In most cases, neutropenia acts as a complication of initial diseases, but can progress independently.
A decrease in this indicator leads to a greater chance of infection by bacteria, suppresses the immune system and gives access to infectious diseases to the body. The greater the decline of neutrophils, the greater the risk of infectious and bacterial diseases.
To prescribe effective treatment, it is always necessary to establish the root cause that contributed to the development of such a condition. The disease is quite rare and occurs in one person per one hundred and fifty thousand of the population.
Depending on the severity of the disease, according to statistics, death occurs in ten to sixty percent of registered cases.
Basic concepts of NP
The main cells that saturate the body are leukocytes, one of whose functions is to identify foreign agents, suppress them and store in memory the encounter with each of the individual types of harmful proteins.
Neutrophils are found in granulocytes, which are part of white blood cells containing special granules. Compared to all other components of granulocytes, their majority are neutrophils.
That is why the term agranulocytosis (decrease in the number of granulocytes) is called the identical term neutropenia.
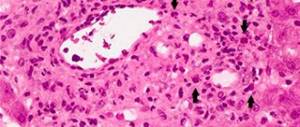
In most formations of purulent inflammatory foci, neutrophils are recorded, so their main task is to neutralize parasitic microorganisms.
The formation of purulent foci occurs due to the deformation of microbes , their tissue formations and neutrophils, which rapidly move from the blood to the site of inflammation.
Neutropenia
Types of neutropenia
The initial classification of neutropenia is based on the severity of the disease.
The following three stages are distinguished:
- Mild degree is characterized by the presence of 1000 to 1400 neutrophils per microliter of blood;
- The average degree is determined by indicators from 500 to 1000 NF;
- Severe degree – decline of NF boundaries below five hundred per microliter.
The degree is proportional to the development of burdens. The last degree of neutropenia is characterized by progression of complications.
The extreme stage is characterized by both strong inflammatory processes and its disappearance, which indicates that the granulocytes are completely depleted.
Granulocytes
What causes NP?
The progression of this pathological condition can be either an independent process or a consequence of various diseases.
Provoking factors include:
- Long-term exposure to radiation on the body;
- Congenital diseases and genetic mutations. These include congenital pathologies of immunity, disorders of granulocytes of genetic origin, etc.;
- Deformation of neutrophils due to exposure to antibodies;
- The formation of neutropenia as one of the symptoms of the initial disease (tuberculosis, bone cancer, HIV, lupus erythematosus);
- Taking certain medications (analgesics, diuretics (diuretics), anti-inflammatory drugs).
To fully understand the processes of the occurrence of the disease, we will consider each of its types separately.
Autoimmune neutropenia
It progresses due to the formation of destructive antibodies to neutrophils by the immune system. Such antibodies can be either emerging counteracting agents to other diseases, or specifically to neutrophils, if signs of other autoimmune diseases are not detected.
In most cases, this type of neutropenia is diagnosed in children with congenital pathologies of the immune system.
Severe forms of immune diseases contribute to the sudden decline of neutrophils and the rapid acquisition of diseases of infectious origin.
In newborns, neutropenia can be detected as a consequence of the transfer of antibodies from the mother when taking certain medications.
And also with a hereditary predisposition called parodic neutropenia (manifests from the first months, after which it appears every trimester).
Drug-induced neutropenia
In most cases, this type of neutropenia is registered in the adult age category. It progresses as a result of allergic reactions and toxic effects of medications. Chemotherapy, in this case, does not affect neutrophil levels in any way.
The occurrence of this type of neutropenia can occur after consuming antibiotics containing the following:
- Penicillin;
- Cephalosporin;
- Chloramphenicol;
- Certain types of antipsychotics;
- Anticonvulsants;
- Sulfonamides.
After using the above drugs, neutropenia may be recorded and monitored for seven days, after which the levels gradually normalize.
Also, manifestations of neutropenia are possible when using drugs aimed against the occurrence of seizures. In this case, in addition to all the signs of neutropenia, rashes, increased body temperature and possible hepatitis are added.
Frequent provocateurs of neutropenia are chemotherapy and ion irradiation, since during these processes, young synthesizing bone marrow cells are affected.
Indicators of neutropenia can be recorded for up to one month from the date of the procedure. During this month, you need to take special care of the high risk of infection.
Infectious neutropenia
This type of pathological decline of neutrophils often accompanies acute viral diseases. During periods of damage to the body by infectious or viral diseases, the immune system is especially weak and the progression of possible complications is most possible.
