| This article violates the rule against instructions in encyclopedia articles. Its text almost completely repeats the instructions for use of the drug provided by its manufacturer. In addition, the data provided may not be sufficiently objective and reliable (especially regarding the effectiveness and safety of the drug). To maintain neutrality of presentation, it is necessary to rework this article based on independent authoritative sources of information. |
| Erythromycin | |
| Chemical compound | |
| Gross formula | C37H67NO13 |
| CAS | 114-07-8 |
| PubChem | 12560 |
| DrugBank | 00199 |
| Classification | |
| ATX | D10AF02, J01FA01, S01AA17 |
| Methods of administration | |
| oral, intravenous infusion and ointment bases[d] | |
| Other names | |
| Ilozon, Eriderm, Gryunamycin, Eric, Eratsin, Erythromycin, Erifluid, Erigexal, Synerit, Erythroped, Eomitsin, Eritran, Ermitsed, Adimicin | |
| Media files on Wikimedia Commons | |
Erythromycin
(
Erythromycin
) - is the first antibiotic that laid the foundation for the macrolide class.
IUPAC name: 6-(4-Dimethylamino-3-hydroxy-6-methyl-oxan-2-yl)oxy-14-ethyl-7,12,13-trihydroxy-4-(5-hydroxy-4-methoxy-4 ,6-dimethyl-oxan-2-yl)-oxy-3,5,7,9,11,13-hexamethyl-1-oxacyclotetradecan-2,10-dion. It was first obtained by American pharmaceutical scientists in 1952[1] from the soil actinomycete Streptomyces erythreus
.
Synonyms: Adimicin, Grunamycin, Ilozon, Zenerit (erythromycin in combination with zinc acetate), Eomitsin, Eracin, Erigeksal, Eriderm, Eric, Eritran, Erythroped, Erifluid, Ermitsed.
Pharmacological action[ | ]
A bacteriostatic antibiotic from the macrolide group, reversibly binds to the 50S subunit of ribosomes, which disrupts the formation of peptide bonds between amino acid molecules and blocks the synthesis of microbial proteins (does not affect the synthesis of nucleic acids). When used in high doses, depending on the type of pathogen, it can exhibit a bactericidal effect.
Microorganisms whose growth is inhibited at an antibiotic concentration of less than 0.5 mg/l are classified as sensitive, moderately sensitive - 1-6 mg/l, resistant - 6-8 mg/l.
The spectrum of action includes gram-positive microorganisms: Staphylococcus spp.
, producing and not producing penicillinase, including
Staphylococcus aureus
;
Streptococcus spp.
(including
Streptococcus pneumoniae
,
Streptococcus pyogenes
), alpha-hemolytic streptococcus (
Viridans
),
Bacillus anthracis
,
Corynebacterium diphtheriae
,
Corynebacterium minutissimum
;
gram-negative microorganisms: Neisseria gonorrhoeae
,
Haemophilus influenzae
,
Campylobacter jejuni
,
Bordetella pertussis
,
Brucella spp.
,
Legionella spp.
, including
Legionella pneumophila
and other microorganisms:
Mycoplasma spp.
(including
Mycoplasma pneumoniae
),
Chlamydia spp.
(including
Chlamydia trachomatis
),
Treponema spp.
,
Rickettsia spp.
,
Entamoeba histolytica
,
Listeria monocytogenes
.
Gram-negative bacilli are resistant to the drug: Escherichia coli
,
Pseudomonas aeruginosa
, and
Shigella spp.
,
Salmonella spp.
,
Bacteroides fragilis
,
Enterobacter spp.
etc. [2] Is an agonist of motilin receptors. Accelerates the evacuation of gastric contents by increasing the amplitude of pyloric contraction and improving antral-duodenal coordination.
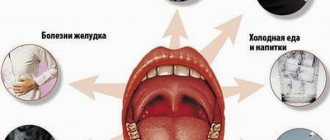
Antibiotics against sore throat: rules for taking antibiotics
Infectious lesions of the upper respiratory tract, in particular tonsillitis, are very common at any age. One of the most popular treatments for sore throat is antibiotics. However, before prescribing them, it is necessary to assess the advisability of taking antibacterial agents, as well as select the most suitable and effective drug for the respective patient.
