A little history
American doctors first encountered this pneumonia-like disease in 1976. It happened in Philadelphia after the American Legion convention. Three days after the end of the event - July 27 - one of the participants suffered sudden death, which was preceded by pneumonia of unknown etiology. After some time, new patients with specific signs of pneumonia were identified among the participants of the congress.
All cases of illness were linked together by official authorities only on August 2, and by that time, death from pneumonia had occurred in 18 patients. As a result, after the congress, 221 people developed pneumonia and 34 patients died.
After analyzing all the cases of this specific pneumonia and isolating its causative agent - Legionella of the Legionellaceae family - this characteristic disease was called “Legionnaires' disease”.
It is assumed that at the American Legionnaires' convention, colonies of this pathogen were in the fluid of the ventilation systems of the hotel in which the participants of the mass event lived. It was in this way that bacteria entered the respiratory system and provoked pneumonia. Subsequently, after a more detailed study of the various forms of this disease, the name of this pathology was changed to “legionellosis”, and the final classification of the forms of this disease has not yet been established.
According to WHO statistics, the mortality rate for legionellosis is about 20%. This disease occurs everywhere, and its prevalence is influenced not only by climatic conditions, but also by anthropogenic factors. This explains that Legionnaires' disease is partly a man-made infection.
The overall incidence of this infectious disease is low worldwide. But every year in different countries (mainly in economically developed ones) sporadic or epidemic outbreaks of legionellosis are observed.
During the period from 2000 to 2007, outbreaks of this disease were observed in Italy, Russia, Spain, France, the USA, etc.
Experts have noted the fact that travelers, tourists, hotel employees and health workers are more likely to get legionellosis. This is explained by the fact that during changes in climatic zones, immunity is often reduced and various vehicles are used for movement, which can be a reservoir for the propagation of the pathogen. And in medical institutions and hotels, an autonomous ventilation system can become a place for the development of Legionella colonies.
Pitfalls in diagnosing legionellosis
Diagnosing pneumonia is not difficult. It is much more difficult to determine the causative agent of legionellosis, especially when the suspicion falls on legionella. The Infectious Diseases Society of America and the American Thoracic Society [4] recommend being wary and considering the possibility of Legionnaires' disease in six categories of patients with pneumonia:
- patients with community-acquired pneumonia who have not responded to antibiotic therapy;
- patients with severe pneumonia, especially those who require intensive care;
- immunocompetent patients with pneumonia;
- patients with pneumonia living in areas with established outbreaks of legionellosis;
- patients who traveled within two weeks before the onset of illness;
- patients with suspected nosocomial pneumonia.
An important method for diagnosing Legionella pneumonia is the isolation of Legionella on selective media from the respiratory tract or lung tissue. A test that allows the isolation of Legionella antigens in urine is often used, although culture is still more sensitive and specific. In addition, PCR is sometimes used to isolate Legionella DNA from urine, sputum, serum samples, or bronchoalveolar lavage fluid.
Causes
The causative agent of legionellosis was first isolated in 1977 by scientists S. Shepard and J. McDade. It turned out to be a gram-negative bacterium, Legionella, which was cultured from a section of the lung of a patient who died of Legionnaires' disease.
Modern science knows about 40 species of Legionella, and 22 of them are dangerous to humans. In 90% of cases, the cause of the disease is Legionella pneumophila.
This pathogen is stable and can survive for 112 days in a liquid medium at a temperature of 25 ° C, and at a temperature of 4 ° C it remains active for up to 150 days. Legionella is killed by exposure to a 3% chloramine solution after 10 minutes and 1 minute after exposure to a 0.002% phenol solution, 70% ethyl alcohol or 1% formaldehyde solution.
The natural source of infection is fresh water reservoirs (especially non-flowing ones) or soil. At a temperature of 35-40 °C, the pathogen begins to actively multiply in protozoa (for example, in amoebas) and becomes resistant to chlorine when such infected microorganisms enter the water supply system.
Due to this adaptability, legionella colonizes and multiplies intensively in water tanks, artificial reservoirs, water supply systems, ventilation systems, fountains, bathrooms and saunas, rooms for balneological procedures, air conditioners and other technical objects in which moisture is present. In such artificial structures, the pathogen receives even more favorable conditions for reproduction and becomes a colony.