In childhood, neutropenia mainly occurs in the form of neutrophils adhering to the walls of blood vessels. This species is short-lived and disappears after seven days.
A severe form of the pathological disease infectious neutropenia is HIV, sepsis and other serious complications, in which not only the disruption of NF synthesis progresses, but also the deformation of neutrophils in the body.
Febrile neutropenia
The main reason that provokes the progression of this type of neutropenia is a severe infectious disease, which begins when the use of cytostatics is prescribed. With this process, harmful microorganisms multiply at a time when the immune system is weak.
In rare cases, it is caused by chemotherapy and other forms of cancer treatment.
The causative agents of this type of neutropenia can be caused by microbes that are not a threat to many people (streptococci, herpes, etc.), but when they develop, in conditions of a small number of neutrophils, they lead to serious infectious diseases and death.
Basically, it can be determined by a rise in temperature, general weakness, and obvious signs of intoxication.
In this case, inflammatory foci are difficult to diagnose, since the immune system hardly reacts. The diagnosis is made by exclusion.
Benign neutropenia
This condition is a chronic condition and is common in children. It lasts for more than two years without showing symptoms or requiring therapy. Diagnosis of this type of neutropenia consists of determining low neutrophils, but normal other blood parameters.
It does not affect the development and growth of the child in any way. Bone marrow failure is the main version of doctors regarding the progression of such neutropenia.
How to determine the manifestation of NP?
The manifestation of symptoms when the body is affected by neutropenia is more clearly manifested in more severe stages of the disease. The main symptoms manifested are very similar to a blood disease in which the functioning of the bone marrow is inhibited.
Signs by which neutropenia can be determined are:
- Ulcers with tissue death inside, located on the skin, mouth, chest and soft tissues;
- Swelling of the oral cavity, its redness;
- Covering the oral cavity with a white or yellow coating;
- Necrotic ulcers in the intestines;
- Pneumonia;
- Cough;
- A sharp increase in temperature;
- The appearance of boils;
- Acute pain in the abdominal area, with a clearly defined pain point;
- Nausea and vomiting, regardless of food intake;
- Constipation;
- Fever;
- Headache;
- Pain in the joints.
As drug-induced neutropenia progresses, the most severe symptoms and the highest mortality rate occur. In the acute period of the disease, death occurs in thirty percent of cases.
With the development of neutropenia at the initial stages, symptoms are not visible. If neutropenia is suspected, it is necessary to carefully examine the oral cavity, skin, anus, places of insertion of catheters and vascular punctures, and also palpate the abdomen.
To make an accurate diagnosis, you need to take laboratory blood tests.
Survey[edit | edit code]
A patient with febrile neutropenia or suspected of having it should be immediately carefully examined. It is mandatory to take samples of blood, urine, feces, sputum, vomit or other available biological fluids of the patient for bacterioscopic and bacteriological examination, as well as emergency radiography of the lungs, a thorough examination of the pharynx and nasopharynx, skin and accessible mucous membranes, perianal area, examination and palpation lymph nodes, careful auscultation of the lungs.
Norms
In a normal state, the quantitative indicator of neutrophils is from forty-five to seventy-five percent (or about 1500 per microliter of blood) of all leukocytes. It is the quantitative indicator of NF in the blood that plays an important role, since the number of other components of leukocytes can fluctuate, but the levels of neutrophils remain normal.
Normal rates vary slightly depending on a person's race. So in dark-skinned people, neutropenia is diagnosed when neutrophils decrease to less than 1200 per 1 microliter of blood. This happens because people with this skin color have lower neutrophil levels than white-skinned people.
The greater the deficiency of these components in leukocytes, the more pronounced the clinical manifestations and the greater the risk of progression of life-threatening complications. Severe forms of this disease are rarely recorded.