The use of antibacterial drugs for sore throat
One of the most serious problems in the treatment of infectious diseases is the unjustified prescription of antibacterial agents. In this regard, before prescribing treatment, it is necessary to answer the following questions:
Angina
- How old is the patient? A person’s age imposes certain restrictions on the use of antibiotics, and can also indicate the type of bacteria that caused the disease. For example, pneumococcal infection very often affects children, and staphylococcus affects adults.
- What is the causative agent of sore throat - viruses or bacteria? In the case of viral tonsillitis (catarrhal form), the use of antibiotics is contraindicated, since it does not affect the course of the disease. If the causative agent is bacteria, then antibiotics are the basis of treatment.
- How does angina proceed - mild or severe with the risk of developing severe complications? Severe forms of the disease require the selection of more “severe” antibacterial agents, or their combinations.
The main factor determining the prescription of antibiotics for angina is the bacterial nature of the disease. To determine this, there are a number of signs specific to bacterial damage:
- The bacterial infection begins acutely (went to bed healthy, woke up sick), severely - the body temperature rises to 39-40 degrees, the patient experiences a headache, general weakness, fatigue, severe pain in the throat and purulent plaque on the tonsils.
- Severe intoxication syndrome can lead to nausea, even vomiting; as well as pain in the upper abdomen.
- The patient's lymph nodes in the neck can be easily felt - they are enlarged and often painful.
- In the case of scarlet fever, a small rash appears on the skin.
Viral forms of sore throat are characterized by a slower onset, low intensity of symptoms (body temperature rises to 38 degrees, etc.), as well as the presence of accompanying symptoms from the respiratory system - nasal congestion, runny nose, cough, etc.
Treatment of sore throat with antibiotics in adults
In terms of the use of antibacterial agents, the category of adult citizens includes all persons over 15 years of age, which is due to the peculiarities of the use of certain drugs. For pregnant and lactating women, treatment of sore throat with antibiotics should be carried out under the strict supervision of a doctor, due to the risk of undesirable effects of drugs on the fetus or infant.
Medicines for sore throat
The prescription of antibacterial drugs for viral sore throat if it occurs in adults is not justified.
Viral sore throats, as a rule, are mild, with minimal symptoms and go away on their own within a week.
However, if, against the background of a viral infection of the tonsils, complications begin to form and a purulent form of sore throat develops, then it is necessary to prescribe antibacterial agents.
Due to the fact that the most common causative agents of sore throat are streptococci and staphylococci, it is optimal to choose antibiotics that affect these microorganisms from the following groups:
- penicillins
- cephalosporins,
- tetracyclines
- macrolides
- fluoroquinolones
The first group of drugs is penicillins. However, before using them, it is necessary to make sure that the sick person is not allergic to these drugs, since they are the strongest allergens.
The most commonly used is Amoxicillin and its protected analogue, Amoxiclav. The drugs are extremely effective and can cure a sore throat without complications.
In addition to them, Flemoxin, Flemoxin Solutab, etc. can be used from this group.
If penicillins are ineffective or the patient is allergic to them, drugs from the cephalosporin group are used. These include: Cephalexin, Cefotaxime, Ceftriaxone, etc. Most of them are available in the form of capsules or solutions for injection.
Severe sore throat in adults is an indication for the use of fluoroquinolones: Ciprofloxacin, Levofloxacin, etc. However, pregnancy and breastfeeding are direct contraindications to them.
Treatment of sore throat with antibiotics in children
Treatment of bacterial forms of tonsillitis (follicular, lacunar, etc.) must necessarily be carried out using antibiotics, due to the frequent development of complications when refusing these drugs. The best and most popular forms of antibacterial agents for young children are syrups and suspensions.
The drug of choice is again Amoxicillin or Amoxiclav. In case of allergy to these drugs, either cephalosporins or Azithromycin (Sumamed) are used.
Antibiotics for sore throat in children should only be prescribed by the attending physician. An incorrectly selected drug may be useless or even harmful to health.
The use of macrolides (Erythromycin, etc.) in children under 15 years of age is contraindicated due to their toxic effect on the body
Contraindications to the use of antibiotics
Despite the high effectiveness of antibacterial agents, their use is limited by a number of contraindications:
Antibiotics
- Allergic reactions and individual intolerance to components. This is especially true for drugs from the penicillin group, which often cause allergic reactions in patients.
