Sepsis in a newborn child is an infectious disease, the appearance of which is preceded by the penetration of pathogenic bacteria through a primary (digestive tract, nasopharynx, skin wounds) or secondary (metastatic pathway) focus. Pathogenic microflora spreads throughout the body (through all organs and tissues of the child) through the bloodstream and lymphatic tract. Neonatal sepsis develops most often in premature babies, since their mucous membranes, immune system and barrier functions of the baby’s skin do not have time to form properly.
Causes
Until the fourth day of life (early sepsis in newborns), the cause of the disease is most often E. coli, group B streptococci, ECHO and Coxsackie enteroviruses, enterococci, enteroviruses or cytomegaloviruses. The later course of sepsis in newborns is usually associated with Staphylococcus aureus, Haemophilus influenzae, group B streptococci, Staphylococcus aureus, Listeria and Escherichia coli.
Sepsis in a newborn
If we talk about the early onset of the disease, the most common cause of sepsis in newborns is gram-negative microbes. Its later occurrence most likely indicates the presence of gram-positive flora in the body (in recent years it has been more common). Premature babies are characterized by a combination of various microorganisms, as well as a change in their predominance in the body (the primary virus is suppressed by a secondary infection).
Infection of the fetus and newborn child can occur antenatally, after childbirth or during childbirth. Of great importance in this case is the health of the mother (the presence of certain chronic infectious diseases), the fact of obstetric intervention, the presence of endometritis and third-party purulent-inflammatory foci, as well as a prolonged anhydrous period.
Predisposition to the appearance of the disease is damage to the skin of a newborn child during obstetric operations, its immaturity, the presence of intracranial postpartum trauma in the newborn or intrauterine hypoxia in the mother.
Signs of the disease
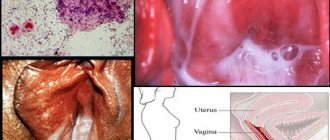
They can be, as already mentioned, very diverse and are determined by the form of the disease. There are several classifications of sepsis. According to the severity of inflammation, septicemia and septicopyemia are distinguished.
Septicemia is a type of disease in which the signs of inflammation are not very pronounced, the first place being a violation of the general condition of the child. However, it is not always possible to identify the source of infection. With septicopyemia, everything is exactly the opposite. Sepsis is also classified according to the type of microorganism that caused it. Finally, the third major classification is based on the source of the pathogen. There are burn sepsis (the pathogen has invaded the site of burned skin), umbilical sepsis, wound sepsis, etc. A special type in this classification is the so-called cryptogenic sepsis, in which the source of infection cannot be detected. Most often this happens with septicemia. A separate disease that is becoming the most common and severe complication of sepsis is septic shock.
Firstly, when describing the signs of sepsis, they should be divided into two large groups: early, which in some cases make it possible to make a diagnosis as early as possible and prescribe adequate treatment, and late, which allow us to judge the duration and severity of the disease.
Early signs appear first and allow, if not to make an accurate diagnosis, then to suspect the presence of sepsis in a child. The very first early sign is the presence in the child’s body of any infectious process, which is a source of microbes. In newborns, this is most often purulent inflammation of the umbilical cord. But the presence of such a lesion does not indicate the presence of sepsis in itself. To make a diagnosis, it must certainly be combined with another important sign - a very serious general condition of the child. The child becomes lethargic, gets tired quickly, and motor activity is significantly reduced. His skin is pale and dry. Body temperature is elevated, sometimes to very significant levels. Heartbeat is weak and rapid. Breathing is rapid. As you can see, such signs can be observed not only with sepsis, but also with a huge variety of other diseases, even with a banal respiratory viral infection. Therefore, making a diagnosis can sometimes be very difficult; special criteria are currently being developed, based on which a doctor could fairly accurately differentiate between sepsis and other diseases. However, an experienced specialist, having noticed a combination of the two above manifestations, can sometimes very quickly and accurately make a diagnosis. If the situation remains unclear, then the child must be under constant supervision, the slightest changes in his condition must be taken into account and assessed. This is especially important for newborns, since their defense mechanisms are very imperfect and their condition can deteriorate to an extremely serious condition in a very short time.