Normal NF indicators for childhood are shown in the table below:
| Total leukocytes | Neutrophils | Lymphocytes | Monocytes | Eosinophils | ||||||||
| Age | average | range | average | range | % | average | range | % | average | % | average | % |
| birth | 18.1 | 9—30 | 11 | 6—26 | 61 | 5.5 | 2—11 | 31 | 1.1 | 6 | 0.4 | 2 |
| 12 hours | 22.8 | 13—38 | 15.5 | 6—28 | 68 | 5.5 | 2—11 | 23 | 1.2 | 5 | 0.5 | 2 |
| 24 hours. | 18.9 | 9.4—34 | 11.5 | 5—21 | 61 | 5.8 | 2—11.5 | 31 | 1.1 | 6 | 0.5 | 2 |
| 1 Week | 12.2 | 5—21 | 5.5 | 1.5—10 | 45 | 5 | 2—17 | 41 | 1.1 | 9 | 0.5 | 4 |
| 2 week | 11.4 | 5—19.5 | 4.5 | 1—9.5 | 40 | 5.5 | 2—17 | 48 | 1 | 9 | 0.4 | 3 |
| 1 month | 10.8 | 6—17.5 | 3.8 | 1—9 | 35 | 6 | 2.5—16.5 | 56 | 0.7 | 7 | 0.3 | 3 |
| 6 months | 11.9 | 6—17.5 | 3.8 | 1—8.5 | 32 | 7.3 | 4—13.5 | 61 | 0.6 | 5 | 0.3 | 3 |
| 1 | 11.4 | 6—17 | 3.5 | 1.5—8.5 | 31 | 7 | 4—10.5 | 61 | 0.6 | 5 | 0.3 | 3 |
| 2 | 10.6 | 5.5—15.5 | 3.5 | 1.5—8.5 | 33 | 6.3 | 3—9.5 | 59 | 0.5 | 5 | 0.3 | 3 |
| 4 | 9.1 | 5.0—14.5 | 3.8 | 1.5—8.5 | 42 | 4.5 | 2—8 | 50 | 0.5 | 5 | 0.3 | 3 |
| 6 | 8.5 | 5—13.5 | 4.3 | 1.5—8 | 51 | 3.5 | 1.5—7 | 42 | 0.4 | 5 | 0.2 | 3 |
| 8 | 8.3 | 4.5—13.5 | 4.4 | 1.5—8 | 53 | 3.3 | 1.5—6.8 | 39 | 0.4 | 4 | 0.2 | 2 |
| 10 | 8.1 | 4.5—13.5 | 4.4 | 1.8—8 | 54 | 3.1 | 1.5—6.5 | 38 | 0.4 | 4 | 0.2 | 2 |
| 16 | 7.8 | 4.5—13 | 4.4 | 1.8—8 | 57 | 2.8 | 1.2—5.2 | 35 | 0.4 | 5 | 0.2 | 3 |
| 21 | 7.4 | 4.5— 11.0 | 4.4 | 1.8—7.7 | 59 | 2.5 | 1—4.8 | 34 | 0.3 | 4 | 0.2 | 3 |
febrile neutropenia
V.A. Okhmat, G.A. Klyasova, E.N. Parovichnikova, V.V. Troitskaya, E.O. Gribanova, V.G. Savchenko
Federal State Budgetary Institution "National Medical Research Center for Hematology" of the Ministry of Health of Russia, Novy Zykovsky Prospect, 4, Moscow, Russian Federation, 125167
For correspondence: Vladimir Aleksandrovich Okhmat, Ph.D. honey. Sciences, Novy Zykovsky pr-d, 4, Moscow, Russian Federation, 125167; tel.; e-mail
For citation: Okhmat V.A., Klyasova G.A., Parovichnikova E.N. and others. The use of antibiotics for febrile neutropenia in patients with acute leukemia. Clinical oncohematology. 2018;11(1):100-9.
DOI: 10.21320/2500-2139-2018-11-1-100-109
ABSTRACT
Target. To evaluate the results of antibiotic use for febrile neutropenia in patients with acute myeloid (AML) and acute lymphoblastic leukemia (ALL).
Materials and methods. The prospective study (2013–2015) included 66 patients with AML and 44 with ALL who received 480 courses of chemotherapy over 6 months.
Results. Febrile neutropenia was recorded in 242 (50%) chemotherapy courses, more often in patients with AML than ALL (93 vs 18%; p < 0.0001). In patients with AML, infections predominated in induction and consolidation (98 vs 89%), in ALL - in induction (55%). In patients with AML compared to patients with ALL, cure from infections was less common when using first-stage antibiotics in monotherapy (24 vs 57%; p <0.0001), but more often when adding drugs from other groups (37 vs 18%; p = 0.01). The effect of prescribing β-lactam antibiotics in patients with AML was less common at the induction stage than at the consolidation stage (47 vs 72%; p = 0.0004). For granulocytopenia for more than 14 days, the response rate with the use of first-stage antibiotics and carbapenems was 23–24%, and in 47% of cases it was recorded with the addition of other antimicrobial drugs, most often antifungals (21%). For fever of unknown etiology, a response was observed with the use of stage 1 antibiotics in monotherapy (45%). In case of clinically and microbiologically proven infection, a significant proportion of cures were observed when β-lactam antibiotics were combined with other drugs (43%).
