Toxoplasmosis is one of the most dangerous diseases caused by parasites.
The causative agents of this disease are microscopic protists, which, when entering the human body, can cause disruption in the functioning of almost all of its systems.
Treatment of toxoplasmosis in adults should be carried out comprehensively and necessarily include taking the necessary antiparasitic drugs, means to maintain immunity and auxiliary herbal medicine.
Absolutely anyone can get toxoplasmosis. There are several main ways of contracting this disease:
- Through domestic animals - cats, which are carriers of toxoplasma, are especially dangerous;
- When consuming raw or undercooked meat and poultry eggs;
- Through mosquitoes, ticks and other blood-sucking insects;
- Through damaged skin at the site of wounds and cuts;
- In close contact with a sick person;
- During blood transfusion and donor organ transplantation;
- Through pests - rats, mice, etc.;
- Through dirty hands.
The development of toxoplasmosis begins in the human intestines. From there, the parasites penetrate the blood vessels and lymph flows and spread throughout the body, settling in the internal organs and tissues.
Having reached the final goal, toxoplasma begins to actively multiply, causing enormous harm to the body.
general information
Toxoplasmosis is an infection caused by the single-celled protozoan parasite Toxoplasma. The infection usually causes no symptoms, although some people experience enlarged lymph nodes, a fever, a feeling of malaise, and sometimes a sore throat or blurred vision and eye pain. In people with weakened immune systems due to AIDS or another disease, toxoplasmosis can reactivate, usually affecting the brain. A reactivated infection may cause weakness, confusion, seizures or coma, or spread throughout the body. Babies infected before birth (called congenital infection) may have birth defects, vision loss, seizures, mental retardation and other disabilities.
- A person becomes infected by passing parasite eggs from an infected object into the mouth or through contaminated food.
- In most cases, the infection is asymptomatic or with minor symptoms.
- Women infected during pregnancy can pass the parasite to their fetus, sometimes causing miscarriage, stillbirth, or serious problems in the newborn.
- Typically, severe symptoms occur only in people with weakened immune systems and are caused by inflammation of the brain (encephalitis), causing muscle weakness on one side of the body, confusion, or coma.
- Other organs are less likely to be affected in people with weakened immune systems.
- Typically, a doctor makes a diagnosis using a blood test, which determines the presence of antibodies to the parasite.
- Properly cooking and freezing meat and thoroughly washing hands after handling raw meat, handling soil, and cleaning cat litter will help prevent the spread of infection.
- Most healthy people do not require treatment, but pyrimethamine in combination with sulfadiazine and leucovorin is often given to symptomatic adults and infected newborns.
Toxoplasma is common throughout the world where cats live. The parasite infects a large number of animals, as well as people. The disease is common in Russia, although only some people show symptoms. Severe infection usually develops only in the fetus and in people who have a disease that weakens the immune system (such as AIDS or cancer) or are taking drugs that suppress the immune system (immunosuppressants), especially those used to suppress organ transplant rejection.
Do you know that…
The parasite that causes toxoplasmosis can only lay eggs in the intestines of cats.
Although the parasite can grow in the tissues of many animals, it lays eggs (oocysts) only in the cells lining the intestines of cats. The eggs are shed in the cat's feces and can cause infection 1 to 5 days later. Eggs in soil can cause infection for several months. Wild birds, rodents, deer, and many domestic animals (especially pigs and sheep) can ingest eggs in food or soil contaminated with cat feces. The eggs release parasites in a form called tachyzoites. Tachyzoites spread throughout the animal's tissues and eventually form cysts.
Treatment of toxoplasmosis
Therapy for acute forms of parasitosis is effective, which cannot be said about other types of pathology, including:
- Intrauterine infection.
- Concomitant immunodeficiency.
- Chronic toxoplasmosis.
This once again confirms the importance of measures that can prevent infection, the essence of which is observing the rules of personal hygiene.
Medicines
Therapeutic regimens have been developed for both animals and humans. The doctor pays special attention to improving immunity, controlling and suppressing parasites. As a rule, this requires several courses and different combinations of immunomodulators, vitamins, minerals, and antiallergic compounds. Protozoa are sensitive to the following medications:
- Delagil.
- Sulfonamides (Norsulfazole, Sulfadimethoxine).
- Antibacterial drugs (Rovamycin or Lincomycin).
Attempts to treat chronic toxoplasmosis are ineffective.