- Diseases associated with liver damage lead to disruption of the metabolism of antibiotics and require adjustment of “standard” dosages.
- Kidney diseases lead to decreased excretion of the antibiotic and its metabolites from the body.
- Macrolides and fluoroquinolones are contraindicated in childhood, as well as for use in pregnant and lactating women, due to the toxic effect on the developing and growing organism.
Indications[ | ]
Bacterial infections caused by sensitive pathogens: diphtheria (including bacterial carriage), whooping cough (including prevention), trachoma, brucellosis, Legionnaires' disease, erythrasma, listeriosis, scarlet fever, amoebic dysentery, gonorrhea; pneumonia in children, genitourinary infections in pregnant women caused by Chlamydia trachomatis
; primary syphilis (in patients with allergies to penicillins), uncomplicated chlamydia in adults (with localization in the lower genitourinary tract and rectum) with intolerance or ineffectiveness of tetracyclines, etc.; infections of the ENT organs (tonsillitis, otitis media, sinusitis); biliary tract infections (cholecystitis); infections of the upper and lower respiratory tract (tracheitis, bronchitis, pneumonia); infections of the skin and soft tissues (pustular skin diseases, including juvenile acne, infected wounds, bedsores, stage II-III burns, trophic ulcers).
Prevention of exacerbations of streptococcal infections (tonsillitis, pharyngitis) in patients with rheumatism. Prevention of infectious complications during medical and diagnostic procedures (including preoperative bowel preparation, dental interventions, endoscopy, in patients with heart defects). Gastroparesis (including gastroparesis after vagotomy surgery, diabetic gastroparesis and gastroparesis associated with progressive systemic sclerosis).
It is a reserve antibiotic for allergies to penicillin.
Erythromycin during pregnancy - reviews
Victoria:
During pregnancy I developed terrible and painful acne. I read that you can get rid of them using Erythromycin ointment. Before use, I consulted with a gynecologist, and she was not against it. I smeared acne on my face and back once a day for a week. The acne gradually disappeared, leaving no trace behind.
Oksana:
Conjunctivitis appeared unexpectedly. Eye drops did not help, so the doctor prescribed erythromycin ointment. At first I was afraid to use it, because an antibiotic during pregnancy can be dangerous, but I still decided to undergo treatment. My eyes were cured in just three days. There were no complications from the ointment.
Anna:
While in the second month of pregnancy, she fell ill with pyelonephritis. The hospital prescribed Erythromycin injections for two weeks. I was very afraid of complications, but the baby was born healthy.
Side effects[ | ]
From the digestive system: nausea, vomiting, gastralgia, abdominal pain, tenesmus, diarrhea, dysbacteriosis, rarely - oral candidiasis, pseudomembranous enterocolitis, liver dysfunction, cholestatic jaundice, increased activity of liver transaminases, pancreatitis.
On the part of the hearing organs: ototoxicity - hearing loss and/or tinnitus (when used in high doses - more than 4 g / day, usually reversible).
From the cardiovascular system: rarely - tachycardia, prolongation of the QT interval on the ECG, atrial fibrillation and/or flutter (in patients with a prolonged QT interval on the ECG).
Allergic reactions: urticaria, other forms of skin rash, eosinophilia, rarely - anaphylactic shock.
Local reactions: phlebitis at the site of intravenous administration.
Overdose[ | ]
Symptoms: impaired liver function, up to acute liver failure, rarely - hearing impairment.
Treatment: activated carbon, careful monitoring of the state of the respiratory system (if necessary, artificial ventilation), acid-base status and electrolyte metabolism, ECG. Gastric lavage is effective when taking a dose five times higher than the average therapeutic dose. Hemodialysis, peritoneal dialysis and forced diuresis are ineffective.
Erythromycin
Latest update of the description by the manufacturer 01.07.2002
Erythromycin* J01FA01 Erythromycin
1 enteric-coated tablet contains erythromycin 200 mg; 16 pcs in a blister, 1 blister in a box.
Macrolide antibiotic.
Pharmacological action - antibacterial.
