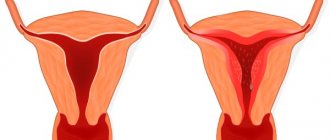
Endometrial hyperplasia is a disease in which the inner layer of the uterus (endometrium) grows. It occurs in women of all ages; simple (glandular), glandular-cystic and adenomatous hyperplasia are distinguished, as well as with or without signs of atypia. The main symptom of the pathology is heavy periods. Complications include chronic anemia and infertility.
Hyperplasia can be cured forever, but more often the disease recurs, since it is difficult to eliminate all the risk factors that predispose to the disease. Diagnosis is carried out using ultrasound, hysteroscopy, and endometrial biopsy. Treatment is usually hormonal; there are also various folk recipes for hyperplasia.
Endometrial hyperplasia: main characteristics
The endometrium is the inner layer of the uterus; due to various circumstances, its excessive growth may occur in a specific area or diffusely over the entire area, which is called hyperplasia (HE). The danger of the pathology lies in the fact that uncontrolled cell growth can lead to various “breakdowns”, which can lead to the development of a malignant tumor—uterine cancer.
In addition, endometrial hyperplasia is accompanied by the following unpleasant consequences for a woman’s health:
- heavy periods;
- pain during menstruation;
- there is a higher risk of retrograde reflux of blood into the abdominal cavity and, as a result, a greater likelihood of infection spreading from the lower genital organs to the upper (appendages), this also increases the risk of endometriosis;
- infertility.
Endometrial hyperplasia during pregnancy
GPE is usually the cause of infertility. This occurs due to deformation of the surface of the uterus, on which the embryo is not able to fixate. As for the development of the disease during pregnancy, the possibility is excluded. The presence of such a diagnosis may mean that hyperplasia was present earlier, but despite its presence, pregnancy occurred. Such cases are rare, but do occur in medical practice.
GPE during pregnancy is fraught with complications, so the woman should be under the supervision of a gynecologist who will monitor the development and condition of the embryo. No treatment can be carried out before birth. To minimize the likelihood of spontaneous abortion, the patient may be prescribed hormone therapy.
Relationship with menstruation
Under the influence of estrogens, in the first phase of the menstrual cycle, the endometrium grows - it thickens. Starting from the middle of the cycle, the level of another sex steroid, progesterone, increases. It is responsible for a special transformation of the endometrium - differentiation of its cells, which subsequently leads to its rejection (if pregnancy does not occur).
Normally, during menstruation, the functional layer of the endometrium is rejected, which is manifested by bloody discharge in a woman. With endometrial hyperplasia, as a rule, the cycle is disrupted, high values of estrogen and low progesterone are observed.
As a result, the endometrium grows, but is not rejected (desquamated). This can only happen locally (in certain areas), but subsequently the process affects the entire surface of the inner layer of the uterus. After some time, the endometrium is still rejected - menstruation occurs, usually heavy.
This is repeated from cycle to cycle - some areas of the pathological endometrium may not even undergo desquamation, which leads to the formation of polyps.
We recommend reading about the treatment of endometrial hyperplasia after curettage. From the article you will learn about when you need to do curettage, the technique of curettage, its consequences and the recovery period. And here is more information about the diagnosis and treatment of endometrial polyp in the uterus.
Structure of the endometrium of the uterus
The uterine mucosa is a complex multi-structural system consisting of integumentary and glandular epithelium, stroma and blood vessels. The endometrium is the inner layer of mucous lining the uterus. Morphologically, it is divided into two sections: basal (main) and functional, which, if pregnancy does not occur, is rejected and excreted from the body. The functional layer under the influence of estrogens and progesterone undergoes significant structural and functional changes.
Normally, immediately after menstruation, when the endothelial layer has been shed, the process of endometrial regeneration begins. Cells multiply and divide, and the thickness of the layer increases. This process is called physiological hypertrophy.
If the menstrual cycle is disrupted, the proliferation of endometrial cells continues, the layer thickens significantly, which leads to an increase in the volume of the uterus. The structure of the endometrium becomes denser, the surface becomes heterogeneous, which prevents the implantation of the embryo into the uterine wall.