Folk remedies
Alternative medicine methods are safe and can be used in the treatment of pregnant women and children. You can take herbal medicines only after consulting your doctor, since some of them (tansy, wormwood) contain toxic components. Natural infusions and decoctions in the right dosage will remove parasites and also strengthen the immune system.
For enemas you can use tansy. Caution is required when ingesting. To prepare the medicinal composition, take 1 tbsp. l. inflorescences, 2 chopped garlic cloves, simmer for 10 minutes in milk. Strain and use warm for enema.
Decoction recipe
- calendula;
- elecampane;
- calamus;
- aspen (bark);
- eucalyptus.
One tbsp. l. collection, in which all ingredients are taken in equal quantities, pour 250 ml of boiling water and leave for 2 hours. Strain, drink a tablespoon 4 times a day.
Infusion recipe
- three-leaf watch;
- tansy;
- centaury.
Insist for a day. Drink 100 ml in the morning on an empty stomach, 300 ml before lunch, 200 ml before dinner.
Pathogen transmission
Toxoplasmosis can develop in several ways:
- By consuming food, water, or other substances (such as soil) contaminated with cat feces containing Toxoplasma eggs.
- By eating meat that contains Toxoplasma cysts.
- The fetus can become infected from an infected mother.
- In rare cases, due to blood transfusions or organ transplants that contain parasites.
Toxoplasma eggs can enter a person's stomach when they touch their mouth or prepare or eat food without washing their hands after handling contaminated cat litter, soil, or other objects. Cysts can enter the human body by eating raw or undercooked meat (most often pork or lamb) from infected animals.
Tests for toxoplasmosis
Before prescribing an examination, the doctor must visually assess and study the signs of health problems. Have a thorough conversation with the patient and listen to complaints. Examination is the beginning of any diagnosis.
What symptoms indicate toxoplasmosis:
- inflamed lymph nodes in the neck, armpits, and groin;
- clearly expressed enlarged liver;
- impaired coordination and reflex function;
- decreased vision and hearing;
- deviation of body temperature from normal;
- ambiguity of thinking.
But this does not yet indicate that the patient needs treatment for toxoplasmosis. To make a correct diagnosis, a specialist prescribes modern, precise methods for studying the causes and factors that provoke the deterioration of the patient’s condition.
Tests for toxoplasmosis:
- study on TORCH infections. Venous blood collection;
- polymerase chain reaction. Isolation of DNA fragments of the parasite and determination of its type and quantity;
- immunoenzyme blood sampling. The stage of infection, the presence of microorganisms, and examination of the lesion are determined;
- serological. The presence of IgM antibody indicates the presence of an intracellular parasite in the body;
- radiography, CT, ultrasound. Used for visual search of affected inflamed areas.
After all the tests have been carried out, when the diagnosis of toxoplasma is positive, the patient receives recommendations from a specialist on what and how he should be treated.
Do not substitute medications and follow the prescription. Self-treatment will lead to complications and worsening of existing symptoms.
Signs and symptoms
People with healthy immune systems usually have few or no symptoms of toxoplasmosis and recover completely. About 10–20% of these people have enlarged but painless lymph nodes. Some of these people also experience periodic fevers, mild malaise, muscle pain and sometimes a sore throat. Symptoms disappear on their own, usually within a few weeks.
— Congenital toxoplasmosis.
Babies with congenital toxoplasmosis may be severely ill and die before or shortly after birth, or they may develop birth defects or other symptoms. Some children do not get sick at all. Other children appear healthy at first, but develop symptoms (such as epilepsy, mental retardation, and chorioretinitis) months or even years later.
Typical symptoms in newborns may include the following:
- infection of the lining of the back of the eyeball and retina (chorioretinitis);
- enlarged spleen and liver;
- jaundice;
- rash;
- easy bruising;
- seizures (epilepsy);
- large head caused by fluid buildup in the brain (hydrocephalus);
- small head (microcephaly);
- mental retardation.
Chorioretinitis can cause blurred vision, eye pain, sensitivity to light (photophobia), and blindness.
- Symptoms in people with weakened immune systems.
Symptoms of toxoplasmosis in people with weakened immune systems depend on the location of the infection, including:
- Toxoplasmosis of the brain (encephalitis): Symptoms include weakness on one side of the body, speech problems, vision problems, headache, confusion, seizures and coma.
