few years ago it was believed that laser coagulation should be carried out only when the disease had reached its “threshold”. But now this opinion has radically changed. It is now believed that laser surgery should be performed at an earlier stage, i.e. at the 2nd, and now even at the 1st stage of the disease.
You should especially hurry when there are signs of “+” disease (dilation of retinal vessels). With this form of the disease, the count is not even weeks, but days. Usually the child's age at this moment is 1.5 - 2 months. During this time, the laser procedure significantly contributes to the subsidence of the activity of the process and the disease enters the stage of reverse development, and this gives hope that your baby will remain sighted. There is no doubt that the indications for laser coagulation and the timing of its implementation should be set by an ophthalmologist together with a neonatologist.
Other types of treatment, such as cryopexy (cold exposure) or any types of conservative treatment are currently of little relevance or benefit. Figures 6 and 7 schematically illustrate the effect of a laser beam: a beam of laser radiation directed through the pupil onto the retina leaves a trace in the form of white dots - laser coagulates. In Photos 1 and 2 you can see how laser surgery is performed.
4-5 (scarring) stages
Stage 4 Unfortunately, it is not always possible to perform laser surgery in time and prevent the progression of the disease. In addition, quite often the process is so aggressive that even a laser does not help. Retinopathy continues to progress and tractional retinal detachment develops. In this case, the transparent gel-like vitreous body degenerates into a scar, which, attaching to the retina, deforms and literally “rips” it from its place. Stage 4 is characterized by the appearance of partial retinal detachment. In this case, two forms are distinguished: 4a - when the detachment does not involve the central section and 4b - when the central zone is involved in the detachment (this zone has the highest visual acuity).
Stage 5 In the most unfavorable course of the disease (5%), again, despite the treatment, retinal detachment can develop into a total, so-called “funnel-shaped” form. This is stage 5 of the disease, in which even successful surgical treatment leads to a less than satisfactory result. Figure 9. At stage 5, the child does not fixate his gaze on objects and the pupil glows gray, as shown in Photos 3 and 4.