Skin tuberculosis is a name that unites a whole group of diseases that manifest themselves on the skin very differently, but all of these diseases have one cause; they arise due to the entry of the tuberculosis bacillus into the skin.
Skin tuberculosis is a fairly rare disease, because the skin is not a suitable environment for the pathogen to multiply. The following are the provoking factors for the development of this disease:
- Improper metabolism in the skin
- Vitamin deficiency
- Vascular problems in the skin
- Failure to comply with sanitary and hygienic conditions
- Poor and deficient nutrition
- Unsuitable climate
- Acute infections: measles, scarlet fever
The causative agent of skin tuberculosis is the tuberculosis bacillus. There is a tuberculosis focus in the patient’s body, which can be in the internal organs or bones, lymph nodes; from this focus, Mycobacterium tuberculosis penetrates the skin either through the blood (hematogenous route) or through the lymphatic vessels (lymphogenous route). But infection can occur through damaged skin from external sources (sputum secreted by the patient, etc.)
Symptoms of skin tuberculosis
Tuberculous lupus of the skin
It is the most common form of cutaneous tuberculosis, affecting the epidermis.
It usually occurs in women, children and adolescents. Most often the face is affected, sometimes the buttocks, arms, and legs.
If the disease is not treated promptly, it can lead to the breakdown of the ear cartilage or the cartilage of the bridge of the nose.
In rare cases, it even leads to cancer and even death.
Scrofuloderma, or colliquative tuberculosis of the skin
Women are mainly affected by this form of the disease, most often manifesting itself in the cervical region.
- At first, almost imperceptible, painless nodules appear on the skin; over time, they grow into one dense nodule.
- If the disease is not treated in time, the skin begins to acquire a blue tint, the dense node gradually softens and comes out, and pus is released.
- After this, a deep scar appears at the site of the ulcer.
Papulonecrotic tuberculosis of the skin
It also usually occurs in young women.
- First, small papules that are hard to the touch appear, then a crust appears on their surface.
- If it is removed, small round ulcers form on the surface of the skin.
- Depressed scars remain on the skin.
Erythema induratum of the skin
Most often, the disease affects young women in the lower leg area, where deep and very dense blue-red nodes appear, which sometimes break out (the resulting ulcers in this case take a very long time to heal).
This type of cutaneous tuberculosis has a high tendency to relapse.
Warty skin tuberculosis
Infection usually occurs through injured skin, so it is most common among medical personnel.
The disease occurs on the arms (hands) and feet.
First, red nodules form, which then grow into warty pustules covered with dead skin debris.
Scars remain on the skin in the affected area.
Causes
Pathology occurs when mycobacteria enters the body. Most often this is the human type. In second place is bull and, in rare cases, bird.
Pathology can arise endogenously or exogenously.
The first option involves the spread of the tuberculosis bacillus already present in the body. The skin is affected in those people who have not been treated for tuberculosis of the skeletal system, lungs, lymph nodes, etc. Also if another location of tuberculosis was treated incorrectly or the patient interrupted the therapeutic course. Sometimes the body does not accept anti-tuberculosis drugs, and the doctor is forced to prescribe other weaker drugs. This variant may also contribute to the spread of MBC to other organs.
Exogenous - this is through direct contact.
- During cutting of cattle meat.
- During the autopsy of the body (in the morgue).
- During surgical operations (if there is a patient with tuberculosis on the operating table).
- In close contact with a person who has skin tuberculosis.
Diagnosis of skin tuberculosis
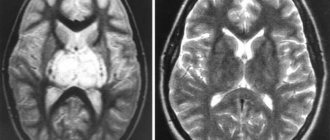
Skin tuberculosis: photo initial stage
As already mentioned, the vast majority of manifestations and forms of skin tuberculosis arise due to the presence of infection inside the body, so to prevent the appearance and development of the disease is diagnosis and prevention (especially fluorography and Mantoux tests).
It is better to identify tuberculosis in time rather than treat it: the process is long and complex, consisting of several stages.
First symptoms
In order to start treatment in a timely manner, you need to know what the pathology looks like. Symptoms depend on the type of skin tuberculosis, but the first signs have something in common.
In adults and children it is observed:
- rash;
- rise in temperature;
- weakness and malaise;
- frequent allergies;
- after performing Mantoux the result is positive.