Conclusion. In patients with ALL and fever of unknown etiology, an escalation strategy of antibiotic use should be considered optimal. In patients with AML at the induction stage, in cases of prolonged neutropenia (> 14 days), and with clinically and microbiologically proven infections, the effectiveness of β-lactam antibiotics in monotherapy is lower. In 37–48% of cases, cure was recorded with the addition of other antimicrobial drugs.
Key words: acute leukemia, AML, ALL, febrile neutropenia, fever of unknown etiology, clinically and microbiologically proven infection, antibiotics.
Received: July 2, 2020
Accepted for publication: October 20, 2020
Read article in PDF
LITERATURE
- Parovichnikova E.N., Troitskaya V.V., Klyasova G.A. et al. Treatment of patients with acute myeloid leukemia according to the protocol of the Russian multicenter randomized trial AML-01.10: results of the coordinating center. Therapeutic archive. 2014;86(7):14–23.
- Parovichnikova E.N., Klyasova G.A., Isaev V.G. and others. First results of therapy for Ph-negative acute lymphoblastic leukemia in adults according to the protocol of the Research Group of Hematological Centers of Russia ALL-2009. Therapeutic archive. 2011;83(7):11–7.
- Voitsekhovsky V.V., Gruzdova A.V., Filatova E.A. and others. Analysis of infectious complications of hemoblastosis in the Amur region. Bulletin of physiology and pathology of respiration. 2012;46:64–8. [Voitsekhovskii VV, Gruzdova AV, Filatova EA, et al. The analysis of infectious complications of hemoblastosis in the Amur region. Byulleten' fiziologii i patologii dykhaniya. 2012;46:64–8. (In Russ)]
- Mikulska M, Viscoli C, Orasch C, et al. Aetiology and resistance in bacteraemias among adult and pediatric haematology and cancer patients. J Infect. 2013;68(4):321–31. doi: 10.1016/j.jinf.2013.12.006.
- Klyasova G.A. Antimicrobial therapy. In the book: Software treatment of diseases of the blood system: a collection of diagnostic algorithms and protocols for the treatment of diseases of the blood system. Ed. V.G. Savchenko. M.: Praktika, 2012. pp. 827–54.
- Averbuch D, Cordonnier C, Livermore DM, et al. Targeted therapy against multi-resistant bacteria in leukemic and hematopoietic stem cell transplant recipients: Guidelines of the 4th European conference on Infections in Leukemia (ECIL-4, 2011). Haematologica. 2013;98(12):1836–47. doi: 10.3324/haematol.2013.091330.
- Tumbarello M, Sanguinetti M, Montuori E, et al. Predictors of mortality in patients with bloodstream infections caused by extended-spectrum-β-lactamase-producing Enterobacteriaceae: importance of inadequate initial antimicrobial treatment. Antimicrob Agents Chemother. 2007;51(6):1987–94. doi:10.1128/AAC.01509–06.
- Savchenko V.G., Parovichnikova E.N., Afanasyev B.V. and others. National clinical guidelines for the diagnosis and treatment of acute myeloid leukemia in adults. Hematology and transfusiology. 2014;59(S2):2–29.
- Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
- Averbuch D, Orasch C, Cordonnier C, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica. 2013;98(12):1826–35. doi: 10.3324/haematol.2013.091025.
- Klyasova G.A., Korobova A.G., Frolova I.N. and others. Detection of enterobacteria with the production of extended spectrum β-lactamases in patients with acute myeloid leukemia and lymphoma upon admission to the hospital. Hematology and transfusiology. 2016;61(1):25–32. doi: 10.18821/0234-5730-2016-61-1-25-32.
- Okhmat V.A., Klyasova G.A., Korobova A.G. and others. Should carbapenems be prescribed to all patients with febrile neutropenia and colonization with enterobacteriaceae producing extended-spectrum β-lactamases? Oncohematology. 2016;11(3):49–57. doi: 10.17650/1818-8346-2016-11-3-49-57.