Human infection with bacteria of the genus Legionella occurs through airborne droplets, soil or airborne dust. In this case, a sick or recovered person does not become a source of infection. The pathogen enters the respiratory tract by inhaling droplets of water or soil particles (i.e., aerosol mixtures) containing Legionella. Infection can occur when working with soil, at a construction site, during certain medical procedures (for example, during balneotherapy or intubation) and when staying in infected areas of hospitals, hotels, in transport, etc.
There is a high human susceptibility to Legionella pneumophila. Infection can be facilitated by the presence of endocrine or immunodeficiency disorders, chronic pathologies, smoking and alcohol abuse.
The incidence of legionellosis is observed in different seasons. More often, this disease is observed in travelers and older people (and in men more often than in women). Cases of nosocomial outbreaks of legionellosis are periodically recorded.
Legionellosis, or air conditioner disease
What is the main danger? Air conditioners, their internal parts and the air passing through the devices are a breeding ground for various microorganisms, and some of them are real “pests” for the human body. During one hour of operation of a typical home air conditioner, about 90 thousand microorganisms fly through it! At the same time, some of them are in no hurry to leave their new haven and settle on filters and other internal parts. Others spread along with the exhaust air to all surfaces of the room: ceiling, walls, furniture, floor. And then, when we inhale the air circulating in the room, these small and seemingly harmless travelers end up on our mucous membranes. Yes, most of them are not dangerous for a healthy human body, but some can cause an infection called Legionnaires' disease, or legionellosis. What kind of infection is this, why is it dangerous, how does it manifest itself and how to get rid of it?
The causative agent of legionellosis is the bacterium Legionella pneumophila. It was discovered back in 1977 and belongs to the group of gram-negative microorganisms1. Statistics provided by the World Health Association say: legionellosis infection is quite dangerous, with a mortality rate of about 20%. Moreover, this disease can be found anywhere, regardless of climate. But the disease is characterized by a pronounced seasonality: outbreaks occur most often in the summer - here there is a direct connection with the operation of air conditioners. Why does this happen and what is the fault of these devices that help survive the heat? Legionella loves moisture, and the condensation that accumulates in the “containers” is an excellent environment for them to live and reproduce, especially in summer at high temperatures2.
In fact, there is more than one type of Legionella - there are about 40 of them! And just over half are dangerous. Legionellosis disease is caused by Legionella pneumophila in 90% of cases.
Fortunately, legionellosis is not airborne. Infection occurs when the “victim” inhales the pathogen along with moistened cold air coming from the air conditioner. Diseases such as weakened immunity, respiratory diseases, chronic respiratory allergies, as well as bad habits (smoking) and stress3 increase the risk of development. Therefore, it is believed that the following groups of people become most frequently ill: travelers, hotel and medical workers, that is, those who are often in rooms with air conditioning or a developed ventilation system. In addition, travelers, due to changes in time zones and climate zones, expose their body to stress, which reduces immunity, which is also of considerable importance.
But are air conditioners the only ones to blame for the spread of legionellosis? It turns out that the bacterium can enter the body in the natural environment. Thus, the main source of infection in nature is soil and water resources with fresh water (rivers, lakes, ponds, reservoirs, swimming pools, fountains, etc.), but only in the summer. When the temperature rises to 35-40 degrees, Legionella actively multiplies in the organisms of amoebas and other protozoa and develops tolerance to various influences.
What is this bacterium afraid of? It is destroyed by a 10-minute exposure to a three percent chloramine solution, a minute exposure to a 0.002% phenol solution, formaldehyde (1%) and ethyl alcohol (70%).
Symptoms For legionellosis, the incubation period can be either short or quite long: from a couple of hours to 7 days. The pathogen, entering various organs through the bloodstream, often attacks the liver, nervous system, kidneys, lungs and even bone marrow. Legionellosis, the symptoms of which may differ depending on which organ is affected, has several clinical forms, which we will discuss below.
Legionella pneumonia. A serious disease that causes respiratory failure, abscesses and pleurisy. Its manifestations are: • Poor appetite; • Very high temperature (39-40 ̊C); • Weakness; • Adynamia; • Both chills and excessive sweating; • Severe muscle pain; • Diarrhea.
With further development of the disease, signs of characteristic toxic damage may appear: • Absent-mindedness, delirium; • Visual and auditory hallucinations; • Fainting; • Slow reactions.
Then shortness of breath, cough and other typical signs of pneumonia appear.
Pontiac fever. This manifestation of infection does not pose such a high danger and is more reminiscent of an acute respiratory infection. This type most often does not lead to serious consequences provided that treatment is started in a timely manner. The symptoms are approximately the same as those of an acute respiratory disease, but they may be accompanied by: • Insomnia; • Dizziness; • Blurred consciousness.
Fort Bragg fever. This is also an unpleasant, but not life-threatening form of infection. The symptoms are similar to those of acute respiratory infections, but skin rashes are added to them.
Diagnosis In order to correctly identify and differentiate legionellosis, diagnosis must be carried out by a specialist in a medical facility. The stages of examining the patient are: • Listening to lung sounds; • X-ray; • Blood tests (clinical and bacteriological), as well as antigen tests, analysis of pleural fluid and sputum.
Due to the similarity of symptoms with some other diseases, it is very important to make the correct diagnosis and differentiate legionellosis from pneumonia of other etiologies, ARVI, Q fever, etc.
Complications The main danger of legionellosis is the high probability of developing complications: abscesses, infectious-toxic shock, endocarditis, pleurisy. Serious consequences can be the development of several types of failure: respiratory, cardiovascular, renal. If therapy is not carried out or is incorrect, and legionellosis is severe, causing complications, this can be extremely dangerous. Therefore, it is so important to start communicating with your doctor in a timely manner, making sure to follow all his instructions and not self-medicate.
Treatment Treatment tactics for legionellosis are selected depending on what form the infection takes. Hence the choice of doctor: it is either a therapist, an infectious disease specialist, or a pulmonologist. To get rid of the disease, a whole range of means is used, which necessarily includes antibiotics and means to relieve symptoms. It is important that the selection of antibacterial drugs must be carried out individually for each patient, taking into account medical history, allergies, previous experience with antibiotics and the severity of the disease. The duration of therapy is quite long - two to three weeks, that is, longer than in the treatment of ordinary ARVI, and in most cases it should be carried out exclusively in a hospital, since the infection seriously disrupts the functioning of the organs and systems of the body4.
If the disease becomes severe, resuscitation measures may be required, including ventilation (artificial) and oxygen therapy.
Prevention The main measure for preventing legionellosis is timely replacement of filters in air conditioning units and cleaning of ventilation systems (several times a year), regular wet cleaning of the premises where it is used: washing floors, walls, ceilings, showers, bathtubs and other plumbing using hot ( above 80 °C) water and/or chlorine-based disinfectants5. In medical institutions, mandatory disinfection and cleaning of medical equipment.
The person himself, who is often in the area where air conditioners operate (that is, every resident of a large city), must take the following measures to help protect himself not only from Legionnaires' disease, but also from other ailments provoked by the operation of air conditioners. After all, air conditioners not only create a significant temperature difference between indoors and outdoors, but also dry out the air, which is harmful to our mucous membranes. • Do not set the air conditioner temperature below 18°C. Optimal - 22-23°C. If it is hot outside, say, 38 °C, then the temperature in the room must be kept at least 25 °C, since the difference should not be more than 10 °C. • Keep the room humidified, use humidifiers or other methods to eliminate dryness. • Choose a place away from a direct stream of air, no matter how hot it is: a properly configured air conditioner cools the entire room, so you should not try to get into the very breeze. • Lead a healthy and active lifestyle, toughen up, carefully monitor your diet, and stock up on vitamins in the summer. • Walk in the fresh air more often, try not to spend the entire working day in an air-conditioned room: leave the office, take a walk during lunch. • Do not place the air conditioner at home directly above the sleeping or working area. • To protect local immunity, you can use various drugs that activate the body's defenses. Unique local immunomodulators based on bacterial lysates may be suitable: IRS®196 nasal spray and Imudon®7 lozenges. In complex therapy, they help the body cope with the disease 2 times faster8.
Nasal spray IRS®19 is a sprayed fine aerosol that coats the mucous membrane of the nasal passages and helps reduce the risk of developing the disease9.
1. World Health Organization - https://www.who.int/ru/news-room/fact-sheets/detail/legionellosis (date of publication 02/16/2018, access date 06/02/2018) 2-3. Bacteriologist, Ignatiev A.A., epidemiology - https://uhonos.ru/infekcii/legionellez/ (date of access: 06/02/2018) 4. L. Mulazim-ogly, V. Yu. LEGIONELLIOSIS. (From Harrison's Principles of Internal Medicine. 14th edition, 2002) - https://humbio.ru/humbio/infect_har/002609df.htm 5. A. Messineo, D. Panno, W. Mazzucco (Translated with abbreviations from the REHVA magazine, Scientific editing by S. N. Khorev, chief project engineer of Promstroyproekt CJSC) Prevention of the appearance of Legionella bacteria in heating, ventilation and air conditioning systems - https://www.abok.ru/ for_spec/articles.php?nid=3310 6. Instructions for medical use of the drug IRS®19 dated 05/17/2016 7. Instructions for medical use of the drug Imudon® lozenges dated 07/02/2018. 8. Kladova O.V. et al., “Clinical effectiveness of Imudon in patients with tonsillopharyngitis against the background of acute respiratory diseases. Children's infections, 2005, No. 1, p. 55-59. 9. Namazova-Baranova L.S. and other topical immunomodulators: from the treatment of rhinitis to collective prevention of acute and chronic respiratory pathology // Issues of modern pediatrics, - 2011, Volume 10. - No. 5, pp. 32-38.
How does the disease develop?
Legionella enters the human body through the respiratory tract. The pathogen is fixed in different parts of the respiratory system (including in the lung tissue). The depth of its penetration depends on the size of aerosol infected particles, their dose and breathing patterns. Microorganisms can also enter the human body along with protozoa infected by them and during certain surgical and other medical procedures. It is possible that they will be introduced into the body along with contaminated drinking water.
Through the bloodstream, the pathogen can enter various systems and organs. The lungs, liver, kidneys, nerve tissues and bone marrow are most often affected. With a high level of Legionella in the blood, the disease can develop as a septic type and be accompanied by the appearance of secondary purulent foci or septic endocarditis.
Causes
The disease develops as a result of the penetration of morphological legionella into the body. These bacteria are characterized by good resistance to various factors and external influences.
When the causative agent of this pathology enters the body of an adult or child, severe damage to the lung parenchyma occurs. If this internal organ swells, a strong inflammatory process occurs, blood cells accumulate and disintegrate.
Legionellosis of the lung is a common disease. People who have bad habits such as smoking and drinking alcoholic beverages are at greatest risk. Their immunity is greatly reduced. Elderly people and travelers are susceptible to the development of legionellosis.
Symptoms
The first signs of the disease can be observed after 2-10 (on average 4-7) days from the moment of infection. Their severity and further course of Legionnaires' disease will depend on the clinical form of the disease.
The most common forms of legionellosis are:
- Legionnaires' disease (or severe pneumonia);
- acute alveolitis;
- Pontiac fever;
- Fort Bragg fever.
More rarely, legionellosis can occur in subclinical or generalized forms. In such cases, the patient may experience damage to multiple organs or sepsis.
Legionnaires' disease (severe pneumonia)
Legionnaires' disease often occurs as severe pneumonia.
In the first days of the disease, patients present the following complaints:
- intense headache;
- severe weakness;
- adynamia;
- loss of appetite;
- diarrhea (in some cases);
- increased temperature (39-40 °C);
- chills;
- sweating;
- intense muscle pain.
Somewhat later, patients show signs of toxic damage to the nervous system:
- fainting and fainting;
- hallucinations;
- lethargy;
- emotional lability;
- rave.
In some cases, neuralgic disorders can manifest themselves with the following symptoms:
- involuntary movements of the eyeballs of an oscillating nature (nystagmus);
- violation of coordination of movements;
- paralysis of the extraocular muscles;
- difficulty in pronunciation.
A few days later, the patient shows signs of pneumonia:
- first dry and then wet cough with a small amount of mucopurulent or bloody sputum;
- chest pain (during breathing);
- dyspnea.
When listening to the lungs, areas of weakened breathing, dry and wet rales, and pleural friction noise are determined. X-ray films reveal focal infiltrates in the lungs, which sometimes merge and form large foci of darkening.
This form of legionellosis is severe and may not respond well to treatment. The disease can be complicated by the development of pleurisy, abscesses, respiratory and heart failure. In some cases, Legionnaires' disease ends in infectious-toxic shock.
When the blood vessels and heart are damaged, the patient develops the following symptoms:
- decreased blood pressure;
- bradycardia with periods of tachycardia.
30% of patients experience symptoms of damage to the digestive organs and kidneys:
- prolonged diarrhea;
- jaundice;
- a feeling of transfusion and rumbling in the intestines;
- changes in biochemical blood parameters;
- signs of kidney failure.
After recovery, headaches, signs of asthenia (weakness, memory loss, dizziness, irritability) and renal failure are observed for a long time. X-rays of the lungs reveal pleural abnormalities and pulmonary infiltrates over several weeks.
Acute alveolitis
From the first days of the disease, the patient develops a dry cough, which is accompanied by a rise in temperature to high numbers and general intoxication (headaches, a feeling of weakness, muscle pain, unmotivated fatigue, severe weakness, etc.). Later, during a cough, mucopurulent sputum begins to separate. The patient experiences increasing shortness of breath. While listening to the lungs, diffuse crepitus is determined.
This form of legionellosis is accompanied by the effusion of fibrin and red blood cells from the blood vessels into the alveoli. The alveolar septa swell, and with a protracted and progressive course of the disease, the patient may develop fibrosis.
Pontiac fever
Legionellosis can occur in the form of an acute respiratory disease (Pontiac fever) and is not accompanied by damage to lung tissue. In such cases, the incubation period usually lasts about 5 hours or 3 days.
The patient's temperature rapidly rises to high levels (usually up to 40 ° C) and the following symptoms appear: headache, severe weakness, chills and diffuse muscle pain, development of confusion and dizziness. High temperature is observed for about 2-5 days and is accompanied by a runny nose, tracheobronchitis or bronchitis. In some cases, abdominal pain and vomiting are observed.
Pontiac fever is often accompanied by neurological disorders. The patient may experience the following symptoms:
- impaired coordination of movements;
- disorders of consciousness;
- sleep disorders;
- dizziness.
Unlike severe pneumonia (Legionnaires' disease), this form of legionellosis has a more favorable course. Its symptoms disappear after a few days, but the asthenic state and autonomic disorders persist for a longer time.
Fort Bragg fever
This rarer form of legionellosis occurs as an acute febrile illness, which is accompanied by the appearance of exanthema (rashes in the form of spots, vesicles or papules). The incubation period for Fort Bragg fever usually lasts several hours or up to 10 days.
The patient's temperature rises to 38-38.5 °C, chills, general intoxication and respiratory symptoms (usually signs of bronchitis) appear. Against the background of these manifestations, a scarlatina- or measles-like, large-spotted or petechial rash is observed. Elements of the rash can be localized on any part of the skin, and after they disappear, there is no peeling.
The course of this form of legionellosis is usually favorable. The duration of the disease is about 3-7 days.
Clinical course of Legionella infection
With a disease such as legionellosis, symptoms do not appear from the moment of initial contact, but after the incubation period. It should last about 2-10 days: during this period of time, Legionella multiplies in the body, but the activity of pathological processes is low, which causes minor (subclinical) symptoms. The infection occurs either along a mild path, characterized by a flu-like syndrome, or as a pneumonia with severe damage to the respiratory tract.
The first type of legionellosis is associated with good protective abilities of the body. As a result of contact with infection, acute respiratory legionellosis develops, similar to bronchitis. This type of clinical course is called Pontiac fever. The second type of disease is Legionella pneumonia. It is more severe and has a high mortality rate.
It is worth noting that Pontiac fever is no less serious disease, it is only less dangerous legionellosis. Legionnaires' disease (symptoms of the disease are identical to those of other atypical pneumonias) is a manifestation of severe Legionnaires' pneumonia, which often leads to death for the patient.
The classification also includes legionellosis, the symptoms of which are the most severe. This is alveolitis - a more severe form of pneumonia, increasing intoxication of the body and reducing the likelihood of recovery. At the same time, it is also worth distinguishing two forms of legionellosis depending on the place of occurrence. This is nosocomial legionellosis and sporadic, that is, out-of-hospital. The diagnosis of hospital-acquired legionellosis is valid only if clinical signs appear 2 or more days after admission to the inpatient department.
Diagnostics
Diagnosis of legionellosis is always complex and consists of carrying out the following activities:
- listening to sounds in the lungs;
- X-ray of the lungs;
- laboratory tests: bacteriological studies of blood, sputum and pleural fluid, clinical (general) blood test, blood test to indicate pathogen antigens using ELISA and RIF methods.
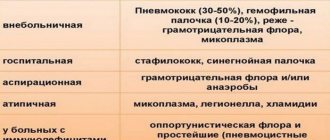
When making a diagnosis, a differential diagnosis of legionellosis with the following diseases is required:
- pneumonia of various etiologies (pneumococcal, mycoplasma, staphylococcal, provoked by Pseudomonas aeruginosa, klebsiella, etc.);
- ARVI;
- psittacosis;
- Q fever and other pulmonary pathologies.
Characteristics of symptoms of Pontiac fever
Pontiac fever is an example of a mild disease called legionellosis. Symptoms of legionellosis of this nature resemble influenza or severe parainfluenza: the patient is worried about a high temperature (38-39 degrees), which appears approximately 36 hours after initial contact with the infection. Intense muscle pain and headaches also develop, and a dry cough begins. Occasionally, especially with a fever of more than 38 degrees, vomiting develops.
As the temperature rises, the accompanying symptoms are disturbing: thirst, dry mouth, decreased amount of urine. Chest pain also appears, although this symptom is more associated with Legionella pneumonia affecting the pleura than with Pontiac fever. Occasionally, against the background of intoxication, photophobia, impaired thinking and concentration of attention appear, although after recovery, as a rule, there are no neurological complications.
It is noteworthy how legionellosis manifests itself: the symptoms are not immediately noticeable, nor is the time of first contact with the infection. And as soon as enough pathogens have accumulated in the body, they appear. It seems to the patient that all clinical signs appeared without precursors, that is, against the background of complete health. This makes its own adjustments and can become the basis for an unjustified diagnosis of meningitis, because this disease also begins as the flu.
Treatment
Patients with severe legionellosis must be hospitalized. In the future, treatment tactics are determined individually.
For Pontiac fever, therapy may be limited to symptomatic medications without antibiotic therapy. The patient may be prescribed:
- antipyretic and anti-inflammatory drugs;
- nasal drops;
- expectorants;
- multivitamin preparations;
- drinking plenty of fluids.
For other forms of legionellosis, the patient is prescribed macrolide antibiotics. The most effective is Erythromycin. It can be administered intramuscularly or intravenously (stream or drip). In the absence of positive dynamics, the patient is additionally prescribed Rifampicin. The course of antibiotic therapy is usually about 2-3 weeks. If necessary, the effect is secured by prescribing Pefloxacin or Ofloxacin.
Treatment aimed at eliminating the pathogen is complemented by measures to combat intoxication, the development of bleeding, respiratory, cardiac and renal failure. To eliminate gas exchange disorders, oxygen therapy and artificial ventilation are often performed. If necessary, anti-shock measures are provided.
Etiology
L. pneumophila
cells proliferate in cultured human lung fibroblasts
Legionellosis is an infectious pathology induced by the introduction of microorganisms of the genus Legionella
.
According to modern data, about 90% of legionellosis is associated with the species L. pneumophila
.
Among other Legionella species, the disease is most often caused by L. micdadei
,
L. longbeuchae
,
L. dumoffii
and
L. bozemanii
[14][15][16]. Legionellosis, caused by the latter bacteria, develops, as a rule, against the background of immunodeficiency states. In total, 17 out of 41 Legionella species are pathogenic to humans.
Legionella pneumophila
on an electroscanogram
Morphologically, Legionella are gram-negative aerobic bacilli that can persist for a long time in the environment. Legionella often has pointed ends. They do not form capsules. Sometimes rods can stain gram-positive, but the cell wall of Legionella has a typical gram-negative structure. Legionella is oxidase- and catalase-positive, hydrolyzes sodium hippurate and gelatin, does not reduce nitrates and urea. Among carbohydrates, Legionella hydrolyzes only starch.
Legionella pneumophila
on an electroscanogram
There is good growth of Legionella under aerobic conditions on media enriched with adsorbents for the absorption of metabolites. The optimal temperature for bacterial growth is 35 °C[17], the optimal acidity is 6.9. After 3-5 days on solid media, bacteria form gray glassy colonies with smooth edges. Legionella usually does not grow well in liquid media. The cultivation of Legionella on chicken embryos has also been described.
The pathogenicity of Legionella is associated with the formation of two toxins (cytotoxin and a toxin that is lethal for laboratory mice), as well as with the formation of a number of other proteins, lipopolysaccharide and some enzymes that ensure the penetration of the pathogen and its spread (protein kinases, phospholipase C and legiolysin).
Prevention
Means for the specific prevention of legionellosis have not yet been created.
Measures to prevent the spread of this disease are aimed at constant monitoring of the sanitary and hygienic condition of water pipes, swimming pools and other artificial reservoirs, medical equipment, air conditioning and ventilation systems. To disinfect them, disinfectants or special ultraviolet irradiators are used.
After identifying patients with legionellosis in the outbreak, the following measures are carried out:
- hospitalization of the patient (if necessary);
- observation of his immediate environment;
- dispensary observation of the ill person.
The patient's sputum, dishes and underwear should be disinfected by autoclaving or disinfection with a 25% phenol solution.
Legionellosis is not transmitted from a sick person to a healthy person, and therefore isolation and prevention among contact persons is not carried out.
Legionellosis has no specific symptoms, but due to the danger of this disease, it requires seeking medical help. When its first signs appear - fever and cough - you should definitely contact a therapist or pulmonologist. Timely treatment can prevent the development of serious complications and death. Remember this and be healthy!
Prevention of Legionnaires' disease
To prevent legionellosis, when working with water supply systems, they are guided by regulations, and there are instructions for maintaining and monitoring water supply systems.
Other potential sources of Legionella bacteria include spas and hot tubs. They also need careful and regular examination. Prevention of Legionnaires' disease includes regular cleaning and maintenance of water facilities.
Those at risk: smokers, elderly people with AIDS, cancer, chronic lung disease, kidney disease or diabetes should avoid public water systems such as jacuzzi, spas, hot tubs, etc. in hotels, resorts and cruise ships.
Water cooling systems have several aspects that are regulated by infection prevention guidelines. This includes commissioning, operation, maintenance, cleaning and routine procedures.
There should be regular checks for microbial growth, leaks, algae, blockage or stagnation and water splashing.
Water in all systems must not stagnate and chemicals must be added where necessary to limit the accumulation of scale, microbiological growth, etc.
Cooling towers must be operated and maintained with regular inspections. At least monthly water purification, microbiological monitoring and regular six monthly cleaning procedures.
Cleaning should include physical cleaning as well as disinfection.
Prevention of Legionnaires' disease in air conditioning systems
- Air conditioning systems must also be efficient in design, commissioning, operation, maintenance and cleaning.
- There should be easy and safe access for maintenance of air filters.
- Air filters should be designed so that they do not accumulate moisture.
- Maintenance and cleaning procedures.
Which doctor should I contact?
If you have a cough and fever, it is best to consult a pulmonologist. However, at the first stage, both a therapist and a family doctor can help the patient. After clarifying the diagnosis, you will probably need to consult an infectious disease specialist. If organs other than the lungs are affected, the patient is examined by a cardiologist, neurologist, ophthalmologist, gastroenterologist, nephrologist. If infectious-toxic shock develops, treatment is carried out by a resuscitator.
Rating: (votes - 1 , average: 5.00 out of 5)
Epidemiology
Legionella lives in soil and freshwater bodies of standing and blooming water. This is their natural habitat. There are man-made artificial systems in which conditions for Legionella to survive are more favorable. Microbes actively grow and multiply in the fluid of air conditioners, cooling systems, boilers, fountains, swimming pools, and shower units. The most common sources of Legionella contamination are cooling towers, home warm water systems, and spas.
Legionella accumulates in the liquid contained in centralized air conditioners
Legionellosis is transmitted by airborne droplets or airborne dust. The pathogen accumulates in air conditioners and showers and disperses into the air when they are turned on. Infection in persons with immunodeficiency can occur when swimming in warm fresh water. In such cases, aspiration of water plays a significant role.
Home air conditioners and split systems do not pose a danger to humans and are not sources of infection. Moisture does not accumulate in them in large quantities. Humidifiers can contain contaminated water if it is not changed regularly.
Extrapulmonary legionellosis develops due to contaminated water entering surgical and traumatic wounds. The contact route is quite rare for legionellosis, but not exceptional. The disease is manifested by local symptoms in the area of the wound or skin lesion and systemic signs of intoxication.
The most susceptible to infection are predominantly male persons from the risk group: smokers, drinkers, drug users, those suffering from diabetes mellitus, lung diseases, metabolic disorders, AIDS, and long-term use of immunosuppressants.
Legionellosis is most often detected among hotel clients and medical workers in pulmonology hospitals, hemodialysis centers, and intensive care units. Legionellosis is characterized by a summer-autumn seasonality.
Legionella is distributed throughout the world and forms part of the microbial flora of many natural and artificial aquatic systems and soils. The greatest epidemiological significance is the entry and reproduction of pathogens in the water supply and air conditioning systems. The mechanism of infection is airborne droplets and airborne dust.
The susceptibility of the population is high, but more often the disease occurs as an acute respiratory infection (Pontiac fever), pneumonic odds develop in people with reduced resistance. Risk groups: middle-aged and elderly people, smokers, patients with alcoholism, drug addiction, diabetes, and those in a state of immunodeficiency. The disease is recorded throughout the year, but more often in the summer months.
Pathogenesis
Little is known about the pathogenesis of legionellosis. The gateway to infection is the mucous membrane of the respiratory tract. Penetration of the pathogen into the body occurs through inhalation of water aerosols (showers, air conditioners, baths, ultrasonic water sprays, humidifiers of artificial ventilation systems, fountains, etc.).
Despite the fact that Legionella is found in the sputum of patients, evidence of transmission of infection from person to person has not been established. Most cases of Legionnaires' disease involve the lungs. Pathological changes, as a rule, cover at least one lobe of the lung and occur in the form of confluent pneumonia.
The inflammatory process spreads to the terminal bronchioles and alveoli (larger bronchi are usually intact). In the affected area, massive exudation of polymorphonuclear neutrophils and macrophages is detected with the phenomena of intense lysis of leukocytes, accumulation of nuclear detritus and fibrin. Severe swelling of the interstitial tissue is also noted.
The fact that cigarette smokers are more susceptible to infection than nonsmokers suggests that impaired alveolar macrophage function may play a role in the development of the disease. It is assumed that these phenomena are associated with the release of toxins by Legionella, causing other clinical manifestations of the disease. It should be noted that all the described changes are not pathognomonic for legionellosis and occur with pneumonia of other etiologies.
Microbes enter the body by inhaling water aerosols and settle on the epithelium of the respiratory organs. The target cells for Legionella are alveolar macrophages of the lower respiratory tract. Pathological changes develop in the lung tissue. Usually one lobe of the lung is affected. The disease can occur as confluent pneumonia.
The alveoli and bronchioles become inflamed, and exudate, consisting of polymorphonuclear neutrophils and macrophages, accumulates in the affected area. Leukocytes are lysed, and interstitial edema is noted. The development of fibrinous-purulent pneumonia, lung abscess, fibrinous-exudative pleurisy is possible. These processes and other clinical manifestations of pathology are caused by the release of toxins by Legionella.
After the death of microbial cells, endotoxins are released into the blood, which have a negative effect on the human body. Patients develop microcirculation disorders, hemorrhagic inflammation, and lymphoplasmacytic infiltration.
Treatment of legionellosis
The fundamental element in the treatment of legionellosis is the use of drugs of etiotropic significance, among which the most commonly used are antibacterial drugs of the pharmacological group of macrolides (Erythromycin in a daily dose of 4 g orally, and in severe cases - intravenous drip in a daily dose of 1 g). In a situation where antibacterial therapy does not have the desired effect in the form of leveling the intoxication syndrome in the first two days of use, therapy should be supplemented with Rifampicin in a daily dosage of 1.2 g for a course of 14 days. In addition to antibacterial and anti-inflammatory therapy, the patient is advised to use immunostimulating drugs.
Prevention of legionellosis involves monitoring the cleanliness of the air conditioning system, the quality of tap water, which is used for hygiene and medical procedures, and the operation of the ventilation system. Prevention of legionellosis involves the use of various measures aimed at effectively reducing the concentration of the pathogen, and the main method of disinfection in this situation is thermal, as well as chemical. Specific methods for the prevention of legionellosis are not carried out due to the fact that this pathology does not belong to the category of anthroponotic infections.
Legionellosis – which doctor will help? If you have or suspect the development of legionellosis, you should immediately seek advice from doctors such as an infectious disease specialist or a pulmonologist.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!