Editor
Anna Sandalova
Pulmonologist, doctor of the highest category
The respiratory organs have constant communication with the external environment. That is why they are one of the first to respond to the influence of unfavorable factors. Occupational lung diseases (pneumoconiosis) occur with prolonged and systematic contact with industrial respiratory pathogens. An important point is the implementation of this contact during a person’s work activity.
This article will focus on silicosis. The features of the pathogenesis, clinical picture, diagnosis and treatment of the disease are considered.
General information and ICD-10 code
Pneumoconiosis is a heterogeneous group of lung diseases. They are caused by prolonged inhalation of industrial dust and are characterized by rapidly growing irreversible fibrosis.
Silicosis is one of the types of pneumoconiosis . Often in the medical history of patients you can see an alphanumeric entry: J62.8. This is the so-called ICD-10 code for pulmonary silicosis in adults.
The disease occurs due to prolonged exposure to silicon dioxide. Over the course of several years, irreversible changes occur in the lungs. Regular exposure to silica dust causes local inflammation. Further, foci of fibrosis form in the lungs. Subsequently, they organize and grow, forming nodules.
Silicosis is considered an extremely dangerous disease . It quickly leads to decompensation of the lungs and the occurrence of chronic respiratory failure.
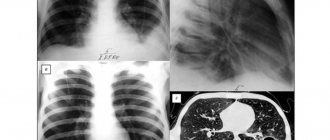
The histological picture of the disease is shown in the photo:
Silicosis, like other pneumoconioses, without proper treatment and care quickly leads to permanent disability of the patient. Therefore, treatment and prevention of industrial diseases are an important healthcare task.
Notes[ | ]
- Disease ontology database (English) - 2020.
- Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018.
- Senkevich N.A., Likhachev Yu.P.
(pat. an.), Grigoryan E.A. (rent.). Silicosis // Great Medical Encyclopedia: 30 volumes / chapter. ed. B.V. Petrovsky. — 3rd ed. - Moscow: Soviet Encyclopedia, 1985. - T. 24. Vascular suture - Teniosis. - pp. 392-400. — 544 p. — 150,800 copies. - See Silicosis in Anita L. Wolfe and Jay F. Colinet
.
The best ways to reduce dust in coal mines. Best Practices for Dust Control in Coal Mining.
DHHS (NIOSH) Publication No. 2010–110 - [www.oo2.ru/files/2006-1/___1_2006.pdf SILICOSIS OF THE PULMONARY: a disease of sandblasters?] (unspecified) // “Cleaning. Coloring". — 2006. — February (vol. No. 1). — P. 14-15. (unavailable link)
- ↑ 12
NIOSH Report on the Development and Testing of an Air Shower to Protect Miners from Dust - ↑ 1 2 Beglova Z.K.
Initial pathomorphological changes in the lungs of practically healthy workers under the influence of molybdenum mine dust: collection of articles: [rus.] / ed. Zaitsev N.A., Letavet A.A. — Institute of Mining named after. A.A. Skochinsky. - Moscow: Publishing House "Nauka", 1964. - T. 6. - P. 232-234. — 319 p. — 1000 copies. - ↑ 1 2 Bondarev O.I., Rykova O.V., Razumov V.V., Cherdantsev M.V., Bugaeva M.S.
Histological and cytological characteristics of atrophic bronchopathy in miners: [Russian] // Medicine in Kuzbass. - Kemerovo, 2012. - T. 11, No. 4 (October). — P. 35-42. - ISSN 1819-0901. - Razumov V.V., Zinchenko V.A., Danilov I.P., Tretyakova S.Yu.
Occupational hygiene and occupational pathology. Materials of the XXXVIII Scientific and Practical Conference: [Russian] / ed. Zakharenkov V.V. and others - Novokuznetsk: KuzGPA, 2003. - On the need to improve the methodological basis for the diagnosis of occupational diseases. — P. 102—104. — 200 s. — ISBN 5-85117-061-1. - [www.oo2.ru/node/168 Material quality] (undefined) // “Cleaning. Coloring". — 2008. — July (vol. No. 5). — P. 24. (inaccessible link)
- Jay F. Colinet, James P. Rider, Jeffrey M. Listak, John A. Organiscak, and Anita L. Wolfe.