Streptococcal, staphylococcal and mycoplasma infections, tonsillitis, acute sinusitis, pneumonia, Legionnaires' disease, endocarditis, enteritis, osteomyelitis, chlamydia, syphilis.
Hypersensitivity, liver failure.
Nausea, vomiting, diarrhea, liver dysfunction, jaundice, pseudomembranous colitis, allergic reactions.
Orally, 1 hour before meals or 2 hours after meals, with a sufficient amount of liquid. The dosage is determined individually, usually by adults:
200–400 mg 4 times a day every 6 hours, if necessary, increase the dose to 4 g per day;
children:
30–40 mg/kg/day, in 2–4 divided doses. Course - 7–10 days.
In a place protected from moisture, at a temperature not exceeding 25 °C.
Keep out of the reach of children.
3 years.
Do not use after the expiration date stated on the package.
Erythromycin - instructions for medical use - RU No. P N002712/01-2003 dated 2008-10-07 Erythromycin - instructions for medical use - RU No. LP-000211 dated 2016-03-21 Erythromycin - instructions for medical use - RU No. LSR- 009305/08 dated 2016-09-12 Erythromycin - instructions for medical use - RU No. LSR-009305/08 dated 2018-11-19 Erythromycin - instructions for medical use - RU No. LS-002688 dated 2017-11-08
Category ICD-10 Synonyms of diseases according to ICD-10
| A38 Scarlet fever | Pastia symptom |
| A41.9 Septicemia, unspecified | Bacterial septicemia |
| Severe bacterial infections | |
| Generalized infections | |
| Generalized systemic infections | |
| Generalized infections | |
| Wound sepsis | |
| Septic-toxic complications | |
| Septicopyemia | |
| Septicemia | |
| Septicemia/bacteremia | |
| Septic diseases | |
| Septic conditions | |
| Septic shock | |
| Septic condition | |
| Toxic-infectious shock | |
| Septic shock | |
| Endotoxin shock | |
| A49.0 Staphylococcal infection, unspecified | Staphylococcal infection |
| Staphylococcal infections | |
| A49.1 Streptococcal infection, unspecified | Poststreptococcal glomerulonephritis |
| Streptococcal infection | |
| A49.3 Mycoplasma infection, unspecified | Pulmonary infection caused by mycoplasma |
| Mycoplasma infection | |
| Mycoplasma infections | |
| Mycoplasma meningoencephalitis | |
| Mycoplasmosis | |
| Urogenital infection caused by mycoplasma | |
| Urogenital mycoplasmosis | |
| A71 Trachoma | Granular conjunctivitis |
| A74.0 Chlamydial conjunctivitis | Ocular chlamydial infection |
| Infectious conjunctivitis and keratoconjunctivitis caused by Chlamydia trachomatis | |
| Chlamydial eye infection | |
| Chlamydial eye diseases | |
| Chlamydial blepharoconjunctivitis | |
| Chlamydia of the organs of vision | |
| H00.0 Hordeolum and other deep inflammations of the eyelids | Meibomyitis |
| Meibomite | |
| Barley | |
| H01.0 Blepharitis | Blepharitis |
| Inflammation of the eyelids | |
| Inflammatory diseases of the eyelids | |
| Demodectic blepharitis | |
| Superficial bacterial eye infection | |
| Superficial eye infection | |
| Squamous blepharitis | |
| H10.5 Blepharoconjunctivitis | Blepharoconjunctivitis |
| Staphylococcal blepharoconjunctivitis | |
| Chronic blepharoconjunctivitis | |
| H10.9 Conjunctivitis, unspecified | Secondarily infected conjunctivitis |
| Hyperpapillary conjunctivitis | |
| Catarrhal conjunctivitis | |
| Year-round conjunctivitis | |
| Non-purulent conjunctivitis | |
| Non-purulent forms of conjunctivitis | |
| Non-purulent conjunctivitis | |
| Non-infectious conjunctivitis | |
| Subacute conjunctivitis | |
| Trachomal conjunctivitis | |
| H16 Keratitis | Adenoviral keratitis |
| Bacterial keratitis | |
| Spring keratitis | |
| Deep keratitis without epithelial damage | |
| Deep keratitis without damage to the epithelium | |
| Discoid keratitis | |
| Arborescent keratitis | |
| Keratitis rosacea | |
| Keratitis with corneal destruction | |
| Superficial keratitis | |
| Superficial punctate keratitis | |