Another large group of signs are the so-called late ones. They do not develop immediately, but as the disease progresses. Their development is associated with disorders of various organs and systems, which can be very diverse.
The nervous system is always affected, and in young children it is primarily affected. These violations manifest themselves in a variety of ways. The child becomes lethargic, drowsy, loses appetite, and is practically indifferent to surrounding objects. In some cases, especially in the initial stages of the disease, he, on the contrary, is agitated, whiny, and refuses to eat. Very often, a small child responds to the septic process by developing convulsive seizures. Disorders develop in the muscles of the arms and legs, they become weak, sluggish, and their strength is reduced. In severe cases of sepsis, signs of inflammation in the meninges appear: the child suffers from a severe headache, which intensifies when exposed to bright light or loud sound. Older children are in bed in a peculiar position, which is called the “pointing dog pose”: the child lies on its side, the head is straightened, the legs are somewhat tucked towards the body, the entire spine is curved in the form of an arc. Impairments of consciousness often develop, which can be of varying degrees of severity - from mild stupor to coma.
The cardiovascular system
Violations manifest themselves in the form of toxic and infectious lesions of the heart. Blood pressure drops, pulse becomes weak and frequent. The appearance of a child is characteristic: his skin becomes pale, the tips of his fingers and toes, his nose and earlobes acquire a bluish tint. Sometimes the skin may have a characteristic café-au-lait color. When listening to the heart, its work is weak, it beats frequently, and various additional noises can be heard. Violations of the blood vessels are caused by damage to their walls, as a result of which they easily rupture and a lot of hemorrhages appear on the child’s skin. Changes in the child’s blood pressure and pulse are very characteristic. Blood pressure in young children, due to imperfect mechanisms of its regulation, can drop to very low values, even to the point of loss of consciousness. The pulse increases in accordance with the rule: with an increase in body temperature by one degree, the heart rate increases by 10 beats per minute. The most severe complication of the heart in sepsis is the development of heart failure - cyanosis of the skin, swelling, shortness of breath, significant impairment of the general condition, enlarged liver, and bleeding from the gastrointestinal tract occur.
Respiratory system
At first, with the development of sepsis, the frequency of respiratory movements decreases slightly due to general muscle weakness, and then, as the above changes in the heart and blood vessels increase, it begins to increase. As a result, shortness of breath appears, which at first occurs only during physical exertion (in young children - during excitement, crying), and then constantly, even at rest. The mechanisms of breathing regulation in young children are also not yet developed, so they can very often develop severe breathing disorders, up to a complete stop.
Digestive system
The functions of all digestive organs during sepsis are greatly reduced. As a result, the child’s appetite decreases, he refuses to eat, but consumes a lot of fluid due to the rise in body temperature. Very often, young children develop vomiting and diarrhea as a reaction to a severe infection. The intestinal protective barriers are weakened, which contributes to the development of dysbiosis.
Kidneys
In sepsis, kidney damage manifests itself in a decrease in their function. The amount of urine excreted during the day begins to gradually decrease and during the height of the disease may be practically absent. At the same time, harmful metabolic products, which are normally excreted by the kidneys, accumulate in the body and further disturb the child’s condition. Swelling develops. Therefore, with severe manifestations of renal dysfunction, children should not be given liquid in large quantities. Gradually, as the child’s condition normalizes, kidney function also normalizes. The amount of urine gradually increases and returns to normal levels. With a long course of sepsis, kidney functions cannot be restored, and sometimes their impairment can become irreparable. During the disease, changes in urine tests are observed in the form of an increase in the number of leukocytes.
Also, the signs of the disease can vary significantly depending on the form of the disease.
Septicemia is a type of sepsis in which the body’s reaction to the introduction of the pathogen is very pronounced, while the signs of a purulent disease are very mild. The severity of a child’s condition is determined not so much by the presence of pathogenic microorganisms in the body, but by the excessive reaction of the body itself to their introduction. The source of the disease where the microbes are located often cannot be found. The violation of the general condition of the child is very pronounced. Body temperature rises to very high values, fever develops. This form of sepsis is also called fulminant, since its manifestations develop very quickly. In some cases, if medical care is not provided within a fairly short period of time, the child’s death occurs.