Best Practices for Dust Control in Coal Mining. — National Institute for Occupational Safety and Health. — Pittsburgh, PA; Spokane, WA: DHHS (NIOSH) Publication No. 2010-110, 2010. - 84 p. There is a translation: The best ways to reduce dust in coal mines. NIOSH 2010 PDF Wiki - Andrew B. Cecala, Andrew D. O'Brien, Joseph Schall, Jay F. Colinet et al.
Dust Control Handbook for Industrial Minerals Mining and Processing. — National Institute for Occupational Safety and Health. — Pittsburgh, PA; Spokane, WA: DHHS (NIOSH) Publication No. 2012-110, 2012. - 84 p. Translated: Guide to Dust Protection in Mining and Processing 2012 PDF Wiki - Coal Mine Dust Exposures and Associated Health Outcomes. A Review of Information Published Since 1995. Translation available: Protecting US miners from coal dust
- Jon C. Volkwein, Robert P. Vinson, Steven J. Page, Linda J. McWilliams, Gerald J. Joy, Steven E. Mischler and Donald P. Tuchman.
Laboratory and Field Performance of a Continuously Measuring Personal Respirable Dust Monitor. - Pittsburgh, PA: National Institute for Occupational Safety and Health, 2006. - 55 p. — (DHHS (NIOSH) Publication No. 2006-145). There is a translation: PDF Wiki - Silica Safe: Create-A-Plan (undefined)
. web.archive.org (December 20, 2012). Retrieved September 12, 2019. - Kaptsov V.A., Chirkin A.V.
On the effectiveness of personal respiratory protection as a means of disease prevention (review) //
Federal Budgetary Institution “Russian Register of Potentially Hazardous Chemical and Biological Substances” of Rospotrebnadzor
Toxicological Bulletin. - Moscow, 2020. - No. 2 (149). — P. 2-6. — ISSN 0869-7922. - NIOSH Dust Control Guidelines (2012)
- Ivanova I.S.
Silicosis (Russian) //
Research Institute of Occupational Medicine of the Russian Academy of Medical Sciences and the State Committee for Sanitary and Epidemiological Surveillance of Russia
Occupational medicine and industrial ecology. - 1994. - No. 10. - P. 19-23. — ISSN 0016-9919. - Artamonova V.G., Mukhin N.A.
Occupational diseases. - 4th ed. - Moscow: Medicine, 2009. - P. 56-73. — 480 s. — 3000 copies. — ISBN 5-225-04789-0. - Bogdanskaya N.I., Tolgotskaya M.S.
Preventive effect of polyvinylpyridine-N-oxide of different molecular weights on experimental silicosis: [rus.] // Hygiene and Sanitation. - Moscow, 1973. - No. 4. - P. 102-104. — ISSN 0016-9900. - Velichkovsky B.T.
Basic pathogenetic mechanisms of occupational lung diseases of dust etiology (Russian) // Occupational Medicine and Industrial Ecology. - Moscow, 1999. - No. 8. - P. 20-27. — ISSN 0016-9919.
Causes
As previously stated, the main etiological risk factor is exposure to pulverized silica . If production is not provided with the latest dust suppression mechanisms, then everyone who has contact with raw materials is at risk of getting sick. Silica is widespread. It can be found at any mining facility or where minerals are processed.
Therefore, the risk group consists primarily of mining developers, foundry workers, as well as those directly involved in the production of building materials.
Pathogenesis
The pathogenesis of silicosis is not well understood . It is assumed that silica entering the lungs causes activation of alveolar macrophages. They, in turn, provoke the release of specific chemotactic factors and inflammatory mediators.
Cellular reactions begin to increase, fibroblastic elements are released. This leads to sclerosis of the lung parenchyma and a decrease in the volume of functioning tissue.
Over time, the effects of local hypoxia only increase fibrosis. Respiratory failure increases, and rapid decompensation of the condition occurs.
