Causes
The causes of all forms of angina include the appearance of atherosclerotic formations on the inner walls of the heart arteries.
When plaques significantly close the lumen of the vessel, then there is insufficient blood supply to the myocardium. At high loads, the heart needs a larger portion of oxygen, but the affected arteries cannot satisfy this need. Oxygen starvation leads to chest pain.
The development of angina may occur more quickly under certain circumstances. These risk factors include:
- age category of people over 45 years old;
- high blood pressure;
- diabetes mellitus;
- smoking;
- alcohol addiction;
- increased blood clotting.
Mainly men are susceptible to the disease.
As a rule, angina develops against the background of atherosclerosis of the coronary vessels, in which atherosclerotic plaques form on their walls. Such formations narrow the lumen of blood vessels, which prevents the flow of oxygen-rich blood.
An attack of angina pectoris occurs at the moment of oxygen starvation, when the lumen of the arteries decreases by 50-70%. Sometimes angina develops against the background of other diseases:
- allergies and infectious lesions of the body;
- vasculitis, arthritis and other complications after rheumatism;
- diseases of the gastrointestinal tract, etc.
Treatment of unstable angina
The goal of therapy is to prevent myocardial infarction.
Treatment is carried out in a hospital, tactics are chosen based on ECG results.
The patient is prescribed bed rest. Directions of therapy:
- eliminate cardialgia;
- get rid of the underlying disease.
Treatment of all forms of angina with an unstable course is complex, the following methods are used:
- use of medications - injections, infusions, tablets before and after surgery;
- surgical intervention - in case of a variant form of the disease, the development of severe complications;
- diet therapy - reduces the risk of a recurrent attack, improves the condition of blood vessels and blood flow.
Medication
As a pain reliever during an attack of angina, the patient is given Nitroglycerin under the tongue and administered through a dropper with Heparin. Afterwards, to treat an unstable form of pathology in order to eliminate its symptoms, the following drugs are used:
- Anticoagulants (Heparin) - inhibit blood clotting and thin it, preventing the formation of blood clots. Administration intravenous and subcutaneous.
- Lipid-lowering drugs (Atorvastatin) - normalize cholesterol levels in patients with atherosclerosis. Used in tablets, they reduce the risk of new attacks of angina.
- Disaggregants (Clopidogrel, Aspirin) – prevent platelets from sticking together.
- Calcium channel antagonists (Verapamil) - reduce myocardial oxygen demand, dilate blood vessels and improve blood supply to the heart.
- Diuretics (Furosemide) - eliminate swelling, remove excess fluid, are indicated for heart failure.
- ACE inhibitors (Enalapril) - block the synthesis of an enzyme that constricts blood vessels, reducing blood pressure.
- Beta-blockers (Anaprilin) - reduce the strength and frequency of heart contractions, are prohibited for Prinzmetal's angina.
Surgical
In case of a large area of ischemia, rapid progression of pathology, heart failure and damage to large arteries, an operation is indicated, which is performed using the following methods:
- Angioplasty is a minimally invasive treatment in which the doctor inflates the lumen of a narrowed vessel using a catheter with a balloon. The operation is performed through a puncture of the femoral artery with local anesthesia. Symptoms of the pathology disappear completely in 60% of patients.
- Coronary artery bypass grafting is performed when the main artery stenosis is above 50%. The doctor creates a bypass for blood flow through a shunt, which is attached below the area of narrowing of the lumen and to the aorta. The condition improves in 80% of patients, angina resolves in 63%. The risk of heart attack after such an operation is 7%.
- Intracoronary prosthetics or stenting - a conductor is inserted into the area of narrowing of the artery and a balloon catheter is placed. He inflates the vessel and the doctor places a stent in the area of stenosis: a tube made of metal fibers. The design expands the gap and prevents the walls from sticking together. The stent is drug-coated, which reduces the risk of new stenosis. The disadvantage of this design is that it slowly “grows together” with the wall of the vessel.
Etiology of the disease
The main etiological factor in which coronary heart disease develops is atherosclerotic damage to the choroid plexus. With vascular atherosclerosis, cholesterol is deposited in the area of damage to the vessel wall, and gradually, due to the formation of a cholesterol plaque, the lumen of the arterial vessels narrows.
The severity of symptomatic signs depends on the degree of obturation. Unstable angina also develops against the background of a disease such as increased blood clotting. When this disorder occurs, the risk of blood clot formation increases.
