What is balanoposthitis
Balanoposthitis is an inflammatory lesion of the skin of the glans penis and the part of the foreskin in contact with it. The external manifestations of the disease depend on its origin. This may include redness and swelling, blisters, ulcers, peeling, discharge and plaque.
If the inflammation is infectious, then unprotected sex can easily infect your partner. Accordingly, the infection that causes balanoposthitis gets to the head from the partner’s genitals, as well as from the tongue, pharynx, and rectum. A man himself can introduce his own E. coli, staphylococcus, or streptococcus under the foreskin. Most often they are discovered during diagnosis.
Do you use condoms during sexual intercourse?
Balanitis and balanoposthitis: what is the difference
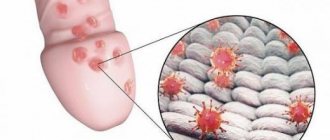
Balanitis is an isolated inflammation of the glans penis. The foreskin is not affected. Balanoposthitis is a combined inflammation. When the skin of the prepuce is pulled back, pathological signs are clearly visible on it. Inflammation of the inner lobe of the foreskin usually occurs almost immediately after damage to the glans. Both types of lesions are clearly illustrated in the picture below. On the left – balanitis, on the right – balanoposthitis.
Forms of balanoposthitis
According to the nature of the course, acute and chronic forms are distinguished. In the first case, severe itching and pain appear in the area of the head, ulcers form, pus is released, and urination becomes difficult. In some cases, the inguinal lymph nodes even become enlarged and the temperature rises.
In the chronic form, symptoms are mild. A man experiences discomfort mainly after sex or under the influence of provoking factors: cold, alcohol, physical overload.
Depending on the type of inflammation, balanoposthitis can be non-infectious (allergic, radiation, autoimmune), toxic (chemicals, medications, alcoholism) and infectious. The latter is the most common. It is provoked by fungi, aerobic and anaerobic bacteria.
Depending on the type of pathogen, inflammation can be specific or nonspecific. Specific is provoked by sexually transmitted infections and, depending on their type, can be, for example, chlamydial (circinar), gonorrheal, mycoplasma, trichomoniasis, gardnerellosis, herpetic (genital herpes).
Nonspecific develops mainly due to poor hygiene: the accumulation of smegma in the fold of the preputial sac is a favorable environment for the development of bacteria.
If the pathogen comes from the outside (during sex, from dirty hands during masturbation), then primary balanoposthitis is diagnosed. In secondary cases, the pathogen enters through the blood or lymph.
All types of balanoposthitis have specific symptoms, differ in the type of pathogen and the nature of the inflammatory process. Urologist, dermatovenerologist Lenkin Sergey Gennadievich tells more about the classification
According to external manifestations, balanoposthitis is divided into three types:
- Simple. It manifests itself as redness of the head and foreskin, swelling, and effusion. Erosion of various forms gradually appears on the skin. Sensations include slight itching and burning.
- Erosive. First, white swollen areas appear on the skin, covered with a loose layer of dead epithelium. Subsequently, they are replaced by red erosive spots. A possible complication in the form of phimosis.
- Gangrenous. The ulcers are deep, purulent, and poorly healing. Characterized by severe swelling of the head and foreskin. Additional symptoms may include fever and weakness.
Photos 18+ are presented here and below in the links. Circinar balanoposthitis (chlamydia) – https://prntscr.com/se96ci. Fungal (candidal) balanoposthitis – https://prntscr.com/se96jm. Chronic balanoposthitis – https://prntscr.com/se96qg.
Chronic balanoposthitis occurs against the background of phimosis, a cicatricial lesion of the foreskin. The recurrent form is typical for men with type 2 diabetes mellitus and psoriasis.
Symptoms
The disease begins with subtle symptoms, which become more obvious as the infection progresses:
- Hyperemia of the epidermis of the head of the penis, maceration and swelling
develop . The patient begins to experience burning and itching in the prepuce area. Sexual intercourse or an attempt to expose the head of the penis is accompanied by severe discomfort; - Smegma and drops of urine begin to accumulate in the inflamed preputial sac, which only increases irritation and contributes to the development of infection;
- As the disease progresses, a pinkish or purple rash
; - The patient begins to experience symptoms of general intoxication of the body: headache, chills, nausea, hyperthermia, etc. This is a characteristic sign of acute balanitis or balanoposthitis;
- Due to the development of infection, purulent discharge appears
from the preputial sac, and acute purulent balanoposthitis develops.
