This rather rare and sometimes very dangerous cardiac anomaly was first described in 1866 by the German pathologist Ebstein. It was after him that this congenital malformation of the tricuspid (three-leaf) valve, separating the right ventricle and the atrium, was named. According to statistics, such a valve defect is observed in approximately 0.5-1% of patients with congenital heart defects.
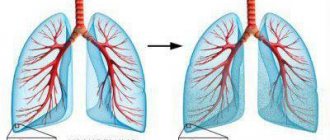
With Ebstein's anomaly, the petals of the tricuspid valve seem to shift towards the cavity of the right ventricle. This arrangement leads to the fact that the volume of the ventricular chamber is significantly reduced, and the cavity of the right atrium increases (sometimes up to a volume of 2.5 liters). Due to the displacement, the ventricle cannot pump enough blood into the pulmonary circulation, and pulmonary blood flow is reduced. As a result, venous blood entering the lungs from the right ventricle cannot be fully enriched with oxygen, and all organs and tissues of the body suffer from hypoxia.
In the absence of timely treatment, Ebstein's anomaly leads to severe hemodynamic disturbances, causing progression of heart failure, thromboembolic complications, supraventricular arrhythmias and bacterial endocarditis. In some cases, this congenital defect can provoke severe arrhythmias, leading to sudden coronary death.
According to doctors' observations, Ebstein's anomaly is often combined with other heart defects. These are pulmonary atresia or stenosis, patent duct aorta, WPW syndrome, chamber septal defects, mitral regurgitation or stenosis. Most often, in patients with such a congenital defect, a concomitant anomaly is a defect in the interatrial septum. Combined defects lead to even greater hemodynamic impairment and oxygen starvation. In addition, the patient has an increased risk of thromboembolic complications.
In this article we will introduce you to the causes, manifestations, prognosis, methods of diagnosing and eliminating Ebstein's anomaly. This information will help you notice the first warning signs in time, and you will be able to ask your doctor any questions you may have.
Causes
Bad habits of a pregnant woman significantly increase the risk of developing congenital heart defects in the fetus.
So far, scientists cannot establish the exact causes of the development of this congenital heart defect. However, according to the observations of cardiologists, predisposing factors for the occurrence of Ebstein’s anomaly may be:
- genetic causes - provoked by point changes in genes or chromosomal mutations;
- environmental factors - gene mutations occur under the influence of physical, chemical and biological mutagens.
Environmental factors include the following external causes that affect the body of the expectant mother and fetus:
- radiation;
- lithium;
- nitrates;
- alcohol;
- phenols;
- benzopyrene (enters the bloodstream when smoking);
- some medications (cytostatics, antibiotics);
- toxicosis;
- risk of miscarriage;
- infections: pathogens of rubella, measles, scarlet fever;
- thyrotoxicosis;
- systemic lupus erythematosus;
- severe forms of anemia;
- phenylketonuria;
- diabetes.
Many experts often associate the occurrence of Ebstein's anomaly with lithium entering the body of the expectant mother in the early stages of pregnancy.
Reasons for development
The main cause of Ebstein's anomaly is chromosomal abnormalities. They arise already at the moment of conception, provoking improper development of internal organs, including the heart. The disorder can be predicted by first performing a genetic examination.
Factors that increase the risk of developing Ebstein's anomaly:
- mother's bad habits;
- severe autoimmune diseases;
- diabetes mellitus, epilepsy;
- severe forms of early toxicosis;
- past infectious and viral diseases;
- taking certain drugs with mutagenic properties;
- drug addiction and alcoholism;
- intoxication of the body.
According to the latest data, such anomalies in the development of the heart in the fetus can be caused by a woman taking lithium and drugs from the benzodiazepine group in the first trimester of pregnancy.
In addition, disruption of intrauterine development can be caused by the action of pesticides, aggressive household chemicals, components of paint and varnish products and other toxic substances. Thus, the risk group includes people living in areas with unfavorable ecology, for example, large industrial regions.
The sudden appearance of Ebstein's anomaly in adults is impossible, since it is a congenital pathology. In isolated cases, it does not appear immediately, and then it can first make itself felt in adulthood, but most often this happens at a maximum of 3-4 years.
The pathology is very dangerous and must be detected in a timely manner.
Anatomical variants of the anomaly
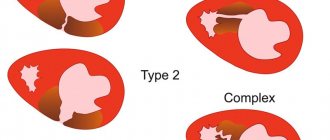
Depending on the nature of the lesion of the tricuspid valve, four variants of Ebstein’s anomaly are distinguished:
- I – the posterior and septal valve leaflets are shifted or completely absent, the anterior leaflet is mobile and large;
- II – all three valves are present, but they are reduced in size and shifted towards the apex of the heart;
- III – the posterior and septal valves are displaced and not fully developed, and too short chords of the anterior valve limit its adequate mobility;
- IV – the posterior leaflet is absent or underdeveloped, the septal one is formed from fibrous tissue, and the anterior one is deformed and shifted towards the outlet of the right ventricle.
