The large intestine is a special section of the gastrointestinal tract. The length of the adult human intestine reaches two meters. This organ consists of the cecum with the appendix, colon and rectum, which ends in the anus. Up to three kilograms of partially digested food collects in the large intestine, and this is where beneficial elements are absorbed. When defecating, a person gets rid of two hundred to three hundred grams of feces, the rest is absorbed. All departments are important for the complete absorption and digestion of food. There are a variety of diseases of the colon. The time interval between food entering the colon and the act of defecation is on average ten hours. Constipation is considered to be a delay in defecation for more than a day. In this condition, a person feels heaviness in the abdomen, becomes irritable, painful spasms and gas formation are possible, and attempts to forcefully defecate do not produce results. The most common organic diseases of the large intestine are:
- ulcerative colitis;
- Hirschsprung's disease;
- Crohn's disease;
- ischemic colitis;
- colitis caused by taking antibiotics;
- colon tumors;
- irritable bowel syndrome;
- diverticulosis of the large intestine;
- dolichosigma;
- megacolon.
There is a group of disorders related to functional bowel diseases:
- constipation (difficulty passing stool);
- diarrhea (frequent defecation, liquid stool);
- irritable bowel syndrome (alternating diarrhea and constipation)
- flatulence (increased gas formation);
- constant pain in the abdomen.
The importance of the large intestine
The large intestine is the part of the digestive tube that ensures the formation and elimination of feces.
Excretory substances (metabolic products), salts of heavy metals, etc. accumulate in the lumen of the colon. The bacterial flora of the colon produces vitamins B and K, and also ensures the digestion of fiber. A feature of the relief of the colon mucosa is the presence of a large number of crypts and the absence of villi.
The vast majority of cells in the epithelial layer of the colon mucosa are goblet cells, which produce a large amount of mucus on the surface of the mucous membrane and, mixing with undigested food particles, facilitate the passage of feces in the caudal direction.
In the right side of the colon, muscle contractions, called antiperistaltic waves, create a reverse movement, helping to temporarily delay the intestinal contents for complete processing by microorganisms.
Differences between the large and small intestines
They are created from muscle tissue, but have a number of physiological and functional differences. However, they are closely related, since they harmoniously take part in the process of digesting food.
| Physiological development | Small intestine | Colon |
| Diameter | 2-4 cm | 4-9 cm |
| Color | Pink | Ash gray |
| Muscle | Smooth, longitudinal | Uneven |
| Omental processes | None | Present |
| Wall thickness | 2 to 3 mm | 3 to 5 mm |
In a living person, the length of the small intestine is 3.5-4 meters, in a dead person it is about 6-8 m due to the loss of intestinal tone, that is, 2 times more.
The length of the large intestine is much smaller - 1.5-2 meters.
There are more than a hundred reliable medical studies that confirm that more than 65 diseases of the human body are in one way or another associated with improper functioning of the intestines.
Colon imbalance can be the cause of many chronic diseases, including arthritis, allergies, asthma, irritable bowel syndrome, liver problems, kidney problems, skin problems, and even heart disease or cancer.
To avoid long-term health problems, it is extremely important to take care of your gut health and keep it functioning properly.
To normalize the functioning of the intestines and the body as a whole, it is recommended to undergo the “Gastrointestinal Health as a Foundation” program 2 times a year.
A well-functioning liver is a neutralizer of all toxins that may enter the liver from the large intestine. Therefore, it is important to maintain liver health: the “Health of Your Liver” program.
Treatment of benign rectal tumors
Currently, surgery is considered the main treatment method for benign rectal tumors. The approach to the choice and nature of surgical intervention is determined by the type and nature of the benign neoplasm.
Treatment of single and group rectal polyps
For single and group polyps, surgical methods became widely used after Albi proved the possibility of their malignancy in 1912.
He removed low-lying single and group polyps of the rectum transanally, and higher-lying ones through a proctoscope. A number of authors subsequently defended conservative tactics for adenomatous polyps, believing that they do not turn into cancer (Fiegel B. et.al., 1962; Castleman N., Krikstein S., 1962). However, modern ideas in oncological science allow us to consider surgical removal of polyps to be the only reliable way to cure rectal polyps, and, consequently, a way to prevent cancer.
It can be carried out in several ways: by transanal excision, by electrocoagulation through a proctoscope, as well as by more extensive operations - posterior rectotomy, resection or amputation of the rectum. Table 22.1 provides information on surgical operations for single and group rectal polyps.
Table 22.1. The nature of surgical interventions for single and group rectal polyps
| No. | Nature of the operation | Number of patients |
| 1 | Transanal excision | 21 |
| 2 | Electrocoagulation | 44 |
| 3 | Posterior rectotomy | 3 |
| 4 | Anterior rectal resection | 2 |
| Total | 70 | |
Transanal excision of polyps is indicated when the tumor is localized at a distance of no more than 8-10 cm from the anus.
The most favorable conditions for such an operation are for polyps located in an area up to 6 cm from the anus. This operation should not be performed if there are clinical or, especially, histological signs of malignancy. In addition, transanal excision of large polyps sitting on a broad base and located no higher than 6 cm from the edge of the anus should not be performed.