| Punctate keratitis | |
| Traumatic keratitis | |
| J03.9 Acute tonsillitis, unspecified (angina agranulocytic) | Angina |
| Sore throat, alimentary-hemorrhagic | |
| Sore throat secondary | |
| Primary tonsillitis | |
| Sore throat follicular | |
| Sore throats | |
| Bacterial tonsillitis | |
| Inflammatory diseases of the tonsils | |
| Throat infections | |
| Catarrhal sore throat | |
| Lacunar tonsillitis | |
| Acute sore throat | |
| Acute tonsillitis | |
| Tonsillitis | |
| Acute tonsillitis | |
| Tonsillar tonsillitis | |
| Follicular tonsillitis | |
| Follicular tonsillitis | |
| J18 Pneumonia without specifying the pathogen | Alveolar pneumonia |
| Community-acquired pneumonia atypical | |
| Community-acquired pneumonia, non-pneumococcal | |
| Pneumonia | |
| Inflammation of the lower respiratory tract | |
| Inflammatory lung disease | |
| Lobar pneumonia | |
| Respiratory and lung infections | |
| Lower respiratory tract infections | |
| Cough due to inflammatory diseases of the lungs and bronchi | |
| Lobar pneumonia | |
| Lymphoid interstitial pneumonia | |
| Nosocomial pneumonia | |
| Exacerbation of chronic pneumonia | |
| Acute community-acquired pneumonia | |
| Acute pneumonia | |
| Focal pneumonia | |
| Pneumonia abscess | |
| Pneumonia bacterial | |
| Pneumonia lobar | |
| Pneumonia focal | |
| Pneumonia with difficulty in sputum discharge | |
| Pneumonia in patients with AIDS | |
| Pneumonia in children | |
| Septic pneumonia | |
| Chronic obstructive pneumonia | |
| Chronic pneumonia | |
| J47 Bronchiectasis [bronchiectasis] | Bronchiectasis |
| Bronchiectasis | |
| Bronchiectasis | |
| Infected bronchiectasis | |
| Panbronchiolitis | |
| Panbronchitis | |
| L08.0 Pyoderma | Atheroma festering |
| Pustular dermatoses | |
| Pustular skin lesions | |
| Purulent allergic dermatopathies | |
| Purulent skin infections | |
| Infected atheroma | |
| Mycoses complicated by secondary pyoderma | |
| Ostiofolliculitis | |
| Pyodermatitis | |
| Pyoderma | |
| Superficial pyoderma | |
| Staphylococcal sycosis | |
| Staphyloderma | |
| Streptoderma | |
| Streptostaphyloderma | |
| Chronic pyoderma | |
| P39.1 Conjunctivitis and dacryocystitis in the newborn | Conjunctivitis in newborns |
| P39.8 Other specified infection specific to the perinatal period | Blennorea in newborns |
| Nosocomial infections in newborns | |
| Neonatal herpes | |
| T79.3 Post-traumatic wound infection, not elsewhere classified | Inflammation after surgery and injury |
| Inflammation after injury | |
| Secondary infection of skin lesions and mucous membranes | |
| Deep wounds | |
| Purulent wound | |
| Purulent-necrotic phase of the wound process | |
| Purulent-septic diseases | |
| Purulent wounds | |
| Purulent wounds with deep cavities | |
| Small granulating wounds | |
| Disinfection of purulent wounds | |
| Wound infections | |
| Wound infections | |
| Wound infection | |
| Infected and non-healing wound | |
| Infected post-operative wound | |
| Infected wound | |
| Infected skin wounds | |
| Infected burns | |
| Infected wounds | |
| Festering post-operative wounds | |
| Extensive purulent-necrotic process of soft tissues | |
| Burn infection | |
| Burn infection | |
| Perioperative infection | |
| Poorly healing infected wound | |
| Postoperative and purulent-septic wound | |
| Postoperative wound infection | |
| Wound infection | |
| Wound botulism | |
| Wound infections | |
| Purulent wounds | |
| Infected wounds | |
| Reinfection of granulating wounds | |
| Post-traumatic sepsis |
The information provided on drug prices does not constitute an offer to sell or purchase goods. The information is intended solely for comparing prices in stationary pharmacies operating in accordance with Article 55 of the Federal Law “On the Circulation of Medicines” dated April 12, 2010 N 61-FZ.