The severity of damage and displacement of the tricuspid valve and the presence of concomitant heart defects determine the degree of hemodynamic disturbances and symptoms of Ebstein's anomaly.
Classification of the disease
Ebstein's anomaly in a newborn has several varieties, differing in anatomical variant:
- Type 1 - the anterior leaflet of the tricuspid valve has large volumes and is well mobile, the septal or posterior leaflet is displaced or completely absent;
- type 2 - the presence of all 3 leaflets of the atrioventricular valve is noted, but their sizes are shifted, which is why they are directed towards the apex of the heart;
- Type 3 - the valve chords are shortened and limit its movement, the septal or posterior leaflet is underdeveloped and displaced;
- Type 4 - the anterior valve leaflet has succumbed to deformation and is displaced towards the outflow tract of the right ventricle, the septal leaflet consists of fibrous tissue, and the posterior one is underdeveloped or does not exist.
Pathology in terms of severity suggests the following stages:
- Stage 1 - observed extremely rarely, has a completely asymptomatic course.
- Stage 2 - the presence of clinical signs is noted. It is divided into 2 types: the first 2a - without changes in heart rate, the second 2b - with paroxysmal arrhythmia.
- Stage 3 - decompensation of the disease.
Symptoms
Based on the patient’s complaints, medical history and objective examination (auscultation), the doctor will suspect a heart defect and prescribe additional diagnostic methods to the patient.
Depending on the degree of hemodynamic disturbances, three stages of the course of Ebstein’s anomaly are distinguished:
- I – asymptomatic (rarely observed);
- II (A and B) – pronounced hemodynamic disturbances (with option A without arrhythmias, with option B with arrhythmias);
- III – decompensated cardiac failure.
In extremely severe forms of Ebstein's anomaly, death can occur during fetal development.
Most often, this tricuspid valve defect begins to manifest itself in early childhood, and in more rare cases, with an asymptomatic course, its first symptoms may appear only in adolescence or young adulthood. In mild forms, the only sign of pathology is blueness of the lips and skin.
Typically, Ebstein's anomaly appears in the first months or years of a child's life, and in severe forms it is detected in the maternity hospital. Symptoms of such a heart defect may be as follows:
- cyanosis of mucous membranes and skin;
- increased fatigue;
- pronounced decrease in tolerance to physical activity;
- dyspnea;
- attacks of heart failure and palpitations;
- chest pain;
- bulging of the right atrium to the left of the sternum (“heart hump”);
- arrhythmia or WPW syndrome (approximately 25-50% of patients);
- hypotension;
- swelling.
When examining a patient, the doctor may reveal:
- systolic and diastolic murmur to the right of the xiphoid process;
- three- or four-beat rhythm;
- second tone splitting;
- displacement of the borders of the heart to the right.
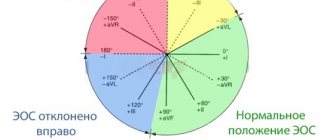
The following abnormalities may be detected on the ECG:
- signs of expansion and hypertrophy of the right ventricle;
- EOS deviation to the right;
- arrhythmias.
A phonocardiogram reveals:
- systolic murmur in the projection of the right ventricle;
- greater amplitude of the third and fourth tones;
- delay of the first and bifurcation of the second tone.
As heart failure progresses, patients experience noticeable pulsation and swelling of the veins in the neck, the liver becomes enlarged, swelling in the legs increases, fingers take on the appearance of drumsticks, and nails become like watch glasses. Severe cardiac decompensation leads to death. In addition, as the disease progresses, arrhythmias become more severe and can lead to sudden cardiac death.
Ebstein's anomaly: symptoms
It should be noted that newborns do not always have symptoms. The fact is that at birth, many babies have an oval window - from it blood can flow from the right atrium to the left, thereby compensating for the defect. In this case, two deviations in the heart balance each other, creating a certain balance.
If we are talking about adolescence or an adult, then the following signs of Ebstein’s anomaly may be observed:
- cyanosis of mucous membranes and skin;
- dyspnea;
- increased fatigue;
- the heart begins to lose rhythm.
Once significant failure occurs (when the right ventricle is unable to cope with pulmonary blood flow), edema occurs.
The rate of change and the manifestation of symptoms depend on how much Ebstein's anomaly has damaged the valve. Surgery at a young age is performed only in emergency cases. In general, people try not to undergo surgery before the age of 15.