Postoperative preparation should include:
1) prescribing a slag-free diet 2-3 days before surgery; 2) on the evening before the operation - a cleansing enema (600-800 ml); 3) in the morning, 1.5-2 hours before surgery - a cleansing enema (600-800 ml) and after bowel movement, a drainage tube must be inserted into it to drain residual water and liquid feces; 4) in patients with constipation, castor oil (30 g) should be prescribed 18 hours before surgery; 5) the operation should be performed under general anesthesia or using epidural anesthesia.
With the patient in the same position as for perineal sectioning, a rectal speculum is inserted into the rectum. If the polyp is located in the anal canal, then it is cut off after applying a Billroth clamp to its pedicle. Hemostasis If the polyp is broad-based, a bordering oval incision is made around it and the polyp is excised. The mucosal wound is sutured with two interrupted catgut sutures.
If the polyp is located at a distance of 6 to 10 cm from the anus, it is necessary to insert a gynecological speculum after overstretching the anal sphincters. With the help of this mirror, the intestinal wall, free of tumor, is retracted. The polyp is captured at the base.
The polyp is excised within healthy tissue and, as it is cut off, the wound of the mucous membrane is sutured with catgut sutures, which can be used as holders, tightening the mucous membrane. After suturing, the mucous membrane is treated with a 1% iodine solution or iodonate. A gas outlet tube wrapped in ointment tampons is inserted into the rectum.
Group and multiple polyps are removed one by one. It should be remembered that between the wounds left after excision of several polyps there should be a strip of healthy mucous membrane, in order to avoid cicatricial deformities and strictures.
After transanal excision of polyps, a special diet and bed rest are prescribed for 4-5 days. To artificially retain stool, opium tincture is given orally (6 drops 3 times a day - 30 minutes before meals). The first dressing should be carried out on the 3rd day after surgery after a preliminary warm (35-36 °C) sitz bath for 10-15 minutes and anesthesia (1.0 ml of 1% promedol solution).
The gas outlet tube with tampons is removed, the wound is washed with antiseptics and the ointment tampon is reinserted into the rectum. The second dressing is after 2 days. For 5-6 days, if you have the urge to stool, you can prescribe an oil enema (60-80 ml). Then daily sitz baths and dressings.
Electrocoagulation of rectal polyps through a proctoscope was first proposed in 1928 by I.S. Friedman and P.I. Gelfer, who used high-frequency currents. Subsequently, the method was improved by a number of authors. This operation is performed when the polyp is localized at a distance of 10 to 25 cm from the anus. This method can be used to remove small polyps with a clearly defined stalk, and small polyps with a wide base.
Preparing patients for this operation is the same as for transanal excision of polyps. The position on the operating table is knee-shoulder. Electrocoagulation of polyps is performed with special active electrodes in the form of forceps or loops. A passive electrode made of a lead plate is fixed in the lumbosacral region.
A rectoscope with a mubus 20 or 25 cm long is inserted into the rectum. Its end is placed at the level of the polyp. An active electrode is inserted and a potential is applied to it for 2-3 seconds. In this case, a slight tightening of the electrode along with the polyp is performed.
As a rule, one cauterization is sufficient. If the polyp is not excised, then cauterization is repeated. It is important that electrocoagulation is performed to avoid relapse at the level of the attachment of the pedicle to the intestinal wall.
Broad-based polyps can sometimes be excised only in parts. First, most of the base is coagulated, and then the remains of the polyp.
In the postoperative period, bed rest is prescribed for 6-7 days, an easily digestible diet, drugs aimed at stool retention, and antibiotics. It should be noted that after electrocoagulation of tumors localized in the rectosigmoid region, pain in the lower abdomen and symptoms of peritoneal irritation may be observed.
In rare cases, perforation of the intestinal wall may occur. We observed this complication in one patient. A polyp measuring 2 cm in diameter on a thin stalk was located at a distance of 1.6 cm from the anus. 1 day after the operation, severe abdominal pain occurred and signs of peritonitis appeared. Laparotomy revealed perforation of the intestinal wall.
Thus, electrocoagulation of rectosigmoid polyps, especially those on a wide base, should be treated with caution. It may be necessary to follow the recommendations to carry out electrocoagulation of such polyps in parts, in several sessions.
There is another danger when performing this operation. Cases of explosion in the rectum and colon during electrocoagulation have been described. This is due to the methane present in the intestine and increasing with charring of the mucous membrane.
Methane microexplosions are observed quite often during electrocoagulation, which is manifested by characteristic clicks. The generally accepted recommendation for the prevention of this complication is intermittent electrocoagulation and additional air supply to the rectum.
To remove large polyps on a wide base, located at a distance of up to 8 cm from the anus, you can use its removal from a wider access. For this purpose, a posterior rectotomy is performed.
Preoperative preparation for this operation is the same as for transanal excision of a polyp. General anesthesia. The patient is placed on the operating table on his stomach so that the patient's pelvis is the highest point. The lower limbs are spread as wide as possible.
Posterior to the anus along the midline, a skin incision 9-12 cm long is made. The coccyx is exposed and under it m. levator ani. The fibers of the gluteus maximus muscle are cut off from the coccyx, after which the m.levator ani is dissected from the top of the coccyx to the external sphincter along the midline. After this, the posterior wall of the rectal ampulla is exposed.
The rectum is isolated from the surrounding tissues using a blunt and sharp method and its lumen is opened. Thus, there is wide access to the tumor located, as a rule, on the anterior or lateral walls.