To prescribe competent treatment, you need to find out what type of pathology is present specifically.
In the photo you can see rashes of various shapes and locations.
Diagnostics
Diagnosis of skin tuberculosis consists of:
- dermatological examination;
- taking anamnesis;
- taking tests for the presence of MBC in the blood and lesions.
A sample of material is taken from the ulcerated surfaces for PCR, bacteriological examination and bacterial culture. Tuberculin tests (Diaskintest or Mantoux) are mandatory.
Treatment
Treatment of tuberculosis of the skin can usually be carried out conservatively. In some (advanced) cases, they resort to a radical method.
Initially, the patient is registered at the tuberculosis dispensary. After examination and clarification of the form of the disease, the phthisiatrician decides on treatment. It is carried out on an outpatient basis. They are admitted to the hospital when there is a threat to life or the spread of MBD to other organs.
Medication
Conservative treatment of tuberculosis involves:
- antibiotic therapy;
- taking vitamins;
- local therapy;
- proper nutrition.
Antibiotics are prescribed in the form of:
- Rifampicin. Take at least 600 mg per 24 hours.
- Isoniazid. No more than 0.9 g in 24 hours.
- Ethambutol. 25 mg per kg for 24 hours.
- Pyrazinamide. From 500 to 2000 mg in 24 hours.
- Streptomycin. 500 to 1000 mg in 24 hours.
The course of treatment usually lasts at least 9 months, sometimes a year. Afterwards, a two-month preventive course is taken annually, for 5 years.
Nutrition should be balanced, high-calorie. It is important to limit your salt intake.
Vitamins and medications that improve microcirculation are also prescribed.
The solution is applied locally to the lesions:
- Saluzida (5%);
- Anestezin (12%);
- Sodium succinate (oil 0.5%).
It is important to strictly comply with all requirements, complete the course and, upon completion, undergo diagnostics again.
Surgical
If lupus or warty tuberculosis is diagnosed, large lesions can be removed surgically. Modern medicine makes it possible to do this through laser therapy, cryodestruction and diathermocoagulation.
Forecast
The prognosis depends on the form of skin tuberculosis, the severity of symptoms and the effectiveness of treatment.
- Tuberculous lupus is a long-term disease. In some cases, the lesion may not show a tendency to progress over many years even without treatment, in others the process slowly spreads, covering more and more new areas of the skin. This is facilitated by intercurrent diseases, unfavorable living conditions and other factors that weaken the body’s defenses and reduce its reactivity.
- Scrofuloderma. The disease is chronic, lasting for months and years with remissions. Mild cases can be successfully treated with modern methods. In cases of advanced ulcerative process, the prognosis is less favorable.
- Warty skin tuberculosis. The prognosis is often favorable, although the course of the disease is long-term and chronic.
- Ulcerative tuberculosis of the skin. The prognosis depends on the course of tuberculosis of internal organs. Currently, due to advances in the treatment of general tuberculosis, the prognosis of ulcerative tuberculosis of the skin and mucous membranes has improved, and the frequency of this disease has sharply decreased.
(Visited 2 124 times, 1 visits today)
Prevention
The incidence rate is influenced by the environment. The state of the environment makes an important contribution to the development of skin tuberculosis. In addition, social factors are not the least important. In this regard, preventive measures should be aimed at improving environmental conditions and cleaning it.
Dispensary observation for patients, as well as outpatient and inpatient therapy should be established. Health care providers should ensure that their patients undergo annual preventive screenings.
Skin tuberculosis is a disease that not only spoils a person’s appearance, but is also a consequence of serious disturbances in the functioning of the body and damage to internal organs. If the disease is detected at an early stage of development, the course of therapy will be significantly shorter and the prognosis will be more favorable.
Your dermatologist
O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”SKIN TUBERCULOSIS is a group of diseases caused by the introduction of Mycobacterium tuberculosis into the skin. In patients with skin tuberculosis, mycobacteria of the human type are more often found.
Tuberculosis of the skin is a fairly rare phenomenon, but recently one can note a trend toward a constant increase in incidence both in Russia and in European countries.
A number of conditions that reduce the body's defenses can contribute to the development of the disease.