Disease statistics
Endometrial hyperplasia ranks second in frequency among gynecological diseases of non-infectious nature. It is more common in women of premenopausal age (up to 80% of all episodes of disease) due to changes in hormonal levels, the presence of excess body weight in the majority and previous diseases of both the genital area and other systems and organs.
There are no exact statistics on endometrial hyperplasia, since strict reporting is not carried out on the pathology, such as, for example, on cancer. It is believed that every fifth to seventh woman under 40 years of age and every third woman with the onset of menopause have to deal with GE.
The risk of developing endometrial hyperplasia is higher in the following groups of women:
with various endocrinological diseases and hormonal disorders - diabetes mellitus, thyroid pathology, polycystic disease, ovarian dysfunction, etc.;
- smokers;
- with excess weight – adipose tissue is a source of estrogen, which leads to hormone imbalance, and this is the basis for the development of endometrial hyperplasia;
- complicated course of childbirth and the postpartum period;
- sexually transmitted infections, endometritis and inflammatory diseases of the pelvic organs in general;
- liver diseases - estrogen transformation occurs in this organ; when the organ’s functioning is disrupted, the level of the hormone increases.
Preventive actions
It is quite possible to prevent the development of endometrial hyperplasia. Women should follow the following recommendations from doctors:
- exclude artificial termination of pregnancy unless there are categorical medical indications;
- undergo preventive examinations with a gynecologist at least once every six months;
- timely and complete treatment of any pathologies of the reproductive system (inflammatory and infectious etiology);
- preventing obesity;
- blood pressure control.
Endometrial hyperplasia is a rather dangerous disease that medicine can treat quite successfully. It is important to seek qualified medical help in a timely manner and strictly follow the gynecologist’s instructions.
Betsik Yulia, obstetrician-gynecologist
4, total, today
( 50 votes, average: 4.36 out of 5)
Uterine fibroids: causes, symptoms, risks and treatment
Necrosis of myomatous node: symptoms and treatment
Related Posts
Differences from endometriosis
Hyperplasia can develop against the background of endometriosis; this is facilitated by changes in tissues during the disease. However, these are completely different diseases. Endometriosis is associated with the appearance of ectopic foci of the endometrium in places where it should not normally be. For example, in the thickness of the uterine wall, on the ovaries, peritoneum, etc.
Endometriosis is often accompanied by an imbalance of sex hormones, which in itself leads to development and hyperplasia. The main differences and similarities between the two diseases are presented in the table below.
| Signs | Endometrial hyperplasia | Endometriosis |
| Cause | Imbalance of sex hormones, chronic inflammation of the endometrium | Not fully known, more inclined to immunological disruptions in the body |
| At what age does it happen more often? | After 35-40 years | In young girls |
| Main features | Heavy periods | Pain |
| Diagnostics | Ultrasound, curettage of the uterine cavity | Ultrasound, curettage of the uterine cavity |
| Does it turn into cancer? | There is a possibility, especially if the hyperplasia is atypical | No |
| Treatment | Hormonal, surgical | |
Modern classification
The uterus undergoes changes every month. The mucous membrane grows and is renewed. If the egg has not been fertilized, then menstruation occurs and the mucous membrane returns to its original size. In place of the endometrium that has come out, a new layer is formed and this happens every month.
Endometrial hyperplasia has the following classification:
- glandular
- glandular-cystic
- focal (polyps)
- atypical
Judging by the name, it is possible to differentiate the subtypes of hyperplasia. Atypical is a precancerous condition; in 10% of cases, adenomatosis turns into a malignant condition.
Glandular and fibrous polyps do not turn into malignant formations, but are a prerequisite for the development of atypical hyperplasia.
Cancerous formations
The second classification allows you to determine the severity of the disease, the choice of treatment regimen and further prognosis.
- Simple glandular hyperplasia. The structure of the glands remains the same; only their number increases. The risk of developing cancer is 1%.
- Complex hyperplasia. Glands accumulate on the surface. The risk of developing cancer is 3%.
- Simple hyperplasia with signs of atypia. The risk of developing cancer is 8%.
- Atypical hyperplasia. The risk of developing cancer is 29%.