The tumor is excised at least 1 cm away from it within healthy tissues along with the mucous membrane, while sparing the muscular layer. The bleeding is stopped, and the mobile mucosa is sutured with catgut sutures. The rectotomy opening is carefully sutured with double-row sutures. The dissected part of the levator ani muscle is sutured with several sutures.
Through a separate skin incision, drainage is introduced into the wound cavity, and the skin is sutured using Donati sutures. After the operation, it is necessary to perform devulcio ani and insert a gas outlet tube wrapped in ointment tampons into the rectum. The gas outlet tube is removed on the 3rd day, drainage - after 6-8 days.
If the rectosigmoid polyp reaches a large size, has a wide base, and also with clinical signs of malignancy, anterior resection of the rectum is advisable, described below.
With surgical treatment of single and group polyps, long-term results are usually satisfactory, although cases of relapse are described. In the sixties, the percentage of relapses, according to various authors, ranged from 10 to 24.5%, and nowadays it is observed less frequently. Of our 70 patients with single and group polyps, relapses were observed in 5 patients (7.1%). All of them underwent electrocoagulation of polyps of the supramullary and superior ampullary sections.
Treatment of villous tumors of the rectum
Treatment of villous tumors is necessarily surgical.
The choice of surgical intervention depends primarily on whether there are signs of cancerous degeneration. If signs of malignancy are already visible during clinical examination, radical surgery is indicated, as for rectal cancer. Some authors believe that, given the high potential for cancerous degeneration, all villous tumors should undergo radical surgery. However, taking into account the absence of cancer cells in histological examination, sparing operations are still allowed for villous tumors.
When signs of cancer are detected in a villous tumor removed in this way, these authors resort to repeated radical surgery or even limit themselves to postoperative radiotherapy in cases where the cancer has not yet infiltrated the mucous membrane in the area of the tumor stalk.
So, mobile, small, pedunculated villous tumors without clinical and morphological signs of malignancy can be removed using gentle operations.
If the villous tumor is located at a distance of up to 10 cm from the anus, then transanal excision is possible. When localized in a segment removed by 9-14 cm, excision is usually performed through a posterior rectotomy. Tumors located in the rectosigmoid region, 15-18 cm from the anus, require anterior resection of the rectum.
If it is impossible to excise a large creeping tumor transanally or with posterior rectotomy, an abdominal-anal resection of the rectum is performed with reduction of the sigmoid colon and preservation of the anal sphincters.
Electrocoagulation of villous tumors is used as an exception in cases where the tumor has a well-defined stalk, is located at a distance of 10-25 cm from the anus, with a histologically proven absence of cancer cells, and also if the patient’s condition does not allow extensive surgery.
Of 15 patients with villous tumors, electrocoagulation was performed in only 1 case. In two patients the tumor was removed through posterior rectotomy, in three - transanally. The remaining 9 patients underwent radical operations: anterior resection of the rectum (4), abdominal-anal resection with reduction of the sigmoid colon (5).
Such a radical choice of operations in these patients was due to the fact that clinical examination revealed areas of compaction or ulceration. Even the absence of biopsy data on malignancy in these cases did not allow performing sparing operations.
Moreover, there is information that a preoperative biopsy may not detect cancer cells, and after a histological examination of the entire removed tumor, cancer is often detected in the latter. Of the 15 patients, this situation occurred in three. All of them underwent radical operations.
With rare benign tumors of the rectum (leiomyoma, fibroma, lymphoma), even if they are small in size, it is rarely possible to remove them transanally or using electrocoagulation. These tumors, unlike polyps, are inactive, do not have a stalk, are poorly relegated to the anus, and are located in the submucosal or muscular layers.
Therefore, the operation of choice for tumors located at a level of 4-12 cm from the anus is their excision through posterior rectotomy, and for higher locations, colectomy or, more often, intestinal resection is performed.
Causes of development of diseases of the large intestine
- heredity;
- the presence of other diseases of the digestive system (gastritis, pancreatitis);
- intestinal infections;
- taking certain medications (long-term and uncontrolled antibacterial therapy can disrupt the composition of the microflora);
- dietary errors (abuse of fatty, fried foods, processed foods, lack of fiber in the diet, etc.);
- lack of vitamins and microelements;
- bad habits;
- excess body weight;
- physical inactivity;
- stress;
- motor impairment;
- digestive problems;
- absorption problems;
- inflammatory processes;
- the appearance of neoplasms.
Statistics say that certain diseases of the digestive system are present in 90% of the population of developed countries.
Inflammatory bowel diseases, which include Crohn's disease and ulcerative colitis, are diagnosed in approximately 200 people out of 100,000 people examined. They mainly affect young people. Men and women get sick with approximately the same frequency.
Increasingly, patients with bowel symptoms are being diagnosed with irritable bowel syndrome. Its prevalence in the world reaches 20%. According to various sources, women suffer from irritable bowel syndrome 2-4 times more often than men, with the highest incidence rates occurring at the age of 30-40 years.
Symptoms of colon disease
Most diseases of the large intestine are asymptomatic for a long time, and then manifest themselves with so-called intestinal discomfort, which increases over time.
Common signs of colon diseases are as follows:
- stool disorders (constipation, diarrhea, unstable stool);
- stomach ache;
Most often, pain occurs in the lateral parts of the abdomen, in the anus.
Pain in the epigastric region or above the navel is less common. As a rule, the pain is dull, aching, bursting, and less often - cramping. They weaken after the passage of gas or bowel movements. Rumbling in the stomach, bloating, and accumulation of gases are more often observed in the afternoon. They intensify in the evening and weaken towards night.