Septicopyemia develops when the body is infected with very aggressive pathogens or with a significant decrease in immune strength. Inflammation comes first, while the disruption of the general condition is not so pronounced. You can always find a purulent focus of inflammation in the body, which serves as a source for the spread of microorganisms. In addition, within a very short time, the same foci appear in a wide variety of organs and tissues. The body's response to infection is normal or even reduced. Bacteriological examination reveals a combination of several different types of microorganisms. The septicopyemic form of sepsis is especially common in premature infants, children in a state of immune deficiency as a result of previous diseases, and children who have suffered harmful effects while in the womb. The disease in these groups of children is very severe, affecting various organs and systems. A particularly unfavorable sign in sepsis is low body temperature, which indicates a profound deficiency of immune mechanisms. Such children begin to lose significant weight to the point of complete exhaustion, and they often develop anemia. Purulent foci are present in large quantities in all organs: skin (carbuncle, abscess), lungs (abscess, pneumonia), heart, kidneys (multiple pustules, abscess), brain (purulent meningitis).
With a long course, sepsis can become chronic, which is characterized by the same manifestations as septicopyemia, but they are much less pronounced. A certain semblance of equilibrium is established between the body of a sick child and the causative agent of the disease, in which neither one nor the other can finally “win.” The pathogen has adapted to exist among the body's immune forces, while the child's organs have adapted to function more or less normally in the presence of pathogenic microbes. But such a balance is in itself very precarious and at any moment can easily shake in one direction or another. A complete recovery may occur, but much more often there is activation of the microorganism and the development of severe complications.
In order for the disease to enter the chronic phase, two main factors must be present:
- insufficiency of the body's immune forces;
- destruction of a large number of tissues in the patient’s body.
A very weak immune response is observed in cases where the child’s body has already “met” this pathogen during the period when it was in the womb. As a result, the immune system has already adapted to these microbes and does not consider them as dangerous. During the chronic phase of sepsis, most antibiotics, unfortunately, are ineffective. The use of hormonal drugs in newborns during sepsis is very dangerous. They, while causing a large number of complications if used irrationally, at the same time contribute to the transition of sepsis into a chronic form because they suppress the immune system.
The processes occurring in the body during chronic sepsis are very complex and diverse, so treating it is quite a difficult task.
Septic shock is a complication of sepsis. But this issue is very relevant due to the fact that this pathology develops quite often, leading to profound impairment of the functions of the child’s body, and sometimes even to his death. This complication can develop with sepsis at any time, in any form. The cause of the occurrence is the simultaneous entry into the child’s blood of a large number of microbial toxins and tissue breakdown products, as a result of which a reaction similar to an allergic one develops. This happens when more aggressive pathogens join existing pathogens, when the natural immune barrier around the source of inflammation is disrupted, or when there is a significant drop in the body’s immune forces. At the same time, all the signs of sepsis remain, often creating the impression that the child is feeling better. But after such a “bright interval” very severe disorders develop. The patient's blood pressure drops very sharply, he loses consciousness, and his body temperature rises significantly. Signs characteristic of allergies develop: redness of the skin, allergic swelling, breathing problems, etc. Disorders of the functions of all organs and systems develop. The most severe changes are observed in the blood coagulation system, in which, on the one hand, a large number of blood clots form in small vessels, and on the other, blood coagulability drops sharply, as a result of which bleeding from internal organs easily develops.
If septic shock develops, the child needs immediate specialized care. If this is not provided, his death occurs.
Septic shock is one of the so-called general complications of sepsis, during the development of which the entire body is affected. There are also a number of local complications that affect only one or another organ. These include the following.
- Thrombophlebitis is an inflammation of the walls of a vein with the subsequent formation of a blood clot on them.
- Pulmonary embolism - the detached part of the blood clot enters the bloodstream and literally gets stuck in one of the branches of the artery supplying blood to the lungs. As a result, severe breathing problems develop, including the death of part or the entire lung.
- Thromboembolism of cerebral vessels . In this case, severe symptoms of damage to the nervous system develop, which are most often irreparable.