Taking medications is necessary, because without them:
- there is a lack of oxygen;
- tissues do not receive proper nutrition;
- growth of the cardiac hump is observed.
In addition, Ebstein's anomaly can cause serious complications:
- fatal arrhythmia;
- cardiac arrest - often fatal;
- stroke - bleeding in the brain.
Patients diagnosed with right ventricular development disorder or defect should follow an individual examination plan.
Diseases often cause discomfort
Diagnostics
If Ebstein's anomaly is suspected, the patient is scheduled to consult a cardiologist and cardiac surgeon. To assess the condition of the tricuspid valve and heart structures, the following studies are prescribed:
- ECG (regular and Holter);
- phonocardiography;
- Echo-CG;
- X-ray of the chest organs.
For a more detailed clarification of the severity of Ebstein's anomaly, the following additional methods of examining the heart may be prescribed:
- MRI;
- ventriculography;
- cardiac catheterization.
In 60% of cases, Ebstein's anomaly can be detected in the fetus. For this purpose, a fetal echocardiogram is performed.
Treatment
Ebstein's anomaly can only be corrected surgically. The choice of time to perform the intervention is determined by the patient’s condition. In the absence of pronounced signs of heart failure and the risk of complications, surgery can be postponed until 15-17 years. This is explained by the fact that the goal of surgical treatment for such a pathology is aimed at completely correcting the malformation of the tricuspid valve, and its replacement is best done when the size of the heart approaches that of an adult.
Before the operation or if the patient refuses the intervention, medications are prescribed to stabilize the heart. Their choice is determined by the clinical case.
Conservative therapy
To maintain cardiac activity in case of Ebstein's anomaly, the following medications can be prescribed:
- cardiac glycosides;
- diuretics;
- ACE inhibitors;
- calcium channel blockers;
- beta blockers;
- antiarrhythmic drugs (if arrhythmias are present).
Patients with this tricuspid valve defect should reduce physical activity. The amount of permissible load is determined by the clinical case and is recommended by the doctor individually.
Surgery
Ebstein's anomaly can only be eliminated surgically.
The main goal of treatment for Ebstein's anomaly is to eliminate the tricuspid valve defect, i.e. for its replacement or reconstruction.
The following prostheses can be used for prosthetics:
- biological - valves from the heart of a pig;
- mechanical - devices made of synthetic materials and metal.
The choice of valve prosthesis depends on the clinical case. When using biological prostheses, the patient will not need to take medications to ensure the normal functioning of the implanted valve. And after the introduction of a mechanical prosthesis, patients have to constantly take medications that thin the blood and prevent blood clots from settling on the valve leaflets. An important criterion for the patient is the fact that a mechanical prosthesis is more durable and, with proper medication use, can last for decades.
When planning a valve replacement operation, the doctor must familiarize the patient with all the intricacies of the upcoming operation and life after it. In addition, the patient should be aware of the expected results of the planned intervention. As a rule, tricuspid valve replacement is successful in 90% of patients.
If, due to deteriorating health conditions, the operation cannot be postponed until 15-17 years of age or the tricuspid valve is subject to correction, then the patient undergoes reconstructive surgery to repair the abnormal valve:
- plastic surgery according to Boyd;
- annuloplasty with a support ring according to Carpentier;
- annuloplasty according to Amosov;
- suture annuloplasty according to De Vega.
In the presence of concomitant defects and pathologies with Ebstein's anomaly, the following cardiac surgeries can be performed:
- repair of atrial septal defect;
- Fontan operation;
- elimination of the dilated right atrium;
- anastomosis according to Blalock-Taussig.
In case of disturbances in the conduction system and heart rhythm, the following interventions can be performed:
- for WPW syndrome – radiofrequency ablation;
- for arrhythmias - implantation of a cardioverter-defibrillator or pacemaker.
After surgical treatment, the patient is prescribed medications and follow-up with a cardiologist.
Forecast
In the absence of surgical treatment, the prognosis of Ebstein's anomaly is always unfavorable. With a severe defect, approximately 6.5% of patients die in the first year of life, by 10 years - 33%, and by 30-40 - 80-87%.
After surgical treatment, the prognosis becomes favorable, and work capacity is restored in about a year. Long-term consequences of cardiac surgery include the occurrence of postoperative arrhythmias and severe cardiomegaly.
Ebstein's anomaly is a rare congenital valve defect. The severity of its manifestations depends on the degree of damage to the tricuspid valve, hemodynamic disorders and the presence of concomitant defects in the heart structures. This anomaly can only be corrected surgically. The time and technique of such operations are selected individually and depend on the patient’s condition.