The endogenous route of spread (hematogenous, lymphatic) is much more common than the exogenous route. It is possible to spread the pathogen per continuitatum from neighboring organs affected by the tuberculosis process or by autoinoculation (with intestinal tuberculosis, mycobacteria can be introduced through feces into the skin surrounding the anus).
Histologically, in tuberculosis, granulomas of epithelioid cells surrounded by lymphocytes are detected in the skin. Characteristically, there are giant Langerhans cells and caseous necrosis in the center of the tubercle. Mycobacteria themselves can also be detected.
Clinic.
Dermatological forms of tuberculosis include pathological processes that vary in clinical picture.
Tuberculosis lupus (lupus vulgaris) is the most common form of skin tuberculosis.
The main morphological element is a tubercle (lupoma), which is an infectious granuloma. The tubercles tend to grow peripherally, merge to form solid foci, and become ulcerated. After resorption of the infiltrate, a scar or cicatricial atrophy of the skin remains.
With vitropresia of the tubercle, the “apple jelly” phenomenon and retraction of the tubercle when pressed on it with a button-shaped probe (Pospelov test with a probe) are revealed.
Highlight:
- flat,
- ulcerative,
- tuberose,
- tumor-like
- verrucous,
- papillomatous,
- psoriasiform,
- mutilating,
- disseminated
forms of tuberculous lupus. A combination of one or more forms (usually flat and ulcerative) in the same patient is possible.
The rash is usually localized on the face, but can also be on the torso and limbs. The mucous membrane of the nasal cavity and mouth is often affected.
Tuberculous lupus usually occurs against the background of a positive reactivity of the body. More often registered in women. Sometimes it develops after a BCG vaccination or some time later at the site of a vaccination scar.
It is characterized by a sluggish, long-lasting and benign course.
Colliquatic cutaneous tuberculosis (scrofuloderma) is the second most common form of cutaneous tuberculosis.
The rashes are initially represented by dense, painless nodules, which, quickly increasing in volume, turn into a node tightly fused to the underlying tissues. The skin above it acquires a bluish tint. Subsequently, the node softens and opens with the release of purulent contents with inclusions of necrotic tissue. At the site of the node, an ulcer forms with soft edges, a yellowish coating and flaccid granulations at the bottom. After its healing, very characteristic “ragged” scars of irregular shape remain, covered with papillary-like outgrowths of the skin and bridges.
Scrofuloderma occurs primarily as a result of the introduction of mycobacteria into the skin from affected lymph nodes or through the lymphogenous route from other foci of tuberculosis present in the patient.
The neck area is most often affected. Mostly women are affected.
Tuberculin reactions usually give a positive result.
Papulonecrotic tuberculosis of the skin is characterized by hemispherical papules the size of a hemp seed, reddish in color with a bluish tint, and dense in consistency. Necrosis occurs in the central part of the papule. Necrotic masses shrink into a tight crust, after removal of which a rounded ulcer with steep edges is formed. After its healing, a characteristic depressed, or “stamped” scar remains.
Papules are located scatteredly on the legs, thighs, buttocks, extensor surfaces of the upper extremities, mainly in the joint area.
It is observed more often in young women.
The Mantoux test is positive in most patients.
Erythema induratum of Bazin's clinical picture resembles nodose vasculitis.
The main element is a dense, fused to the skin, low-painful node. The skin over it is initially unchanged, but later it may become reddish in color with a bluish tint.
With regression, an area of scar atrophy of varying severity remains. Sometimes the node softens and ulcerates (Hutchinson type). The ulcers are shallow, their bottom is covered with a yellow-green coating.
The nodes are localized on the legs, thighs, upper limbs, and abdomen; Women are more likely to get sick.
Warty skin tuberculosis is characterized by painless reddish nodules; in the center of the infiltrate, warty growths appear, covered with horny masses. The rashes are most often located on the fingers, back and palm surfaces of the hands, and soles.
More common among slaughterhouse workers and veterinarians.
Tuberculosis of the facial skin, lupous miliary disseminated , is a very rare form of skin tuberculosis.
It is characterized by the appearance on the face of small pinkish-brown soft nodules that can ulcerate and heal with the formation of a scar or resolve without ulceration.
Tuberculide Levandowski rosacea-like is a form of skin tuberculosis, similar to disseminated miliary tuberculosis of the face, in which, against the background of rosacea-like skin changes (erythema, telangiectasia), pinkish-brown nodules are located, sometimes with pustules in the center, drying into a crust, after rejection of which a scar remains.