Etiology of the disease
Silicosis is considered an occupational disease. This pathology is widespread throughout the world and has been known for a long time.
Despite the modern development of technology, construction industries remain dusty and have a harmful effect on the respiratory system of workers, causing occupational diseases.
Once in the human lungs, silicon compounds settle in them and accumulate there. It often happens that a person, while at work, does not feel any serious deviations. But over time, even if he leaves this job, silicon in the body makes itself felt.
People who work in quarries and processing silicon-containing rocks are most susceptible to the disease. Modern machines used in this area work with large dust production without suppressing it in any way. As a result, people working for them are forced to breathe harmful dust. In some cases, even protective equipment does not help.
Silicosis may be caused by working in a quarry
The pathogenesis of silicosis is not yet fully understood. It is known that the higher the concentration of silicon dioxide in dust, the higher the likelihood of pathology occurring. Particles from 0.5 to 5 microns are considered the most dangerous. They are the most aggressive and are able to reach the pulmonary parenchyma.
With the development of immunotherapy, it was found that silicosis develops when microphages (blood particles) capture dust microparticles and die because of this. As a result, nodules begin to form. Dust, released from dead blood particles, also becomes material for the formation of nodules.
Against this background, a restructuring of the immune system begins; in patients with silicosis, an increase in immunoglobulins is observed.
Symptoms depending on stage
Symptoms of the disease depend on the clinical stage of the process. In addition, the length of work experience in hazardous conditions, the dispersion of dust particles, the concentration of silicon, and the state of human health are important.
Symptoms common to any stage are:
- dyspnea;
- chest pain;
- cough;
- intoxication manifestations (weakness, fatigue, autonomic disorders).
At the first stage of the disease, the patient is bothered by slight shortness of breath, which appears only with physical effort, a rare dry cough and low-intensity chest pain. Physical examination most often reveals no abnormalities. External respiration indicators remain within normal limits.
With the development of the second stage, the phenomena of hypoxia increase. The patient experiences shortness of breath even with minor physical exertion. Chest pain becomes constant. The cough is unproductive, paroxysmal.
Auscultation and percussion reveal signs of chronic bronchitis (dry or variable wheezing, bronchial breathing) or pulmonary emphysema (increased airiness of the lung tissue, weakened breathing). FVD reveals severe respiratory failure.
The third stage is terminal. Shortness of breath persists even at rest, the patient assumes a forced body position. The cough becomes constant. The intensity of chest pain increases. Objective data indicate pulmonary or cardiopulmonary failure. At this stage, the condition quickly decompensates.
When working in hazardous conditions, it is extremely important to undergo regular preventive examinations. Regardless of the stage of silicosis, patients must be removed from work in contact with dust.
Description and types of pulmonary silicosis
Silicon particles or grains of sand do not dissolve in water.
In addition, they are not destroyed in any biological fluids. Over time, the amount of dust in the lungs increases, forming accumulations. These particles provoke the growth of connective tissue. You get some kind of knots that make breathing difficult. Types of pulmonary silicosis:
- Acute silicosis
. Occurs in the first 3-4 months of contact with silicon particles. The symptoms are very clear. This stage of silicosis can develop into tuberculosis. - Chronic illness
. It may be asymptomatic for several years. The patient only feels a slight discomfort. - Accelerated form
. It is somewhere between acute and chronic silicosis. Develops faster than the chronic form. Against the background of this disease, autoimmune diseases often occur with the addition of a bacterial infection.
Diagnostics
The diagnosis of silicosis is established on the basis of anamnestic (working with silica), clinical (cough, shortness of breath, chest pain), laboratory (signs of inflammation) and radiological data. If pneumoconiosis is suspected, a general blood test, urine test, biochemical tests and a chest x-ray are required.
The clinical picture of the disease does not always correspond to the stage of the pathological process . In order to reliably determine the degree of disease progression, it is necessary to evaluate the x-ray picture.