Name of the drugPrice for 1 unitPrice per package, rub.Pharmacies
| Erythromycin tablets, enteric-soluble, film-coated, 250 mg, 10 pcs. polymer jar (jar) 10, cardboard pack 1 No. LSR-009305/08, 2008-11-24Biosintez JSC (Russia) | |
| 4.5 | 45.00 To the pharmacy |
| Erythromycin tablets, enteric-soluble, film-coated, 250 mg, 20 pcs. contour packaging 10, cardboard pack 2 No. LSR-009315/08, 2008-11-25AVVA-RUS OJSC (Russia) | |
| 4.95 | 99.00 To the pharmacy |
| Erythromycin lyophilisate for the preparation of solution for intravenous administration 100 mg, 1 pc. bottle, cardboard pack 1 No. P N000664/01, 2007-10-01 Sintez OJSC (Russia) | |
| 23 | 23.00 To the pharmacy |
| Erythromycin ointment for eyes 10000 IU/g, 1 pc. aluminum tube 10 g, cardboard pack 1 No. Р N002127/01, 2008-11-06 Sintez OJSC (Russia) | |
| 71profitable | 71.00 To the pharmacy |
| 72 | 72.00 To the pharmacy |
| 72 | 72.00 To the pharmacy |
| Erythromycin ointment for eyes 10000 IU/g, 1 pc. tube 10 g, cardboard pack 1 EAN code: 4604060203058, 4604060992822 No. LS-002421, 2011-08-01 Tatkhimpharmpreparaty OJSC (Russia) | |
| 72profitable | 72.00 To the pharmacy |
| 88 | 88.00 To the pharmacy |
| 94 | 94.00 To the pharmacy |
| Erythromycin ointment for external use 10000 U/g, 1 pc. aluminum tube 15 g, cardboard pack 1 No. LS-002688, 2011-07-12Biosintez JSC (Russia) | |
| 75.6 | 75.60 To the pharmacy |
| Erythromycin ointment for external use 10000 U/g, 1 pc. laminated tube 1 15 g, cardboard pack 1 No. Р N002127/02, 2008-10-13 Sintez OJSC (Russia) | |
| 84 | 84.00 To the pharmacy |
| Erythromycin ointment for eyes 10000 IU/g, 1 pc. laminated tube 10 g, cardboard pack 1 No. LS-002421, 2011-08-01 Tatkhimfarmpreparaty JSC (Russia) | |
| 88 | 88.00 To the pharmacy |
| Erythromycin ointment for external use 10000 U/g, 1 pc. tube 15 g, cardboard pack 1 No. LS-002688, 2011-07-12Biosintez PJSC (Russia) | |
| 102 | 102.00 To the pharmacy |
Source: https://www.rlsnet.ru/tn_index_id_3720.htm
Method of administration and dosage[ | ]
Orally (tablets, capsules, oral suspension, granules or powder for the preparation of oral suspension), intravenously (lyophilisate for the preparation of solution for injection), rectally (suppositories).
Intravenously[ | ]
Intravenously slowly (over 3-5 minutes) or drip. A single dose for adults and adolescents over 14 years of age is 0.25-0.5 g, a daily dose is 1-2 g. The interval between doses is 6 hours. For severe infections, the daily dose can be increased to 4 g (all doses are based on based on the basis). For intravenous jet administration, the drug is dissolved in water for injection or 0.9% NaCl solution at the rate of 5 mg per 1 ml of solvent. For intravenous drip administration, dissolve in 0.9% NaCl solution or 5% dextrose solution to a concentration of 1 mg/ml and administer at a rate of 60-80 drops/min. It is administered intravenously for 5-6 days (until a clear therapeutic effect occurs), followed by a transition to oral administration. If well tolerated and in the absence of phlebitis and periphlebitis, the course of intravenous administration can be extended to 2 weeks (no more).