If urgent treatment of the disease is not started at this stage, it turns into an erosive form.
. It is characterized by the following symptoms:
- The appearance of whitish growths on the skin - areas of dead epidermis;
- Deep inflammation leads to rupture of the mucous membrane and skin
. Bright red erosions with clear boundaries form on the head of the penis and prepuce.Their surface may be covered with pus. The patient experiences acute pain syndrome. It is impossible to expose the head of the penis;
- The inflammatory process also affects the lymph nodes, and lymphadenitis develops.
If a man’s immune system is weakened, and therapy for acute balanitis or balanoposthitis is not started, the infection becomes gangrenous:
- Local symptoms include signs of general intoxication of the body: weakness, headache, hyperthermia up to 39°C, nausea;
- Due to suppuration of erosions on the skin and mucous membranes of the penis, multiple deep ulcers with purulent discharge are formed.
- As a result of severe swelling, the penis takes on a bell shape;
- The necrotic process in the prepuce area can lead to perforation and disintegration of the foreskin.
ATTENTION!
If you notice any balanitis, immediately contact a urologist. The sooner treatment begins, the less likely it is to develop complications.
Symptoms
The first symptoms of balanoposthitis are discomfort in the area of the head and foreskin, redness or spots. Then the itching and pain intensify, the skin lesions become more pronounced, and pus begins to be released. Inflammation of the head leads to swelling of the urethral sponges and their closure, making urination difficult.
Redness around the head of the penis
With candidal balanoposthitis, the skin of the head and foreskin becomes bright red, white lumps and plaque form on it.
The herpetic form is characterized by the formation of small transparent blisters, which constantly hurt and itch, then burst. Sores remain in their place.
Herpetic balanoposthitis with associated infection - https://prntscr.com/se975f.
Dermatovenerologist Vyacheslav Vasilievich Makarchuk talks about what symptoms accompany balanoposthitis
Reasons for development
The disease is combined, as it combines two diagnoses - balanitis and posthitis. Contact of the head and foreskin provokes mutual transmission of inflammation. Thus, only men who have not undergone circumcision can suffer from balanoposthitis directly.
Infectious and non-infectious factors can provoke the development of balanoposthitis. The main reasons are the following:
| Reason and photo | Short description |
| Injuries | They appear in the form of abrasions and mechanical damage, for example, when fastening your fly unsuccessfully. |
| Failure to comply with personal hygiene rules | It is necessary to thoroughly wash the external genitalia every morning and evening. |
| Allergic reaction | Gels, synthetic clothing, latex and lubricants used can cause allergies. |
| Excessive cleaning | Excessive attention to hygiene is as harmful as ignoring it. |
| Bacteria | Most often, it is pathogenic microflora that provokes inflammation of the genital organs. |
| Fungal infection | Most often, this is a Candida fungus, which can be caught through unprotected sexual contact with a woman with thrush. |
| Specific infections, including STDs | For example, balanoposthitis can be a consequence of syphilis. |
| Phimosis | Narrowing of the foreskin increases the risk of inflammation of the tissue underneath. |
| Skin diseases | We are talking about a variety of dermatitis, lichen, psoriasis, etc. |
| Significant decrease in immunity | A decrease in natural defenses increases the risks of a pathological reaction to contact with foreign microorganisms. In immunodeficiencies, balanoposthitis is a common diagnosis. |
| Wearing tight underwear | Compression of the organ and friction against the tissue, especially if it is synthetic, negatively affect men’s health. |
| Violation of tissue trophism | Internal disorders of a systemic or local nature associated with metabolism and tissue nutrition. This problem is especially relevant for people with diabetes and alcoholics. |
| Unexplained | When the exact cause of the development of balanoposthitis cannot be determined, its idiopathic form is diagnosed. |
Diagnostics
Diagnosis of balanoposthitis includes examination by a urologist, taking a smear from the surface of the head and skin of the prepuce, and scraping from the urethra. The biomaterial is studied by microscopy and sown on a nutrient medium to identify the pathogen. If diabetes is suspected, a blood test for sugar and hormones is taken.