Other signs of colon disease include discharge of mucus or pus from the anus, bleeding or blood in the stool, frequent false urge to defecate (tenesmus), and incontinence of gas and feces.
Many inflammatory and tumor diseases of the colon are accompanied by serious metabolic disorders. As a result, a person feels increasing weakness, exhaustion, and the functions of the genital organs are impaired.
Sick children have slower growth and development.
Diverticulosis, symptoms and treatment
Mental shock
Diverticulosis is a pathological change in tissue structure. Various complications pose a great danger. The most dangerous thing is the transition of the disease to a malignant form. The formation of diverticula occurs as a result of stretching of the walls of the large intestine. Gastroenterologists monitor the course of the disease. The likelihood of the disease progressing to oncology requires careful monitoring by a doctor. Diverticulosis is divided into the following subtypes:
- asymptomatic;
- symptomatic course;
- complicated.
Early diagnosis is only possible through endoscopic examination. When monitoring the patient, it is necessary to monitor changes in diverticula. In some cases, surgery is performed. Sick people require control over the quality of food and organization of food intake. Preventive bowel cleansing is practiced in all cases.
Colon diseases
Ulcerative colitis is a chronic inflammatory disease of the large intestine that affects the mucous membrane of the rectum and its other parts. The inflammatory process from the rectum can spread to the entire colon.
Crohn's disease affects the entire intestine, stomach and esophagus. Inflammatory changes are single or multiple. The inflammatory process spreads to the entire thickness of the intestine. Complications - formation of fistulas (purulent tracts), fever, damage to joints, eyes, liver, skin rashes.
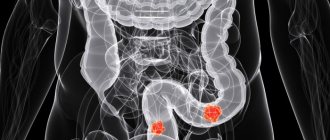
Tumors of the large intestine - benign and malignant (cancer of the colon and rectum). Risk factors for tumors include a diet rich in refined foods and animal fats, the presence of colon polyps, hereditary polyposis, heredity, and long-term ulcerative colitis.
Colon dyskinesia is a disorder of the motor function of the colon and, to a lesser extent, the small intestine, not caused by organic lesions and characterized by pain, changes in bowel function, and sometimes increased secretion of mucus.
Colon diverticulosis is a disease in which small pouch-like protrusions (diverticula), up to one to two centimeters in size, form in the intestinal wall .
Hemorrhoids are a disease consisting of dilation of the veins in the lower part of the rectum, where nodes form and sometimes bleed.
Appendicitis is inflammation of the appendix .
Dysbiosis is a change in the composition and quantitative relationships of normal microflora (microorganisms) that populate the human body .
Anti-inflammatory products from NSP:
- Morinda;
- Noni juice;
- Colloidal silver;
- Aloe Vera Juice;
- Olive leaves.
Ulcerative colitis
Ulcerative colitis (colon ulcer) is a chronic inflammation of the intestinal mucosa, caused by the formation of ulcers.
The causes of this disease are not clear. Researchers' opinions are divided, and different groups of doctors put forward different hypotheses:
- hereditary disease, the catalyst for its triggering is an unfavorable environment;
- infectious disease, the disease occurs due to a pathogen that has not yet been identified;
- autoimmune disease, the body's own immune system produces antibodies.
The precursor to ulcerative colitis is stress, unbalanced nutrition, dysbacteriosis, and physical inactivity. Most often people between twenty and sixty years old are affected.
The disease occurs with alternating remission and exacerbation. The severity of the disease varies from mild to very severe. In the acute period of mild severity, the body temperature rises to 38 degrees, the person feels exhausted, there is an admixture of blood and mucus in the stool, and bowel movements up to six times a day. In the acute period of severe disease, the body temperature reaches 39 degrees, tachycardia, dizziness, tremor, and apathy appear. The frequency of defecation reaches eight times a day, the urge is accompanied by painful spasms, feces mixed with purulent and bloody contents. In case of acute pain and bleeding, you should immediately consult a doctor. Such clinical phenomena are similar to acute surgical pathology, and the loss of time in this case is extremely dangerous. In order not to blur the clinical picture, taking painkillers is highly undesirable! In some cases, you can take medications to relieve cramps.
Read
About Filtrum and Lactofiltrum: how to choose the best product
To confirm the diagnosis of ulcerative colitis, you need to take a general blood test and do an endoscopic examination of the mucous membrane. Fibercolonoscopy is done through the anus. This examination method is not suitable for the acute period, as there is a possibility of rupture of the intestinal wall. In this case, irrigoscopy is performed. This is an x-ray examination.
Ulcerative colitis
During the treatment of ulcerative colitis, the main task is to exit the acute period and achieve stabilization of the patient’s condition. Anti-inflammatory, antispasmodic drugs, and cytostatics are prescribed. In severe cases, with severe bleeding and large blood losses, blood transfusion is recommended. The use of antibacterial agents is prescribed as needed. In extremely severe cases of the disease, intravenous feeding of nutritional mixtures may be required. If all measures aimed at improving the condition do not produce results, rectal resection is indicated.
Classification of types of digestion
According to the origin of digestive enzymes, they are divided into three types:
- own;
- symbiont;
- autolytic.
According to the localization of the polymer splitting process:
- intracellular digestion;
- extracellular digestion: distant (cavitary);
- contact (wall, membrane).