Orally[ | ]
The regimen for taking the drug and eating is determined by the dosage form and its resistance to the effects of gastric juice. The average daily dose for adults is 1-2 g in 2-4 doses, the maximum daily dose is 4 g. Children from 4 months to 18 years, depending on age, body weight and severity of infection, 30-50 mg/kg/day . in 2-4 doses; children of the first 3 months of life - 20-40 mg/kg/day. In case of severe infections, the dose may be doubled.
For the treatment of diphtheria carriage - 0.25 g 2 times a day.
The course dose for the treatment of primary syphilis is 30-40 g, the duration of treatment is 10-15 days.
For amoebic dysentery, adults - 0.25 g 4 times a day, children - 30-50 mg/kg/day; Course duration is 10-14 days.
For legionellosis - 0.5-1 g 4 times a day for 14 days.
For gonorrhea - 0.5 g every 6 hours for 3 days, then 0.25 g every 6 hours for 7 days.
For gastroparesis - orally (for the treatment of gastroparesis, erythromycin for intravenous use is more preferable), 0.15-0.25 g per 30 minutes. before meals 3 times a day.
For preoperative bowel preparation to prevent infectious complications - orally, 1 g 19 hours, 18 hours and 9 hours before surgery (3 g in total).
For the prevention of streptococcal infection (for tonsillitis, pharyngitis) adults - 20-50 mg/kg/day, children - 20-30 mg/kg/day, course duration - at least 10 days.
For the prevention of septic endocarditis in patients with heart defects - 1 g for adults and 20 mg/kg for children, 1 hour before the treatment or diagnostic procedure, then 0.5 g for adults and 10 mg/kg for children, again after 6 hours.
For whooping cough - 40-50 mg/kg/day. within 5-14 days.
For conjunctivitis of newborns - 50 mg/kg/day. suspension in 4 doses for at least 2 weeks.
For pneumonia in children - 50 mg/kg/day. suspension in 4 doses for at least 3 weeks.
For genitourinary infections during pregnancy - 0.5 g 4 times a day for at least 7 days or (if this dose is poorly tolerated) 0.25 g 4 times a day for at least 14 days.
In adults, with uncomplicated chlamydia and intolerance to tetracyclines - 0.5 g 4 times a day for at least 7 days.
To improve this article it is desirable:
Please, after fixing the problem, remove it from the list of parameters. After eliminating all the shortcomings, this template can be deleted by any participant. |
Rectally[ | ]
Children aged 1 to 3 years - 0.4 g / day, from 3 to 6 years - 0.5-0.75 g / day, 6-8 years - up to 1 g / day. The daily dose is divided into 4-6 parts and administered every 4-6 hours.
Release form, composition and packaging of Erythromycin
The medicine is available in forms for oral, external and intravenous use.
| Dosage of erythromycin | Tara | Quantity | |
| Pills | 100, 200 milligrams, 250 mg, 500 mg | Coated tablets, white, in cells or bottles | 5, 10 pieces per cell. Plastic and dark glass bottles (10, 20 pieces) |
| Ointment | 1 % | Tuba | 15 grams |
| Eye ointment (sterile) | 1 % | Tuba | 10 grams |
| Lyophilisate for injection | 100 milligrams | Sealed bottle | 10 bottles per box |
| Granules for suspension | 200 milligrams per 5 milliliters | Bottle | Box with instructions |
Preparations containing erythromycin are produced by many Russian enterprises and may have other names.
Tyumen Chemical Pharmaceutical Plant, in particular, named its drug Erythromycin-Lect (250 milligram tablets).
Special instructions[ | ]
In severe forms of infectious diseases, when taking the drug orally is ineffective or impossible, resort to intravenous administration of a soluble form of erythromycin - erythromycin phosphate
.
Erythromycin suppositories are prescribed in cases where oral administration is difficult.
Due to the possibility of passage into breast milk, you should refrain from breastfeeding when prescribing erythromycin.
During long-term therapy, it is necessary to monitor laboratory parameters of liver function. Symptoms of cholestatic jaundice may develop within a few days of starting therapy, but the risk increases after 7 to 14 days of continuous therapy.
The likelihood of developing an ototoxic effect is higher in patients with renal and/or liver failure, as well as in elderly patients.
Some resistant strains of Haemophilus influenzae
sensitive to simultaneous administration of erythromycin and sulfonamides.
May interfere with the determination of catecholamines in urine and the activity of “liver” transaminases in the blood (colorimetric determination using definylhydrazine).