- Toxoplasmosis that has spread throughout the body (acute disseminated toxoplasmosis): Rash, fever, chills, difficulty breathing, and fatigue.
Forms of toxoplasmosis and features of their course
Acute forms of the disease
Depending on the clinical syndrome, medical practice distinguishes between glandular (lymphogangliar), typhus-like (exanthematous), visceral, meningoencephalitic (cerebral) and ocular forms of the disease.
The glandular (lymphogangliar) form is characterized by hypertrophy of the lymph nodes (while they remain painless), headache, fever, disruption of the autonomic nervous system, damage to the liver, spleen and biliary tract.
The typhus-like (exanthematous) form is characterized by an acute onset with fever, chills, headaches, pain in muscles and joints. On days 4-7 from the onset of the disease, a profuse maculopapular rash appears on the body. It spreads throughout the body, with the exception of the plantar area and palms. The lymph nodes, liver and spleen enlarge, the organs of vision and the central nervous system are affected. This form of toxoplasmosis is very difficult and often ends in death.
The visceral form occurs due to the generalization of parasites by the hematogenous route and their damage to various organs. In this case, patients may be diagnosed with interstitial pneumonia, hepatitis, myocarditis and other severe heart damage.
The cerebrospinal form is characterized by signs of acute meningoencephalitis, and symptoms depend on the extent of inflammation in the brain. In this case, the temperature also rises and sometimes a characteristic rash appears, as well as meningeal symptoms and severe intoxication.
Patients may develop paralysis, paresis, psychosis, hearing and vision loss, and death may occur.
In the acute ocular form of toxoplasmosis, damage to the visual apparatus manifests itself in the form of iridocyclitis, choreoretinitis, exudative or serous retinitis and vitreous opacities.
Chronic toxoplasmosis
This form of the disease is characterized by signs of chronic intoxication. Damage to the reticuloendothelial, nervous and cardiovascular systems, musculoskeletal system, digestive tract, and visual organs is noted.
Note: during the period of exacerbation of the pathological process, short-term parasitemia (presence of the pathogen in the peripheral blood) is observed.
Acquired toxoplasmosis
This form can be characterized by various clinical manifestations and severity. The disease occurs in both acute and chronic forms with exacerbations and remissions. In this case, various internal organs, organs of vision and hearing, and the central nervous system are involved in the inflammatory process.
Congenital toxoplasmosis
This form is a consequence of intrauterine infection of the fetus. In the case when transplacental transmission of the pathogen from mother to child occurs in the first trimester of pregnancy, the fetus often dies. If he remains alive, he, as a rule, develops severe lesions of the central nervous system, such as hydrocephalus, acrania, anencephaly, microcephaly, etc.
With later intrauterine infection, the newborn is diagnosed with signs of hydrocephalus, meningoencephalitis and choreoretinitis.
Infection in the last trimester of pregnancy leads to the birth of a child with symptoms of a generalized infection and damage to many internal organs.
Affected Populations
Up to half the world's population is infected with toxoplasmosis. In the United States of America, 23 percent of the population are carriers, in Russia - about 20 percent, and in some areas of the world the proportion of carriers reaches 95 percent.
The global annual incidence of congenital toxoplasmosis is estimated at 190,100 cases. High levels of the disease have been reported in South America, some Middle Eastern countries, and low-income countries. In this regard, this nosology is classified as a group of forgotten diseases.
Congenital toxoplasmosis
When the fetus is infected in utero, congenital toxoplasmosis develops, which in itself is very dangerous for a newborn baby. The severity of the disease depends on the trimester in which the infection occurred. The sooner this happened, the more serious the consequences will be.
There are three forms of congenital toxoplasmosis, which follow one after another:
- The acute form is characterized by severe intoxication of the fetal body, enlargement of the spleen and liver. This course of the disease causes various eye lesions. If the infection occurred shortly before birth, then symptoms may appear a couple of days after birth, in the form of redness of the skin and rashes on it. Yellowness of the skin often appears due to liver damage. There is an increase in lymph nodes that are sensitive to palpation. The child reacts painfully to touching them. Swelling of the face and lower abdomen may occur.
- The subacute form causes encephalitis and meningoencephalitis, characterized by the formation of lesions in the lining of the brain. Symptoms include drowsiness, prolonged or short-term convulsions, paralysis and paresis of the limbs, increased pressure in the cerebrospinal fluid (CSF), the formation of calcifications in the brain and its edema. All these lesions lead to developmental delays, as well as numerous eye pathologies.