Focal (local) endometrial hyperplasia
The main difference between focal endometrial hyperplasia is that pathological changes are recorded only in certain areas of the inner lining of the uterus - locally, and not diffusely (everywhere). That is, the test results will indicate that there are foci of hyperplasia, but healthy endometrial tissue from normal areas is also detected.
Depending on the histological picture (endometrial tissue is sent for examination after curettage of the uterine cavity), various variants of focal hyperplasia are distinguished. Detection of one type or another affects further treatment and prognosis.
Focal hyperplasia of the endometrium of the uterus according to ultrasound data
Simple (glandular)
With simple hyperplasia (the second name is glandular), an increase in the thickness of the endometrium is observed, but in its structure it does not differ from the norm. This is the simplest variant of hyperplasia, has a benign prognosis, is better amenable to drug treatment and is practically not fraught with the development of uterine cancer.
Glandular cystic hyperplasia
This is the next stage in the development of the pathological process. At the same time, the endometrium thickens, its cells begin to divide chaotically, which leads to disruption of their location. Compression of the glands occurs, as a result of which the outflow of secretions becomes difficult and cystic growths of the endometrium occur. With timely treatment, the prognosis is favorable.
Adenomatous (atypical) hyperplasia
The most unfavorable option. At the same time, endometrial cells lose their normal functions, are located chaotically, and tissues with atypical characteristics appear. Adenomatous hyperplasia more often requires radical surgical treatment and has a high risk of degeneration into cancer, especially without proper treatment.
Other types of hyperplasia
Polypous endometrial hyperplasia is also sometimes identified. In this case, cell division occurs in one place, resulting in polypous growths. They may also have signs of glandular, glandular-cystic or adenomatous hyperplasia, from which the further prognosis of the disease is determined.
Classification of hyperplasia
Hyperplastic processes of the endometrium are divided into 2 groups:
| Endometrial hyperplasia | Uterine polyp |
| Glandular | Fibrous |
| Glandular-cystic | Glandular |
| Atypical | Glandular fibrous |
| Adenomatous |
The risk of malignant degeneration is of great importance for future treatment: the detection of atypical cells in the endometrium is the first sign of oncological pathology. Any variant of atypical hyperplasia indicates a high probability of developing endometrial cancer in the near future.
According to the distribution of hyperplasia, they are distinguished:
- focal lesion;
- diffuse variant of pathology.
A polyp of the uterine body can be considered as a focal thickening of the endometrium or a tumor-like formation of the inner lining of the uterus. Adenomatous polyp is a precancerous process that requires surgical intervention.
Uterine polyp
Signs of endometrial hyperplasia and its symptoms
Hyperplasia, as a rule, occurs with a clear clinical picture, the main symptoms are the following:
- Heavy menses, with clots. They are caused by the fact that during menstruation a large (hypertrophied) layer of the endometrium is rejected. Often women notice clots of different sizes - from small to 10 cm or more.
- Intermenstrual bleeding. Especially characteristic of polyps. More often they occur in the middle of the cycle and in this case they can be confused with ovulatory discharge.
- Cycle disruption. Since the development of hyperplasia is based on an imbalance between estrogens and gestagens, problems almost always occur in women. As a rule, menstruation occurs with delays from several days to a couple of weeks.
- In menopause - the appearance of bloody discharge against the background of a long absence of menstruation. It can be either one small spot or bleeding.
- Pain during menstruation. Women note that recently their periods are not only heavy, but also painful. In this case, the peak of unpleasant sensations is often accompanied by the release of clots.
- Infertility. The abnormal endometrium does not provide a good site for the attachment of the fertilized egg, so women with hyperplasia often cannot become pregnant. After recovery, everything gets better.
Watch this video about the symptoms and consequences of endometrial hyperplasia:
Treatment of hyperplasia without curettage
If detected at an early stage, endometrial hyperplasia is treated with medication. Also, the indication for conservative therapy is the patient’s adolescence and the elimination of the risk of developing cancer. Treatment takes place in stages:
- Prescription of oral contraceptives that suppress ovarian activity. As a result of administration, a balance is achieved between estrogens and gestagens, bleeding stops. In parallel, in case of large blood loss, antianemic therapy can be carried out;
- Suppression of endometrial growth using progesterone drugs, often combined with taking medications that normalize the activity of the nervous system. A course of gonadotropin-releasing hormone agonists is prescribed, completing the main part of the treatment;
- After completion of drug treatment, restorative therapy to normalize the functioning of the reproductive system.