It is imperative to exclude an allergic reaction, since it is often the cause of inflammation. Due to incorrect diagnosis, men spend years unsuccessfully treating a non-existent fungus or conditional infections, and the condition does not improve.
Treatment
The tactics and duration of treatment depend on the test results. For example, the staphylococcal form of inflammation is stopped with the help of antibiotics in 7-10 days, therapy for gonorrheal, syphilitic or specific (caused by an STD) can take more than a month.
Treatment of secondary balanoposthitis is complicated by the presence of a provoking factor. If it is diabetes, then it must be put into remission, normalize the sugar level and wait for the general condition to improve. Primary foci of infection in the body must be neutralized, otherwise the pathogen will again penetrate the tissue of the penis.
Treatment of uncomplicated balanoposthitis is carried out at home according to the regimen prescribed by the doctor.
Drugs
Mild localized balanoposthitis is usually treated with local remedies (creams, ointments, baths) so as not to cause unnecessary harm to the stomach and liver. Tablets are prescribed for progressive inflammation affecting the urethra and other organs.
Antibiotics
The choice of tablets for balanoposthitis depends on the cause of inflammation, which is determined by the results of smear microscopy and bacterial culture.
Table 1. Means for the treatment of various types of balanoposthitis
| Type of balanoposthitis | Pathogens | Pills | Drug name | Reception scheme |
| Infectious nonspecific | Coccus or rod flora (streptococci, Escherichia coli) | Broad-spectrum semi-synthetic penicillins. Most effective in combination with beta-lactamase inhibitors. | “Amoxicillin + clavuanic acid” (from 335 rub.) | The doctor describes the scheme |
| Tetracyclines. Suppress protein synthesis of pathogens. In addition to nonspecific flora, they are also active against mycoplasma and chlamydia. | "Tetracycline" (from 24 rub.) | |||
| Gonorrheal | Gonococci | Fluoroquinolones. Destabilize DNA chains in bacteria. | "Ciprofloxacin" (from 22 rub.) | 500 mg once |
| "Ofloxacin" (from 38 rub.) | 400 mg once | |||
| Macrolides. Suppress protein synthesis in bacterial cells. | "Azithromycin" (from 34 rub.) | 1 mg once | ||
| Infectious specific (trichomoniasis, gardnerellosis) | Trichomonas, gardnerella | Antiprotozoal synthetic antibacterial substances. They disrupt the respiratory processes of protozoa and anaerobes and inhibit the synthesis of their DNA. | "Metronidazole" or "Trichopol" (from 92 rub.) | 0.5 g 2 times a day for 5-7 days |
| "Tinidazole" (from 70 rub.) | In the first 2 days, 2 g once a day, days 3 and 4, 0.5 g twice a day. | |||
| Lincosamides. Suppress protein synthesis in microbial cells. | "Lincomycin" (from 82 rub.) | 500 mg 3 times a day | ||
| Fungal (candida) | Candida fungus | Polyene antibiotics (natural antimycotics). They have the broadest profile of antifungal activity. The active substances make the walls of fungal cells porous, as a result of which they die. | "Nystatin" (from 100 rub.) | The scheme is assigned individually |
| “Tetracycline with nystatin” (from 28 rubles) – a combined remedy against sexually transmitted infections and fungus |
In recent years, cases of ineffectiveness of ampicillin and cefoxitin have been recorded more often. Metronidazole retains its activity. It combines well with fluoroquinolones, aminoglycosides, co-trimoxazole, and macrolides.
To treat erosive balanoposthitis, antibiotics are prescribed in accordance with test results, since erosion can occur against the background of allergic and infectious inflammation.
How to take metronidazole : 0.5 g 2 times a day for 5-7 days.
What antibiotics are suitable for a child : for balanoposthitis, children are prescribed mainly local drugs; oral antibiotics are used in case of emergency (spread of infection, enlarged lymph nodes, intoxication). Tablets are prescribed from the age of 12; antibiotics in the form of a suspension are suitable for younger boys:
- "Suprax". Not recommended for children under six months old.