- The chronic form indicates that the child suffered from the previous two illnesses in utero. The consequence of this is pathological irreversible changes in the nervous system and organs of vision. Toxoplasma continues to actively multiply in the body of a sick child, which leads to repeated exacerbations.
If the infection occurs at the embryonic stage of fetal development, this often leads to miscarriage or death in the first days after birth, which is why toxoplasmosis is dangerous.
Congenital toxoplasmosis can also occur in a mild form, which does not exclude its manifestation months or years later. Is it possible to cure congenital toxoplasmosis? The disease can be cured, but birth defects will not go away.
Diagnostics
Diagnostics include:
- A blood test to detect antibodies against the parasite.
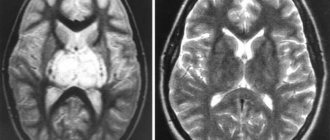
- If there is possible damage to the brain, computed tomography or magnetic resonance imaging followed by a spinal puncture (lumbar puncture).
- Tissue from the brain or other affected organs is examined under a microscope and tested for parasite DNA.
Typically, the diagnosis of toxoplasmosis is based on a blood test, which determines the presence of antibodies to the parasite. (Antibodies are proteins produced by the immune system to protect the body from attacks, including from parasites). A blood test can be used to diagnose a new infection.
These blood tests may be performed in people who have a weakened immune system but do not have symptoms of toxoplasmosis. The purpose of the analysis is to identify a previous infection, the reactivation of which may occur if the immune system is further weakened. However, if the immune system is compromised by AIDS, blood tests may indicate the absence of infection when in fact it is present (false negative results).
Sometimes tests to detect the parasite's genetic material (DNA) are also done on blood samples, tissue taken through a biopsy, or cerebrospinal fluid (the fluid that surrounds the brain and spinal cord) obtained through a spinal tap.
If there are complaints of vision problems, the eyes are examined for lesions characteristic of toxoplasmosis, and blood tests are done to detect antibodies to the parasite.
To check for infection in the fetus, your doctor may take a sample of the fluid around the fetus (amniotic fluid) for testing (a procedure called amniocentesis). This fluid is tested for antibodies to the parasite and to identify the parasite's genetic material. Because it is difficult to diagnose toxoplasmosis during pregnancy, in a fetus, or in a newborn, doctors often consult an expert.
If cerebral toxoplasmosis is suspected, a computed tomography (CT) or magnetic resonance imaging (MRI) scan of the brain is performed, usually followed by a spinal tap to obtain a sample of cerebrospinal fluid. Occasionally, a sample of infected brain tissue is taken and examined under a microscope to determine the presence of parasites and test for the genetic material (DNA) of the parasites.
Pathogens
The causative agent of toxoplasmosis is toxoplasma , the simplest single-celled creature, which, at the same time, turns out to be very complex in its composition and level of adaptability to living conditions. Toxoplasma penetrates the cells of the nervous tissue, the pulmonary epithelium, the cells of the heart muscle and muscles, affecting them.
Toxoplasma affects not only humans: it can exist in the body of many living beings without causing disease in them. Toxoplasma has been found in more than 400 species of living creatures, including mammals and birds.
Moreover, the peculiarity of Toxoplasma is that almost all organisms (including humans) are intermediate hosts of Toxoplasma. This means that Toxoplasma can exist in these organisms, but cannot actively reproduce. This is why Toxoplasma is almost never transmitted from one person to another, except for cases of transplacental infection and infection during organ transplantation.
The same applies to many other animals in whose bodies Toxoplasma can live. You can only get infected from them through raw meat. The exception is cats, or rather the entire large family of cats, which are the definitive (or primary) hosts of toxoplasma. In the body of a cat, toxoplasma goes through its entire life cycle, multiplies there, and cases of human infection with toxoplasmosis are often associated with cats.
Standard Treatments
Treatment includes:
- Pyrimethamine and sulfadiazine, clindamycin or atovaquone plus leucovorin.
- For eye infections - drugs that are effective against toxoplasmosis, plus a corticosteroid.
Most infected individuals without symptoms and with healthy immune systems do not require treatment.
Individuals with symptoms of toxoplasmosis may be treated with pyrimethamine, sulfadiazine, and leucovorin. Leucovorin is intended to protect against decreased production of blood cells in the bone marrow, which is a side effect of pyrimethamine. If pyrimethamine is not available, trimethoprim-sulfamethoxazole can be used. If the patient cannot take sulfadiazine, clindamycin or atovaquone is used instead.