Some clinics offer their patients alternative methods of treating endometrial hyperplasia: homeopathy, folk remedies, installation of an intrauterine device containing gestagens to gradually thin the endometrial layer. Before agreeing to alternative treatment, it is recommended to consult with several doctors, and then, based on their recommendations, draw conclusions and make a decision.
Thickening of the endometrium of the uterus: causes of pathology
The pathological thickening of the endometrium of the uterus is based on an imbalance between estrogens and gestagens. However, other factors may also cause the development of the disease.
Proliferation of the endometrium in the uterus in women
In women of reproductive age, the causes of endometrial growth in the uterus may be the following conditions:
- metabolic disorders and, as a result, excess body weight;
- diseases of the endocrine glands - pancreas (diabetes mellitus), thyroid, adrenal glands;
- premenopausal changes, failures;
- ovarian cysts;
- constant use of certain medications, especially those based on glucocorticosteroids;
- chronic inflammatory processes of the genital organs, which provide the basis for the development of hyperplasia;
- frequent abortions and diagnostic curettage of the uterine cavity.
Endometrial hyperplasia in teenage girls
The causes of hyperplasia in teenage girls are approximately the same factors, but stress, hereditary diseases, and pathologies of endocrine organs play an important role.
Causes of pathology
The most important and prognostically dangerous causative factor is the imbalance between the main female hormones - estrogens and gestagens. Long-term and monotonous estrogen stimulation of the endometrium occurs against the background of the following conditions:
- lack of ovulation (anovulation);
- persistence or atresia of the follicle (changes in the ovaries in which the egg is not released and estrogen production increases);
- decrease in the amount of progesterone due to insufficiency of the corpus luteum.
General and gynecological diseases that provoke the occurrence of pathology in the endometrium are of great importance:
- metabolic syndrome with increasing obesity and high blood pressure;
- endocrine pathology (thyroid disease, diabetes);
- chronic inflammation in the uterine cavity (endometritis);
- interstitial uterine fibroids;
- adenomyosis or any variant of genital endometriosis;
- cystic ovarian tumors;
- long-term infertility with unsuccessful attempts at treatment.
Hyperplastic processes in the uterine cavity can lead to endometrial cancer. This situation is possible against the background of the following risk factors:
- polycystic ovary syndrome (PCOS);
- menstrual irregularities that last 12 years or more;
- long-term absence of pregnancy in a woman who refuses to use oral contraceptives;
- combination of severe obesity and arterial hypertension;
- diabetes.
Malignant degeneration of hyperplastic endometrial cells in the presence of risk factors occurs in cases where examination is not carried out on time and there is no treatment. Any type of thickening of the inner lining of the uterus requires the correct approach to diagnosis and treatment, which is an effective method of preventing cancer pathology.
Why is endometrial hyperplasia of the uterus dangerous?
Hyperplasia of the endometrium of the uterus is dangerous due to the following complications:
- anemia of a woman due to heavy monthly blood loss;
- degeneration of tissues into malignant ones;
- infertility.
All these consequences can be prevented if the pathology is detected in a timely manner, treated and the factors that provoke the development of the disease are removed.
Can the disease develop into cancer?
In most cases, hyperplasia does not develop into cancer, but it is a background disease for such changes. The greatest danger is from focal atypical hyperplasia (adenomatous). Inexperienced histologists, viewing such a sample under a microscope, may even miss signs of an existing malignant degeneration among adenomatosis. Therefore, gynecologists always pay closer attention to this type of hyperplasia.
The risk of developing cancer is higher if:
- endometrial polyps, especially with signs of atypia;
- adenomatous hyperplasia;
- recurrent glandular hyperplasia, which does not respond well to conservative treatment.