The first stage of silicosis on an x-ray is characterized by an increased pulmonary pattern. Its deformation may also be observed. In addition, against the background of an inflammatory process in the lungs, slight changes in the pleura may appear. This is the so-called heaviness. On x-rays it appears as small linear shadows.
You can often find single round shadows with a diameter of about 1 mm. This is how the initial stage of fibrosis of the pulmonary parenchyma manifests itself. These nodules must be differentiated from tuberculous lesions. With mycobacterial infection, single lesions are located mainly in the upper parts of the lungs, multiple lesions are located everywhere. In silicosis, fibrous nodules are localized in the middle sections.
The second stage of silicosis is characterized by pronounced reticulation of the pulmonary field. Numerous shadows with a diameter of 2-4 mm appear. They are located mainly in the lower and middle sections. Often the nodules merge, forming a picture of a “snowstorm” (multiple shadows that are layered on top of each other). The roots of the lungs are expanded. The pleura is often thickened, and inflammatory strands are visible.
Radiological signs of the third stage are due to massive fibrosis of the pulmonary parenchyma. The shadows merge into vast conglomerates. Compensatory emphysema occurs. In the picture it looks like an alternation of darkening and brightening. Thickenings of the interlobar pleura are formed.
During the examination, it is important to evaluate the nature and severity of concomitant pathology. If a patient has decompensated cardiopulmonary diseases, the disease rapidly progresses and often has an unfavorable outcome.
Silicosis
Silicosis is a form of pneumoconiosis that develops when fibrogenic dust containing crystalline silicon dioxide (silica) is inhaled and deposited in the lungs. Silicosis became most widespread at the end of the 19th century and the first half of the 20th century. due to the rapid development of the mining industry, machine tool and mechanical engineering, where workers were exposed to dust containing free silicon dioxide. Today, the disease is becoming a thing of the past, although employment in certain industries is still associated with an increased risk of developing silicosis. Silicosis results in massive pulmonary fibrosis, which can progress even after exposure to fibrogenic dust ceases. The clinical study of silicosis is carried out by pulmonology and occupational pathology.
Treatment and clinical recommendations
Silicosis is an extremely dangerous disease, prone to progression, so treatment must be approached extremely responsibly.
Folk remedies
Treatment with folk remedies is considered unacceptable . Such tactics can lead to deterioration of the patient’s condition and disability. Various non-traditional methods are used only as adjuvant therapy. However, it is worth considering that patients often have a complicated medical history. Therefore, you can resort to such treatment only with the permission of a doctor.
At home and stationary
Silicosis can be treated both on an outpatient basis (at home, under the supervision of a doctor) and on an inpatient basis (specialized hospitals, pulmonology departments, silicosis dispensaries). The choice of regimen depends on the stage of the disease and the patient's condition. Young people who do not have concomitant diseases can be treated on an outpatient basis in the early stages.
Patients with a complicated medical history should be hospitalized in a hospital.
Treatment of silicosis is carried out according to clinical guidelines and protocols approved by the Ministry of Health. At the moment, there is no technique that can reverse the changes that have occurred. Treatment is primarily aimed at preventing complications, improving the patient’s quality of life and slowing the progression of the disease.
Therapy for silicosis includes the following areas:
- change in the patient’s working conditions (transfer to a job where there is no direct contact with dust);
- to give up smoking;
- rehabilitation therapy (special resorts);
- bronchoalveolar lavage (washing the airways followed by removal of the solution);
- pathogenetic therapy (antifibrotic, immunomodulatory agents);
- oxygen therapy (in the presence of severe oxygen deficiency).
Expert opinion
Anna Sandalova
Pulmonologist, doctor of the highest category
Ask a Question
The effectiveness of therapy directly depends on the stage of the disease and the patient’s adherence to treatment. Therefore, it is necessary to regularly undergo preventive examinations and conscientiously take the prescribed treatment.
Prognosis and prevention
Due to the fact that etiotropic therapy for silicosis has not been developed, disease prevention is of great importance.
Primary prevention is aimed at preventing contact with a pathogenic factor.