- Aynioglu Mujeeb VR, Jambunathan P, Tyagi A. Comparison of Efficacy of Piperacillin/Tazobactam Vs Cefoperazone/Sulbactam as Empirical Therapy in Patients with Febrile Neutropenia. Ann Int Med Dent Res. 2017;3(2):51–5. doi: 10.21276/aimdr.2017.3.2.me12.
- Demir HA, Kutluk T, Ceyhan M, et al. Comparison of sulbactam-cefoperazone with carbapenems as empirical monotherapy for febrile neutropenic children with lymphoma and solid tumors. Pediatric Hematol Oncol. 2011;28(4):299–310. doi: 3109/08880018.2011.552937.
- Jing Y, Li J, Yuan L, et al. Piperacillin-tazobactam vs. imipenem‐cilastatin as empirical therapy in hematopoietic stem cell transplantation recipients with febrile neutropenia. Clin Transplant. 2016;30(3):263–9. doi:1111/ctr.12685.
- Okhmat V.A., Klyasova G.A., Parovichnikova E.N. and others. Spectrum and etiology of infectious complications in patients with acute myeloid leukemia at the stages of induction and consolidation of remission. Hematology and transfusiology. 2017;62(1):9–15.
- Pizzo PA. After empiric therapy: what to do until the granulocyte comes back. Rev Infect Dis. 1987;9(1):214–9. doi: 1093/clinids/9.1.214.
- Link H, Maschmeyer G, Meyer PF, et al. Interventional antimicrobial therapy in febrile neutropenic patients. Ann Hematol. 1994;69(5):231–43. doi: 1007/BF01700277.
- Viscoli C, Cometta A, Kern WV, et al. Piperacillin-tazobactam monotherapy in high-risk febrile and neutropenic cancer patients. Clin Microbiol Infect. 2006;12(3):212–6. doi: 10.1111/j.1469-0691.2005.01297.x.
How is it diagnosed?
To make an accurate diagnosis, if neutropenia is suspected, the doctor will refer the patient for laboratory blood tests. The most common methods of blood testing for neutropenia include:
- Complete blood count (CBC ). Helps determine the quantitative state of granulocytes;
- Biochemical blood test (BAC). It is a more informative method of blood testing than a clinical blood test;
- Study of the hematopoietic function of the bone marrow . It is of greatest importance in which it is possible to evaluate the inhibition of any of the hematopoietic germs and identify why this happened;
- Double blood culture. Blood cultures are performed to check for the presence of pathological bacteria and fungal agents;
- Sowing the contents from the drainage outlet . It is performed in patients who have undergone surgery;
- Stool examination. It is recommended to examine stool for infectious diseases, when stool is weak, after surgery;
- Myelogram. The result of microscopy of a bone marrow smear, expressed in the form of a table or diagram, which determines the qualitative and quantitative components of cell nuclei in myeloid tissues;
- Hemogram.
Diagnosis methods depend on the general condition of the patient and the suspicions of the attending physician.
How is NP treated in adults?
There is no one specific treatment regimen for neutropenia, since the symptoms are different for everyone and are provoked by different diseases. The severity of therapy depends on the age category of the patient, the nature of the bacteria that provoked the inflammation and the general health of the patient.
If the disease is mild, no treatment is required, and exacerbations that sometimes occur are treated with the same methods as for other affected people.
When diagnosing a severe form of neutropenia, constant medical supervision is required, twenty-four hours a day, so hospitalization cannot be avoided.
If the body is affected by diseases of infectious origin, the following groups of drugs are prescribed:
- Antifungal;
- Antiviral;
- Antibacterial.
The dosage at the treatment stage is significantly higher than during the prevention of the disease.
The prescription of a particular drug mainly depends on the individual reaction of the body to the tolerance of a particular medication.
The main methods of therapy are:
- Broad spectrum antibiotics. They are used until the doctor determines what is perceived best by the body. Such drugs are administered into a vein.
We are talking about improving the condition and using an effectively selected drug if the patient’s health improves in the first three days from the start of treatment. If no progress is observed, the dose is increased or another treatment is used;
When neutropenia progresses from radiation or chemotherapy, antibiotics are prescribed until the levels of NF in the blood reach at least five hundred neutrophils per microliter of blood:
- Preparations of the fungicide group (Amphotericin) are used if fungal infections are added to infectious diseases, but fungicides are not used for preventive actions against fungal agents;
- Colony-stimulating drugs (Filgastrim) . Used for severe forms of neutropenia, as well as for children with congenital abnormalities of the immune system;
- Vitamins (folic acid). Prescribed as maintenance therapy;
- Glucocorticosteroids . Prescribed when neutropenia is provoked by immune diseases;
- Medicines that improve metabolic processes in the body (Methyluracil, Pentoxyl). Prescribed as maintenance therapy.