Is it possible to get pregnant
As a rule, pregnancy does not occur against the background of endometrial hyperplasia. This is due to the following:
- defective endometrium, to which the fertilized egg cannot attach;
- imbalance of sex hormones and, as a result, anovulation or eggs with defective genetic material.
Pregnancy is possible after complete recovery following a course of conservative treatment, usually hormonal therapy.
Is it possible to have sex
Endometrial hyperplasia is not a contraindication for sexual relations. However, women with GE often suffer from heavy periods, which limits their intimate life.
Treatment
Therapy for endometrial hyperplasia is carried out after receiving the histological result. There are 2 treatment options:
- medicinal;
- surgical.
- Conservative therapy
The main goal of drug therapy is to prevent another uterine bleeding and restore the menstrual cycle. For women dreaming of having a child, normal menstruation and the presence of ovulation are important treatment factors. Restoring hormonal balance is achieved by using the following drugs:
- gestagens;
- combined hormonal contraceptives.
Drug treatment of hyperplasia
The doctor selects the treatment regimen individually, taking into account age, hormonal levels, type of hyperplasia, the result of histological examination and the woman’s desire to give birth to a baby. You can use traditional methods as part of complex therapy only after consulting a doctor.
- Surgical intervention
Uterine bleeding that occurs due to endometrial hyperplasia must be stopped by removing excess endometrium. Most often, surgery is performed to scrape the uterine cavity. The best options may be modern techniques - laser and electrosurgical ablation of the endometrium. If precancerous changes are confirmed or cancer is detected, the uterus must be removed (hysterectomy).
Before hysteroscopy
Diagnosis of the disease
Diagnosis of the disease includes a routine examination by a doctor and clarification of the medical history, complaints, as well as instrumental methods - ultrasound, hysteroscopy, diagnostic curettage of the uterine cavity, endometrial biopsy. A more detailed description is presented in the table.
| Method | The essence | What can be revealed |
| Ultrasound | Using ultrasound waves, you can obtain a two-dimensional or three-dimensional image (scan) of the uterus and detect echo signs of pathologies. | Thickening of the inner layer of the uterus (endometrium) more than 5-7 mm on days 3-5 or more than 20-25 mm in the middle of the cycle. Polyps, especially large ones, are visualized independently as hyperechoic inclusions. |
| Endometrial biopsy | On an outpatient basis, the contents of the uterine cavity are “sucked in” using a special aspiration tube. Then the resulting material is subjected to histological or cytological examination. | Atypical cells and signs of endometrial hyperplasia. |
| Hysteroscopy | A special instrument (hysteroscope) is placed inside the uterine cavity. With its help, you can obtain an image of the endometrium on the monitor screen, as well as carry out various manipulations - removal of polyps, cauterization of pathological areas, etc. | You can see areas with hyperplasia, polyps and remove/cauterize them. |
| Diagnostic curettage | Using sets of curettes and dilators, the uterine cavity is curetted - the inner layer is removed, which normally should be rejected on its own every month. Subsequently, the obtained material is sent for research. | It is possible to reliably say whether there are signs of hyperplasia or not in the obtained material, determine whether there are atypical cells, confirm/refute malignant tissue degeneration |
Diagnostics
To diagnose pathology, a number of laboratory, instrumental and functional studies are required. During a routine examination, a gynecologist cannot diagnose a pathology, but can only suspect it based on the patient’s complaints.
Laboratory diagnostics can determine the nature of hormonal pathology and identify the presence of an inflammatory process.
The informativeness of ultrasound in diagnosis reaches 99%. Using transvaginal ultrasound, you can determine:
- size and shape of the uterus;
- The thickness of the endometrium in pathology is determined to be more than 15 mm;
- the presence of oval dense formations or thickening of the endometrium characteristic of the pathology;
- the presence of polyps, fibroids or adenomyosis.
Hysteroscopy allows you to determine pathologies in the gland, the presence of polyps, thickening of the mucosa, and also conduct histology of suspicious tissues. The manipulation is carried out on days 5-7 of the cycle.
Diagnostic curettage allows you to remove the entire pathologically changed layer and send it for histology. The manipulation should be carried out on the eve of menstruation. The information content of this diagnostic study reaches 90%.
Histology allows us to assess the nature of the changes.