- "Amoxiclav". Suitable for children from one year old.
- "Augmentin". Can be given to infants.
- "Cefixime". For children from one year old.
- "Klacid." From 0 to 12 years.
Fluoroquinolones, which include Ofloxacin, Ciprofloxacin, Tsifran, are not prescribed to minor children, since these drugs interfere with the normal formation of cartilage.
What antibiotics can be taken for balanoposthitis with diabetes mellitus: in diabetes, infections tend to develop rapidly and often recur, so taking antibiotics should be started as early as possible. Drugs that reduce renal function (aminoglycosides) are contraindicated. For balanoposthitis, Fosfomycin, Amoxicillin, Cefixime, Norfloxacin, Levofloxacin are prescribed. At the same time, it is necessary to normalize the sugar level, otherwise the treatment will be ineffective. This is especially true for erosive and fungal balanoposthitis.
Antifungal agents
In addition to polyene antibiotics, triazole derivatives are prescribed for fungal balanoposthitis: Fluconazole (from 70 rubles) and Itraconazole (from 342 rubles).
Itraconazole dosage regimen: 200 mg once a day for 3 days. With the primary disease, relief occurs after 2-3 days, complete cure - after 2-4 weeks. For chronic candidal balanoposthitis it is effective in 87% of cases.
How to take Fluconazole : on the first day 400 mg, then 200 mg per day. The duration of treatment depends on the degree of effectiveness. Not prescribed for children under 4 years of age.
Other groups of drugs
For the treatment of viral (herpes) balanoposthitis, the antiviral drug “Acyclovir” is prescribed (from 22 rubles). Dosage regimen: 400 mg three times a day for no longer than 10 days. For relapses: 200 mg 4 times a day for 5 days.
For allergic balanoposthitis, symptoms are relieved with antihistamine tablets. A popular drug is Claritin (from 227 rubles). Dosage regimen: one tablet once a day.
Not all doctors prescribe immunomodulators (Viferon, Amiksin) as part of the treatment of balanoposthitis, since opinions on their effectiveness differ. Some experts consider them not only useless, but also dangerous. This position is due to the fact that interference in immune processes can lead to serious systemic pathologies.
Ointments
- Against fungus: Miconazole, Clotrimazole.
- For healing ulcers and erosions: Bepanten, Baneocin, Dermovate, solcoseryl ointment.
- Against itching and inflammation: Advantan, Triderm.
- Antiseptic regenerating: "Levomekol", liquid streptocide.
- For weeping ulcers: zinc ointment, “Tsindol”.
- Against herpes: Acyclovir.
Detailed article on the choice of ointments for the treatment of balanoposthitis.
Dermatovenereologist Vyacheslav Vasilyevich Makarchuk tells which antimicrobial ointments to use for the treatment of balanoposthitis
If there are erosions, before applying the ointment, it is necessary to treat the head and foreskin with an antiseptic. This can be chlorkegsidine, Miramistin, or baths (three times a day for 5-10 minutes).
Baths
How to prepare baths:
- With furatsilin: dissolve the tablet in a glass of warm water, wait until it cools.
- With manganese: dissolve the crystal in a separate bowl, then take about half a teaspoon from there and add it to the bath container (just enough so that the solution turns light pink, otherwise the skin can be burned).
- With chamomile: pour boiling water (0.2 l) over a tablespoon of the herb and leave until it cools. In the same way you can use string, sage, St. John's wort.
The juice of aloe and Kalanchoe pinnate has good softening and wound-healing properties. It can be used for peeling of the head, as well as for healing minor erosions. You need to lubricate the head and foreskin with juice 2-3 times a day.
Diet
For the entire period of treatment for balanoposthitis, you should completely abstain from alcohol, spicy, salty, fatty foods, and caffeine, so as not to irritate the urethra and not to burden the liver (it functions in an enhanced mode due to medication).
You should eat more vegetables, greens, fruits, less red meat, potatoes, and flour products. It is advisable to exclude sweets.