Therefore, if there is a child with sepsis in the hospital, it is necessary to monitor his general condition and the condition of the purulent focus every day. If the focus is not found, then it must be looked for inside the body using the latest diagnostic methods (ultrasound, X-ray, computed tomography, etc.).
With sepsis, laboratory test values change. An increase in the number of leukocytes is determined in the blood. In some cases, a decrease is observed, which is a less favorable sign. Anemia and the presence of pathogens in the blood are also detected. In case of sepsis, it is very important to examine the pus obtained from the lesion, as this allows you to directly determine the presence of pathogenic microorganisms, their type, and sensitivity to antibiotics.
Symptoms
Neonatal sepsis, which most often begins with symptoms within the first six hours of a baby's life, can also develop within 72 hours. Its appearance may be indicated by the baby’s rare pulse, an increase (sometimes decrease) in his body temperature, lethargy and worsening of the sucking reflex. Also, along with the symptoms described above, sepsis manifests itself through cramps, abdominal enlargement, difficulty breathing, muscle twitching, vomiting, jaundice and diarrhea.
However, it is important to understand that symptoms are directly related to the source of infection. If we talk about omphalitis (infection of the umbilical cord stump), then its symptoms are umbilical bleeding and purulent discharge. With peritonitis, the infection manifests itself through bloody diarrhea and an increase in the size of the newborn's abdomen.
Mechanism of sepsis in infants: risk group, further treatment
Sepsis in newborns is a terrible and dangerous disease that is not always possible to cope with. It is necessary to know the warning signs in order to react in time. In case of sepsis, the child should quickly end up in the hospital, only there his life can be saved.
Newborn
What is neonatal sepsis
Sepsis is one of the most dangerous diseases. About 30-40 percent of newborns die from it. You can save a child by noticing the symptoms of the disease in time. Over a short period of time, the body is affected by inflammation, which is provoked by a bacterial or fungal infection.
Among the causative agents of sepsis are streptococcus, staphylococcus, pneumococcus, and salmonella. The disease begins almost immediately after the baby is born or during the first month of his life. The factors that cause it can have an effect during pregnancy, during childbirth, or after it.
What is sepsis in newborns?
Congenital heart disease in newborns - causes and consequences
Sepsis in newborns in pediatrics varies depending on the time of its onset:
- Nosocomial – manifests itself in the maternity hospital. The medical facility is closed to understand what caused the disease and to prevent infection of other babies.
- Early sepsis makes itself felt on days 3-5 of a baby’s life. Infection occurs in the womb or during childbirth. For example, the baby swallowed amniotic fluid in which pathogenic microorganisms lived.
- Late - begins a week after the baby is born. The child could become infected both during the birth canal and after discharge from the hospital.
The classification of sepsis is also based on the speed of its development.
Thus, it can manifest itself with lightning speed, when symptoms are noticeable already on the first day, be acute and last 3-6 weeks, subacute, lasting 1.5-3 months.
It is most dangerous for a child when the disease develops immediately. It is important to take immediate action here. Sepsis can also be prolonged, then the baby recovers in about 3 months.
Causes of sepsis in newborns
Purulent septic diseases of newborns - description, prevention
Among the factors that can lead to sepsis are the following:
- Infectious diseases of the mother during pregnancy. This applies not only to gynecological pathologies, but also to problems with the digestive organs and urinary system. Cystitis can lead to serious consequences, especially if it is not treated in a timely manner. It often provokes kidney disease, pyelonephritis, which leads to more serious complications.
- Frequent abortions, as a result of which the uterine tissue is injured and damaged, which contributes to the spread of infections.
- Intrauterine hypoxia.
- Early rupture of amniotic fluid.
- Use of non-sterile instruments by obstetricians and other medical personnel.
- Infections developing in a newborn. This can be conjunctivitis, bronchitis, pneumonia, cystitis. Pemphigus is dangerous, manifested by the formation of blisters on the skin containing pus.
- Birth trauma, in particular damage to the skull.
- Damage to the skin and mucous membranes of the child.
