Features of the disease
Ventricular fibrillation (VF) is characterized by chaotic contractions of myocardial tissue.
Their frequency increases from 250 to 480 per minute. The movements of the ventricles cease to be coordinated. As a result, blood circulation stops and the heart stops. The ECG produces irregular and chaotic waves that vary in width, height and shape. At the beginning of the attack they are high-amplitude. This is the so-called large-wave fibrillation. Afterwards, the waves become low-amplitude and their duration increases. At this stage, the effectiveness of defibrillation decreases.
https://www.youtube.com/watch?v=HxldipUjVdE
Often this condition occurs as a complication of extensive myocardial infarction.
Fibrillation is the leading cause of sudden death from heart problems.
About 75-80% of sudden deaths that are caused by cardiac problems occur due to VF. This disease occurs in both young and old people.
The risk group includes those patients who have suffered sudden circulatory arrest. Unexpected death affects 10-30% of such patients.
The chance of experiencing VF in people who suffer from idiopathic dilated cardiomyopathy is 10%. Within 1 year after a major heart attack, the disease affects 5% of patients. For hypertrophic cardiomyopathy – 3%.
Fibrillation is characterized by random contraction of the muscle fibers of the heart. The stages of development of the disease quickly replace each other: the patient feels weak, loses consciousness, and his pupils dilate. About 2 minutes pass from the onset of the attack to clinical death.
Classification of species
Experts distinguish 3 types of VF after heart attacks: primary, secondary and late. Although discussions regarding the classification of this disease are still ongoing.
Primary fibrillation occurs 1-2 days after a heart attack. It shows that the myocardium is characterized by electrical instability, which resulted from acute ischemia.
About 60% of primary VF occurs within 4 hours, 80% - 12 hours after a heart attack. Such fibrillation often leads to sudden death. With left ventricular failure and cardiogenic shock, secondary VF sometimes develops in people who have suffered a myocardial infarction.
If fibrillation began 48 hours after a heart attack, it is called late. About 40-60% of people who experience this disease die. In most cases, such fibrillation begins 2-6 weeks after a heart attack. More often it developed in those people whose anterior wall of the heart was damaged.
Doctors distinguish between 2 types of fibrillation. If the rhythm of contractions is correct, and their number does not exceed 200-300 per minute, then we are talking about ventricular flutter. With abnormal rhythm and contraction frequency from 200 to 500 per minute. talking about flickering.
In most cases, the cause of primary and other types of gastric fibrillation is a complication of myocardial infarction. Experts identify the following reasons for the development of VF:
- IHD of the heart (acute and post-infarction, coronary circulatory disorders);
- hypertrophic cardiomyopathy: death occurs in young people with excessive physical exertion;
- dilated idiopathic cardiomyopathy: fibrillation begins against the background of hemodynamic disorders in half of these patients;
- problems with the right ventricle (arrhythmogenic cardiomyopathy);
- different types of heart defects (the most common cause is aortic stenosis);
- specific cardiomyopathies;
- violation of the electrophysical characteristics of the myocardium.
The disease sometimes develops even in the absence of problems with the heart muscle. Risk factors that in some cases lead to ventricular fibrillation include:
- a sharp decrease in blood volume (this causes a drop in pressure and an increase in heart rate);
- severe poisoning (hypokalemia develops and cardiac excitability increases);
- hypothermia of the body;
- hormonal imbalance that arose due to pathologies of the thyroid gland;
- chronic stress or excessive nervous tension;
- overdose of drugs: diuretics or cardiac glycosides.
There are cases when the cause of ventricular fibrillation cannot be determined.
Symptoms and signs
You can suspect VF in a person based on characteristic signs:
- after 5 sec. the person becomes dizzy and weak;
- in 20 sec. the patient loses consciousness;
- after 40 sec. from the onset of the attack, the patient experiences characteristic convulsions: the skeletal muscles begin to contract once tonically, and at the same time defecation and urination occur involuntarily;
- after 45 sec. from the onset of ventricular fibrillation, the pupils dilate and reach their maximum size after 1.5 minutes.
The breathing of patients with ventricular fibrillation is noisy, frequent, and accompanied by wheezing. By the end of the second minute it becomes less frequent and clinical death occurs.
The patient sometimes has time to complain about:
- strong heartbeat;
- dizziness and weakness;
- heartache.