If the immune system is healthy, treatment usually continues for several weeks.
Patients with AIDS and other diseases that weaken the immune system are prescribed the same drugs, but treated for longer (usually at least 6 weeks). Relapses are common, and there are few options for long-term maintenance therapy until the immune system improves.
Toxoplasmosis: treatment during pregnancy
A special group of patients who require individual additional examination and subsequent prescription of drugs. Single-celled microorganisms are very dangerous to the life of the fetus. They penetrate the placenta and infect him.
And the further development of the disease depends on the stage of pregnancy at which the infection occurred:
I trimester . It is difficult to predict the subsequent behavior of the organism at this stage. In most cases, intrauterine fetal death occurs. In the rest - serious damage to the central nervous system, brain, loss of vision, acquisition of chronic disorders of the kidneys and liver;
II trimester . It is characterized by inflammatory processes of the brain, such as encephalitis, and partial or complete loss of vision.
III trimester . After birth, the child will have jaundice, pneumonia, anemia, and developmental delay.
In this case, specialists try to eliminate toxoplasmosis and correctly treat it.
Therefore, therapy is prescribed during pregnancy:
- 12-13 weeks of pregnancy. Spiramycin and Immunoglobulin are administered by injection. Medicines are prescribed individually by a doctor;
- after 16 weeks. "Spiramycin" in tablet form. The daily dose is from 1.5 – 3 grams. The course lasts from 4 to 10 weeks;
- "Fansidar." It is recommended to take 2 tablets once a week. The duration of the course is 2 months. Additionally, the use of folic acid;
- "Rovamycin". Does not affect the fetus. Use only during pregnancy as prescribed by your doctor.
Throughout the entire period of gestation, the mother is under constant supervision by a specialist. If necessary, subject to hospitalization until birth. In case of complications, surgical termination of pregnancy is performed.
Forecast
Immunocompetent patients have an excellent prognosis, and lymphadenopathy and other symptoms usually resolve within a few weeks of infection.
Toxoplasmosis in immunocompromised patients often recurs if treatment is stopped. Suppressive therapy and immune reconstitution significantly reduce the risk of recurrent infection.
Individuals with congenital toxoplasmosis may experience multiple complications, including mental retardation, seizures, deafness, and blindness. Treatment can prevent the development of adverse effects in symptomatic and asymptomatic children with congenital toxoplasmosis. Children with congenital toxoplasmosis usually have a good prognosis and by the fourth year of life are on average identical in development to uninfected children.
Toxoplasmic encephalitis and brain abscess can lead to permanent neurological complications, depending on the location of the lesion and the degree of local damage and inflammation. The basal ganglia appear to be predominantly involved. People with CNS toxoplasmosis may develop a seizure disorder or focal neurological deficit.
General symptoms of toxoplasmosis
It is quite difficult to identify identical processes. Signs that indicate disease processes should be considered only based on the forms corresponding to the disease.
Spicy . Rarely, enlarged lymph nodes in the armpits, groin, and neck can be observed. Characteristic pain symptoms in the right hypochondrium, indicating liver dysfunction. Temperature rises to 39°C. Sometimes treatment is not required. After 1-2 weeks, spontaneous recovery occurs.
Chronic . Mostly it is weak. Often shows no symptoms. Headaches, weakness, fever. If you do not contact a specialist in a timely manner, your health may worsen and worsen.
Congenital . The baby develops severe complications after birth: jaundice, rash, disproportionate head size, lack of hearing and vision, mental and physical development retardation.
Purchased or distributed . The reason is decreased immunity. Inflammatory processes spread to all organs and systems with characteristic signs of their disorders. This includes HIV-infected patients, patients of oncology clinics, people after organ transplantation.
Ocular . The risk group is teenagers. Late manifestation of congenital acquired toxoplasmosis. Provokes pain in the eyes, loss of concentration and sharpness, blindness.
Cerebral . Brain damage. Leads to migraines, loss of sensitivity, paralysis, coma.
Prevention
Pregnant women should avoid contact with cats. If exposure is unavoidable, pregnant women should, at a minimum, avoid cleaning the cat's litter box or wear gloves during such cleaning.