Symbiont digestion
Symbiont digestion is the hydrolysis of nutrients due to enzymes synthesized by the symbionts of the macroorganism - bacteria and protozoa of the digestive tract. Symbiont digestion occurs in humans in the large intestine.
Fiber in food in humans, due to the lack of the corresponding enzyme in the secretions of the glands, is not hydrolyzed (this has a certain physiological meaning - the preservation of dietary fiber, which plays an important role in intestinal digestion), therefore its digestion by the enzymes of symbionts in the large intestine is an important process.
Enzyme products from NSP:
1. Digestive enzymes
- Digestive enzymes replenish the deficiency of digestive enzymes.
- Improves the breakdown and absorption of nutrients.
- Digestive enzymes also normalize the functioning of the digestive organs.
2. Protease Plus
- Used as a systemic enzyme preparation.
- Improves the breakdown and absorption of proteins.
- Reduces blood viscosity, improves blood circulation.
- Has anti-inflammatory and anti-edema effects.
3. Ag-X
- Reduces inflammatory processes in the digestive system, reduces pain.
- Strengthens the secretion of digestive enzymes and bile, improves the digestion of food in the gastrointestinal tract.
- Increases the body's protective properties.
How is cancer diagnosed?
A general blood test will help detect a tumor in time.
Due to the non-specificity of the symptoms of intestinal cancer, it is very difficult to detect it in the early stages. That is why it is so important to promptly contact specialists at the first signs of dysfunction of the gastrointestinal tract.
This is especially true for people for whom the risk of tumor formation is considered increased (we are talking, in particular, about people over 50 years of age).
One way or another, if during a conversation with the patient the doctor has reason to suspect the visitor has cancer, he will refer the patient for additional diagnostic examinations. To detect a malignant tumor in a timely manner, doctors carry out a number of research procedures. Among them:
- visual examination of the patient;
- taking anamnesis;
- examination of the intestine by palpation;
- sigmoidoscopy;
- general blood analysis;
- stool occult blood test;
- colonoscopy.
Read: Small intestine cancer: why does it occur and is it possible to cure it?
All of the above studies are carried out strictly in the order described above. Usually, the procedures mentioned are enough to confirm or refute the diagnosis of colon cancer. In other cases, the doctor may refer the patient for other, more detailed examinations:
- Ultrasound of the abdomen;
- Ultrasound of the pelvic organs;
- endorectal ultrasound;
- intestinal biopsy.
It is worth noting that a tumor formed in the lower intestine can usually be detected by palpation. However, with neoplasms that have spread to the upper part of the mentioned organ, everything is not so simple.
Often, to detect them, it is necessary to conduct more than a dozen different tests and examinations. That is why, if you discover one or more alarming symptoms that may indicate intestinal cancer, you should not neglect any of the available diagnostic procedures.
The importance of colon microflora
Bacteria live both outside (skin) and inside the human body.
Normal microflora of the human body
For the occurrence of an infectious process, the state of the macroorganism is important, along with the properties of the pathogen. It is determined by a complex set of factors and mechanisms that are closely interrelated and is characterized as susceptibility (sensitivity) or immunity (resistance) to infection.
The most important factor of nonspecific protection is the normal microflora of the skin and mucous membranes.
Normal human microflora plays an important role in protecting the body from pathogenic microorganisms. Representatives of normal microflora participate in the nonspecific protection of the areas of the gastrointestinal, respiratory, genitourinary tracts and skin that they inhabit.
Microorganisms living in certain biotopes (communities) prevent adhesion (gluing) and colonization of body surfaces by pathogenic microorganisms.
The protective effect of normal microflora may be due to competition for nutrients, changes in the pH of the environment, and the production of active factors that prevent the introduction and proliferation of pathogenic microorganisms
Microflora of the large intestine
The microflora of the large intestine is a set of bacteria that coexist with the human body. The intestinal microflora accounts for approximately 2 kg of bacteria out of 3-4 kg of total microflora, with most of them living in the large intestine.
The symbiotic microflora of the large intestine plays a significant role in the production of certain vitamins and amino acids, as well as in suppressing the growth of foreign bacteria and stopping putrefactive processes.
Intestinal microflora not only helps digestion processes, but also performs and supports human immunity.
Intestinal problems are the cause of many diseases.
Normal microflora contributes to the maturation of the immune system and maintaining it in a state of high functional activity, since the components of the microbial cell nonspecifically stimulate cells of the immune system.
Treatment with antibiotics, which changes the composition of the normal microflora, and sometimes its complete disappearance, causes severe dysbacteriosis, which significantly complicates the disease.
In cases of disturbance in the composition of biotopes or in case of a significant decrease in the natural immune defense of the body, diseases can also be caused by representatives of the normal microflora of the body.
The role of bacteria in the digestive process
Everything that enters the human body is processed, broken down and absorbed, bringing benefit or harm, but always leaves behind some waste or undigested particles. The functions of “cleaning” and “removing” in the body are performed by bacteria of the large intestine, which are part of the healthy microflora.
Our digestion largely depends on these bacteria. According to scientists, there are about five hundred different types of bacteria in the human gastrointestinal tract. Only 30-40 varieties of them are the main “workers”.
The relationship between the host organism and bacteria constitutes a harmonious symbiotic system, i.e. they are mutually beneficial. The body gives bacterial cells food and a “place in the sun,” and in return they perform the extremely important work of processing food, removing residues, strengthening the immune system, protecting against dangerous viruses, etc.
Diversity of gut bacteria
During the life of bacteria in the large intestine, organic acids are formed that lower the pH of the environment, which prevents the development of pathogenic microbes and destroys putrefactive and gas-forming bacteria.
According to health hazards, representatives of the microflora of the large intestine are divided into:
- beneficial (lactobacillus and bifidobacteria);
- opportunistic, i.e. not dangerous under certain conditions (E. coli);
- pathogenic (Proteus and staphylococci).
In the large intestine, there should normally be the following ratio of microorganisms: per 100 bifidobacteria, 1 lactobacilli and up to 10 pcs. coli. Violation of this proportion can lead to a decrease in the protective function of microflora and provoke the occurrence of various diseases.
Danger of pathogenic organisms
The action or “hibernation” of pathogens largely depends on a person’s lifestyle. With a healthy immune system, pathogenic microorganisms are suppressed and do not pose a threat.
The destruction of the body’s defenses can be provoked by:
- unhealthy lifestyle and junk food;
- alcohol or other intoxication;
- frequent ARVI;
- uncontrolled use of medications, especially hormonal drugs and antibiotics;
- stress and depression;
- other harmful factors (environmental pollution, hazardous production, etc.).
The importance of bifidobacteria
The main part of the microflora of the large intestine consists of bifidobacteria. Their main functions:
- take part in protecting the body from pathogenic microbes (forming a protective layer on the mucous membrane);
- carry out parietal digestion (in close proximity to the intestinal walls) and break down solid particles;
- synthesize amino acids, proteins and vitamins (B1, B2, B3, B6);
- stimulate the absorption of calcium, iron and vitamin D;
- increase the growth of immune cells and affect the synthesis of interferon (a protein that resists viruses);
- have an antiallergic effect, slowing down the production of histamine, which causes allergies;
- carry out detoxification - remove intestinal poisons, bind carcinogenic chemicals.
The importance of lactobacilli
Lactobacilli appear in the human body immediately after birth and colonize almost all parts of the gastrointestinal tract from the oral cavity to the large intestine.
Functions of lactobacilli:
- acidity balance;
- during the life of lactobacilli, lactic acid and hydrogen peroxide are formed, which suppress pathogenic bacteria;
- synthesis of protective substances, due to which an antibiotic barrier is formed in the stomach and small intestine;
- maintaining the immune response and targeted stimulation of immune cells;
- have an antitumor effect, suppressing the development of cancer cells.
The meaning of E. coli
Escherichia coli is an opportunistic bacteria.
Normally, with a healthy microflora, E. coli:
- breaks down lactose;
- synthesizes vitamins B and K;
- produces substances similar in action to antibiotics and stimulates the production of antibodies.
Colostomy
The surgeon creates a colostomy by suturing the end of the colon to an opening in the abdomen. This opening is called a stoma. It may be round or oval and appear red and moist.
Touching it does not cause pain, since there is no innervation. Therefore, you need to be careful not to injure her, as you may not feel that any damage has been done. After surgery, the stoma will be swollen and gradually become smaller and flatter. A colostomy bag is attached to the skin on the abdomen above the stoma.
For bowel cancer, a colostomy may be temporary. It allows the intestines to recover after tumor removal. A few months later, another operation is performed to restore the intestines and close the stoma.
A nurse at Asaf HaRofeh Hospital will teach you how to care for your stoma and how to clean and change colostomy bags.
An ileostomy is different in that the end of the small intestine is sutured to an opening in the abdominal cavity.
Imbalance of intestinal microflora
After taking antibiotics, injuries, stress, surgery, or as a result of a poor diet, the composition of the microflora may change and there will be more pathogenic bacteria. This condition is called dysbiosis. This leads to the fact that the synthesis of certain fats, enzymes and vitamins in the intestines stops, due to which the slender symbiotic system is damaged.
The human body requires immediate help to restore its lost balance. You can't just "eliminate" dangerous germs. Decreasing the number of bacteria is no better than increasing it. The main guarantee of maintaining health is maintaining the quantitative and qualitative balance of the body's microflora.
NSP products containing bifidobacteria and lactobacilli:
1. Bifidophilus Flora Force
- Restores normal intestinal microflora.
- Regulates the functioning of the gastrointestinal tract.
- Supports the body's natural defenses against bacteria and viruses.
- Normalizes the synthesis of vitamins E and K.
- Creates favorable conditions for the reproduction and growth of beneficial microorganisms.
2. “Bifidosauriki” - chewable tablets for children with bifidobacteria
- Normalize the function of the digestive system.
- Supports the body's natural defenses against bacteria and viruses.
- They create a favorable environment for the growth of beneficial microorganisms.
- Restore intestinal microflora.
Colon cancer stage 3
Like any cancer, stage 3 colon cancer poses a serious threat to human life.
This stage of the disease is characterized by more severe symptoms than the previous two, so more often the disease is detected in an advanced form.
The disease develops over several years and people live without realizing there is a problem. To prevent serious complications, you should consult a doctor for any disturbances in the gastrointestinal tract.
Stage 3 cancer has little chance of survival, so primary and auxiliary therapy should be immediately carried out to save life.
Stage 3 difference
This degree is characterized by a significant increase in the tumor, which already occupies more than the semicircle of the intestine. The tumor grows through the intestinal wall and can affect the abdominal cavity.
At this stage of the disease, it is possible that only a primary tumor may be present or regional metastases may occur that affect the lymph nodes near the tumor.
Depending on how far the damage to the lymph nodes has progressed, specialists determine how long the patient has to live.
According to statistics, if stage three cancer has not spread beyond the intestines, the chance of survival is at least 99%.
Existing complaints
Stage three intestinal cancer is suspected if the patient has the following complaints:
- Blood is visible in the stool.
- Abdominal pain, flatulence, independent of diet. Dieting doesn't help.
- Abnormal stool (constipation is replaced by diarrhea).
- After defecation, the feeling of incomplete bowel movement persists.
- The abdomen has become larger or a certain area has become enlarged.
- Decreased appetite, aversion to food. If meat dishes have become disgusting for the patient, we can talk about the presence of cancer.
- A sharp decrease in body weight, loss of strength.
- When the liver and gallbladder are affected by metastases, the patient’s skin acquires a yellow tint.
- Pain in organs affected by metastases.
- Intestinal obstruction.
Clinical picture
An enlarged tumor leads to intestinal obstruction. The intestinal lumen is blocked by a neoplasm, feces cannot move and accumulate. Intestinal distension occurs.
Therefore, this condition is accompanied by pain, flatulence and signs of intoxication: vomiting, nausea, loss of strength. When an obstruction forms, a person develops a low-grade fever (within 37.1–38.0 °C), and the abdominal muscles are tense.
Sometimes pain in the right side contributes to the erroneous diagnosis of appendicitis.
Gradually, the intensity of the symptoms increases, the pain intensifies, gas retention occurs, constipation gives way to diarrhea, and there is a strong rumbling in the stomach. Partial or complete obstruction occurs. The presence of such symptoms in people over 50 years of age requires an examination to detect cancer. Even a slight delay sometimes costs a person his life.
If third-degree cancer is suspected or a neoplasm is detected, a series of studies are carried out to determine the nature of the tumor, its type, stage of development, the presence of metastases, and damage to other organs. The following methods are used for this:
- Sigmoidoscopy. Examination of the condition of the inner surface of the rectum and sigmoid colon using a sigmoidoscope, which is inserted through the anus.
- Biopsy. A piece of tumor tissue is taken to identify cancer cells in it.
- Colonoscopy. Examination of the inner surface of the large intestine.
- X-ray, CT.
- A blood test for tumor markers determines the presence of a cancerous tumor in the body.
- Ultrasound examination reveals the presence of a tumor and metastases in other organs.
X-ray examination is the main method for diagnosing cancer, carried out as part of prevention.
Elimination of stage 3 intestinal cancer will require radical therapy.
Unlike the initial stages of the disease, treatment of stage 3 intestinal cancer requires complex measures. Surgery cannot solve the problem without additional therapy. Therefore, in this case, depending on the characteristics of the disease, radiation therapy (the so-called “irradiation”) and chemotherapy are performed.
Radiation therapy involves exposing the tumor to x-ray radiation. As a result, the growth of the tumor slows down somewhat. During chemotherapy, special drugs are introduced into the body to destroy the tumor.
But at the same time, this method also negatively affects the general condition of a person, since not only cancer cells are destroyed, the functioning of all cells of the body is disrupted.
Therapy is accompanied by side effects: vomiting, nausea, hair loss.
If the cancer has not metastasized, chemotherapy is sufficient. In the presence of metastases, radiation therapy is used. This prevents the development of more metastases, and accordingly, a person has a greater chance of survival.
In case of stage 3 disease, surgical intervention may be contraindicated due to individual characteristics. Therefore, a palliative course of radiation therapy is often carried out, including 10 “irradiation” sessions.
Folk remedies
Recently, the folk method of treating cancer with the drug “ASD-2” has become very popular. In the middle of the last century, this remedy was widely used to treat people; this drug was especially important in the army.
Then it began to be used only in veterinary medicine. Currently, with the help of ASD-2, which is an antiseptic stimulant, people are beginning to treat cancer on their own in order to avoid surgery.
The drug has no contraindications. However, in order to avoid negative consequences, you should always consult with your doctor before using it.
Based on the results obtained during the diagnosis, the doctor prescribes the necessary treatment, taking into account individual characteristics. Typically, at stage 3 of cancer development, surgery is ineffective and is performed only in case of intestinal obstruction.
If the situation allows, the entire tumor is removed through surgery, along with the affected part of the intestine and the lymph nodes affected by the pathology. This is a complex procedure that often leads to disability for the patient. It is possible to remove the intestine out through the abdominal cavity.
A fictitious anal opening is created. In this case, the patient's life expectancy is short.
Avoidance of food of animal origin and high physical activity reduces the risk of colon cancer by 10-20 times.
Since at stage 3 of the development of intestinal cancer the lymph nodes and other organs are affected, the prognosis is unfavorable. Often patients with this diagnosis live for about a year, at best no more than 3 years.
If the intestinal walls are damaged, the chance of survival is 85%. Damage to nearby lymph nodes reduces this figure to 66%. For metastases in regional lymph nodes - 35%.
The more lymph nodes affected, the worse the prognosis.
It is important to diagnose cancer as early as possible. To do this, as part of prevention, you should regularly undergo a medical examination, including, in particular, ultrasound and colonoscopy. For example, in Japan, people over 35 years of age must undergo a colonoscopy every year. Thus, the country's mortality rate from intestinal cancer has been reduced by 2 times.