Persons predisposed to developing the disease:
- patients with chronic diseases of the pancreas, diabetes mellitus;
- diseases associated with transmission at the genetic level;
- excess body weight;
- bad habits;
- sedentary lifestyle.
Angina: stable and unstable
Stable angina is characterized by a certain set of factors:
- unfavorable weather conditions with cold wind, rain, snow;
- emotional stress;
- clearly established limits of physical activity (example: brisk walking more than 500m, climbing stairs above the first floor).
Stable angina can belong to one of 4 functional classes, each of which has its own permissible level of physical activity and its own degree of severity of the clinical picture.
The attack ends at rest, lasts no more than 15 minutes, and is easily controlled with Nitroglycerin.
Unstable angina poses a great danger because it is impossible to accurately predict its appearance and clinical picture (set of symptoms), there is no way to dose the level of stress for the patient, and it is difficult to identify provoking factors.
Each such attack occurs suddenly, is unpredictable in its manifestation and threatens to develop into a myocardial infarction; the patient may die from sudden cardiac arrest.
The symptoms in this case are more severe, the duration of the dangerous condition reaches 30 minutes, the Nitroglycerin tablet does not help much.
Causes of unstable angina
What is unstable angina in terms of etiology, what are the possible mechanisms of its development?
A prerequisite for an attack in IHD is narrowing of the coronary arteries. Excess cholesterol settles on the walls of the vessel, atherosclerotic plaques appear, which means a decrease in its lumen.
Not enough blood reaches the heart. The myocardium is forced to work even harder to make up for this deficiency, but the situation is getting worse.
Indeed, with increased activity, the heart muscle requires even more oxygen, which can only come with blood.
When arterial patency deteriorates by more than 50%, hypoxia (oxygen starvation) of the myocardium intensifies and reaches a critical limit.
Metabolic processes in cells are disrupted, and this phenomenon is accompanied by a pathological change in the intracellular structure. At this moment the person feels severe angina pain.
A prolonged attack provokes the onset and further spread of tissue necrosis (death). The patient is diagnosed with myocardial infarction.
Stable angina pectoris occurs when the heart urgently needs a larger portion of oxygen (physical activity, stress), and the affected coronary vessels cannot supply the organ with enough blood.
If a cholesterol plaque grows to a significant size, its integrity may be compromised. This happens when it contains a lot of fatty deposits, but lacks collagen, there is inflammation of the vascular wall, or increased blood viscosity.
The detached part “sticks” with platelets and forms a thrombus, which can completely block the lumen of the artery or leave a very narrow passage. This is the main cause of unstable angina.
Such clots can migrate, penetrating into any part of the coronary vessel.
Another cause of the pathology is a sudden spasm of the coronary vessels; it occurs regardless of the load. Moreover, narrowing of arteries that are not affected by atherosclerosis is possible. This phenomenon is typical for Prinzmetal angina (vasospastic, variant) - a very rare disease.
In addition to the main reasons for the manifestation of unstable angiotic attacks, there are a number of factors that increase the risk of developing such a symptomatic complex:
- physical stress beyond measure;
- physical inactivity;
- lack of rest and night sleep;
- obesity;
- bad heredity;
- Marfan disease;
- high blood cholesterol;
- increased sensitivity of blood vessels to serotonin or other vasoactive substances;
- intense expression of emotions, stressful situation, high mental stress;
- progressive hypertension;
- the harmful effects of tobacco tar and ethyl alcohol;
- cardiac diseases (chronic myocardial failure, post-infarction condition, hypertrophic type cardiomyopathy, heart defects);
- diseases not related to the heart (iron deficiency anemia, thyroid pathologies, diabetes mellitus).
Braunwald classification
Among other classifications, the division of unstable angina into classes and levels, proposed back in the 19th century by the American cardiologist Braunwald, has become widespread.
- The doctor classified angina pectoris of the secondary type as class A. Pathological symptoms in this case arise under the influence of additional factors (extracoronary adhesion) that contribute to the aggravation of coronary disease: anemia, fever, infectious attack, unstable heart rhythm, hypotension, the presence of hypertension (difficult to treat), a strong emotional outburst.
- Class B includes the so-called primary angina syndromes. They develop in diseases of the heart and coronary circulatory system.
- Class C includes unstable angina detected after a myocardial infarction (in the first 10-14 days).
In accordance with the Baunwald classification, the classes of unstable angina reflect the clinical circumstances of the occurrence of ischemic symptoms, which are characterized by instability of manifestation.
The following groups characterize the severity of the ongoing attack:
- The first group is angina pectoris, recorded for the first time during the month preceding the day of going to the hospital. Manifests itself stably under conditions of physical activity.
- The second group of unstable angina according to the classification is subacute syndrome. The attacks are more severe, they began to occur in a calm state. Time of occurrence – last month, with the exception of 2 days preceding the doctor’s appointment.
- The third group is an acute symptomatic complex. Angious pains haunt a person without reference to physical activity in the last two days.
Symptoms of unstable angina
- pain in the heart or chest of a compressive nature;
- pain in other parts of the body (arms, stomach, teeth, shoulder blades, lower back);
- feeling of lack of air;
- secretion of a large amount of sweat;
- cardiopalmus;
- anxious thoughts;
- dizziness;
- weakness;
- nausea;
- a sharp increase or decrease in pressure.
The following signs help to distinguish the unstable and therefore most dangerous form of pathology:
- The symptoms began to progress, the condition during an attack became more difficult to bear, the pain spread to neighboring areas (left arm, neck, back, jaw).
- Acute angiotic manifestations (compression, heat, heaviness in the chest) or suffocation are occurring more and more often.
- For an attack to occur, a much lower level of stress is required; angina pectoris occurs even in a calm state.
- Signs of acute ischemia were discovered after surgery for coronary artery bypass grafting, less than three months before the visit to the doctor.
- Nitroglycerin does not relieve pain well.
- The paroxysm lasts longer than 15 minutes.
- Prinzmetal's angina occurs mainly in young men, regardless of the influence of physical activity. Between attacks, the patient can withstand significant muscle tension without consequences. Heart pain often occurs in the morning. They are caused by spasms of the coronary arteries, which are not always susceptible to atherosclerotic changes. The pathology progresses rapidly and creates a high risk of developing myocardial infarction.
Treatment
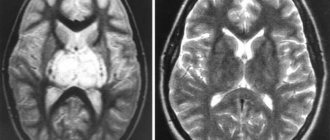
The basis for making a diagnosis is the patient’s complaints about the progression of angina attacks, medical history data and the results of examination using various instrumental and laboratory methods:
- drawing up an ECG protocol based on daily Holter monitoring;
- performing scintigraphy;
- echocardiography (regular and under load);
- coronary angiography method;
- analyzes of biological fluids.
Classification
Unstable angina is usually divided into 4 groups.
- Primary. The disease is considered to be in an unstable phase within 30 days after the first attack.
- Post-infarction, when attacks appear within 2 days after a heart attack or in the acute period.
- Progressive. There is a deterioration in the condition, and the time between pain syndromes is reduced within the last month.
- Prinzmetal's angina. This group of diseases is characterized by pathogenesis with a precise indication of spasmodic narrowing of the cardiac arteries, and not atherosclerotic.
The angina described by Prinzmetal is included in the current classification of unstable angina. It has the following clinical picture:
- pain occurs during rest, deviations are visible on the ECG;
- During physical exertion, patients do not feel pain and cope well with the load;
- painful feelings develop in the morning;
- Nitrate drugs and the drug group of calcium antagonists show good results in relieving pain;
- In most situations, pain appears in men at a young age.
Unstable angina and its classification are interconnected with various factors - the possibility of developing into an acute form of heart attack, frequent manifestations of severe pain, and physical or psycho-emotional tension.
Depending on the level of severity and duration, angina pectoris can be:
- first degree. Heart attacks last no more than 2 months, do not appear in a calm position, but painful attacks are severe and progress;
- second degree. Angina attacks at rest have been observed during the last month, but not in the last two days;
- third degree. Attacks of pain at rest appeared over the next two days.
Unstable angina, according to the Braunwald classification, is determined by the clinical manifestation of pain and its causes in relation to the risk of its development into an acute infarction.
According to Braunwald, angina is divided into three classes of the disease, and the signs of the disease are distributed in groups A, B, C:
- The first class is characterized by common angina pectoris under significant stress. Painful attacks appear with significantly less stress than noted before, pain appears more often, such situations were initially noted during the last two months. During a calm state, pain does not bother me for two months.
- The second class includes the chronic type of angina during the rest period, or a form of the disease that occurred within the range from 2 days to 30 days.
- The third class is characterized by an acute form of this heart disease in a calm position, which developed over the next two days.
Division into circumstantial manifestations:
- A (called secondary) - when the pain syndrome is caused by diseases that are not related to cardiac activity, for example, anemia, acute infectious diseases, thyrotoxicosis;
- B (called primary) - directly associated with heart ailments;
- C – appears within the first 14 days after a heart attack.
Unstable angina according to Braunwald is diagnosed as class 2 A. That is, painful attacks appear in a quiet position, last for two months, and the patient has a history of other concomitant diseases that contribute to the development of spasm in the cardiac arteries.
The table clearly shows the classification of unstable angina according to Braunwald.
Stable is considered the most favorable for the patient and, subject to medical recommendations, allows you to avoid dangerous complications for a long time.
What is the difference between stable and unstable angina? To answer this question, it is necessary to compare how both forms of the disease manifest themselves.
The classification of unstable angina is associated with the determination of the likely development of an acute infarction, the dependence and frequency of painful attacks, and physical and emotional stress.
According to severity and duration, they are distinguished:
- first degree - the onset of the disease less than two months ago, develops at rest, the course is severe and progressive;
- second degree (subacute course) - the disease lasts more than two days, before this time no attacks were observed;
- the third (acute form) - developed only in the last two days.
According to the severity of clinical manifestations
Treatment recommendations
In the treatment of NSS, a special standard has been developed to normalize the patient’s condition. Please take into account the fact that treatment takes place only in a hospital setting. After completing the therapeutic course, the patient is sent for further rehabilitation at home with mandatory compliance with a list of strict rules and restrictions.
The standard of care for SUDs has several goals:
- restoration of the quality of coronary patency;
- stabilization of symptoms and elimination of pain;
- prevention of acute heart attack and death;
- ensuring the possibility of recovery and adaptation to life.
To combat the primary symptoms, until qualified assistance is provided, you can take no more than 2 tablets of Nitroglycerin . Another useful tip is to take 2 Aspirin tablets, which thins the blood and provides protection against possible thrombosis.
When a patient is admitted to the hospital and admitted to the hospital, he should:
- adhere to bed rest with gradual easing of restrictions as health is restored;
- eat often, healthy foods, but in small portions, so as not to overload the digestive and cardiovascular systems;
- take all medications as prescribed;
- undergo procedures prescribed by the attending physician.
Treatment tactics largely depend on what complications appear and how the patient feels. The sooner a patient can be hospitalized, the less risk there is to his health and life.
Drug therapy
For unstable angina of the heart, medications of different groups are used. The drugs are prescribed in a complex manner.
- In acute conditions, nitro-containing agents must be administered intravenously.
- When the exacerbation passes, the dosage of Nitroglycerin or its analogues for oral administration is selected individually.
- The patient is prescribed anticoagulant medications. They are aimed at reducing blood clotting and protecting against thrombosis.
- At the same time, aspirin-containing medications are used to prevent stomach damage.
- Adrenergic blockers are needed by almost all patients with unstable angina. An exception is the diagnosis of Prinzmetal's angina. Such drugs should not be used if the patient has chronic bronchitis or bronchial asthma.
- If the diagnosis does not show significant vascular damage, then calcium channel antagonists are added to the complex drug treatment.
- Medicines required for symptomatic treatment are prescribed on a temporary basis. Their list directly depends on the problems, diseases and complications that occur in parallel with unstable angina of the heart.
The standard of treatment is selected taking into account individual characteristics. A thorough diagnosis is required to choose the best option for influencing the heart muscle and associated diseases.
Complications
Complications due to unstable angina occur when adequate treatment is not carried out, the standard is violated, or the patient simply does not adhere to the rules and recommendations of the doctor. If you do not deal with the problem of SUD, this can lead to:
- sudden ventricular fibrillation followed by death;
- acute attacks of myocardial infarction;
- acute heart failure;
- pulmonary edema;
- pulmonary thromboembolism.
Therefore, if, against the background of IHD, attacks begin to become more frequent and uncharacteristic symptoms appear, you should definitely seek help and undergo a full course of treatment. Refusal to hospitalize and ignoring the doctor’s recommendations shifts all responsibility for life onto the patient himself. It is better to trust qualified specialists and receive timely and adequate assistance.
Thanks everyone for your attention! Be healthy and do not self-medicate! Subscribe to our website, leave comments, ask questions, invite your friends to join us and be sure to come back!
Classification of degrees of pathology
Severity of the disease:
- first degree development of manifestations of an anginal attack against the background of complete calm;
- second degree of unstable angina, symptoms appear with moderate physical activity, the interictal period is shortened in duration;
- The third degree of the disease is characterized by a rare recurrence of an anginal attack, which is provoked by significant physical exertion.
Classification of the disease depending on provoking factors and concomitant pathologies:
- group A, the development of anginal attacks is provoked under the influence of diseases not related to heart pathology, for example, endocrine diseases, anemia or infectious lesions;
- group B develops an attack against the background of organic pathologies in the heart wall;
- group C post-infarction causes of the disease.
Classification of angina: according to WHO, according to Braunwald and others
Angina pain (angina pectoris) is a pathology that is a variant of ischemic heart disease (CHD), and is manifested by cardiac attacks that occur against the background of oxygen starvation of the myocardium.
If pain is initiated by physical activity, then doctors talk about angina pectoris. In cases where chest pain develops during sleep or during rest, we are talking about a pathology of rest.
In addition, there is also stable and unstable angina.
Currently, a variety of classifications are used to fully characterize angina.
In their practice, cardiologists prefer to use its classic versions, which have the only standard around the globe.
Features of the classification of the stable form of the disease
Stable angina pain is a type of disease when pain in the chest occurs during the period of exposure to physical loads on the body and tends to fade after they are removed. The classification of stable angina is based on the principle of identifying functional classes of the disease, depending on the nature of the physical activity provided.
The following functional classes of angina are distinguished:
- FC I – attacks rarely develop under significant physical stress;
- FC II - chest pain occurs when moving quickly over a distance exceeding 300 meters, or after climbing stairs to the height of the second and subsequent floors (the second functional class of angina is assigned to patients in whom attacks develop against the background of stress, smoking or have meteorological dependence );
- FC III - attacks appear if the patient climbed to the first floor or walked a distance of 100-300 meters at a fast pace;
- FC IV - angina pain occurs with minimal physical activity or in a calm state.
To assess the condition of patients with this type of disease, four degrees of angina are distinguished:
- Latent or angina manifestations of the first degree - a person’s habitual activity and lifestyle do not provoke the development of an attack;
- Grade 2 or mild angina – there is minimal limitation of usual physical activity;
- Moderate severity (grade 3 angina) – characterized by a noticeable limitation of motor activity due to the risk of developing cardialgia syndrome;
- Severe or stage 4 angina pectoris - attacks of angina pain occur with any physical activity.
The main forms of unstable angina pectoris
Unstable angina is a variant of the development of coronary heart disease, which in practice manifests itself as intense, pressing pain in the pericardial region, which can independently regress or transform into more complex forms of coronary artery disease - myocardial infarction, sudden death of coronary origin.
According to the modern classification, it is customary to distinguish the following types of unstable angina:
This form of the disease is characterized by the duration of the onset of the first cardialgic manifestation, which is no more than one to two months. The disease is often complicated by such an acute form of coronary artery disease as myocardial infarction. In a number of clinical cases, unstable angina, which occurs for the first time, can transform into a stable form of the disease.
This type of disease is characterized by a particular intensity of pain, an increase in the frequency of attacks and their duration, as well as the appearance of characteristic changes in the electrocardiogram that have not previously been recorded.
- Early post-infarction angina pain
It is characterized by the appearance of pain symptoms from 1 to 28 days after myocardial infarction.
This type of disease is known as vasospastic.
The pathology is extremely rare and is manifested by the development of angina attacks in a state of absolute rest (usually during sleep) without any contributing factors.
Typical signs of Prinzmetal's angina
Unstable angina has several common symptoms with the stable form of this disease. Among them are:
- pain in the chest area, maybe a little to the left, the patient feels as a squeezing, pressing, less often burning pain, which radiates to the left half of the body (arm, bottom of the shoulder blade, jaw);
New York cardiologist M. Prinzmetal described a type of angina pectoris in 1959, which is included in the modern classification of unstable forms of angina pectoris. In pathogenesis, great importance is attached to the increased tone of the vagus nerve.
Possible complications
In difficult cases, the following complications develop:
- Myocardial infarction. Serious circulatory disorders lead to the death of heart muscle cells.
- Heart rhythm disturbances: acceleration, deceleration, the appearance of extraordinary contractions.
- Changes in the myocardium lead to heart failure. In this case, the heart does not contract enough and therefore cannot provide proper blood circulation. This condition is dangerous as it can be fatal.
- The risk of sudden death increases. It is difficult to closely monitor the patient's condition, so there may be a gradual or rapid deterioration in health, resulting in a serious risk of irreversible changes.
Unstable angina can develop myocardial infarction.
The above complications are the most serious, so they must be taken into account when prognosis of the disease.
What symptoms and signs are used to determine unstable angina?
The main symptom of angina is pain in the heart or chest. Patients note a pressing or squeezing nature of pain that radiates to the shoulder blade, neck, jaw, and left arm. Pain in the right arm and upper abdomen is less commonly reported.
A painful attack causes the patient to groan and experience a feeling of fear of death. Externally, the condition manifests itself in pale skin, increased blood pressure, numbness of the limbs and rapid heartbeat. During an atypical attack, the following symptoms are observed:
- dyspnea;
- pain in the arms, neck, or teeth;
- tachycardia;
- sweating;
- general weakness;
- nausea.
Rarely, attacks are not accompanied by specific manifestations; this phenomenon is called “silent” angina.
As a rule, attacks appear suddenly at the peak of nervous or physical stress. Due to pain and other symptoms, the patient is forced to stop for 10-15 minutes to recover.
The duration of attacks is no more than 15 minutes, after which the pain disappears on its own or after taking Nitroglycerin. The drug dilates the blood vessels of the heart, ensuring the supply of sufficient oxygen to the myocardium.
After the end of the attack, the disease does not manifest itself, the patient returns to his usual lifestyle.
Features of the disease
In order for all parts of the heart to receive sufficient nutrition, a constant flow of blood through the arteries is required. A person's myocardial oxygen demand may change. This depends on physical activity, illness, state of rest, etc. If the heart muscle is not at rest, tachycardia occurs, that is, the number of heart contractions increases. Therefore, there is a need for more energy, which the muscle receives due to the influx of more blood.
With normal patency of the coronary arteries, through which the myocardium receives nutrition, blood passes in normal, sufficient quantities. But the narrowing of one or more arteries leads to oxygen starvation and hypoxia processes with all the ensuing consequences. Angina is divided into stable and unstable. In the first case, diagnosis is simplified due to clear and understandable symptoms. Stable angina is characterized by:
- typical duration of pain;
- characteristic repeatability;
- dependence on strong anxiety, physical activity, etc.
Such angina can be easily eliminated by simply taking a Nitroglycerin tablet. But with unstable angina, the symptoms are somewhat different, and its treatment becomes more complicated, since there is no clear relationship between the physical condition and the work of the heart. The pain continues for a long time, and it is almost impossible to say when the attack will recur. Therapy becomes problematic because it is difficult to determine optimal restrictions in terms of physical activity.
The main danger of unstable angina is the risk of any next attack turning into an acute infarction, that is, the patient is in a pre-infarction state. In order to start treating a heart problem in time and prevent possible consequences, you should know about the causes and symptoms of the development of such a disease, which occurs against the background of coronary artery disease.
Causes
The causes of unstable angina pectoris include the same factors that are characteristic of coronary artery disease. Namely:
- coronary vessels are affected by atherosclerosis and narrow by 50%;
- Thrombosis of the heart vessels occurs due to increased coagulability, decreased blood flow speed, and thromboembolism of various parts.
There are additional risk factors that increase the likelihood of developing NCC. These include:
- age over 45 years;
- hypertension;
- diabetes;
- alcohol abuse;
- tobacco addiction.
Experts believe that due to thrombosis, the manifestation of unstable narrowing of the lumens in the vessels increases.
Symptoms
It is important to be able to differentiate between stable and unstable angina. Let's start with the general symptoms that allow us to recognize NSS:
- pain occurs in the area of the myocardial muscle;
- the pain can be pressing and squeezing, radiating to the shoulder blade, throat, left upper limb;
- pain syndromes are of high intensity;
- the person begins to sweat profusely;
- there is a feeling of fear of death;
- dizziness appears;
- suffocation may appear, but as a subjective symptom;
- breathing does not become faster.
In rare cases, pain may be felt in the patient's chest area, between the shoulder blades, or move to the abdomen. Some patients experienced girdling pain. To provide medical care, the doctor must understand what type of angina he is experiencing.
To distinguish between stable and unstable angina, there are certain features that help differentiate the diseases. In case of unstable form of cardiac angina:
- recurrence of attacks occurs more often;
- the attack lasts more than 15 minutes;
- pain is more intense and stronger;
- during physical activity it is not possible to provoke pain;
- discomfort is equally intense during exercise and at complete rest;
- Taking Nitroglycerin only temporarily improves your well-being or may not help at all.
To eliminate unpleasant symptoms and relieve pain, some patients have to take an increased dose of Nitroglycerin. Otherwise, relief will not come.
Diagnostic methods
To diagnose the disease, the patient is initially interviewed and all existing complaints about his health condition are clarified. Establish the relationship between attacks and the presence of other symptoms and causes.
Next, an electrocardiogram is prescribed, which is supplemented with daily ECG monitoring. Laboratory tests are also used for diagnosis - a general blood test, which shows the number of leukocytes.
Ultrasound examination determines where the areas with reduced myocardial contractility and cardiac output indicators are located.
To determine the level of narrowing of the heart arteries, an angiogram is used when a contrast agent is injected into the vessels.
If signs of ischemia can be detected on the ECG during an attack, and sometimes 2–3 days after the pain has disappeared, then it is impossible to determine whether it is stable or unstable angina pectoris only on the basis of this type of examination.
For the purpose of accurate diagnosis, the following is carried out:
- taking anamnesis;
- ECG monitoring;
- Ultrasound and Dopplerography;
- general and biochemical blood tests;
- angiography.
History taking
Diagnostic methods
The presence of IHD in a person indicates the need to carefully monitor one’s health and promptly respond to attacks that occur. To begin adequate and timely treatment of unstable angina, you should seek help from specialists and undergo a comprehensive diagnosis. When characteristic symptoms appear, the doctor collects an anamnesis, finds out the causes and circumstances of pain attacks and other signs. Basically, NSS is checked using an ECG. An electrocardiogram can provide information about the current state of the heart muscle and the behavior of the myocardium.
If treatment takes place in a hospital, doctors use the Holter monitoring method. To do this, a special device is connected to the patient, which reads the data on the ECG during the day, after which the changes in the cardiogram are assessed. To clarify treatment tactics, the results of laboratory tests are attached to the cardiogram. To do this, you should donate blood samples for general and biochemical analysis. Ultrasound examination is needed to view myocardial contractions and diagnose decreased cardiac output.
To check the state of patency of the coronary vessels, an angiogram method is used by introducing a special contract composition. A diagnostic set of measures, which includes electrocardiographic, ultrasound and laboratory research methods, is necessary to confirm the diagnosis of unstable angina of the heart and select the optimal treatment tactics.
Treatment
The main goal in the treatment of angina is to prevent progression and sudden death. Can be conservative or surgical.
- Non-drug treatment:
- emergency hospitalization;
- strict bed rest, refusal of physical activity.
- Drug therapy:
- cupping involves the use of nitrates. Neuroleptanalgesia, a method of intravenous pain relief, is also possible;
- medications, including beta blockers, statins and calcium antagonists;
- blood thinners, including antiplatelet agents and direct anticoagulants.
- Surgery:
- coronary angioplasty with stenting;
- coronary artery bypass grafting.
https://www.youtube.com/watch?v=o3hUW9ZZOss
Development mechanism
The development of the pathological process begins with the consumption of foods rich in fatty components, which cannot be sufficiently absorbed in the body. The residual amount of lipids, circulating through the arteries along with the blood flow, settles in the vessel wall. First, so-called grease spots and streaks form. Next, an atherosclerotic plaque is formed, which does not make itself felt for a long time. Eventually, the covering, the membrane of the plaque that protects the formation from the blood flow, breaks through and ulcerates. A blood clot forms in its place.
The thrombus grows quite quickly and closes the lumen of the vessel. A sufficient amount of oxygen and nutrients does not reach the cardiomyocytes; they give a signal to neighboring nerve endings that they are in a state of hunger and hypoxia. The pain syndrome breaks down, which is a bell indicating a serious problem has arisen.
Diagnostics
Management of patients with coronary insufficiency (a particular type is unstable angina) is the task of a specialized doctor.
If there is suspicion, it makes sense to hospitalize the person for a short time; this is the most correct decision, because the patient’s life is at stake. The next episode could be the last.
Scheme of events:
- Oral interview with the patient. The complaints are typical, which allows us to draw conclusions almost immediately.