In the case of a large number of deformed neutrophils in the cavities of the spleen, it is likely to be removed, but in severe forms of neutropenia, surgery is contraindicated.
The definitive treatment consists of surgery, which consists of a bone marrow transplant.
The treatment method is the most dangerous, but the most effective.
Symptoms
Febrile neutropenia is defined as a sudden (over several hours, and sometimes even several tens of minutes) increase in the patient's temperature above 38 ° C, against the background of a decrease in the absolute number of circulating neutrophils below 500 per cubic millimeter or the absolute number of circulating granulocytes below 1000 per cubic millimeter. This is characterized by severe general weakness, chills, and severe general condition. Possible heavy sweating, tremor (as a result of chills), tachycardia, hypotension, up to signs of cardiovascular collapse or shock.
Moreover, since with such a critical decrease in the number of neutrophils, the body’s inflammatory response to infection is sharply suppressed, it is not possible to quickly detect the source of infection, the cause of the increase in temperature. The patient’s lungs are “clean” (no wheezing), there are no symptoms from the pharynx, nasal passages, urinary tract or gastrointestinal tract, no soft tissue abscesses or pustular skin lesions are detected. These lesions can appear much later, sometimes shortly before the death of the patient, when the intensity of the infection becomes so great that even in a situation of deep suppression of the immune system, an inflammatory reaction will appear.
Thus, the diagnosis of “febrile neutropenia” is a “diagnosis of exclusion”, a diagnosis that is made when it is impossible to quickly establish the cause of an increase in temperature in a patient with neutropenia, or to find a focus of inflammation. If a specific cause for the increase in temperature is discovered, the diagnosis changes to a more accurate one (for example, we may be talking about pneumonia or bacterial sepsis against the background of neutropenia).
What is characteristic of NP in childhood?
The manifestation of poor bone marrow function is a major factor in the progression of neutropenia. In newborn children, neutrophil levels in the blood are diagnosed as neutropenia when their level drops to less than one thousand neutrophils per microliter of blood.
As the child grows, the norm increases and is set at one and a half thousand.
In the first year of life, the progression of neutropenia is characterized by an acute course or occurs chronically (with an increase in symptoms over several months).
Only three types of neutropenia are recorded in children:
- Benign neutropenia of chronic type;
- Neutropenia provoked by the immune system;
- Hereditary predisposition and genetic mutations.
With mild neutropenia, in childhood, a slight decline in the quantitative indicator of neutrophils is recorded, and obvious symptoms, in many cases, do not appear. In some cases, there are frequent recurrent infectious diseases of an acute form, which tend to last a long time and are complicated by the presence of bacteria in the body.
In this case, effective therapy is medicines against viruses and medicines aimed at combating bacteria.
In the moderate stage, frequently recurring purulent inflammations are noted, and even the registration of an infectious shock state.
In the extreme stage of NP in children, severe intoxication, fever, and purulent inflammation are always manifested, localized in the chest, abdomen and oral cavity. If effective treatment is not applied, death often occurs.
For correct diagnosis, the following points must be observed:
- When registering purulent foci with tissue death, it is necessary to carry out a blood culture to determine the microorganisms that provoke this condition;
- For symptoms of moderate severity, a myelogram study should be performed;
- Determination of all signs of neutropenia and a careful first examination of the child;
- Identification of hereditary predisposition factors;
- If neutropenia is viral, blood serum should be examined;
- Every week it is necessary to do a clinical blood test and monitor all types of blood cells.
When a child’s body is affected by hereditary neutropenia, the general criteria are:
- Detection of genetic defects using biological examinations;
- The manifestation of obvious deviations, both externally and in test results, in the first three months after the birth of the child;
- Heavy heredity.
Serious forms of hereditary neutropenia include the following:
Myelocachexia. With this type of neutropenia, there is a slow release of neutrophils from the bone marrow. This species is characterized by the accelerated breakdown of granulocytes into cells in the bone marrow and a low motor response of microorganisms to a chemical stimulus.