High physical activity, proper nutrition, giving up bad habits, timely treatment of emerging diseases, and lack of stress significantly reduce the risk of colon cancer.
Judging by the fact that you are now reading these lines, victory in the fight against diseases of the gastrointestinal tract is not yet on your side...
Have you already thought about surgery? This is understandable, because all organs of the gastrointestinal tract are vital, and their proper functioning is the key to health and well-being. Frequent abdominal pain, heartburn, bloating, belching, nausea, bowel dysfunction... All these symptoms are familiar to you firsthand.
Importance of fiber for the colon
The benefits of fiber aren't just limited to gut health. Fiber is a means of preventing atherosclerosis, diabetes, dysbiosis and intestinal tumors, not to mention diseases such as functional digestive disorders.
The effect of fiber on the body begins in the oral cavity. Part of the low molecular weight fibers is used to nourish the microflora of the oral cavity.
In the stomach, the fibers swell and create the illusion of fullness, which helps fight overeating and obesity.
In the small intestine, fiber has a multifaceted effect: it accelerates the movement of food and slows down the absorption of carbohydrates. Slow absorption of carbohydrates is very important for both the prevention of diabetes and the prevention of obesity.
The effects of dietary fiber on the large intestine are realized through three main components:
- water holding capacity;
- binding of harmful compounds (mutagens, toxins, heavy metals);
- nutrition of beneficial microflora.
The water-retaining properties of fiber are relevant for the prevention of constipation and functional intestinal diseases.
It has now been proven that the presence of daily stool is an important factor in the prevention of colon cancer .
NSP products containing fiber
Loklo
- Is a source of dietary fiber.
- Improves intestinal motility and promotes cleansing.
- Has a prebiotic effect for intestinal microflora.
- Reduces cholesterol and blood sugar levels.
- Has an oncoprotective effect, binds and removes toxic substances
Abdominal or laparoscopic surgery in Israel
Surgery for intestinal cancer is performed using both abdominal and laparoscopic approaches.
In the first case, the surgeon makes one large incision in the abdomen to remove the tumor. Its size can range from the lower part of the sternum to the level of the pelvic bones.
During a minimally invasive operation, the surgeon makes several small incisions through which he works using a laparoscope and special instruments.
This type of surgery takes longer, but patients usually recover faster. Sometimes during laparoscopic surgery the surgeon switches to open surgery. The doctor at Asaf HaRofeh will explain in detail all the risks and benefits of these approaches.
Several medical centers in Israel have robotic systems that are used during laparoscopic surgery. Robotic surgery reduces:
- Number of transitions to abdominal surgery.
- The likelihood of complications during and after surgery.
- Length of time spent in the clinic.
If the tumor is blocking the intestines
Surgery for bowel cancer is usually planned in advance, after diagnosis. But sometimes the tumor completely blocks the organ when it is discovered. This condition is called intestinal obstruction. In this situation, surgery is required immediately.
The surgeon may place a stent during a colonoscopy. It holds the organ open so that the intestines can resume normal function. Or immediate surgery to remove the tumor may be necessary.
Parasites and the large intestine
Most parasites are found in the colon or migrate directly through it.
According to the Royal Academy of Medicine of Britain, 95% of diseases are directly or indirectly related to the colon. The Academy has identified more than 40 types of toxic substances that form in the colon.
These toxins enter the bloodstream and have a destructive effect on the body. Dr. Bernen Jensen estimates that the average person over 40 has between 2 and 12 kilograms of fecal material in their colon. In these remains that are not released, parasites of all sizes thrive, poisoning the entire body.
Parasites get the best of what their owner has, leaving him with only scraps. This is why many people who lead a healthy lifestyle and take vitamins do not experience improved health. By the way, unusual reactions to herbs in the form of discomfort, pain, rashes can also be correlated with the presence of parasites in the body.
Due to the vital activity of parasites, the body does not receive a significant amount of nutrients:
- Intoxication with waste products of helminths.
- Destruction of healthy intestinal microflora by parasites.
- Decreased immunity.
- General poor health.
- Disturbances in the functioning of the gastrointestinal tract.
- Severe damage to organs and systems, as individual consequences of helminthiasis.
Approximate diagram of an antiparasitic program.
I wish you good health!
Recommendations of nutritionist Salo I.M.
The full recording of the material on the topic “The importance and role of the large intestine for the body” can be listened to below:
Treatment methods for colon cancer and prognosis for recovery
Colon cancer is treated using three main methods:
- surgically;
- chemotherapy;
- irradiation.
The surgical method is aimed at removing the tumor itself, part of the intestine and lymph nodes. This saves the patient from the possible return of the disease. Typically, the surgical method is used only when the disease has just begun to progress.
Chemotherapy is the use of powerful drugs that can suppress cancer. The course of such therapy usually takes several weeks and also has side effects. Patients experience severe malaise, nausea, decreased immunity, and even the appearance of painful ulcers on the mucous membranes.
Radiation therapy is used in advanced stages of cancer. Using special equipment, doctors irradiate the affected part of the intestine. The duration of such therapy usually includes several weeks. Although the method is painless, patients suffer from nausea, vomiting, itchy skin and loss of appetite.
With timely initiation of treatment, the prognosis for recovery is positive. The main thing is not to waste time!