A blood test is also performed to determine the amount of hormones. To exclude proliferative processes, mammography is prescribed.
Most often, to diagnose the condition of the endometrium, an ultrasound examination and hysteroscopy are performed.
Article on the topic:
Hormone tests in gynecology: which ones and when to take?
What to do after diagnostic cleaning
After diagnostic curettage, it is necessary to follow all the doctor’s recommendations, they are usually the following:
- abstain from sexual intercourse for 10-14 days;
- take antibacterial agents to prevent inflammatory changes;
- do not visit saunas, swimming pools, or take hot baths for the next two weeks.
Diagnostic curettage is used most often as a method of treatment (for example, for bleeding) and to clarify the diagnosis, including during treatment to confirm its effectiveness. However, the “gold standard” for suspected endometrial pathology is hysteroscopy. It allows you not only to see the changed areas of the endometrium, but also to specifically remove them, take a biopsy from the most “suspicious” place and at the same time carry out curettage of the uterine cavity.
Hysteroscopy
Prevention
An examination by a gynecologist every six months is the best means of preventing all female diseases, including endometrial hyperplasia. In addition, there is a set of preventive measures:
- Do not leave gynecological and hormonal ailments to chance;
- Entrust the doctor with the selection of COCs;
- Use contraception responsibly and avoid abortions;
- Exercise;
- Monitor your body weight and do not gain excess weight;
- Regularly undergo general medical examinations.
Some women, after being diagnosed with endometrial hyperplasia, admit that they have felt unwell for a long time, but were afraid to go to the doctor. This behavior is a big mistake. A diagnosis is not a reason to become depressed; many patients who underwent treatment were freed from the disease forever and were subsequently even able to give birth to children. Whatever the reasons, do not delay in visiting a doctor; it is dangerous to develop endometrial hyperplasia, and the consequences can be dire.
How to treat endometrial hyperplasia
Treatment of endometrial hyperplasia includes medications (mainly hormonal drugs), operations (with removal of the uterus and organ-preserving), as well as traditional methods. Schemes are prescribed only by a doctor after confirming the diagnosis.
Medicines
In order to “rebuild” endometrial cells for normal growth, it is first necessary to restore the balance between estrogens and gestagens.
For this purpose, drugs like progesterone are prescribed (they imitate its action), as well as those that affect the secretion of hormones by the pituitary gland and hypothalamus - in this case, the woman “plunges” into artificial menopause with minimal concentrations of steroids in the blood, as a result the endometrium atrophies, and menstruation stops. Groups of medications and patterns of their use are presented in the table below.
| Group of drugs | Representatives | How are they assigned? |
| Oral contraceptives - can only be used for simple glandular hyperplasia in young girls without significant aggravating diseases and risk factors | Claira Regulon Janine Jess Midiana Dimia Yarina | According to the usual contraceptive regimen for 28 days (including days of taking “pacifiers”) |
| Gestagens | Duphaston | 10 mg twice a day from 10/14 to 24 days of the cycle. In continuous mode (less often). |
| Norkolut | From days 10 to 25 of the cycle, 5-10 mg or on a continuous basis (in women after 40-45 years). | |
| The Mirena IUD is especially effective for hyperplasia due to adenomyosis. | It is installed for 5 years inside the uterine cavity and releases the medicine in doses | |
| GnRH agonists create an “artificial menopause” in the body. | Buserelin | 4.2 mg once every 4 weeks for 4-6 months |
| Zoladex | One capsule subcutaneously every three months | |
| Diferelin | 3.75 mg every 4 weeks subcutaneously |
Surgery
There are several options for surgical interventions for hyperplasia:
- Cauterization of the uterine mucosa using a coagulator, laser, or cryo-knife. In this case, not only the functional, but also the basal layer of the endometrium is removed, as a result of which it no longer grows.
- Removal of the uterine body - in case of recurrent hyperplasia, polyposis, ineffectiveness of conservative treatment.
Why is curettage done?
Curettage is necessary to stop bleeding. Often, it is with this complaint that women are admitted to gynecological hospitals, and only later it turns out that they have endometrial hyperplasia. In this case, the manipulation is performed on an emergency basis.