Men with balanoposthitis should focus on a balanced diet rich in vitamins A, B, C, E, selenium, iodine, cyanine
Surgical intervention
Indications for surgical treatment:
- Cicatricial phimosis (narrowed foreskin, on which, due to attempts to open the head, cracks and then scars have formed).
- Frequent relapses.
- Chronic form of balanoposthitis.
In the above cases, the problem can only be solved by circumcision. The foreskin is excised in a circle, then the remaining skin is sutured under the glans. Thus, it remains constantly open, the physical causes of the development of balanoposthitis (preputial pocket) are eliminated. After circumcision, the head will be hypersensitive, but after 1-2 months this discomfort will go away (read more about the pros and cons of male circumcision).
Read more: How to reduce the sensitivity of the head of the penis.
Circumcision scheme
If balanoposthitis occurs against the background of ordinary phimosis (when most of the head opens), then plastic surgery of the foreskin can be done. The surgeon makes a longitudinal incision in a narrow place, then stitches it transversely, expanding the lumen of the prepuce.
Treatment for diabetes mellitus
Diabetes mellitus is a systemic disease that negatively affects almost all organs. To stop the inflammatory process, you must first normalize the blood sugar level, otherwise restoration of the skin is impossible.
To heal erosions, they are first washed with antiseptics, and only then regenerating ointments (Solcoseryl, Diaderm) are applied.
Solcoseryl is a drug for the rapid healing of wounds, burns and other injuries. Price from 432 rubles
The best remedies for balanoposthitis
The drug will only help if it is prescribed correctly and if the bacteria are not resistant. The most effective remedies for balanoposthitis are the following:
- For mild inflammation and as a treatment before applying ointment: chlorhexidine (from 17 rubles), furatsilin (from 22 rubles). The head is treated with chlorhexidine and poured under the foreskin, and warm solutions for baths are made based on furatsilin.
- For localized balanoposthitis (without urethritis and cystitis), combined ointments are used: “Akriderm GK” (from 448 rubles), “Triderm” (from 470 rubles). The drugs are effective against mixed infections (genital + nonspecific + fungal). Apply a thin layer to the glans and foreskin. It should be noted that they contain corticosteroid hormones, which can thin the skin with prolonged use.
- For fungal (candidal) balanoposthitis, Nystatin is effective. As for synthetic antifungal agents in tablets, the previously popular Clotrimazole is being replaced by Itraconazole (most effective when taken on an empty stomach). Clotrimazole works well externally in the form of an ointment.
- In severe forms of balanoposthitis (until culture results are obtained), broad-spectrum antibiotics are prescribed. Amoxiclav is considered the most harmless and universal.
- For healing ulcers and erosions: Advantan ointment (from 529 rubles), Levomekol (from 122 rubles), methyluracil ointment (from 68 rubles). The glucocorticosteroid Advantan (Comfoderm) most effectively suppresses inflammatory and allergic reactions.
Chronic course
Many patients, having felt the initial signs, do not go to the doctor and do not receive timely help. In addition to the fact that they become a source of infection, the disease takes a chronic form.
Chronic candidal balanoposthitis in men, the photo clearly represents the degree of damage to the organ, has a protracted clinical course with frequent relapses. Up to seven exacerbations can be observed during the year. This development of candidiasis is typical for those who are carriers of a genitourinary tract infection, a weakened protective function, or diabetes mellitus.
This degree is characterized by:
- Constant but moderate itching, burning;
- Pain on palpation;
- Edema;
- Ulcers and erosions with necrotic tissue at the edges;
- Hyperemia;
- Curdled discharge, films, unpleasant odor;
- Purulent discharge from the urethra;
- Painful erection and sexual intercourse.
Chronic progression occurs in two directions: indurative and ulcerative-hypertrophic.
Consequences and complications of balanoposthitis
Long-term attempts at self-treatment of balanoposthitis will provoke its transition to a chronic form, which means constant low-grade inflammation with periodic exacerbations. As a result, the scalp skin becomes thinner and changes its structure. Due to frequent irritation, nerve endings first become hypersensitive, which leads to painful sex and premature ejaculation, and then can atrophy. Subsequently, the skin of the prepuce and glans begins to gradually grow together. This is facilitated by their constant sticking together due to the secreted inflammatory fluid and pus.