The meat must be thoroughly cooked to a temperature of 74–77°C. After handling raw meat, soil, or cleaning cat litter, you should thoroughly wash your hands.
Potential organ donors must undergo tests to prevent the spread of the parasite during organ transplants.
Trimethoprim-sulfamethoxazole (an antibiotic) may be used to prevent reactivation of toxoplasmosis in people with AIDS or people whose immune systems are otherwise weakened. If a person cannot take this drug, pyrimethamine (an antiprotozoal drug) combined with sulfadiazine or clindamycin (antibiotics) can be substituted. Other options are atovaquone (an antiprotozoal drug) with or without pyrimethamine, or dapsone in combination with pyrimethamine. Because pyrimethamine can reduce the production of blood cells in the bone marrow, leucovorin (also known as folinic acid) is given concomitantly to prevent this side effect.
People with AIDS are also prescribed antiretroviral drugs to help strengthen the immune system and reduce the risk of reactivation of toxoplasmosis.
Pregnancy
During pregnancy, toxoplasmosis is asymptomatic and can only be determined through laboratory tests. In some cases, patients complain of the following symptoms:
- Migraine.
- Lymphadenitis.
- Low-grade fever.
- Cold symptoms. Therefore, the woman assumes that she has a common cold and delays going to the doctor.
In the chronic course of the disease, neurological disorders, decreased visual acuity, and internal damage are added to the general symptoms. In severe stages of infection, skin rashes, fever, and pain in muscles and joints appear.
If the infection has passed before the child is conceived, then a pregnant woman is not afraid of it, since the immune system can independently cope with the pathogen. If the infection is primary during pregnancy, then toxoplasma affects the child, penetrating the placental barrier. The severity and severity of the period is associated with the duration of pregnancy: the higher it is, the greater the chance of the child being born healthy.
It may also be interesting: What you need to know about trichuriasis
Doctors cannot say that during pregnancy the pathogen is an indicator of abortion. However, if the patient has antibodies to the pathogen, the risk of having a baby with abnormalities is high. A woman must make a choice: to terminate the pregnancy or not.
If there are no antibodies to toxoplasma during pregnancy, you will have to be tested monthly. Then the chances of giving birth to a healthy baby increase.
Classification of toxoplasmosis
Acquired
More than 90% of patients do not feel any symptoms of the disease.
The acquired disease can be secretive (latent), acute or chronic. The latent course is divided into primary and secondary periods (after exacerbation or relapse of chronic toxoplasmosis). 95−99% of patients infected with toxoplasmosis do not experience any symptoms, since the infection has a latent form. An acute form of infection with characteristic manifestations develops over an incubation period of 2–3 weeks. Primary chronic toxoplasmosis can be sluggish.
Congenital
Toxoplasmosis, like cytomegalovirus infection, can be transmitted from a sick mother to her child. If a woman falls ill before the 20th week of pregnancy, this is a fatal prognosis for the baby. Most often, the fetus dies due to fatal developmental defects. When infection occurs after the 20th week of pregnancy, the baby survives but is found to have severe brain damage after birth. An infant develops acute toxoplasmosis while he is still in the womb. After birth, active meningoencephalitis and its manifestations are observed. In this case, toxoplasmosis will never be cured.
Complications of toxoplasmosis
As has already become clear, toxoplasmosis is a dangerous disease, the presence of which you may not even suspect. Since the infection rate is very high, it is necessary to closely monitor your health and promptly consult a doctor if you have any alarming symptoms. And this applies not only to this disease, but to all others
The consequences of toxoplasmosis are dangerous, which can lead to death:
- toxic shock - a disease that provokes the failure of all vital organs;
- encephalitis or inflammation of the brain;
- cerebral edema;
- arachnoiditis - damage to the spinal cord or arachnoid membrane of the brain;
- epilepsy;
- paralysis;
- paresis of the limbs - loss of muscle tone and impairment of their motor function;
- atrophy of the optic nerve, leading to blindness due to the replacement of nerve fibers with connective tissue;
- endocarditis – inflammation of the inner lining of the heart;
- pneumonia.
Among other things, toxoplasmosis significantly depletes the human immune system, which entails a lot of different diseases. It is this pathogen that causes the death of most HIV-positive people. Toxoplasmosis in men also threatens sexual dysfunction, and in women during pregnancy it causes fetal pathologies and even miscarriages.
What is toxoplasmosis
There is no clearly established classification of toxoplasmosis; experts adhere to several criteria:
- mechanism of occurrence - congenital and acquired toxoplasmosis are distinguished;
- severity - acute, chronic, erased or latent toxoplasmosis, the symptoms and treatment of which vary significantly.
What toxoplasmosis is can be understood by studying the characteristics of the parasite’s activity. Once in the intestines, the infection penetrates the circulatory and lymphatic systems and spreads throughout the internal organs, forming accumulations of parasites in the tissues in the form of pseudocysts. These formations may not show themselves for decades. The carrier of the parasite is considered relatively healthy - he does not have the disease toxoplasmosis. Such a latent course is typical when people with a strong immune system are infected.
Clinical signs of toxoplasmosis in humans are nonspecific and varied. One of the characteristic symptoms of the disease is the so-called calcinomas - limited areas of necrosis of tissue structures susceptible to calcification. When palpated in the thickness of the muscles, they are felt as solid formations.
Disease prevention
By following simple rules, you can protect yourself from infection, since treating toxoplasmosis is more difficult than preventing it. Prevention of toxoplasmosis consists of:
- You cannot eat meat that has not undergone heat treatment, as well as unwashed vegetables and fruits. Refrain from buying ready-made food from dubious places, because you cannot be 100% sure of the quality of the products and the method of their preparation.
- If you take a cat from the street, have it diagnosed by a veterinarian. Testing is also necessary for free-ranging domestic cats.
- Wash your hands well after working in the garden or playing in the sandbox, because there may be animal feces containing toxoplasma.
And finally, I would like to remind you that your health may depend on timely contact with a specialist, and self-medication will only worsen the situation.
Diagnosis of toxoplasmosis
Initial diagnosis consists of a detailed history and examination of the patient. The doctor should ask about the patient’s living conditions, the presence of concomitant diseases, bad habits, find out whether there was contact with animals, and whether the person has allergies. If the infection is in the acute stage, examination of the patient will reveal:
- increased subfebrile body temperature;
- enlarged lymph nodes, liver, spleen;
- pain in internal organs upon palpation;
- a general blood test will reveal antibodies, leukocytosis, monocytosis, lymphocytosis.
The examination of a patient with a chronic form of toxoplasmosis will take place in several stages:
- Examination of the cardiovascular system. When listening to the heart, tachycardia and arrhythmia may be observed. The patient himself will complain of sudden jumps in blood pressure, pain in the heart area, and weakness.
- Palpation of the gastrointestinal tract. During diagnosis, increased size of the liver, spleen, and pain in the epigastric zone will be observed. The patient's complaints will be directed toward bloating, nausea, constipation, loss of appetite, and constant dry mouth.
- Palpation of muscles. Diagnostics will help detect tightness in the muscles, hypertonicity, and limited joint mobility. The affected person will complain of muscle soreness, weakness, periodic inflammation of large cartilaginous tissues - elbows, knees, ankles.
Laboratory research
Various laboratory diagnostic methods help doctors make an accurate diagnosis. Of particular importance are:
- Allergological method. The test involves giving a person an allergy test by injecting a small amount of toxoplasmosis pathogens under the skin. The drug is administered into the shoulder area in an amount of 0.1 ml. After a while, redness or infiltration (accumulation of the drug in the tissues) appears at the puncture site. If the radius of redness is up to 13 mm, the reaction is considered negative. If the size of the circle exceeds 14 mm, the reaction is positive, the patient needs treatment .
- Parasitological method. Diagnosis is based on the collection and examination of various body fluids for the presence of toxoplasma or antibodies to them. Suitable for diagnosis are blood, cerebrospinal fluid, pieces of tissue from a lymph node (biopsy), amniotic fluid.
Article on the topic: How to treat spinal spondyloarthrosis?
The most effective laboratory test is the serological method. This diagnosis is carried out by collecting venous blood and then filtering it to obtain liquid serum. The material is tested for specific antibodies to pathogens:
- the presence of Ig M antibodies means that a person is infected with toxoplasma and the disease is in an acute or chronic stage;
- detection of Ig G antibodies means that the infection was completely destroyed.
Venous blood can retain specific antibodies for six days, so sometimes the material can be subjected to additional diagnostics. Among other serological tests, the following are often used to diagnose toxoplasmosis:
- Compliment binding reaction. Starting from the second week of the disease, the reaction to the binding of antibodies to compliments will be positive.