Do not drink milk or dairy products.
Medicines that increase the acidity of gastric juice and acidic drinks inactivate erythromycin (with the exception of enteric-coated tablets); erythromycin succinate
better absorbed when taken with food).
Newborns receiving erythromycin are at high risk of developing pyloric stenosis.
Numerous clinical studies have proven the antral and duodenal prokinetic effect of erythromycin.
Erythromycin during pregnancy: description of the drug
Erythromycin is an antibiotic that was discovered in 1952. It is one of the first representatives of macrolides and has a destructive effect on a relatively large number of pathogenic bacteria. The active substance of Erythromycin is erythromycin.
After entering the body, Erythromycin changes the interaction between amino acids, which leads to stopping the proliferation of bacteria. In this case, only a few gram-negative pathogens, viruses, and fungi can exhibit resistance.
Erythromycin is produced in the form of liquid for injection, ointment and tablets:
- The tablets contain 100 ml of erythromycin, as well as cellulose, sodium lauryl sulfate, magnesium stearate.
- The ointment for external use contains 0.01 g of erythromycin per 1 g of ointment. Among the auxiliary agents, the ointment contains paraffin and lanolin.
- Lyophilisate for intravenous injection contains 100 or 200 ml of erythromycin.
Interaction[ | ]
Reduces the bactericidal effect of beta-lactam antibiotics (penicillins, cephalosporins, carbapenems). Increases the concentration of theophylline. IV administration of erythromycin enhances the effect of ethanol (accelerating gastric emptying and reducing the duration of action of ethanol dehydrogenase in the gastric mucosa). Increases the nephrotoxicity of cyclosporine (especially in patients with concomitant renal failure). Reduces the clearance of triazolam and midazolam, and therefore may enhance the pharmacological effects of benzodiazepines. Slows down the elimination (increases the effect) of methylprednisolone, felodipine and coumarin anticoagulants. When co-administered with lovastatin, rhabdomyolysis increases. Increases the bioavailability of digoxin. Reduces the effectiveness of hormonal contraception. Drugs that block tubular secretion prolong the half-life of erythromycin. When taken simultaneously with drugs that are metabolized in the liver (carbamazepine, valproic acid, hexobarbital, phenytoin, alfentanil, disopyramide, lovastatin, bromocriptine), the concentration of these drugs in plasma may increase (it is an inhibitor of microsomal liver enzymes). When taken simultaneously with terfenadine or astemizole, arrhythmia may develop (ventricular fibrillation and flutter, ventricular tachycardia, even death), with dihydroergotamine or non-hydrogenated ergot alkaloids (ergotamine) - vasoconstriction to spasm, dysesthesia. Incompatible with lincomycin, clindamycin and chloramphenicol (antagonism).
Features of the use of Erythromycin during pregnancy
If a woman is prescribed Erythromycin, the following nuances must be taken into account:
- Before starting to take Erythromycin, hypersensitivity to macrolides should be excluded in a woman.
- The decision to prescribe Erythromycin is always supported by an analysis to determine the pathogen and its sensitivity to the antibiotic.
- During treatment, the woman's liver enzyme levels are regularly checked.
- If treatment is carried out with Erythromycin tablets, it is necessary to avoid the simultaneous use of drugs and dairy products.
Interaction with other drugs
Erythromycin can weaken the therapeutic effect of beta-lactam antibiotics (including penicillins and cephalosporins), so they are not prescribed at the same time.
Important
Drug antagonism is observed with Chloramphenicol and Lincomycin.
When used in parallel with antihistamines Astemizole and Terfenadine, heart rhythm disturbances may occur.
This drug potentiates the effect of benzodiazepines, the antianginal and diuretic drug Felodipine, the glucocorticoid Methylprednisolone and indirect anticoagulants (Warfarin and other coumarin derivatives). The bioavailability of the cardiac glycoside Digoxin increases.
Macrolide enhances the toxic effects of the immunosuppressant Cyclosporine.
In combination with the α-blocker dihydroergotamine, Erythromycin causes vasospasm.
Concurrent use of Lovastatin can lead to myopathy with the destruction of muscle cells - rhabdomyolysis.
The effectiveness of birth control pills decreases while taking Erythromycin.