Curettage is routinely performed to clarify the diagnosis if GE is suspected (for example, based on ultrasound results), as well as to monitor treatment and decide on the need to adjust drug dosages.
Nutrition
The diet for hyperplasia should be varied and include sufficient amounts of the following nutrients:
- proteins – meat, eggs, fish, cottage cheese, kefir;
- carbohydrates – preferably complex (from various cereals, fresh and dried fruits);
- fats - vegetable or butter, nuts, cheese.
Nutrition should enrich the body with vitamins (especially A, E, C, group B) to prevent the appearance of atypical cells.
It is important not to eat food in excess of the prescribed caloric intake, otherwise weight will increase, and this will provoke a worsening of hyperplasia.
Traditional methods
The following folk recipes can be used to treat hyperplasia:
- Tincture of boron uterus. Take 20-30 g of dried herb and mix with 500 ml of vodka. Leave for about 20 days in a cool, dark place. Then pass through gauze and take 15-20 drops 2-3 times a day.
- A decoction of boron uterus. Steam 10-20 g of herb in 500 ml of boiling water, let it brew in a water bath for about another hour. Take a tablespoon three times a day.
- Juice of burdock and golden mustache. Wash and peel the fresh roots of both plants and squeeze out the juice. Mix and drink a tablespoon two to three times a day.
- Nettle tincture. Take 200 g of herb and infuse it with 500 ml of alcohol in a cool, dark place. Drink a teaspoon twice a day.
- Nettle infusion. Steam two or three tablespoons of the herb in 500 ml of boiling water. Leave in a water bath for another 30 minutes, strain through gauze and take 100 ml 3-5 times a day.
- Herbal infusion. Take one portion of serpentine root, shepherd's purse and twice as much calamus root, cinquefoil, knotweed and nettle. Mix and take 10 g of the mixture, steam 500 ml of boiling water and put in a thermos for a couple of hours. Take 100 ml 2-3 times a day.
Treatment during menopause
Treatment of hyperplasia in menopause is often surgical rather than conservative - curettage of the uterine cavity is always performed, and therapy is prescribed based on the results obtained. Recurrent hyperplasia is an indication for removal of the uterus. Among hormonal drugs, Norkolut is usually prescribed.
A feature of the menopausal period is that under the mask of hyperplasia, according to ultrasound, there may be an accumulation of serous fluid or fibrous polyps - both conditions, if confirmed by curettage, do not require any treatment, but only observation.
Can it be cured forever?
It is possible to cure hyperplasia forever if, after normalization of endometrial growth, all factors provoking the disease are eliminated, including normal body weight, blood pressure numbers, etc.
Watch this video about the treatment of endometrial hyperplasia with photodynamic therapy (PDT):
Is relapse possible?
No woman is immune from relapse of endometrial hyperplasia, even with adequate treatment. More often the disease returns if:
- the entire course of treatment has not been completed or an insufficient dose of drugs has been selected;
- risk factors have not been eliminated (diabetes mellitus, excess body weight, etc.);
- there are concomitant gynecological diseases (for example, polycystic disease, uterine fibroids and others).
Simple glandular endometrial hyperplasia: what to do?
It is important to understand that any variant of the hyperplastic process can become the basis for serious gynecological pathology. Treatment tactics depend on the following factors:
- age (in postmenopausal women, glandular endometrial hyperplasia is a precancerous condition);
- severity of menstrual irregularities;
- a woman’s desire to give birth to a baby;
- the presence of concomitant problems with the ovaries and endocrine organs.
The optimal method of treatment at the first stage is to perform hysteroscopy (a method of visual examination of the inner surface of the uterus) with mandatory removal of the thickened endometrium (taking biopsy material). This is especially important for women after 45 years of age. In the absence of oncology, all possible methods of therapy can and should be used to eliminate hyperplastic processes in the uterine cavity.
A good method of treating endometrial hyperplasia is successful conception, pregnancy, childbirth and long-term breastfeeding. If pregnancy is not necessary, then it is necessary to use one of the methods of hormone therapy (oral contraceptives, hormonal IUD). Based on the research, the doctor will choose the optimal treatment option to prevent future problems with women’s health.