Ulceration and suppuration may begin in the area of the hemangioma. This is a formation of blood vessels on the surface of the skin. It is not considered dangerous; in surgery, removal is provided when it grows or causes inconvenience. In rare cases, hemangioma appears in the etiology of sepsis as a factor provoking the spread of infection.
https://www.youtube.com/watch?v=HnCRXM2e-wo
Infantile hemangioma
Note! The risk of developing sepsis increases in babies born prematurely and whose weight does not reach 2 kilograms. At risk are children born during multiple pregnancies and babies with diagnosed congenital malformations.
How does sepsis manifest?
Hydronephrosis of the kidneys in newborns - what is it, consequences of the disease
The faster sepsis is recognized, the greater the chance of saving the child’s life. The disease manifests itself with symptoms:
- Unusual behavior: the newborn is very lethargic or extremely restless;
- Poor appetite, the child refuses to eat;
- Excessive regurgitation, vomiting;
- In a newborn with sepsis, the skin color is very pale and may have a grayish or yellowish tint;
- The nasolabial triangle takes on a blue tint;
- Diarrhea;
- Rapid breathing;
- Heart rhythm disturbances;
- Cramps, muscle twitching;
- Changes in body temperature: it can be either very low or elevated;
- Purulent lesions on the skin and mucous membranes. They often appear on internal organs and even affect bones;
- Skin rashes different from miliaria and atopic dermatitis.
Skin rashes
Clinical manifestations vary significantly, with symptoms depending on the original site of injury.
What happens during sepsis
The pathogenesis of sepsis begins with the appearance of a focus of purulent inflammation in the patient’s body. It serves as a source of infection. It is delivered through the blood and lymph to tissues and organs, affecting them. As a result, their functions are impaired.
Note! With sepsis, not only does blood poisoning occur, but blood vessels are also damaged and become easily permeable. Because of this, the infection spreads faster, spreading throughout the body. Babies have weak immunity, and it is impossible to contain it and stop the action of the purulent focus.
What to do if you notice symptoms of sepsis
A child with sepsis should be hospitalized immediately. He may have to be in intensive care. He receives the first dose of the medicine within an hour after dangerous symptoms are noticed. This way, the chance of recovering quickly and avoiding dire consequences increases significantly.
Helping a sick baby
Prognosis and treatment
With the rapid development of sepsis, about half of newborns die. In less acute forms, the mortality rate is slightly lower.
Bacterial sepsis in a newborn is treated only with antibiotics. They are administered intravenously to achieve greater effect. After bacterial culture is obtained, therapy is adjusted. Test results are never expected. Therapy begins instantly; precious minutes cannot be wasted. This is provided for by sepsis treatment protocols based on the recommendations of experienced doctors.
The child may also need breathing support and medications to adjust blood pressure.
In some cases, hormonal agents are used; in severe cases, blood or plasma is transfused. During treatment, it is important to increase the baby’s immunity; there are medications that can enhance the body’s defenses. If the cause of the spread of infection is a wound, for example, an umbilical wound, it must be treated with antibacterial agents, making sure to remove the pus.
Diagnostics
Initially, an experienced specialist establishes the septic condition of the newborn, after which an etiological diagnosis is made. At the next stage, to identify sepsis in a newborn, a diagnosis and assessment of the dysfunction of the child’s systems and organs and changes in hemostasis is carried out. The main difficulty in diagnosing sepsis in children is that the disease is very similar to the most dangerous diseases of both infectious and non-infectious nature. In children older than six days, the disease is identified by the primary lesion and microbiological examination of its secretions, blood and urine tests.
Leg sepsis
Strengthening the protective properties of the body of a sick child
It is a very important measure in the treatment of sepsis. A sick child is able to fully recover only when his body has the necessary reserve of immune forces. This is especially true for newborns, since their immunity tends to deplete very quickly. Currently, drugs that affect a variety of components of antimicrobial defense are widely used.
A feature of the treatment of young children is that they cannot be treated with drugs that directly stimulate immune mechanisms. Instead, they create artificial immunity by introducing ready-made antibodies into the body. Such therapy must be used at least in the first week of the disease. Previously, direct methods of blood transfusion to sick children were used, since it was believed that human blood has strong properties to inhibit pathogens. But at present, this type of technique has been abandoned due to the frequent development in children of various allergic reactions to foreign blood, in addition, with direct transfusions there is a possibility of infection with the human immunodeficiency virus (HIV).