External signs include:
- pallor of the skin and mucous membranes;
- rapid breathing, shortness of breath;
- loss of consciousness;
- absence of pulsation in large arteries.
Doctors have 4 minutes to restore heart rhythm. If this cannot be done, then irreversible changes begin in the body.
Symptoms
Loss of consciousness
At the beginning of the clinical picture of ventricular fibrillation and flutter, the symptoms of the underlying disease may come first, which can subsequently lead to a complication - ventricular flutter or fibrillation. An attack of angina, myocardial infarction, or attacks of palpitations with short-term loss of consciousness may be the first harbingers of a deterioration in the condition. There are also times when, against the background of complete well-being during sports, sudden death occurs in young and healthy people.
At the time of an attack of flutter and fibrillation of the ventricles of the heart, the patient’s skin turns pale, subsequently acquiring a bluish tint (cyanotic). The brain experiences a lack of oxygen (hypoxia), as a result of which the patient loses consciousness. The pulse weakens until it disappears completely. Breathing becomes spontaneous and ineffective, and breathing movements of the chest may stop altogether.
Loss of consciousness may be accompanied by tonic convulsions. Brain hypoxia is also accompanied by weakened reflexes. Within 60 seconds from the onset of the attack, the pupils begin to dilate, and their reaction to light weakens. Involuntary urination and defecation are possible. The patient is in a state of clinical death. If assistance is not provided within 5 minutes, the patient's biological death occurs.
1What is ventricular fibrillation
Ineffective electrical activity of the heart
Ventricular fibrillation (VF) is an ineffective electrical activity of the heart, in which failure to provide emergency assistance within 5-7 minutes leads to the death of the patient, i.e. to biological death. A famous French clinician called this pathological phenomenon “delirium of the heart.” Muscle fibers contract chaotically, not obeying the pacemaker, which sends impulses for contraction.
The heart loses its role as a system and cannot perform its hemodynamic function. The myocardium and brain, as well as the entire body, do not receive nutrients and oxygen due to critical heart failure. If you look at the heart from the outside, it looks like a quivering, flickering organ.
How the heart flutters
Ventricular fibrillation
The ventricles are hollow muscular sacs that forcefully expel the blood coming to them from the atria into the great vessels. The right ventricle pumps blood in the pulmonary circulation - in the lungs, the left ventricle gives oxygen to the brain and the rest of the body. Working in parallel, the systemic and pulmonary circulation provide our body with the necessary supplies of oxygen and nutrients. In a healthy person, the ventricles contract at a frequency of 60-90 beats per minute. If there is a malfunction in their work, they begin to contract very often.
With ventricular flutter up to 300 beats per minute, with fibrillation up to 500 beats. Now imagine for a few seconds how, with such a contraction frequency, the ventricles can fill with blood? Absolutely right, at the indicated contraction frequency, the human heart cannot adequately provide the body with what it needs - oxygen. Within minutes, circulatory failure develops. In the absence of timely assistance, circulatory arrest occurs and the patient’s biological death occurs. In 90 percent of cases, ventricular fibrillation causes sudden cardiac death in people.
Prevalence, stages of development
The risk group includes those patients who have suffered sudden circulatory arrest. Unexpected death affects 10-30% of such patients.
The chance of experiencing VF in people who suffer from idiopathic dilated cardiomyopathy is 10%. Within 1 year after a major heart attack, the disease affects 5% of patients. For hypertrophic cardiomyopathy – 3%.
Ventricular fibrillation (flicker) is the disorganized electrical activity of the ventricular myocardium, which is based on the re-entry mechanism.
During VF, their full contractions stop, which is clinically manifested by cessation of blood circulation, accompanied by loss of consciousness, absence of pulsation and blood pressure in large arteries, absence of heart tones and breathing.
In this case, frequent (300 to 400 per minute), irregular, and without a clear configuration electrical oscillations with varying amplitude are recorded on the ECG.
In this case, ventricular contractions are ineffective and cardiac output is practically absent. With VT, the ECG shows regular flutter waves of the same shape and amplitude, reminiscent of a sinusoidal curve. VT is an unstable rhythm that quickly turns into fibrillation, and occasionally into sinus rhythm.
- VF is the leading cause of sudden cardiac death.
- Etiology of ventricular fibrillation (flickering)
- The following diseases and pathologies may be the reasons for the development of VF. states:
IHD. First of all, the cause of the development of VF is an acute violation of the coronary circulation, acute and post-MI.