Prevention methods
Prevention of endometrial hyperplasia is as follows:
- if complaints arise, you must consult a doctor promptly;
- it is important to avoid inflammatory diseases of the pelvic organs;
- avoid abortions and other intrauterine manipulations;
- It is recommended to use hormonal contraceptives as contraception;
- treatment of concomitant extragenital diseases, especially blood pressure, diabetes, obesity.
We recommend reading about the nature of menstruation with hyperplasia. From the article you will learn about how the menstrual cycle changes with endometrial hyperplasia, methods of examining the patient and treatment. And here is more information about the treatment of endometrial hyperplasia without curettage.
Endometrial hyperplasia is one of the most common pathologies of the female reproductive system. In most cases, the disease manifests itself as heavy periods and rarely develops into a cancerous tumor. To establish a diagnosis and prescribe the most appropriate treatment, it is necessary to undergo uterine curettage or hysteroscopy.
Normal endometrium
The inner lining of the uterus is subject to the hormonal influence of the ovaries, which work in a cyclic two-phase mode. In the first half of the cycle, the thickness of the endometrium increases; in the second half, the quality of endometrial tissue changes, which is necessary for a full pregnancy to occur.
Normal and endometrial hyperplasia
Criteria for normal menstruation:
- cycle duration - from 21 to 35 days (average 28);
- duration of menstruation - from 2 to 7 days;
- the approximate volume of blood loss is no more than 80 ml.
The following types of bloody discharge are not considered a pathology:
- irregular periods for 1.5-2 years in girls after the first arrival of menstruation or in women before menopause;
- bleeding at the time of ovulation (ovulatory bleeding);
- scanty bleeding a week after conception (implantation bleeding).
Normally occurring periods are a criterion for a woman’s hormonal and reproductive health. The hyperplastic process appears against the background of endocrine imbalance, which occurs for various reasons, therefore, for any problems with menstruation, you must consult a doctor for examination and treatment.
Useful video
Watch this video about the treatment of endometrial hyperplasia without surgery:
Similar articles
- Treatment of endometrial hyperplasia without curettage
Not every doctor will begin treatment of endometrial hyperplasia without curettage. The thing is that this is a diagnostic procedure that allows you to most accurately establish a diagnosis, exclude oncology and choose the best treatment option. Read more - Endometrial hyperplasia: treatment after curettage
If endometrial hyperplasia is established, treatment after curettage will be aimed at containing the progression of the disease and preventing possible complications from the diagnostic procedure. Read more
- Removal of the uterus for endometriosis: all the pros and cons...
In some situations, it is necessary to remove the uterus for endometriosis. Indications may include both large lesions and other organ problems. It is necessary to weigh the pros and cons, because one of the consequences of removing the uterus and ovaries is early menopause. Read more
- The essence of the disease endometrial hyperplasia
Often it is menstruation with hyperplasia that becomes the reason to consult a doctor. Due to the pathology, periods become long, heavy, with pain and clots. Read more
Causes and characteristic symptoms
Endometrial hyperplasia is a very insidious disease - sometimes it is asymptomatic for a long time. But the main risk factors :
- Puberty;
- Menopause;
- Increased estrogen levels;
- Inflammatory processes in the pelvic organs;
- Sexual infections;
- High blood sugar;
- Overweight;
- Hypertension;
- The uterine device, if it is installed incorrectly;
- Surgical operations affecting the genitourinary system;
- Hereditary factor.
The cause of endometrial hyperplasia is revealed only through a detailed examination of the patient. Doctors advise women to listen more carefully to their bodies and not to ignore dangerous symptoms :
- Spotting between periods;
- Heavy periods after a short delay with the presence of large clots;
- On the contrary, the discharge is too scanty due to endometrial pathologies;
- Cessation of menstruation for several cycles in a non-pregnant woman;
- Brown discharge after sexual intercourse;
- Difficulty conceiving during regular sexual activity without the use of contraception;
- Frequent pain in the groin area.
The presence of even one alarming symptom from this list is a reason to visit an antenatal clinic as soon as possible. Treatment of timely detected endometrial hyperplasia is usually limited to taking medications and preserves the woman’s reproductive abilities.