You can stimulate your own immunity in children starting from six months of age. In younger children, this is possible after the signs of the disease have subsided, after a week of the disease. Recently, vaccination of sick children with toxins produced by microorganisms has become increasingly common, but this is not always effective, and in some cases can lead to the development of quite severe complications.
A large number of synthetic drugs are also used that improve overall metabolism, affecting mainly immune cells. Their influence also improves the production of antibodies.
Another important task in the treatment of sepsis is the prevention of allergic reactions. The fact is that in young children, during the development of severe infectious diseases, the immune response is distorted in such a way that, on the one hand, it becomes insufficient to fight the pathogen, and on the other, allergic reactions develop. To combat them, desensitizing agents and hormonal drugs are used.
As already mentioned, the use of hormones for diseases in young children is not entirely desirable. There must be compelling reasons for their appointment, which may include the following.
- Children with endocrine disorders in whom the natural production of these hormones is reduced from birth, especially if it is known that the child tends to react very violently to infectious diseases (high temperature, fever, diarrhea, vomiting, lack of appetite).
- Children whose disease is very severe and who had already received hormonal therapy for some reason before the disease. Moreover, when hormones are withdrawn, there is always a risk of developing a number of sometimes severe complications.
- Children receiving large doses of antibiotics or receiving several types of antibacterial drugs at the same time. This is due to the fact that when antibiotics are prescribed in children, allergic reactions often intensify.
- Children who have a strong allergic reaction to the introduction of pathogens into the body.
- A long and very severe course of the disease, as this depletes the functions of the body’s glands.
You should always remember that when prescribing hormonal drugs, you must strictly adhere to their dosage and regimen of use. When prescribing hormones, in order to avoid complications, which develop very often, it is necessary to simultaneously give children drugs containing potassium and anabolic steroids. You should always strive for the most rational combination of doses of antibiotics and hormonal drugs. A very good result is obtained by combining hormones with immunoglobulins and serums that create passive immunity. Hormonal drugs, unless there are special reasons for this, should not be prescribed for a period of more than a week. Their course should be started and discontinued gradually and carefully, since with abrupt withdrawal there is a risk of developing insufficient adrenal function.
Any infection, especially one as severe as sepsis, is very stressful for the body of a newborn child. Therefore, all of its metabolic processes are under very great stress. As a result, the need for nutrients and vitamins increases significantly. A small child especially needs B vitamins. Therapy with vitamin preparations must begin when the disease has just been identified. You can use not only vitamins, but also their various derivatives, which help improve metabolism and normalize the functions of certain organs.
Since the nervous system is the first to suffer when microbial toxins enter the bloodstream, from the first days of the disease it is necessary to use various drugs that help normalize blood flow in the brain and restore its functions. Various sedatives can be prescribed to children. Disturbed functions of the respiratory and cardiovascular systems are also subject to correction. Such special measures, used only when necessary, are the introduction of so-called energy mixtures, transferring the child to artificial ventilation, the use of diuretics, blood purification, etc.
Treatment
The duration of treatment for sepsis in newborns is always determined by the attending physician, and the course itself continues until all symptoms of the disease disappear, the blood returns to normal, and weight begins to be restored. The staphylococcal variety of the disease is usually treated with either oxacillin (100 to 150 mg per kilogram of body weight) or methicillin (150 to 200 mg per kilogram of body weight). To combat colisepsis, gentamicin (4 to 5 mg per kilogram of body weight) and colimycin (30 to 50 mg per kilogram of body weight) are used for one or two weeks.
Tobramycin (4 to 7 mg per kilogram of body weight) and standard dosage ampicillin intramuscularly are used against protes infections. Penicillin (from 300 thousand to 500 thousand E per kilogram of weight) is used in combination with prednisolone to combat hemolytic streptococci.
For heavy hemorrhages, newborns are prescribed vitamin C (300 to 500 mg) and vitamin K (3 mg each). In some cases, intramuscular administration of calcium gluconate and blood transfusion (with the addition of a small amount of gramavanine and plasma up to 20-30 milliliters) every three to four days are additionally prescribed. Joint suppuration and osteomyelitis are treated using conservative methods - antibiotics (in large doses).