It includes:
- use of less fibrogenic materials in production;
- sealing the technological process;
- proper planning of the ventilation system;
- use of respirators with a high degree of protection;
- identification of persons predisposed to this type of disease.
The goal of secondary prevention is the early identification of patients before they develop a full-blown clinical picture.
The prognosis depends on the duration of human contact with silica, the degree of changes in the lung parenchyma, the presence of concomitant diseases and adherence to treatment. Patients whose disease is detected in the early stages and who have completed a full course of rehabilitation and treatment have a favorable prognosis. In this case, residual changes remain in the lungs without a tendency to progress.
Late detection, irrational treatment and continued exposure to harmful factors lead to a steady deterioration of the condition. At the same time, concomitant diseases may arise that worsen the prognosis (silicotuberculosis - a combination of silicosis and mycobacterial infection).
The outcome of this condition is unfavorable: systemic cardiopulmonary failure develops, worsening the quality of life, leading to disability and even death of the patient.
How to remove dust from your lungs
Therapy methods
Currently, pulmonary silicosis cannot be completely cured. All measures are aimed at stopping the progression of the disease and preventing complications. This allows a person to live longer.
The first and main condition is to stop the entry of silicon oxide into the body with dust. To do this, the patient needs to change jobs.
Subsequently, drugs are prescribed that have a cleansing effect on the patient’s lungs and blood; oxygen therapy, inhalations with various drugs and physical procedures are recommended.
Medication
Currently, treatment of silicosis with drugs is ineffective. Medicines are mainly used to treat concomitant diseases and their prevention. There are no medications that can cleanse the lungs of dust. Patients are prescribed corticosteroids, expectorants, and bronchodilators.
Patients are required to be vaccinated against influenza and pneumococcus. In case of acute progression of the disease, surgery is performed, including lung transplantation.
Oxygen therapy
In severe forms of silicosis, the patient suffers from a lack of oxygen. Therefore, he is indicated for oxygen therapy. This is when the patient is placed in a special cell, a mask is placed on his face, or he is sent to a special room. There are many methods, but they all have one goal - to give the patient more oxygen without harming the respiratory tract.
Pure oxygen has a poisonous effect on the body. Therefore, it is diluted with special gases and served to the patient in the form of a gas mixture with a high concentration of oxygen. To moisten it, a Bobrov apparatus is used so that oxygen does not dry out the airways. The following gases are used: helium, argon, carbogen.
Oxygen therapy has contraindications. These include pulmonary hemorrhages, epilepsy, and the last stage of silicosis with the presence of cavities in the lungs. People with claustrophobia are contraindicated to perform procedures in a pressure chamber.
Inhalations and physiotherapy
If a person is diagnosed with silicosis, he is advised to carry out inhalations with oxygen or drugs.
Bronchodilators and proteolytic enzymes are often prescribed for inhalation. Alkaline and salt-alkaline mixtures are actively used. This procedure promotes good expectoration and partial cleansing of the lungs from deposits of various types, including dust.
Physiotherapy also has a positive effect. Electrophoresis is prescribed for the chest, UHF, and UV radiation. These methods have a beneficial effect on the lymph and blood, which helps remove dust from the body and slow down the course of the disease.
In the first two stages, patients are sent to medical sanatoriums. It is useful to carry out breathing exercises for silicosis; many complexes have been developed for this. You should pay attention to nutrition and daily routine. Nutrition should be complete and high-calorie. Sleep should be long enough to restore strength.
Reference materials (download)
| # | File | file size |
| 1 | Medical history. Silicosis stage 1, nodular form (2g, 2s, cn, em, co). Vibration disease (stage 1-2). Vegetative-vascular polyneuropathy of the upper extremities | 68 KB |
| 2 | Federal clinical guidelines for the diagnosis, treatment and prevention of pneumoconiosis. 2014 | 1 MB |
| 3 | Occupational diseases. Pneumoconiosis. Presentation.Orlova | 967 KB |
| 4 | Clinical protocol for the diagnosis and treatment of pneumoconiosis. Ministry of Health of the Republic of Kazakhstan 2016 | 521 KB |