In the first year of life, the newborn has a relative lack of neutrophils and a clear increase in eosinophils, as well as a high level of monocytes in the blood.
When the body is damaged by bacteria, a pronounced decline in leukocytes in the blood is recorded.
Kostman's syndrome. It is a severe form of hereditary NP, which is characterized by the transmission of a pathological gene. A separate morbidity rate is also observed. When a child is affected by this syndrome, frequent damage to the child’s body occurs due to infectious and bacteriological diseases, which tend to recur frequently.
With this pathological condition, a clear decline in the number of neutrophils in the blood is recorded, sometimes reaching levels below three hundred NF per microliter of blood. Children affected by this syndrome are at risk for progression to leukemia.
When this disease is diagnosed in childhood, certain therapy is prescribed, which must be taken throughout life. Colony-stimulating drugs (Filgrastim) are used for therapeutic purposes.
If this group of medications does not have the desired effect, then bone marrow transplantation is recommended, which is performed through surgery.
Cyclic neutropenia. It is a rather rarely diagnosed form of neutropenia, which is inherited. A characteristic difference from other types of neutropenia is an intermittent course, with the presence of periodic complications. This name has a clear framework for the repetition of exacerbations (usually from three to eight days) with breaks between attacks of two to three weeks.
When an exacerbation occurs, deviations appear in laboratory tests due to a sudden decrease in the number of neutrophils, and the concomitant growth of monocytes and eosinophils, as well as the appearance of formed purulent foci in different places of the body.
During periods of remission, the child’s general health is restored, and all test abnormalities return to normal. A distinctive method of treating this type of neutropenia is the use of colony-stimulating factors 48 hours before the onset of a possible exacerbation.
The duration of therapy depends on how quickly the granulocyte count in the blood is restored.
Diagnostics
Famous children's doctor E.O. In the diagnostic process, Komarovsky calls for paying attention to symptoms such as fever and infections: pneumonia, sinusitis, lymphadenitis and stomatitis.
In his opinion, they are the first manifestations of neutropenia. In addition, it is important to pay attention to precipitating factors, frequency of illness and infections observed in family members.
The disease is diagnosed by counting blood cells
It is necessary to conduct laboratory tests, which include donating blood twice a week for six months. This approach will allow us to identify periodic hereditary neutropenia. It is important to compare recent tests with previous tests to rule out a congenital form. If necessary, bone marrow and antineutrophil antibodies are examined.
Prevention
To prevent the progression of neutropenia, it is necessary to follow simple rules that will protect not only from this disease, but also from many others.
These include:
- Normalize your daily routine , allocating time for proper sleep (at least 8 hours);
- Moderate exercise for 30 minutes every day;
- It is recommended to engage in light sports (physical education, swimming, etc.) , and also devote at least one hour a day to walking;
- Avoid strenuous physical activity;
- Eat properly . The diet must be balanced so that the body receives all the necessary nutrients and microelements;
- Maintain the body at normal temperature . The body should not get too cold or too hot;
- Avoid stressful situations . Eliminate strong emotional stress (both positive and negative), constant stress;
- Get rid of bad habits . Toxins supplied with alcoholic beverages and cigarettes have a detrimental effect on the body.
Experts' forecast
With timely access to the hospital, proper examination and rapid selection of effective complex therapy, the outcome is favorable.
If neutropenia is a symptom of another disease, then the course of treatment is aimed at eliminating the root cause. In severe forms, hospitalization and constant monitoring by health workers are necessary.
As well as a number of laboratory examinations aimed at determining the damaging factor. Only during hospitalization will the doctor be able to select the most appropriate medications , since each body reacts to certain types of medications individually.
If ignored or ineffective treatment, serious blood diseases progress, which after severe stages will lead to death.
To prevent diseases and timely diagnose them in the early stages, you need to take an annual blood test, undergo examinations and go to the hospital at the first symptoms.
Treatment of the disease
Treatment of the disease depends entirely on the cause that led to its occurrence. This means that most often the infection must be treated. The doctor decides in what conditions to carry out treatment, inpatient or at home.
Medicines include vitamins, antibiotics and drugs aimed at strengthening the immune system. If the disease is very severe, the patient is placed in an isolated room in which sterile conditions are maintained and ultraviolet radiation is provided.
After discussion, the conclusion suggests itself: a symptom arises - run to the doctor. But in order to detect a symptom, you need to be more attentive to your health, which does not tolerate self-indulgence.