Treatment of neonatal sepsis
All forms of sepsis in newborns are treated in the intensive care unit or neonatal pathology department.
It is recommended to feed a child with sepsis breast milk. If his condition allows, then you can put the baby to the breast. If sucking from the breast requires a lot of effort from the baby, then it is worth feeding expressed breast milk from a bottle or beaker. When a baby is unable to breastfeed due to a condition or is too small for gestational age, expressed breast milk is inserted into the stomach through a tube. If there is no mother's milk, then the baby should be fed with formula milk. They can be fermented milk, low-lactose, lactose-free, enriched with prebiotics and other components. The mixture is selected depending on how the child absorbs food, whether there is bloating, or whether the stool is disturbed. Premature babies should be fed special milk formulas that contain broken down protein for better absorption.
At the height of the child’s illness, it is better to place him in an incubator. Humidity in the incubator is not lower than 60%, and the temperature is not lower than 30°C are important components of proper care for a sick child.
Direct treatment of sepsis in newborns proceeds simultaneously in two directions. The first is the impact directly on the pathogen that caused the disease. And the second is the correction of dysfunctions of all organs involved in the process.
Antibiotic therapy is prescribed as early as possible. Depending on the form of neonatal sepsis, a choice is made in favor of one drug or another. Until the pathogen is isolated, the antibiotic or combination thereof that will be most effective against the suspected microorganisms is prescribed. When the pathogen is known, an antibiotic with a narrower spectrum of action is prescribed. The choice is made in favor of drugs that easily penetrate into the cerebrospinal fluid, into the brain, as well as into bone and lung tissue. Priority is given to drugs that are least toxic to children. It is preferable to administer antibiotics intravenously.
Most often, treatment begins with antibiotics belonging to the penicillin class (Oxacillin, Ampicillin, Amoxiclav). They are usually combined with aminoglycosides, which include Gentamicin, Netromycin, Amikacin. Cephalosporins are also used. If starting antibiotics are ineffective, Vancomycin, Meronem, Linezolid are prescribed. You can be confident about the effectiveness of the measures taken if the child feels better after two days from the start of treatment. If the severity of symptoms of SVR and organ failure persist or increase, it is necessary to change the antibiotic.
In addition to antibiotics, for sepsis in newborn children, therapy is aimed at correcting immunity, intravenous infusions of the required amount of fluid (glucose, salts, vitamins), anti-shock therapy and restoration of impaired functions of internal organs. Human immunoglobulins (Pentaglobin) are used to correct immunity. The mortality rate of children receiving this treatment is significantly reduced. This is especially significant in case of sepsis in premature infants, because the immune system is initially weakened. Intravenous infusions of glucose-saline solutions help replenish the lack of fluid and improve the properties of the blood. If nutrition is not absorbed orally, the child must be given proteins, fats and carbohydrates intravenously, which is called parenteral nutrition.
Antishock treatment of neonatal sepsis includes therapy with drugs that maintain blood pressure at normal levels (Dopamine, Dobutamine, Adrenaline). Sometimes it is necessary to supplement treatment with hormonal drugs (Hydrocortisone). This increases the survival rate of sick children. To correct disorders of the blood coagulation system, children are transfused with fresh frozen plasma. It helps to compensate for the lack of blood clotting factors that is observed in sepsis.
In addition to the treatment of life-threatening conditions, treatment with antifungal agents (Duflucan), vitamin therapy, and interferon therapy (Viferon) are simultaneously carried out.
Course and consequences
The only outcome in the absence of comprehensive treatment is death. With rapidly progressing septic shock (from 3 to 5 days), the newborn dies before the fifth day of his life. However, such a course of the disease is recorded only in 15 cases out of a hundred. In the absence of septic shock or its timely stopping with medication, the disease becomes acute and lasts up to two months. This course of sepsis is more common (80 cases out of a hundred).