The reaction to tuberculin is sharply positive.
Acute miliary skin tuberculosis is a manifestation of general miliary tuberculosis. Characteristic is the appearance on the face, trunk, and limbs of small pointed papules, somewhat reminiscent of papules in papulonecrotic tuberculosis, but with a more pronounced hemorrhagic component.
Mycobacteria are often found in papules.
Lichenoid tuberculosis (lichen scrophulosorum, lichen scrofulous) is represented by miliary papules of a yellowish-brown color or the color of normal skin. Nodules of a soft consistency, often with a small scale in the center; Flat papules with a shiny surface, reminiscent of lichen planus, may be observed.
The disease most often affects the skin of the torso, less often the limbs and face; the rashes tend to cluster.
The process is usually resolved without a trace, tuberculin reactions are positive; usually accompanies tuberculosis of other organs.
Miliary-ulcerative tuberculosis occurs secondarily as a result of autoinoculation in patients with active tuberculosis of other organs in the absence of immunity.
The usual localization is the mucous membranes of natural orifices and the surrounding skin.
The rashes are represented by nodules the size of a pinhead, which turn into pustules, and then into ulcers with an uneven and lumpy bottom, caused by yellowish nodules, which are abscesses - “Trill grains”.
All the described forms are a manifestation of secondary tuberculosis , since they all develop, as a rule, against the background of foci of tuberculosis infection already existing in the body or in people who have previously had tuberculosis, most often of pulmonary localization, as evidenced by Ghon foci and compaction of lung tissue identified during X-ray examination , focal shadows against the background of fibrous changes in the pulmonary pattern.
Primary skin tuberculosis is very rare, mainly in infants.
Represented by primary tuberculous affect or primary tuberculous chancre. This is a fairly deep-lying infiltrate that turns into an ulcer. After 2-3 weeks, lymphangitis and regional lymphadenitis develop, representing the primary tuberculosis complex.
Flow. Tuberculosis is a disease that occurs with exacerbations and, often, with relapses in the winter and autumn periods.
Exacerbation refers to the appearance of new elements on the skin during treatment and during the first year after it.
The diagnosis of tuberculosis is made by:
- anamnesis data (indications of past pulmonary tuberculosis, contact with patients),
- clinical picture,
- tuberculin test results,
- histological and cultural studies.
- Sometimes they resort to infecting laboratory animals - guinea pigs.
In cases that are difficult to diagnose, a trial treatment is permissible.
Differential diagnosis is carried out with:
- angiitis of the skin,
- skin cancer
- tubercular syphilide,
- leishmaniasis,
- deep mycoses,
- leprosy.
Treatment:
- tuberculostatic chemotherapy,
- means aimed at increasing immune defense,
- normalization of metabolic disorders,
- vitamin therapy (especially B vitamins).
It is necessary to take into account the resistance of mycobacteria to tuberculostatic agents.
- In dermatological practice, treatment usually begins with a combination of rifampicin and isoniazid, sometimes pyrazinamide or thiacetazone is added to this.
- Then these drugs are replaced with streptomycin, ethambutol, PAS.
The main course lasts on average 10-12 months.
After the main course, anti-relapse treatment is carried out.
Dispensary observation for 5 years.
See also:
Papulonecrotic tuberculosis of the skin B. A. Berenbein “Diagnostics of skin diseases” A guide for doctors.
Return to the list of articles on skin diseases
Articles about some other skin diseases:
Acrogeria familial Gottrona O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Acrodermatitis enteropathica O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Amyloidosis of the skin O. L. Ivanov, A. N. Lvov “Consultation with a dermatologist”
Sneddon-Wilkinson subcorneal dermatosis O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Itchy skin Paul K Baxton “ABC of Dermatology”
Skin mucinosis O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Wissler-Fanconi syndrome B. A. Berenbein, A. A. Studnitsin “Diagnostics of skin diseases” A guide for dermatologists.
Telangiectasia O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Tuberous sclerosis O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Phlebotoderma O. L. Ivanov, A. N. Lvov “Dermatologist’s Handbook”
Follicular mucinosis B. A. Berenbein, A. A. Studnitsin “Diagnostics of skin diseases” A guide for dermatologists.