Against the background of balanoposthitis, cicatricial phimosis often develops. The inflamed tissue is thin, it bursts, resulting in scars that tighten the skin. Smearing them with absorbable ointments is, as a rule, useless. Cicatricial phimosis can only be treated by circumcision.
Dermatovenerologist Vyacheslav Vasilievich Makarchuk talks about the complications and consequences of balanoposthitis
There are also more serious complications of balanoposthitis:
- Deformation of the head due to purulent melting of tissue.
- Gangrene of the head and penis.
- Malignant neoplasms.
Chronic balanoposthitis provokes urethritis, cystitis, prostatitis and even pyelonephritis, since the infection tends to rise higher in the urethra.
Chronic balanoposthitis with atypical candida
There are many types of candida.
More or less often cause inflammatory processes of the penis of 5-8 types.
The clinical course of infection with atypical candida is unfavorable.
Symptoms are often more severe.
The disease is not always completely cured.
Many types of candida are completely insensitive to the antimycotics used: clotrimazole, fluconazole.
They need to be treated with other medications.
Otherwise, balanoposthitis is highly likely to become chronic or recurrent.
But to find out that the disease is caused by atypical candida, the patient needs a full examination.
In most cases it is not.
As soon as the doctor finds out that the disease is caused by candida, he prescribes fluconazole and sends the person home.
Does not conduct an in-depth examination.
What for?
After all, in 80% of cases it is candida albicans.
You can get rid of it easily and quickly.
However, 20% is a fairly large number.
This means that treatment may not respond to one in five patients, and balanoposthitis sometimes becomes chronic for this reason.
In our clinic, patients with inflammation of the head undergo a full examination.
We take a smear for PCR and, if necessary, perform a culture.
As a result, the doctor knows exactly what type of candida is causing the disease.
Therefore, he selects for therapy exactly the drug to which the fungi are not resistant.
FAQ
Is it possible to have sex with balanoposthitis?
In the acute form it is impossible, but in the chronic form - only with a condom. There are two reasons: the likelihood of infection of the partner and the high risk of relapse. The local immunity of the head and prepuce is weakened, so inflammation can worsen due to secretions and mechanical stress.
Is it possible to masturbate?
In the acute form, it is impossible due to increased irritation. If there are signs of narrowing of the foreskin, masturbation can lead to paraphimosis - pinching of the head by the preputial ring.
Do they take you into the army with balanoposthitis?
They take it because it is a curable disease. Below is a screenshot of a question to a urologist from the site https://www.infomedical.ru/faq/answer.php?id=4925:
Is it possible to go to the bathhouse and sauna?
In case of acute balanoposthitis it is not possible, in case of chronic balanoposthitis it is possible, but without abuse.
Prevention - reliable protection against balanoposthitis
Preventive measures must be observed from the moment the newborn is born:
- compliance with hygiene procedures for the genital organs of a child of any age, women and men;
- Hygienic procedures are required before and after sexual intercourse;
- it is advisable to shave or cut short the hair in the penis area, which will reduce the likelihood of the onset of an inflammatory process;
- in case of casual contacts, ensure protected sex using a condom.
- It is recommended to use antiseptic drugs: a solution of potassium permanganate and Chlorhexidine;
- when the first symptoms appear, you should immediately consult a doctor;
- when a boy is born, diapers and pampers should be selected correctly in size to avoid chafing and injury to the genitals;
- be sure to leave a newborn baby without clothes for a short time in a warm room to ventilate the skin in the groin area;
- do not move the baby’s skin on the penis to avoid tearing it and causing inflammation;
- For adult boys and men, during water procedures, move the foreskin and thoroughly rinse the glans, ensure the cleanliness of the underwear;
- At the first signs of illness, you should immediately contact a urologist.
Reviews about the treatment
Judging by thematic forums, problems with the treatment of balanoposthitis arise due to incorrect diagnosis. As a result, out of desperation, men begin to be treated with all available methods, only worsening the condition. A typical patient question and urologist's answer are given below (site https://potencya.com/forums.php?m=posts&p=961):
From the site https://medicinform.ru/index.php/topic/56555-balanoposthitis/: