Where does bilirubin come from?
The transport iron-containing protein of the blood - hemoglobin, being an integral part of red blood cells, binds to oxygen and ensures its delivery to all organs and tissues of the body.
Since the blood is constantly renewed by replacing old, damaged red blood cells and other blood elements with new ones, this process is accompanied by the formation of a huge number of by-products.
Such as:
- Pigments;
- Slakov;
- Toxins.
In a high and not very high degree of danger to the body.
Bilirubin is one of these elements of the breakdown of used red blood cells and is a hemoglobinogenic pigment.
A high percentage of bilirubin is produced by decaying red blood cells - 85%, the remaining 15% is formed during the utilization of myoglobin and cytochromes.
In the human body, the spleen, bone marrow and the main detoxification laboratory of our body, the liver, are responsible for the renewal of blood elements.
It is in the liver that the synthesis of proteins, including hemoglobin, occurs, accompanied by the largest formation of wastes and toxins, which are bound by liver enzymes and, neutralized, are eliminated from the body naturally.
The decay process occurs continuously - within a day, approximately one hundredth of all red blood cells are destroyed, forming in adults about 300 mg of bilirubin, which we detect in the blood during tests.
If its content is too high, this indicates various disorders of hemoglobin synthesis or excretion.
The main symptom of such disorders is:
- The appearance of a icteric color of the eye sclera;
- Yellowness of the skin.
Correct diagnosis of bilirubin metabolism disorders does not present any difficulties, since modern science has studied and described them in sufficient detail.
Norm of bilirubin
When deciphering the tests, it should be borne in mind that bilirubin comes in three types:
- Indirect or toxic, formed during the breakdown of hemoglobin elements in the blood. It is also called free, unbound or unconjugated. It should be contained in the blood of a healthy person no more than 16.2 µmol/l.
- Direct (bound, conjugated), which is the product of the binding of indirect bilirubin with glucuronic acid. This bilirubin is no longer toxic, since the body neutralizes it with the help of liver enzymes and removes it as part of bile. Normal level of direct bilirubin: 0-5.1 µmol/l.
- Total bilirubin, the normal value of which should be in the range of 0.5 – 20.6 µmol/l
Visible symptoms of hyperbilirubinemia (high bilirubin levels) usually appear at values greater than 34 µmol per liter in serum, but it can be increased several times.
A situation where bad bilirubin fluctuates and is significantly overestimated in tests requires immediate medical attention, as it poses a threat to life.
Bilirubin norms in the table
| Direct mmol/l | Indirect mmol/l | Total mmol/l | |
| In newborns | 8.7 | 14 | 23.1 |
| In a teenager | 8.5 | 10.3 | 13.7 |
| In men and women | 1,7-5,1 | 3,4-16,2 | 5,1-20,6 |
Treatment with folk remedies
To reduce bilirubin, you can use folk remedies that are easy to use at home.
Traditional medicine:
- Infusion of mint and chamomile . To prepare the infusion you will need dried herbal flowers. They are combined in equal proportions and filled with boiling water. For 4 tablespoons of the mixture take 400 milliliters of water. The drink is consumed 100 milliliters twice a day: in the morning and before bed.
- An infusion based on motherwort and St. John's wort . For cooking, herbs are taken in equal quantities. For 50 grams of mixture you will need 500 milliliters of hot water. The drink is infused for 1 hour. It is recommended to consume it twice a day, 100 milliliters.
- Beetroot juice . Beetroot juice is consumed before each meal.
- Milk thistle infusion . Pour 50 grams of milk thistle seeds into a liter of boiling water and simmer for 30 minutes over low heat. The infusion is taken one teaspoon six times a day.
Useful video
Share this post
- Related Posts
- Feet are constantly cold: reasons for women and men
- What to do if the nail on the big toe comes off in children and adults
- What belongs to protein foods: list of products
- What to do in case of sunstroke: signs and first aid for a child and an adult
- How to monitor and care for dental and oral health: basic rules
- Symptoms and signs of beer alcoholism in men and women
Metabolism of bilirubin: main stages
Newly formed bilirubin is a water-insoluble compound that is quite toxic to the body.
Then it goes through the following stages of transformation:
- It interacts with albumin, a blood protein, which, by binding to it, transfers it to the liver through the bloodstream. Albumin also performs a neutralizing function, preventing bilirubin from poisoning the blood. Since the protein-bilirubin complex is quite large, it does not penetrate the kidney filters and is not excreted in the urine.
- Bilirubin in the liver is separated from albumin, penetrates the liver tissue and is transported further along the liver membranes.
- To be excreted from the body, bilirubin must become soluble in water so that it can be evacuated with bile. For this purpose, it binds to glucuronic acid in the liver, resulting in the formation of bilirubin diglucuronide, a soluble compound.
- The final stage is the excretion of bilirubin with bile. Bile is a kind of tightly packed container of toxins - everything that is thrown out by the body accumulates in it. Capturing cholesterol and bilirubin fractions, bile enters the intestine, where it breaks down into its components. Bilirubin fragments are converted here into urobilinogens, which are excreted in the feces. Part of the bilirubin penetrates the intestinal walls and, entering the blood again, is subsequently filtered by the kidneys and excreted in the urine.
Types of bilirubin
Bilirubin in the body is presented in the form of several fractions:
- Indirect fraction, which is bile pigment. It is insoluble in water and can penetrate the cell membrane. The main toxic effect is associated with this. This fraction of bilirubin is synthesized in the cells of the reticuloendothelial system through the enzymatic transformation of heme, which is formed during the breakdown of hemoglobin. Next, it binds to carrier proteins, most often albumin, and penetrates the liver.
- The direct fraction (free) is formed in liver cells by combining with glucuronic acid. Thanks to this reaction, the pigment acquires water-soluble properties and, together with bile, enters the duodenum. In the gastrointestinal tract, bilirubin undergoes further changes. A small part of it is reabsorbed into the blood, and then filtered in the kidneys and excreted in the urine. Basically, it ultimately turns into stercobilin, which is found in feces and provides its characteristic color.
Some patients do not quite understand what total bilirubin is in a blood test. This value is obtained by adding the concentration of the direct and indirect fractions.
How to suspect that you have bilirubinemia?
The organ responsible for the exchange of bilirubin in the body is the liver. Therefore, it is she who reacts with a symptom peculiar to her - the abundant formation of icteric pigment, indicating a malfunction of the organ.
Appearing jaundice indicates the following disorders:
- Too much bilirubin is produced, which indicates the possibility of anemia due to the excessive breakdown of red blood cells and a high level of unconjugated bilirubin in the blood;
- There is a violation of the outflow of bile for some reason, which causes an increase in the concentration of bilirubin in the body;
- Increased formation of bilirubin in the reticuloendothelial system;
- Metabolic disorder of the hepato-biliary system.
Sometimes the degree of coloration with yellow pigment does not correspond to the analysis indicators.
This occurs due to the individual characteristics of the body - the presence of obesity or severe edema can neutralize high pigmentation, and an ascetic physique enhances it.
The increasing intensity of symptoms of hyperbilirubinemia manifests itself in the following order:
- The sclera of the eyes turn yellow;
- A yellow color appears in the oral mucosa;
- The face, soles, and inside of the hands are painted;
- The entire surface of the body is pigmented;
- With increased bilirubin, the state of health is depressed, performance and general tone are reduced.
It should be borne in mind that yellowness can also appear when:
- Abundant consumption of foods high in carotene (tomatoes, carrots);
- Diabetes mellitus;
- Hypothyroidism.
Unlike hyperbilirubinemia, in these cases the sclera of the eyes remains of a normal color.
Diseases accompanied by high bilirubin
The increase in direct and indirect bilirubin varies in different pathologies.
A high level of direct bilirubin may indicate the presence of the following diseases:
- Chronic hepatitis C;
- Autoimmune hepatitis;
- Acute viral hepatitis;
- Poisoning by toxic compounds, both food and chemical;
- Cirrhosis;
- Malignant and benign neoplasms in the liver;
- Jaundice of pregnancy;
- Hereditary jaundice.
High indirect bilirubin may indicate:
- Congenital hemolytic anemia;
- Infectious diseases (malaria, typhoid fever, sepsis);
- Drug-induced hemolytic anemias;
- Toxic anemia resulting from poisoning;
- Lucy-Driscoll, Crigler-Najjar, Gilbert syndromes;
- Autoimmune hemolytic anemia, developing against the background of rheumatoid arthritis, lupus erythematosus, lymphocytic leukemia, etc.
What to do with high bilirubin?
To reduce the concentration of liver enzyme, it is necessary to identify and eliminate the underlying disease that caused the increase in levels. Therapy uses an integrated approach - drug treatment, diet, physiotherapeutic methods.
Phototherapy is prescribed to stabilize bilirubin levels and is safe even for the smallest
Bilirubin is higher than normal - how to treat:
- Infusion therapy – special solutions are administered intravenously to relieve symptoms of intoxication and cleanse the body.
- Phototherapy is irradiation with blue lamps, which accelerates the process of converting indirect bilirubin into direct bilirubin; the method is safe even for small children.
- Prescribing medications to eliminate signs of the underlying disease.
- Nutrition correction.
With a slight increase in indicators, treatment can be carried out at home, severe forms are treated in a hospital.
Drug treatment
If bilirubin is elevated, various drugs are used for correction, the action of which is aimed at eliminating unpleasant symptoms and restoring the liver.
Hepatoprotector Karsil is prescribed to restore normal levels of bilirubin in the blood
What drugs are prescribed for increased bilirubin:
- hepatoprotectors – Karsil, Essentiale forte;
- medicines based on ursodeoxycholic acid - Ursosan, Urdoxa, eliminate inflammatory processes, dilute bile, promote its better outflow;
- antiviral agents - long-acting interferons, Ribaverin;
- immunomodulators – Taktivin, Timalin;
- antibiotics – Neomycin, Vancomycin;
- choleretic drugs – Allahol, Holagol;
- enzymes – Panzinorm, Festal;
- enterosorbents – Enterosgel;
- glucocorticosteroids - Prednisolone, prescribed for high levels of direct bilirubin;
- Phenobarbital - prescribed for Gilbert's syndrome and some other serious liver pathologies.
Increased bilirubin in the blood: causes
Increased levels of bilirubin in the blood are a consequence of one of three main factors:
- Dysfunction of bile outflow from the liver.
- Intensive destruction of blood cells.
- Disorders of bilirubin metabolism (problems with its binding and removal from the body).
Let's look at these factors in more detail.
Outflow dysfunction
With this disorder, bound bilirubin returns back into the blood and accumulates in it, causing high direct bilirubin levels.
In this case, the causes of jaundice are:
- Bile ducts blocked by stones, tumors, parasites;
- Compression of the bile ducts by external causes - enlarged lymph nodes, incorrect position of organs, etc.;
- Inflammatory process of the bile ducts, leading to their hardening and narrowing;
- Anomalies of the biliary tract.
With outflow dysfunction, the following signs of hyperbilirubinemia appear:
- Intense yellow pigmentation of the skin;
- Severe skin itching;
- Light, almost white color of stool;
- Dark colored urine;
- High levels of conjugated (direct) bilirubin;
- Paroxysmal pain in the right hypochondrium;
- Problems from the gastrointestinal tract - nausea, constipation, diarrhea, bitter belching.
Accelerated destruction of red blood cells
High levels of indirect bilirubin with symptoms of jaundice are explained by the intensive breakdown of red blood cells.
The reasons for this may be:
- Extensive hemorrhages due to injuries, pulmonary infarctions;
- Transfusions of blood incompatible by Rh factor or group affiliation,
- Infectious diseases (typhoid fever, sepsis, malaria);
- Poisoning by poisons;
- Malignant tumors of the hematopoietic organs.
The symptoms of this hemolytic jaundice are expressed by:
- Pale skin due to anemia;
- Coloring the mucous membranes and skin lemon-yellow;
- Pain in the spleen area (left hypochondrium);
- Possible increase in body temperature;
- Dark color of urine and feces due to the presence of stercobilin and urobilin compounds in them;
- Symptoms of oxygen starvation of tissues (headaches, fatigue, palpitations).
Bilirubin metabolism disorders
Disturbances in the metabolism of bilirubin are accompanied by its accumulation in the tissues of the body, which affects the functioning of organs and systems and is again manifested by jaundice.
These pathologies may have:
- Hereditary causes.
- Acquired during life.
Hereditary jaundice
They arise due to improper processes of binding, transport and removal of bilirubin from the liver, caused by congenital anomalies.
The reasons for this are:
- Lucy-Driscoll syndrome;
- Gilbert's syndrome;
- Dubin-Johnson syndrome.
The most common of them is Gilbert's syndrome.
With this disease, there is a deficiency of the liver enzyme, which is responsible for the binding of bilirubin to glucuronic acid, therefore there is a high content of unbound fractions in the blood serum.
This genetic defect can also be asymptomatic, in which bilirubin rises slightly, manifesting as jaundice occasionally during stress, excessive exercise, or alcohol.
The nature of the disease is benign, with a favorable prognosis; specific treatment is not provided.
Acquired jaundice
Divided into 2 types:
- Prehepatic jaundice, in which there is too much bilirubin produced and the liver does not have time to bind it for excretion.
- Hepatic, or parenchymal jaundice, in which there is damage to the bile capillaries and liver parenchyma, resulting in impaired uptake and binding of bilirubin entering the liver, which leads to high levels of direct bilirubin in the serum.
These types of hyperbilirubinemia are caused by:
- Hepatitis (drug, alcohol, autoimmune).
- Liver cirrhosis.
Hepatitis is characterized by:
- General weakness;
- Jaundice staining of mucous membranes and skin;
- Pain in the right hypochondrium;
- General intoxication (increased body temperature);
- Joint and muscle pain;
- Changes in the color of stool and urine.
Hepatitis can occur in acute and chronic forms.
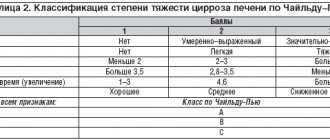
Cirrhosis
It represents changes in the structure of the liver due to the death of the main liver cells - hepatocytes.
Because of this, the liver lobules decrease and disappear, the hepatic capillaries and vessels are distorted, dead cells are replaced by connective tissue, which leads to the loss of the functional ability of the entire organ.
The most common cause of adult liver cirrhosis is alcoholism.
Symptoms of liver cirrhosis:
- Skin itching;
- Enlarged liver and spleen;
- Dilation of the veins of the esophagus, intestines;
- Yellowness of the skin;
- Accumulation of fluid in the peritoneum.
Symptoms and manifestations of high bilirubin in the blood
Increased bilirubin has specific symptoms: yellowness of the skin and mucous membranes, dyspepsia, bitter taste in the mouth, constant nausea, gray coating on the tongue, cephalgia, vertigo, itchy skin, chronic fatigue syndrome, discolored feces and dark urine, discomfort in the right hypochondrium due to enlarged liver. In cases of viral etiology of hepatitis, there may be a high temperature. Laboratory indicators only confirm the clinical diagnosis.
Methods for reducing bilirubin
Modern medicine has effective methods for controlling bilirubin metabolism. This area of medicine has been thoroughly researched and therapeutic agents are constantly being improved.
Methods for normalizing bilirubin levels in each specific case depend on the factors that caused the deviation, since icteric symptoms are only a consequence, and treatment measures should be aimed at eliminating the causes of the disorder.
Generally accepted medical practice for severe hemolysis of red blood cells provides:
- Conducting infusion therapy with glucose or albumin.
- Carrying out plasmapheresis.
For metabolic disorders in children and adolescents, phototherapy is used, in which irradiation of the skin promotes the conversion of free bilirubin into bound bilirubin.
If the enzyme capacity of the liver is insufficient, drugs are prescribed that enhance its activity.
We must not forget that high bilirubin in the blood, like yellowing of the skin, always indicates serious problems in the body, and therefore early identification, diagnosis of the causes that caused it, and immediate treatment are of primary importance.