- RIF (immunofluorescence reaction). This method helps to identify the antibody-antigen complex. The taken sample of biomaterial is treated with fluorochrome. If a greenish glow is subsequently observed in the smear, the reaction is considered positive, and the patient is prescribed appropriate treatment.
- Enzyme-linked immunosorbent assay (ELISA). This analysis helps to identify the presence and quantity of different antibodies or anti-agents of infection.
Instrumental
To clarify the diagnosis and identify abnormalities in the functioning of various organs and systems of the body, the doctor may prescribe additional instrumental diagnostic methods. These include:
- Electrocardiogram - shows whether there are abnormalities in the functioning of the heart.
- Comprehensive ultrasound (ultrasound examination) of the abdominal organs. Necessary to determine the size of the liver, spleen, and pancreas.
- X-ray of lungs and tissues. Gives doctors an idea of what the cartilage tissue looks like and whether there is damage to the musculoskeletal system.
- Perimetry, refractometry and other methods determine the presence of ophthalmological problems.
Treatment of infection
An adult needs therapy only if the infection is acute and the symptoms of toxoplasmosis are pronounced. Treatment of toxoplasmosis in adults who are sick from birth is carried out under any conditions and lasts a lifetime. When an adult is considered to be a carrier of the parasite and toxoplasmosis does not manifest itself in any way, therapy is not needed, since the adult’s life is not in danger.
Characteristics of drug therapy
Biseptol is often prescribed for the treatment of toxoplasmosis.
The main goal of therapy is to stop the infectivity of the causative agent of toxoplasmosis. For the treatment of acute toxoplasmosis, sulfonamides are used in combination with Chloridine and Delagil. In addition, antibiotics from the tetracycline group are used. The most commonly prescribed drugs are Biseptol or Rovamycin for toxoplasmosis. The active ingredient spiramycin in the drug "Rovamycin" is well tolerated by patients and does not interact with other drugs. The entire course of treatment is selected individually for each patient.
For almost all cases of infectious infection, including chronic ones, medications are used to maintain immunity, vitamins, antihistamines to reduce the allergic reaction to toxins secreted by parasites, and the symptoms are cured. An adult can recover at home or treat the infection in a hospital, since it does not threaten the health of others.
Folk remedies
To get rid of toxoplasmosis, on the advice of a doctor, traditional medicine recipes are used along with medications. An adult can get rid of toxoplasmosis using herbal decoctions. The collection may include chamomile flowers, eucalyptus, wormwood, calendula, aspen, and gentian. To prepare a medicine for toxoplasmosis you will need 50 g of dried gentian roots, 50 g of wormwood, 100 g of chamomile and tansy flowers, 120 g of buckthorn bark. The ingredients should be crushed and mixed. The product is prepared at the rate of: 1 tablespoon of mixture with herbs per 1 glass of boiling water. The decoction must be infused for 12 hours in a thermos. The medicine is taken 1 hour before meals on an empty stomach. Treatment of toxoplasmosis with folk remedies lasts 1 week.
Garlic is used to cure the infection. A decoction is also prepared from it. The recipe is as follows: several cloves are peeled, crushed with a knife and placed in a saucepan. Next, pour the vegetable with a glass of milk and cook over low heat for 15 minutes. The resulting product should be drunk in small portions throughout the day. The patient is treated this way for 10 days.
Main features
The absence of symptoms does not guarantee the absence of consequences of the disease. Therefore, it is worth considering the main signs of toxoplasmosis:
- periodically the body temperature rises slightly;
- lymph nodes become inflamed;
- headaches may occur;
- the liver and spleen increase in size;
- performance decreases, memory deteriorates;
- apathy occurs;
- appetite and sleep are disturbed.
Toxoplasmosis is divided into acute and latent. In humans, it occurs in a chronic or latent form and practically does not manifest itself. In the acute period, the disease is quite rare. Very often these people have a weak immune system or are HIV positive. In acute form it causes the following symptoms:
- high body temperature;
- enlarged lymph nodes, spleen, liver;
- a rash or signs of jaundice appear on the body;
- vision problems;
- lethargy, drowsiness, decreased muscle tone.
These symptoms can appear in other diseases, so doubts arise: whether it is necessary to treat toxoplasmosis or whether it is better to start curing for other diseases. Considering that this is a rather serious disease, at the first signs of the disease, it is necessary to begin treatment immediately. Inaction sometimes leads to destructive actions in the body.