With hypertrophic cardiomyopathy, sudden cardiac death most often occurs in young people during intense physical activity.
Dilated cardiomyopathy. Sudden death usually occurs against the background of expression. hemodynamic disorders in half of patients with dilated cardiomyopathy.
Channelopathies are the following pathological syndromes: Brugada syndrome, arrhythmogenic dysplasia (cardiomyopathy) of the right ventricle, long QT syndrome), Wolff-Parkinson-White syndrome (WPW).
The “precursor” of VF in Brugada syndrome and long QT syndrome is most often ventricular tachycardia of the “pirouette” type; in arrhythmogenic dysplasia of the right ventricle – monomorphic ventricular tachycardia.
tachycardia, with WPW syndrome – polymorph. gastric tachycardia.
Among valvular heart defects, the occurrence of VF and sudden cardiac death most often results from aortic stenosis. In patients with mitral valve prolapse, VF occurs extremely rarely and is associated with nar. electrophysiological properties of the myocardium.
Specific cardiomyopathies leading to VF and sudden cardiac death primarily include inflammatory cardiomyopathies. character, especially with sarcoidosis.
- More rare causes of ventricular fibrillation:
- Intoxication with cardiac glycosides (strophanthin K).
- Electrolyte disturbances.
- Electric shock.
- Hypothermia.
- Hypoxia and acidosis.
- Coronary angiography, cardioversion.
- Side effects when taking certain medications: sympathomimetics (epinephrine, orciprenaline, salbutamol), barbiturates, anesthetics (cyclopropane, chloroform), narcotic analgesics, TAD, phenothiazine derivatives (chlorpromazine, levomepromazine), amiodarone, sotalol, class I antiarrhythmic drugs ( most often - against the background of “pirouette” tachycardia due to QT prolongation).
- Diagnosis of flutter and ventricular fibrillation
- Diagnosis of flutter and VF is based on ECG data and clinical manifestations.
ECG signs of VF: Frequent (300–400 per min), but irregular random waves, differing from each other in different shapes and amplitudes. Large and small wave VF are distinguished. With the latter, the amplitude of the flicker waves is less than 0.2 mV and the likelihood of successful defibrillation is much lower.
ECG signs of TG: Frequent (200–300 per min) regular flutter waves of the same shape and amplitude, reminiscent of a sinusoidal curve.
In VF, clinical death always occurs suddenly, simultaneously; its onset is accompanied by a characteristic single tonic contraction of skeletal muscles.
Although agonal breathing may persist during the first 1-2 minutes of sudden cessation of cardiac activity, an early sign of this condition is the absence of pulsation in the large arteries and, less reliably, of heart sounds. Cyanosis develops quickly and the pupils dilate.
ECG registration allows you to confirm diagnoses and establish the immediate cause of sudden cardiac arrest (fibrillation, ventricular asystole, electromechanical dissociation).
- Treatment
- For TG and VF, emergency care boils down to immediate defibrillation
- If a defibrillator is not available, a single precordial shock should be applied.
- If it was not possible to restore sinus rhythm, then it is necessary to immediately begin chest compressions and artificial ventilation (ALV).
- Therapeutic measures after cardiopulmonary resuscitation
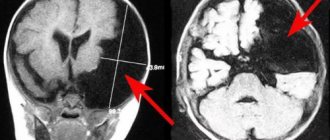
After successful resuscitation, patients usually remain for a more or less long time with hemodynamic instability, inadequate gas exchange and the phenomena of anoxic encephalopathy, so they must be hospitalized in a block or department of intensive observation and treatment. In the intensive care unit, oxygen therapy and peripheral vein catheterization are indicated.
In cases of short resuscitation after a short period of VF, spontaneous breathing of oxygen in high concentrations under the control of pulse oximetry data is usually sufficient to correct hypoxemia.
In this case, hemoglobin oxygen saturation should be at least 95%. Inadequate spontaneous ventilation and acidosis increase the risk of recurrent cardiac arrest and contribute to secondary brain damage.
Therefore, tracheal intubation and mechanical ventilation are indicated for such patients.
Common post-resuscitation complications are various heart rhythm disturbances. For its prevention, it is important to control the level of K in the blood plasma, which should be maintained within 4-4.5 mmol/l.
Correction of acidosis begins with ensuring adequate ventilation of the lungs and hemodynamics, resorting to the administration of sodium bicarbonate only if these measures are insufficiently effective. Taking into account the negative impact of post-resuscitation hyperglycemia, the neurological status is corrected with simple insulin according to indications.
- Treatment of VF in the acute stage of myocardial infarction and after reperfusion
- There are several types of VF depending on the time of its occurrence from the onset of MI, the severity of existing structural changes in the myocardium and the severity of hemodynamics, as well as depending on the prognosis for life.
- There are early VF, which occurs in the first 24–48 hours from the onset of myocardial infarction, and late VF, which develops after 48 hours from the onset of the disease.
- In addition, a distinction is made between primary and secondary fibrillation.
Primary VF occurs in patients without signs of cardiogenic shock or severe HF, its appearance is explained by electrical instability in the area of ischemic or necrotic myocardium. Primary VF is not prognostically unfavorable and does not significantly affect long-term survival.
Secondary fibrillation, which develops in the presence of severe organic myocardial lesions or against the background of cardiogenic shock or acute left ventricular failure, has a poor prognosis.
Regardless of whether VF developed as a result of myocardial reperfusion or due to ongoing ischemia, the only effective way to eliminate it is electrical cardioversion according to the algorithm described above. From pharma. drugs can be used intravenously 1 mg Adrenaline.
- In cases of VF that are resistant to applied electrical discharges, intravenous amiodarone can be used to increase the likelihood of success of resuscitation measures and the effectiveness of cardioversion.
- Intravenous infusion of antiarrhythmic drugs continues from 48 hours to several days until there is confidence in the absence of relapses of VF.
- When VF episodes recur, in addition to continuing antiarrhythmic therapy (usually with amiodarone), correcting acid-base and electrolyte balances, use the maximum possible doses of β-blockers, resort to implantation of dual-chamber pacemakers, cardioverter-defibrillators, and perform myocardial revascularization procedures (percutaneous coronary interventions, coronary shunting).
Reasons of the heart
Development factors are not always cardiogenic as it might seem. Approximately 40-45% of cases are due to non-cardiac causes, but it’s still worth starting with the first ones.
- Myocardial inflammation. It has a viral or bacterial origin in most clinical situations. Autoimmune is noticeably less common, against the background of current rheumatism and other pathological processes. It is treated strictly in a hospital.
Changes that occur against the background of this condition cannot be adequately restored after the fact. Radical measures will be required for prosthetics or implantation of a defibrillator to correct the rhythm.
- Scarring of the myocardium (cardiosclerosis) as a result of coronary insufficiency and other conditions. This is an irreversible phenomenon. It requires mandatory maintenance treatment. Most likely, throughout your entire life.
- Cardiomyopathy. Regardless of the form and stage of development. Dilated and hypertrophic give approximately equal chances of developing ventricular fibrillation. The more pronounced the organic changes in the heart, the more significant the functional disorders.
Patients with considerable experience in the absence of medical care practically cannot count on a favorable outcome. Transplantation has some acceptable clinical significance, but it is difficult, expensive and unrealistic even in developed countries.
- Heart defects, congenital and acquired. First of all, stenosis of the mitral valve or aorta, then other conditions, such as aneurysm or septal disorder.
Recovery is carried out urgently using surgical methods. If the volume of regurgitation (reverse blood flow) is not yet fatal and there is no fibrillation yet, it makes sense to conduct dynamic monitoring.
No one will dare to operate on a patient without sufficient grounds. Not counting emergency cases.
- Block of the bundle branches (right or left) or the entire atrioventricular node (AV block). The signal cannot pass to the ventricles; against the background of total obstruction, an urgent operation to implant a defibrillator is indicated. Even this is not a guarantee of a favorable outcome. Although the chances of survival are significantly increased.
- Cardiomelagia. Also called bull's heart. The essence of the pathology lies in the proliferation of organ structures. Recovery is impossible, treatment is supportive. Drug therapy does not have much clinical significance.
- Coronary insufficiency. There are two types: angina or heart attack. In this case we are talking about the first option. Its essence lies in changing the lumen of the corresponding artery with the impossibility of providing the muscle layer with nutritional compounds.
In this case, the process does not reach a certain critical point. That is, there is supply, but it is insufficient. Angina pectoris occurs in attacks, each such episode leads to necrosis of part of the cardiac structures, the probability of stable fibrillation is constantly growing.
Read more about the causes of angina attacks, first aid measures and treatment here.
- Heart attack. Occurs as a result of acute malnutrition of the myocardium. It is determined by extensive areas of cardiac damage. Restoration is not possible. Lifelong maintenance therapy is required. The effect and prognosis depend on the area of the lesion.
2Reasons
Coronary heart disease
What can trigger such a formidable rhythm disorder as ventricular fibrillation? Quite often, fibrillation is preceded by ventricular flutter, and subsequently the resulting VF, in the absence of resuscitative care, turns into ventricular asystole (complete absence of contractions). Not one or two, but a whole series of diseases, if untreated or as a result of complications arising from them, can lead to the development of ventricular fibrillation. This list includes both heart diseases and pathologies of other organs and systems:
- Cardiac causes: coronary heart disease, myocardial infarction, cardiomyopathy, ventricular tachycardia, ventricular extrasystoles, SVC syndrome (Wolf-Parkinson-White), myocardial inflammation (myocarditis), Brugada syndrome, long QT syndrome, valve defects (stenosis and insufficiency of the aortic valve) and etc.
- Non-cardiac causes: hypothermia, sarcoidosis, diphtheria, renal and liver failure, overdose of certain medications, cardioversion, etc.
Sudden death due to VF can occur not only in sick people, but also in healthy patients and athletes.
Causes
Ventricular fibrillation and flutter can occur as a consequence of other heart rhythm disturbances, as well as for “non-arrhythmic” reasons.
The development of such a severe complication may be a consequence of recurrent stable or unstable ventricular tachycardia, frequent polymorphic and polytopic ventricular extrasystoles. Bidirectional ventricular tachycardia with long QT syndrome, paroxysmal fibrillation or atrial flutter against the background of Wolff-Parkinson-White syndrome can transform into such a disorder. Ventricular fibrillation and flutter can occur as a side effect of cardiac glycosides and some antiarrhythmic drugs. In this case, arrhythmia develops against the background of electrical instability of the myocardium.
In 25% of cases, the development of ventricular fibrillation and flutter is not preceded by ventricular arrhythmias. These conditions can develop during acute coronary insufficiency, including myocardial infarction. It is believed that undiagnosed atherosclerosis of the main coronary arteries is one of the most common causes of flutter and ventricular fibrillation.
These pathologies are often found in patients with left ventricular enlargement due to various reasons (aortic stenosis, cardiomyopathies). Complete atrioventricular and nonspecific intraventricular block also predispose to the development of these arrhythmias. Other causes may be electrical trauma, hypokalemia, severe emotional stress, accompanied by intense release of adrenaline and other catecholamines. Anesthetic overdose, coronary angiography and hypothermia during cardiac surgery can also cause such severe complications.
Often the development of such rhythm disturbances is preceded by sinus tachycardia in combination with the release of adrenaline. Therefore, ventricular flutter and fibrillation are one of the main causes of sudden death in young people, particularly during sports.
3Diagnostics
Ventricular fibrillation on ECG
The electrocardiographic picture of ventricular fibrillation has characteristic features that distinguish it from other rhythm disorders - atrial fibrillation (AF), ventricular flutter, etc. Let's touch on the main points and ECG characteristics of ventricular fibrillation.
- Rhythm. In VF, despite the work of the pacemaker, the myocardium as a whole is not able to obey it, so each fiber is excited chaotically. Therefore, unlike a normal ECG, the rhythm is not sinus and is irregular.
- Heart rate. As mentioned above, there are no effective cardiac contractions of the myocardium. Only flickering waves of contraction of individual fibers can be traced. On an ECG, the frequency of such waves reaches 500-700 per minute.
- Absence of ventricular complexes. Ventricular complexes (qrs complexes) are not visualized, as is the case with atrial flutter on the ECG. Only waves are visible, which initially have a height of up to 5 mm, and then gradually decrease, eventually turning into a horizontal isoelectric line (asystole, cardiac arrest).
ECG signs of ventricular flutter and fibrillation (fibrillation) and their diagnostic value
ECG signs of atrial fibrillation and its diagnostic value.
Atrial flutter and its diagnostic significance.
Atrial flutter is a significant increase in atrial contractions (up to 200-400 per minute) while maintaining the correct regular atrial rhythm.
This disorder is observed at a young age in patients:
- with mitral heart defects. In elderly and senile patients, atrial flutter occurs when:
— coronary heart disease;
- acute myocardial infarction.
- the presence on the ECG, instead of the P wave, of frequent (up to 200-400 per minute) regular atrial waves f, having a sawtooth shape (in II, III, aVF, V1, V2 leads);
- correct regular ventricular rhythm (correct form of atrial flutter) with equal RR intervals or irregular ventricular rhythm (correct form of atrial flutter) with unequal RR intervals,
— the ventricular complex is not changed;
- each ventricular complex is preceded by a certain (usually constant) number of atrial waves (2:1; 3:1; 4:1, etc.).
Atrial fibrillation, or atrial fibrillation, is a heart rhythm disorder in which frequent (from 350 to 700 per minute), erratic excitation and contraction of individual groups of atrial muscle fibers is observed.
Atrial fibrillation is observed when:
— coronary heart disease;
- the presence on the ECG, instead of the P wave, of f waves having different shapes and amplitudes, best recorded in leads V1, V2, III, aVF;
— the ventricular complex is not changed;
- ventricular rhythm is incorrect (RR intervals vary in duration).
Ventricular flutter is a frequent (up to 200-300 per minute) rhythmic excitation, which, as a rule, turns into flickering (fibrillation), characterized not only by frequent (up to 200-500 per minute), but also by chaotic irregular excitation and contraction of individual muscle fibers of the ventricles.
Ventricular flutter and fibrillation are a common cause of sudden death in patients with:
— acute myocardial infarction;
— coronary heart disease;
- aortic heart defects.
As a result of chaotic contraction of individual muscle fibers of the ventricles, asystole and circulatory arrest occur.
- with ventricular flutter, frequent (up to 200-300 per minute), regular and identical in shape and amplitude waves, reminiscent of a sinusoidal curve;
- with ventricular fibrillation, frequent (from 200 to 500 per minute), irregular waves, differing from each other in shape and amplitude.
93.79.221.197 © studopedia.ru Not the author of the materials posted. But it provides the opportunity to use it for free. Is there a copyright violation? Write to us | Feedback.
Disable adBlock! and refresh the page (F5)
very necessary
4Forecast
First aid for ventricular fibrillation
Ventricular fibrillation is a fatal rhythm disorder, which in the absence of resuscitation measures inevitably leads to the death of the patient. Together with ventricular tachycardia, VF accounts for ninety-five percent of the causes of sudden death. About 30 percent of patients who experience VF die within a year.
Question 98. Ventricular fibrillation and flutter, causes, diagnosis, emergency therapy
Experts determine ventricular fibrillation by external signs. If the doctor is near the patient during the onset of the attack, he will diagnose:
- increased heart rate;
- lack of rhythm;
- difference between heart rate and pulse;
- no difference between I and II heart sounds;
- wheezing in the lungs.
Competent resuscitation measures can save a person. If the attack occurred outside the hospital, you must call an ambulance. A person’s complaints, sudden fainting and characteristic convulsions can be used to suspect VF.
Before doctors arrive, it is recommended to do the following:
- Make sure that a state of clinical death has occurred.
- It is necessary to “start” the heart: in the absence of a defibrillator, a sharp blow is given to the sternum.
- In cases where the heartbeat is not restored, artificial respiration and cardiac massage begin. If resuscitation is carried out by 1 person, then for 2 insufflations he makes 15 rhythmic pressures on the sternum.
Symptoms and diagnostic methods
As noted above, ventricular fibrillation occurs in the same way as complete cardiac arrest, so the symptoms will be similar to those with asystole:
- In the very first minutes, loss of consciousness occurs;
- Spontaneous breathing and heartbeat cannot be detected, it is impossible to feel the pulse, severe hypotension;
- Widespread bluish discoloration of the skin;
- Dilation of the pupils and loss of their reaction to a light stimulus;
- Severe hypoxia can cause convulsive syndrome, spontaneous emptying of the bladder and rectum.
Ventricular fibrillation takes the patient by surprise; it is impossible to predict the time of its occurrence even in the presence of obvious predisposing factors on the part of the heart. Due to the complete cessation of blood flow, within a quarter of an hour the victim loses consciousness; by the end of the first minute from the beginning of the fibrillation paroxysm, tonic convulsions occur and the pupils begin to dilate.
By the second minute, spontaneous breathing, pulse and heartbeat disappear, blood pressure cannot be determined, the skin becomes bluish, swelling of the neck veins, and puffiness of the face are noticeable.
These signs of ventricular fibrillation characterize a state of clinical death, when changes in organs are reversible and the patient can still be revived.
By the end of the first five minutes of arrhythmia, irreversible processes begin in the central nervous system, which ultimately predetermine an unfavorable outcome: clinical death turns into biological death in the absence of resuscitation measures.
Clinical signs of cardiac arrest and sudden death may indirectly indicate the likelihood of ventricular fibrillation, but this condition can only be confirmed using additional diagnostic methods, the main one of which is electrocardiography.
The advantages of an ECG are the speed of obtaining results and the possibility of performing it outside a medical institution, therefore a cardiograph is a mandatory attribute not only for intensive care units, but also for line ambulance teams.
Ventricular fibrillation on an ECG is usually easily recognized by a doctor of any specialty and an emergency paramedic by characteristic signs:
- Absence of ventricular complexes and any teeth, intervals, etc.;
- Registration of so-called fibrillation waves with an intensity of 300-400 per minute, irregular, varying in duration and amplitude;
- No isoline.
Depending on the magnitude of the waves of random contractions, large-wave ventricular fibrillation is distinguished when the force of contractions exceeds 0.5 cm when recording an ECG (the height of the waves is more than one cell). This type characterizes the onset of arrhythmia and the first minutes of its course.
As cardiomyocytes deplete, acidosis and metabolic disorders increase, the large-wave type of arrhythmia turns into small-wave ventricular fibrillation, which, accordingly, characterizes a worse prognosis and a greater likelihood of asystole and death.
The concept of atrial flutter implies a significant increase in heart rate, when the number of beats reaches 200-400 per minute, but the working rhythm itself remains normal.
Treatment tactics
In the hospital, all actions are aimed at restoring the heart rhythm. These measures are called cardioversion. Doctors perform chest compressions and artificial ventilation. Insufflation of air allows you to provide the body with oxygen.
Electropulse therapy gives good results. The sooner it is carried out, the higher the patient’s chances of survival.
Some argue that after 3 ineffective defibrillator shocks, the patient should be intubated and put on artificial respiration.
VF is continued to be treated with sodium bicarbonate. Injections are given every 10 minutes until blood circulation is restored.
They increase the effectiveness of electrical pulse therapy by intracardiac administration of the drug “Adrenaline hydrochloride”. But such injections are fraught with complications.
For drug stimulation of the myocardium, “Norepinephrine” and “Mezaton” are used.
If defibrillation is ineffective, then in addition to Adrenaline hydrochloride, Anaprilin, Novocainamide, and Lidocaine are administered. The patient continues to undergo cardiac massage and artificial respiration, defibrillation is repeated after 2 minutes.
In cases where the heart stops after electrical pulse therapy, the drugs “Calcium chloride” and “Sodium lactate” are administered.
Resuscitation measures are carried out until the heart rhythm is restored or signs appear that the brain has begun to die.
Emergency care for VF
When ventricular fibrillation develops, there is a very high probability of death within a few minutes. Therefore, the patient’s life prognosis completely depends on how quickly and competently emergency care is provided at the prehospital stage. Unfortunately, it is impossible to hope that the heart rate will recover on its own.
The first and most effective means of restoring rhythm is defibrillation. This is an electric shock with a force of 200 J. The manipulation is performed only by a professional resuscitation team.
Defibrillation
If this is not possible, doctors perform a precordial blow - a quick and sharp blow to the chest area. Sometimes a precordial stroke stops fibrillation.
If necessary, cardiopulmonary resuscitation is performed.
Algorithm:
- The patient is placed on a flat surface, the head is tilted back, the lower jaw is extended so as to ensure unimpeded flow of air to the lungs.
- Perform 12 breaths per minute using the mouth-to-mouth method.
- If there is no pulse, an indirect cardiac massage is performed. Frequency – 100 chest compressions per minute.
- The frequency of pressures and breaths is as follows: if one person is resuscitating, 2 breaths are given for every 15 pressures. If resuscitation is carried out by two people, inhale every 5 pressures.
The result of resuscitation measures and defibrillation is assessed using ECG. The current can be increased to 360 J per minute. If necessary, injections of adrenaline are performed directly into the heart muscle, the patient is intubated, and connected to a ventilator. All this is possible only in a hospital.
Interestingly, even with well-organized care, the survival rate of patients with VF is only 20%. Moreover, in 90% of cases the rhythm is restored in the first minute of the intervention, and by the fourth minute of resuscitation the figure drops to 30%.
Rehabilitation
After ventricular fibrillation, the patient is monitored.
His condition is constantly monitored using a Holter ECG: this is done continuously for 1-7 days.
Treatment is aimed at preventing recurrence of attacks.
If patients experience fibrillation due to heart disease, then surgical intervention is performed. Surgeons can install a device that will correct the myocardial rhythm.
The radiofrequency ablation method is also used - this is the introduction of a special device that destroys the pathological focus of abnormal heart rhythm.
Drug antiarrhythmic therapy is also carried out. To prevent possible complications, anticoagulants are prescribed. They prevent increased blood clotting and reduce the likelihood of developing a heart attack. They also recommend products that improve metabolism and nourish muscles.
Classification
Ventricular fibrillation is usually divided into 3 stages - primary, secondary and late. Primary fibrillation occurs 1-2 days after myocardial infarction. Electrical instability of cardiomyocytes is explained by acute ischemia. More than half of the cases of primary fibrillation are observed in the first 4 hours, 40% - within 12 hours after a heart attack, which is the main cause of mortality in patients with this pathology.
Read also: Cardialgia syndrome
Secondary fibrillation develops due to lack of blood circulation in the left ventricle and is accompanied by cardiogenic shock. This stage is difficult to eliminate by defibrillation, while the primary stage passes after a single electrical impulse. Late fibrillation is observed 48 hours after myocardial infarction or at the 5-6th week of heart disease related to ventricular dysfunction. At this stage, the mortality rate is 40–60%.
Arrhythmia is characterized by symptoms identical to complete cardiac arrest (asystole). Signs of ventricular fibrillation:
- heart rhythm disturbance;
- weakness, dizziness;
- sudden loss of consciousness;
- frequent breathing or lack thereof, wheezing;
- pallor of the skin and mucous membranes;
- cyanosis (blueness of the tips of the ears, nasolabial triangle);
- pain in the heart, cardiac arrest;
- absence of pulse in large arteries (carotid, femoral);
- dilated pupils;
- complete relaxation or convulsions;
- involuntary emptying of the bladder and bowels.
Arrhythmia begins suddenly, its appearance cannot be predicted. Signs of fibrillation determine the state of clinical death, when changes in the body are still reversible and the patient can survive. After 7 minutes of arrhythmia, oxygen starvation leads to irreversible damage to the cerebral cortex and the process of cell disintegration begins, i.e. biological death.
Possible consequences and prognosis
In most cases, complications occur after VF. The prognosis will be better in cases where assistance is provided in the first seconds of an attack. But it is difficult to avoid the negative consequences of this condition.
When the heart stops, total myocardial ischemia occurs. After blood circulation is restored, dysfunction of the heart muscle appears.
The following complications may also develop:
- the appearance of arrhythmia;
- lung problems: aspiration pneumonia, tissue damage due to rib fractures;
- neurological problems (arise due to a temporary deterioration in blood circulation in the brain tissue);
- thromboembolism: blockage of blood vessels by blood clots.
When carrying out defibrillation in the first 6 minutes and other resuscitation measures in the first 3 minutes, the probability of survival is 70%. If more than 12 minutes have passed since the onset of the attack, then less than 20% of patients remain alive.
Anatomical causes
It is important to consider the causes of ventricular fibrillation. As mentioned above, this phenomenon is preceded by fluttering. If both processes are ignored, the person will experience ventricular asystole. This is a pathology in which contraction does not occur. In this case, it will be difficult to help the patient in any way. With fibrillation, blood is not pumped. This leads to a decrease in pressure, the brain begins to starve and die. In order to prevent such a situation, you need to know exactly the reasons for its occurrence.
To find out the factors that provoke ventricular fibrillation and flutter, it is necessary to pay attention to the anatomy of the heart itself. It has four cameras. We are talking about two ventricles and two atria. Due to the impulses sent by the brain, the heart works rhythmically and provides the blood circulation necessary for life. As soon as the signals are disrupted or the way they are perceived changes, a person experiences a malfunction. For fibrillation to appear, it is necessary that the impulse, instead of its usual path from the brain to the heart, begins to move in a circular motion. Because of this, the myocardium contracts randomly. At this moment the muscle does not relax. Within a few minutes it completely stops working correctly.