- Anamnesis collection. Data for organic pathologies is also on the surface. This is the path to identifying the origin of a process.
- Measurement of blood pressure, heart rate.
- Listening to heart sounds. The tones are dull and irregular. Violations worsen the prognosis.
- Daily monitoring using an automatic Holter device.
- Electrocardiography. Specific functional signs on the ECG include widening of the QRS complex, premature appearance of the P wave, doming of the ST segment, and many others. The interpretation is carried out by a cardiologist and diagnostic specialist. Errors may occur.
- Echocardiography. To determine organic changes and defects.
- MRI or CT.
- Angiography of the coronary arteries.
This is enough for the system. It is possible to involve third-party specialists as part of advanced diagnostics if there is no evidence of cardiac sources of the problem.
Description of the disease
As already noted, the cause of coronary artery disease and angina pectoris can be problems with blood vessels. With the accumulation of lipids in the body, cholesterol is deposited on the vascular walls. The worst thing for your health is atherosclerotic deposits in the coronary vessels, which causes myocardial hypoxia. In a situation where a lack of oxygen interferes with the normal course of metabolism, quite noticeable physical activity or nervous excitement causes a painful sensation in the chest. Sometimes the pain can be transferred to the area between the shoulder blades, left shoulder or neck.
For stable angina, it is enough to follow the regimen, taking appropriate medications, and avoiding physical and psychological stress. However, the unstable form of the disease is difficult to predict and preventive therapy. A sudden complication with a fairly high probability can cause myocardial infarction. Therefore, acute attacks with NS require immediate medical attention, placing the patient in a hospital with constant supervision by a specialist.
Therapy tactics
Let us note once again: since angina pectoris is an extremely dangerous complication, patients are subject to urgent hospitalization. Simultaneously with the therapy, the dynamics of the patient’s condition are monitored using ECG and other diagnostic methods.
Treatment is aimed at relieving pain. Preventive measures are taken against recurrent attacks and the occurrence of MI. In general, treatment tactics depend on the etiology and pathogenesis of NS.
Considering the atherosclerotic path of development of the disease, treatment at the initial stage is carried out with acetylsalicylic acid. Taking aspirin tablets slows down the synthesis of cyclooxygenase, which interrupts the processes of inflammation and thrombus formation. The initial dose of the drug is 325 mg. As a rule, the therapeutic effect is noticeable after 15 minutes. Subsequently, the daily dosage is reduced to 160 mg. The tablets should be taken with plenty of water. According to doctors' observations, in comparison with the placebo effect, aspirin therapy significantly reduces the risk of myocardial infarction. To prevent the negative effect of this drug on the gastric mucosa, its modern forms with a coating that dissolves in the intestine should be used.
Nitroglycerin is used to relieve pain in the heart area. 1 tablet (0.5 mg) is placed under the tongue. If necessary, you can take another one after 10-15 minutes. In the absence of the desired effect, general anesthesia with neuroleptics or analgesics is performed. Infusion therapy is also carried out using solutions of heparin and nitroglycerin.
β-blockers have a significant effect in NS. As a result of their use, ischemia of the heart muscle is eliminated, erosive and atherosclerotic processes in blood vessels are stopped, and normal hemodynamics are restored.
A reliable therapeutic effect is provided by a combination of aspirin, heparin and adrenergic blockers. This treatment is used especially if angina is complicated by hypertension, arrhythmia, tachycardia and hyperactivity of the sympathetic nervous system.
Symptoms
Anyone with a history of coronary artery disease should suspect unstable angina if their angina begins to occur at lower levels of exercise than usual, if it occurs at rest, if it persists longer than usual, if it is more difficult to relieve with nitroglycerin, or especially if it wakes them up at night.
People without any history of coronary artery disease may also develop unstable angina. Unfortunately, these people have an increased risk of heart attack because, unfortunately, they often do not recognize the symptoms as angina.
Classic symptoms of angina include pressure or pain in the chest, sometimes tight or “heavy” in nature, often radiating to the jaw or left arm. Unfortunately, many patients with angina do not have the classic symptoms. Their discomfort may be very mild and localized to the back, stomach, shoulders, or one or both arms. Nausea, shortness of breath, or just a feeling of heartburn may be the only symptom. Essentially, this means that anyone middle-aged or older, especially anyone with one or more risk factors for CAD, should be alert to symptoms that may represent angina.
If you think you may have unstable angina, you should contact your doctor or emergency room immediately.