Death from sepsis can occur even in the third or fourth week of the disease, due to multiple organ failure. In its acute form, sepsis in newborns lasts for about two weeks, then a reparation period begins (the functions of the newborn’s organs return to normal, toxicosis subsides), during which the resistant organism is significantly reduced, and the risk of superinfection (virus, fungi or bacteria) entering the body increases.
Consequences
The most serious consequence of this infection is death. According to statistics, approximately half of infants infected with sepsis die. Such an infection rarely gives a favorable outcome; in some cases, septic shock develops - a disruption of all functions of the baby’s body, as a result of which blood pressure drops to zero.
Septic shock is fatal in most cases. It is also possible for the child to develop anemia, malnutrition and impaired phosphorus-calcium metabolism. Such complications are eliminated during recovery from sepsis.
Classification
Sepsis is usually divided into postnatal and intrauterine. The former is also subdivided into early neonatal sepsis and late neonatal sepsis. Intrauterine sepsis usually develops due to placentitis, chorioamnionitis or chorionitis and is a consequence of intrapartum and antenatal infection of the fetus. In such cases, the source of infection is located outside the child’s body. In the case of postnatal sepsis, the source of infection is located only in the child’s body.
Diagnosis of sepsis
Etiology of sepsis in newborns
When a child is exposed to pathogens, an inflammatory reaction occurs (sepsis in newborns), during which cytokines are released in large quantities. The inflammatory process affects the elements that make up the blood (leukocytes, red blood cells, proteins). With a negative effect on the body, necrosis and leukemia can occur. Blood clotting is impaired.
The excess composition of cytokines promotes the development of pathogen cells in the baby’s body, as a result of which sepsis is formed. At this moment, cartisol increases significantly, due to which the activity of the thyroid gland decreases.
Children say! We are traveling on the bus with our daughter (4 years old). The driver announces stops: - Gorky's next stop. Alla frowned and closed her eyes. I ask her: “What’s the matter, what happened?” - Uncle, a bitter stop.
At the last stage of infection development, multiple organ failure occurs, thrombocytosis occurs, provoking a disorder of homeostasis, which often leads to death.
If a pregnant woman has obvious uterine abnormalities accompanied by polyhydramnios, there is a risk that the baby will develop neonatal sepsis.
Watch a video about the development of sepsis in newborns.
Attention parents! High neonatal mortality is most often associated with the influence of negative factors that cause sepsis in newborns, so the disease must be diagnosed on time.
Prevention
As a preventive measure, it is necessary to prevent all kinds of acute infectious diseases accompanied by fever in pregnant women in the last months of pregnancy or promptly treat them if necessary. Here are the main provisions of preventive measures against sepsis in newborns:
- Full compliance with all hygienic and sanitary medical standards in relation to the woman in labor. Thanks to observance of aseptic labor, sepsis in newborns has become much less common in recent years.
- Maintaining navel asepsis and proper care of its stump.
- Proper mother's breast care and proper feeding.
- Compliance with all aseptic instructions during the first toilet of a newborn
- Timely isolation of the sick mother from the child.
- Proper care of your baby's mouth and nose
- Finding the child in a bright and spacious room, illuminated by quartz lamps
- All persons in contact with the child should thoroughly wash and disinfect their hands, and wear a bandage that fits tightly to the face.
In modern hospitals, all medical personnel who come into contact with newborn children are checked for the presence of pathogenic microbes in the feces and oral cavity. Persons suffering from purulent infections or influenza are not allowed to work.
Prevention of sepsis
Begins from the neonatal period of the child. The most important measure is compliance with sanitary and hygienic standards by the management and staff of the maternity hospital in which the child was born. All medical workers and newborn children are constantly examined for carriage of dangerous microorganisms. If they are detected, workers are sent for treatment, and sick children and mothers are immediately isolated from healthy ones. The maternity hospital is under quarantine.
One of the very important activities that, unfortunately, receives very little attention at present, is sanitary education work among the population. This is due to the fact that in families with very young children, proper personal hygiene of each family member and the hygiene of the baby is mandatory.
When a child is discharged from the maternity hospital, he or she must be subsequently monitored by a clinic nurse. It is necessary to identify a special risk group of children who have a weakened immune system, have congenital malformations, or who have suffered an infectious process while in the womb.